Abstract
Objective
This study aimed to examine the perioperative outcomes of robotic inguinal hernia repair as compared to the open and laparoscopic approaches utilizing large-scale population-level data.
Methods
This study was funded by the SAGES Robotic Surgery Research Grant (2019). The New York Statewide Planning and Research Cooperative System (SPARCS) administrative database was used to identify all adult patients undergoing initial open (O-IHR), laparoscopic (L-IHR), and robotic (R-IHR) inguinal hernia repair between 2010 and 2016. Perioperative outcome measures [complications, length of stay (LOS), 30-day emergency department (ED) visits, 30-day readmissions] and estimated 1/3/5-year recurrence incidences were compared. Propensity score (PS) analysis was used to estimate marginal differences between R-IHR and L-IHR or O-IHR, using a 1:1 matching algorithm.
Results
During the study period, a total of 153,727 patients underwent inguinal hernia repair (117,603 [76.5%] O-IHR, 35,565 [23.1%] L-IHR; 559 [0.36%] R-IHR) in New York state. Initial univariate analysis found R-IHR to have longer LOS (1.74 days vs. 0.66 O-IHR vs 0.19 L-IHR) and higher rates of overall complications (9.3% vs. 3.6% O-IHR vs 1.1% L-IHR), 30-day ED visits (11.6% vs. 6.1% O-IHR vs. 4.9% L-IHR), and 30-day readmissions (5.6% vs. 2.4% O-IHR vs. 1.2% L-IHR) (p < 0.0001). R-IHR was associated with higher recurrence compared to L-IHR. Following PS analysis, there were no differences in perioperative outcomes between R-IHR and L-IHR, and the difference in recurrence was found to be sensitive to possible unobserved confounding factors. R-IHR had significantly lower risk of complications (Risk difference − 0.09, 95% CI [− 0.13, − 0.056]; p < 0.0001) and shorter LOS (Ratio 0.53, 95% CI [0.45, 0.62]; p < 0.0001) compared to O-IHR.
Conclusion
In adult patients, R-IHR may be associated with comparable to more favorable 30-day perioperative outcomes as compared with L-IHR and O-IHR, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hernia repair remains one of the most common surgical procedures performed in the United States, with an estimated 800,000 inguinal hernia repairs (IHR) performed annually [1]. Until the late twentieth century, inguinal hernias were repaired using an open approach. Since then, advancements in minimally invasive techniques allowed for the introduction of laparoscopic, and more recently, robotic hernia repair [2].
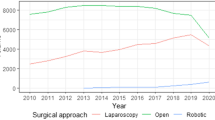
Robotic preperitoneal IHR was first described in urologic literature as a concurrent operation in patients undergoing robotic prostatectomy [3, 4]. With wider availability of the robotic platform, the last decade has seen an exponential increase in the utilization of robotic inguinal hernia repair (R-IHR) [5, 6]. Despite this rapid growth, data comparing open (O-IHR), laparoscopic (L-IHR), and R-IHR outcomes are limited to small case series and retrospective reviews with short follow-up.
This study aimed to examine the perioperative outcomes and recurrence incidence of R-IHR as compared to the open and laparoscopic approaches, utilizing large-scale population-level data.
Materials and methods
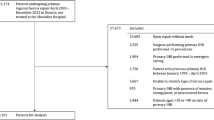
This study was funded by the SAGES Robotic Surgery Research Grant (2019). It was approved by the Institutional Review Board and informed consent was not required as data were collected from a large database containing deidentified data. The New York Statewide Planning and Research Cooperative System (SPARCS) administrative database was used to identify all adult patients undergoing O-IHR, L-IHR, and R-IHR (direct/indirect/femoral) between 2010 and 2016 in New York state. Current Procedural Terminology (CPT) and International Classification of Diseases (ICD)-9 & -10 codes were used to identify outpatient and inpatient procedures, respectively. Exclusion criteria included patients with recurrent hernia repair as their first procedure during the study period, duplicated records, age ≤ 18, or missing/unknown gender. Perioperative outcomes [complications, length of stay (LOS), 30-day emergency department (ED) visits, 30-day readmissions] and estimated 1/3/5-year recurrence rates were compared.
