Abstract
Background
Historically, pre-operative biliary stenting has been associated with higher infectious complication rates following pancreatoduodenectomy. However, alleviation of biliary obstruction is necessary for consideration of pre-operative chemotherapy, which may improve disease-free survival, or for mitigation of symptoms while awaiting surgery. Our aim is to compare contemporary post-operative complication risk among patients with pre-operative endoscopic retrograde cholangiopancreatography (ERCP) stenting compared to those without.
Methods
Patients who underwent a pancreatoduodenectomy for pancreatic cancer with biliary obstruction within the ACS-NSQIP registry from 2014 to 2017 were identified. The primary outcome was to compare the risk of 30-day complication (composite outcome) between patients with and without pre-operative ERCP stenting. Propensity score matching was used to ensure balanced baseline characteristics and log-binomial regression models were used to estimate risk ratios for overall perioperative complication between groups.
Results
From 6073 patients with obstructive jaundice undergoing pancreatoduodenectomy for pancreatic cancer, 92% (5564) were eligible for the study. After performing a propensity score matching on 20 baseline characteristics, 952 patients without stenting were matched to up to four patients who received pre-operative ERCP stenting (n = 3467) for a matched cohort of 4419. A total of 1901 (55%) patients with pre-operative ERCP stenting experienced a post-operative complication compared to 501 (53%) patients without stenting (risk ratio 1.04, 95% CI 0.97–1.11, p = 0.23).
Conclusion
Pre-operative ERCP stenting was not associated with an increased risk of post-operative complication in patients undergoing pancreatoduodenectomy with obstructive jaundice. Biliary stenting may be safely considered for symptom relief and to potentially facilitate pre-operative chemotherapy for pancreatic cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pancreatic cancer located within the head of the pancreas commonly presents with obstructive jaundice. Endoscopic retrograde cholangiopancreatography (ERCP) is a common diagnostic modality that can obtain tissue for definitive diagnosis and alleviate biliary obstruction via stent insertion [1]. If pre-operative chemotherapy is a consideration due to borderline resectability, cholestasis must be addressed to avoid augmented hepatotoxicity related to chemotherapy. Moreover, hyperbilirubinemia has been associated with a greater perioperative risk of blood transfusion, immune dysregulation, and renal impairment following pancreatoduodenectomy [2, 3]. However, this must be tempered against a higher risk of infectious complications associated with biliary stenting prior to pancreatoduodenectomy [4].
Previously, there has been conflicting evidence regarding the safety of ERCP stenting prior to pancreatoduodenectomy [4,5,6]. Despite an aggressive surgical approach, outcomes for pancreatic cancer remain poor, leading to an increasing utilization of biliary stenting to facilitate wider use of pre-operative chemotherapy and a delay in surgical intervention [7,8,9]. Current guidelines do not recommend routinely use of ERCP stenting prior to surgery, however, stent placement may be considered with severe symptomatic jaundice, cholangitis or expected delay in surgery, such as neoadjuvant therapy [10].
In this study, we examined whether ERCP stenting in contemporary practice was associated with an increased risk of complications among patients with pancreatic cancer and obstructive jaundice.
Materials and methods
Design, setting and participants
The National Surgical Quality Improvement Project (NSQIP) was implemented in the United States in all Veterans Affairs hospitals in 1994 to study the ratio of observed to expected adverse events and identify areas for quality improvement [11]. In 2001 the American College of Surgeons (ACS) launched a pilot to enroll NSQIP into private sector hospitals and by 2004 ACS-NSQIP became the first program “to measure and improve the quality of surgical care across the private sector” [12]. Currently, more than 600 ACS-NSQIP participating hospitals in U.S. and Canada perform a systematic review of all surgical procedures for improvement of quality of care and research purposes [13]. Data is collected prospectively by a surgical clinical reviewer (registered nurses or data analysts) on pre-operative, intraoperative and post-operative occurrences up to 30 days after the operation. Data reliability is rigorously maintained by external inter-rater reliability audits and by internal data validation audits [14]. Ethics approval was obtained from Western University’s Research Ethics Board and there was no need for written consents.
The ACS-NSQIP demographic data file and the procedure targeted participant use data file for pancreatectomy from 2014 to 2017 was used. All participants were 18 years of age or older and underwent a total or subtotal proximal pancreatectomy for pancreatic cancer (current procedural terminology codes: 48,150, 48,152, 48,153, 48,154, 48,155). Patients without obstructive jaundice or with a diagnosis other than ampullary carcinoma, distal cholangiocarcinoma, invasive intraductal papillary mucinous neoplasm or pancreatic adenocarcinoma were excluded. The results presented here are reported following the STROBE (Strengthening the Reporting of Observation Studies in Epidemiology) (eTable 1) [15].