Statistical analysis
ANOVA under the assumption of unequal variance and Pearson’s chi-squared test with p-values from Monte Carlo simulation were used to compare patient characteristics and clinical information among different surgery groups (open, laparoscopic, robotic), as well as other clinical outcomes including any complication, 30-day readmission, and 30-day ED visit. Cumulative incidences of recurrent hernia were calculated and deaths were treated as competing risk events. Time to recurrent hernia was defined as the gap between the discharge date of the initial surgery and the admission date of the recurrent hernia, death, or last follow-up date, whichever occurred earliest. Corresponding 95% confidence intervals were reported [7].
Propensity score (PS) analysis was used to estimate the marginal (population average) differences between patients with robotic surgeries and ones with laparoscopic or open surgeries, using a 1:1 matching algorithm. A 1:1 design, as opposed to 1:1:1, was chosen to avoid driving down the sample size too low. Additionally, the differences between L-IHR and O-IHR have been extensively studied, whereas the differences between these approaches and R-IHR have not been fully investigated. All patient characteristics and comorbidities were used to estimate PS according to a logistic regression model with robotic surgery as the modeled outcome. Balanced PS matching was used to select patients from the samples with laparoscopic or open surgeries to form 1:1 pairs with the counterparts with the smallest absolute PS differences in a greedy search using the PSMATCH procedure in SAS. If for any record, no counterpart record lied within the range of 0.2 standard deviations of the logit of the estimated PS, then this record was discarded. Unmatched records were also discarded. The quality of the PS matching was assessed by checking standardized differences between groups before and after matching. Standardized differences less than 10% were considered minimal [8, 9]. Based on matched samples, McNemar’s tests were carried out for any complication, 30-day readmission, and 30-day ED visits. Wilcoxon signed rank test was performed for LOS and stratified log rank tests were used to compare recurrent hernia [10,11,12]. Sensitivity analysis for PS matching was carried out to determine the potential impact of unmeasured confounding variables on the significance of the observed outcome differences [12]. Statistical significance was set at 0.05 and analysis was done using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
From 2010 through 2016, a total of 153,727 patients underwent initial IHR in the state of New York. The majority of patients underwent O-IHR (n = 117,603, 76.5%) and L-IHR (n = 35,656, 23.1%). A minority of cases (n = 559, 0.36%) were performed robotically. Patient demographics, clinical information, and comorbidities are reviewed in Table 1. There was an increasing trend of laparoscopic and robotic hernia repairs during the study period. The majority (n = 419, 75%) of R-IHR were performed in an inpatient setting, whereas most L-IHR and O-IHR were outpatient procedures (L-IHR 94.8%, O-IHR 88.3%, R-IHR 25.0%; p < 0.0001). Patients undergoing R-IHR were generally older with 59.4% ≥ 61 years of age compared to L-IHR (34.4%) and O-IHR (47.2%) (p < 0.0001). Patients with R-IHR also had higher rates of comorbidities compared to L-IHR and O-IHR (65.3% versus 38.0% versus 45.1%, respectively; p < 0.0001), most commonly hypertension (43.7%), COPD (10.9%), and obesity (7.5%) (Table 1).
Univariate analysis found patients with R-IHR to have higher rates of any complication (9.3%, O-IHR 3.6%, L-IHR 1.1%; p < 0.0001), 30-day readmission (5.6%, O-IHR 2.4%, L-IHR 1.2%; p < 0.0001), and 30-day ED visits (11.6%, O-IHR 6.1%, L-IHR 4.9%; p < 0.0001) (Table 2). Complications were mostly cardiopulmonary in nature, such as cardiac complications (n = 5 [0.89%] vs. O-IHR n = 276 [0.23%] vs. L-IHR n = 28 [0.08%]) and pneumonia (n = 5 [0.89%] vs. O-IHR n = 718 [0.6%] vs. L-IHR n = 33 [0.09%]). There were no cases of wound-related complications (abscess, wound dehiscence) with R-IHR. LOS was greatest with R-IHR (1.74 days, O-IHR 0.66 days, L-IHR 0.19 days; p < 0.0001).
Table 3 and Fig. 1 review the unadjusted estimated cumulative incidence of recurrent hernia at 1, 3, and 5 years after initial IHR. Before propensity matching, the mean overall follow-up time was 636.1 days, with a mean follow-up time of 619.2 days for those without any recurrent hernia and 1133.3 days for those with recurrent hernia. The cumulative incidence of recurrence was greatest after O-IHR, and lowest after L-IHR. The overall incidence of recurrence was 6.4% at 5 years (L-IHR 3.9%, R-IHR 6.5%, O-IHR 7.0%). In this unadjusted cohort, overall mean recurrence-free time was 622.8 days (L-IHR 529.9 days, R-IHR 641.6 days, O-IHR 650.8 days).
PS analysis found 346 matched pairs of R-IHR and L-IHR (Table 4) and 459 matched pairs of R-IHR and O-IHR (Table 5). McNemar’s test demonstrated no difference in any complication, 30-day readmission, or 30-day ED visit between R-IHR and L-IHR (Table 6). There was no significant difference in LOS between the matched pairs. In comparing R-IHR and O-IHR, McNemar’s test found a lower risk of any complication with robotic surgery, with an estimated risk difference of − 0.0915 (95% CI [− 0.1273, − 0.0557]; p < 0.0001) (Table 6). Using Wilcoxon signed rank tests and generalized linear regression model, patients with R-IHR had a significantly shorter LOS than O-IHR (estimated ratio = 0.53, 95% CI [0.45, 0.62]; p < 0.0001). Sensitivity analysis found these differences (any complication and LOS) to persist even after adjusting for potential unmeasured confounding variables.
Matched samples were compared for time to recurrent hernia using stratified log rank tests. For R-IHR versus L-IHR, the mean overall follow-up time was 568.3 days, with a mean follow-up time of 557.7 days for those without recurrent hernia and 1018.3 days for those with recurrent hernia. For R-IHR versus O-IHR, the mean overall follow-up time was 651.1 days, with a mean follow-up time of 638.4 days for those without recurrent hernia and 1087.1 days for those with recurrent hernia. R-IHR was suggested to have significantly higher risk of recurrent hernia compared with L-IHR (p = 0.0455), with a z-statistic equal to 2 (positive z-statistic indicating more observed events than expected, implying higher risk of recurrent hernia). This significant difference was found to be sensitive to possible unmeasured confounding factors in the sensitivity analysis. There was no significant difference in time to recurrent hernia between R-IHR and O-IHR (p = 1; z-statistic = 0).
Discussion
In accordance with national trends, utilization of R-IHR in the state of New York increased annually from 2010 to 2016 [5, 6]. Despite this rise in robotic operative volume, O-IHR remained the most common approach followed by L-IHR. Univariate analysis demonstrated R-IHR to have longer LOS and higher rates of overall complications compared to both O-IHR and L-IHR. Higher rates of overall complications in R-IHR compared to other approaches was consistent with data from a recent univariate analysis performed by Huerta et al. [13] However, these trends did not persist on PS analysis. Poorer outcomes on the univariate analysis may be explained by the higher baseline incidence of cardiopulmonary comorbidities and obesity in the robotic cohort (Table 1). After 1:1 propensity matching, there were no differences in perioperative outcomes between R-IHR and L-IHR. Furthermore, R-IHR was found to have a significantly lower risk of complications and shorter LOS compared to O-IHR.
In terms of recurrence, R-IHR was associated with a higher incidence of recurrence compared to L-IHR; however, this was found to be sensitive to possible unobserved confounding factors. As discussed in the meta-analysis conducted by Aiolfi et al., such factors may include surgeon experience [14]. With propensity matching, we accounted for hospital volume as a surrogate for surgeon volume and experience, but there remains room for error. Future studies will need to investigate if the incidence of recurrence changes over time as surgeon experience increases, particularly with newer generations of robotic technology.
While this study was not designed to specifically compare L-IHR with O-IHR, there was a remarkably lower risk of complications and recurrence with the laparoscopic approach. This may be a consequence of baseline patient characteristics or the acuity with which patients presented, allowing for selection bias. Patients undergoing O-IHR had higher rates of baseline comorbidities and higher rates of inpatient procedures compared to L-IHR (Table 1). These patients may have presented more acutely, necessitating an emergent procedure, contributing to the decision for an open procedure and subsequent outcomes. Alternatively, these outcomes may suggest that as we are later in the learning curve for laparoscopy, we are seeing improved outcomes compared to historical studies comparing the open and laparoscopic approaches.
Previously, several small-scale studies have reported on the feasibility and short-term outcomes of R-IHR. The largest case series to date was published by Tam et al., reporting short-term outcomes of 335 consecutive R-IHR across seven hospitals [15]. They found a low incidence of intraoperative complications (0.6%) and an overall complication rate of 16%, which were most commonly urinary retention (4.2%) and scrotal swelling (3.9%). This was a retrospective review over 19 months with a mean follow-up of only 18 days.
Comparative outcomes data are scarce and limited mostly to retrospective reviews with short-term outcomes. In a propensity-matched study performed by Bittner et al., R-IHR and L-IHR patients reported similar acute postoperative groin pain through surveys that used the validated Numeric Pain Rating Scale to objectively quantify pain [16]. Analogous findings were demonstrated in a randomized clinical trial conducted by Prabhu et al., which found no significant differences in R-IHR and L-IHR postoperative pain as measured through the Visual Analog Scale [17]. Like the results of the 1:1 propensity matching of the present study, these studies suggest insignificant difference in the perioperative outcomes between R-IHR and L-IHR patients. However, these studies were limited by their overall sample size (patient matches in Bittner et al. were 83 R-IHR to 83 L-IHR and 85 R-IHR to 85 O-IHR, and only 102 total patients were included in Prabhu et al.) as well as the breadth of their respective outcomes.
A 2018 retrospective review of the American College of Surgeons National Surgical Quality Improvement Program database found R-IHR to have longer operative times, but similar rates of postoperative adverse events and readmissions compared to L-IHR and O-IHR [18]. The study was limited by the overall small sample size of patients undergoing R-IHR (R-IHR n = 69, L-IHR n = 241, O-IHR n = 191). The present study is a similar retrospective review, but includes a much larger sample size, particularly R-IHR. More recently, Pokala et al. compared the outcomes of all three approaches using the national Vizient clinical database [19]. This study included a larger sample size of robotic procedures (n = 594) and found R-IHR to have the lowest overall complication rate (0.67%) compared to L-IHR (4.44%) and O-IHR (3.85%), p < 0.05. The authors concluded that minimally invasive IHR had outcomes superior to open repair despite higher cost. The present study supports these data with the addition of long-term recurrence data.
There are limitations to our study inherent to the use of a retrospective administrative database. The data rely on proper coding with the potential for clerical error. Clinical data are limited as the SPARCS database does not provide operative data related to hernia size, mesh use, type of mesh, and method of mesh fixation. Hospital cost is also a variable which is not captured by the database. Additionally, as mentioned previously, it is difficult to take surgeon experience into account as this is not a captured variable. In the present study, we used hospital volume as a proxy, which is less precise. Selection bias should also be considered, particularly in the decision for an open versus minimally invasive (robotic or laparoscopic) approach. Surgeon comfort level or experience and patient acuity may have contributed to the surgical approach and subsequent outcomes. Despite these limitations, the ability to track patients longitudinally statewide allows for comparison of long-term outcomes.
Conclusion
This study demonstrates that in adult patients in New York state, R-IHR may be associated with comparable to more favorable 30-day perioperative outcomes, as compared with L-IHR and O-IHR, respectively, but with longer LOS. Further randomized studies are needed to assess the clinical variables contributing to these outcomes.
References
Bittner R, Schwarz J (2012) Inguinal hernia repair: current surgical techniques. Langenbeck Arch Surg 397(2):271–282
Poelman MM, van Heuvel B, Deelder JD, Abis GSA, Beudeker N, Bittner RR, Campanelli G, van Dam D, Dwars BJ, Eker HH, Fingerhut A, Khatkov I, Koeckerling F, Kukleta JF, Miserez M, Montogmery A, Munoz Brands RM, Morales Conde S (2013) EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc 27(10):3505–3519
Finley DS, Rodriguez E Jr, Ahlering TE (2007) Combined inguinal hernia repair with prosthetic mesh during transperitoneal robot assisted laparoscopic radical prostatectomy: a 4-year experience. J Urol 178(4):1296–1300
Ito F, Jarrard D, Gould JC (2008) Transabdominal preperitoneal robotic inguinal hernia repair. J Laparoendosc Adv Surg Tech 18(3):397–399
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911
Childers CP, Maggard-Gibbons M (2018) Estimation of the acquisition and operating costs for robotic surgery. JAMA 320(8):835–836
Coviello V, Boggess M (2004) Cumulative incidence estimation in the presence of competing risks. Stata J 4(2):103–112
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrene Earlbaum Associates, Lawrence
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 1:41–55
Rosenbaum PR (2007) Sensitivity analysis for m-estimates, tests, and confidence intervals in matched observational studies. Biometrics 63(2):456–464
Everitt B, Howell DC (2005) Encyclopedia of statistics in behavioral science. Wiley, Hoboken
Rosenbaum PR (2002) Observational studies. Springer, New York
Huerta S, Timmerman C, Argo M, Favela J, Pham T, Kukreja S, Yan J, Zhu H (2019) Open, laparoscopic, and robotic inguinal hernia repair: outcomes and predictors of complications. J Surg Res 241:119–127
Aiolfi A, Cavalli M, Micheletto G, Lombardo F, Bonitta G, Morlacchi A, Bruni PG, Campanelli G, Bona D (2019) Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23(3):473–484
Tam V, Rogers DE, Al-Abbas A, Borrebach J, Dunn SA, Zureikat AH, Zeh HJ, Hogg ME (2019) Robotic inguinal hernia repair: a large health system’s experience with the first 300 cases and review of the literature. J Surg Res 235:98–104
Bittner Iv JG, Cesnik LW, Kirwan T, Wolf L, Guo D (2018) Patient perceptions of acute pain and activity disruption following inguinal hernia repair: a propensity-matched comparison of robotic-assisted, laparoscopic, and open approaches [published correction appears in J Robot Surg. 2018 Jun 18]. J Robot Surg. 12(4):625–632
Prabhu AS, Carbonell A, Hope W, Warren J, Higgins R, Jacob B, Blatnik J, Haskins I, Alkhatib H, Tastaldi L, Fafaj A, Tu C, Rosen MJ (2020) Robotic Inguinal vs Transabdominal Laparoscopic Inguinal Hernia Repair: The RIVAL Randomized Clinical Trial. JAMA Surg 155(5):380–387
Charles EJ, Mehaffe JH, Tache-Leon CA, Hallowell PT, Sawyer RG, Yang Z (2018) Inguinal hernia repair: is there a benefit to using the robot? Surg Endosc 32:2131–2136
Pokala B, Armijo PR, Flore L, Hennings D, Oleynikov D (2019) Minimally invasive inguinal hernia repair is superior to open: a national database review. Hernia 23:593–599
Acknowledgements
We acknowledge the biostatistical consultation and support provided by the Biostatistical Consulting Core at the Stony Brook University School of Medicine. We would like to thank the SAGES Research and Career Development Committee for their support and funding.
Funding
This study was funded by the 2019 SAGES Robotic Surgery Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Konstantinos Spaniolas reports grants from Merck, and is a speaker for Gore outside the submitted work. Aurora D. Pryor reports personal fees from Ethicon, Gore, Merck, Medtronic, and Stryker, grants and personal fees from Obalon, grants from Baronova, outside the submitted work. Talar Tatarian, Connor McPartland, Andrew M Brown, Jie Yang, Lizhou Nie, Maria S. Altieri, and Salvatore Docimo declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Accepted as a Quickshot Presentation and ePoster at the SAGES 2020 Annual Meeting.
Rights and permissions
About this article
Cite this article
Tatarian, T., Nie, L., McPartland, C. et al. Comparative perioperative and 5-year outcomes of robotic and laparoscopic or open inguinal hernia repair: a study of 153,727 patients in the state of New York. Surg Endosc 35, 7209–7218 (2021). https://doi.org/10.1007/s00464-020-08211-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08211-1