Data collection and measures
Demographic characteristics in the ACS-NSQIP data included age, sex, race, and Body Mass Index (BMI). Pre-operative characteristics, including previous health (tumor–node–metastasis [TNM] stage, diabetes mellitus, insulin dependence, current smoker, etc.), pre-operative laboratory values and pre-operative treatments were collected. The primary outcome was a composite of post-operative complications within 30 days after surgery. The composite encompassed a total of 21 complications (twelve major and nine minor); major and minor complications were classified based on Clavien-Dindo ≥ III and < III complications, respectively [16]. Overall codes and definitions are provided in eTables 2, 3, 4. Secondary outcomes included all individual complications, length of stay and the comprehensive complication index (CCI). This index, developed by Slankamenac et al., was created to calculate the sum of all post-operative complications weighting them by their severity (using Clavien-Dindo classification). The index assigns patients a score between 0 and 100 based on their burden of all complications; 0 equal to no complication and 100 equals to death [17].
Statistical analysis
Patients characteristics are summarized using the median (25th, 75th percentile) or frequency (percentage). A logistic regression model was used to estimate propensity scores of not being stented based on 20 baseline characteristics (demographics, pre-operative characteristics, and operative characteristics [laparoscopic and emergency case]) (Table 1). Patients with pre-operative jaundice were identified through the variable ‘PAN_JAUNDICE’; however, exact levels of bilirubin before and after ERCP stenting were not available. For this reason, bilirubin levels were not included in the propensity score model. A greedy matching algorithm without replacement, and a caliper width of 0.2 standard deviations of the logit of the propensity score were used to match patients without stenting to ≤ 4 patients with stenting [18]. Weighted standardized differences were used to compare baseline characteristics between matched groups and any difference greater than 10% was considered significant [19].
Log-binomial regression, with generalized estimating equations (GEE) accounting for the correlation within matched sets, was used to estimate risk ratios (RRs) for post-operative complication, major complication and mortality within 30-days in patients that received a pre-operative biliary stent compared to those who did not. Binomial regression with an identity link function was used to estimate risk differences and their 95% confidence intervals, with GEE used to account for correlation within matched sets.
As an exploratory analysis, negative binomial regression was used to compare the comprehensive complication index between groups and a log-binomial model to examine the individual components of the composite outcome. To compare the length of stay between groups a negative binomial regression was also employed, as the variance was expected to exceed the mean and therefore be over-dispersed for a Poisson distribution.
A two-tailed p-value less than 0.05 was considered statistically significant for all analyses. Analyses were conducted using Statistical Analysis Software (SAS©, version 9.4).
Results
Patient selection is presented in Fig. 1. A total of 6073 cases with pancreatic carcinoma and obstructive jaundice were identified using the procedure targeted participant use data file for pancreatectomy from 2014 to 2017. Patients with a percutaneous or unknown stent status (n = 474), or without a proximal pancreatectomy (n = 35) were excluded. From 5564 patients with obstructive jaundice undergoing pancreatoduodenectomy for pancreatic cancer, 952 patients without stenting were matched to up to four patients who received pre-operative ERCP stenting (n = 3467), for a matched cohort of 4419.
Baseline characteristics
Before matching, there were 4576 patients with pre-operative stenting and 988 patients without. The median age in both groups was 67 years (60, 74), and patients with pre-operative stenting had 4% less females, 4% more Caucasians and 3% had a BMI ≥ 30 kg/m2 than those patients without stenting. Pre-operative chemotherapy was given to 667 (15%) patients with pre-operative stenting vs. 58 (6%) patients without.
Pre-operative baseline characteristics between pre-matched and matched patients are shown in Table 1. After matching, patients had a median age of 67 years (60, 74), about half were women (45%), almost three-quarters were Caucasian (74%) and 23% had a BMI of ≥ 30 kg/m2. According to the tumor–node–metastasis (TNM) classification, most patients had stage IIB disease (T3 [83%], N1 [72%] and M0 [99%]) [20, 21]. Pre-operative chemotherapy was given in up to 7% of the patients and most operations were open (98%). From 4419 pancreatectomies, 59% were total pancreaticoduodenectomies and 41% were subtotal. After matching, all 20 measured baseline characteristics were well balanced between the two groups, with all standardized differences less than 10%.
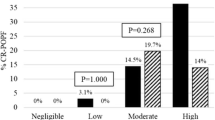
Overall post-operative complications
Post-operative complications in the first 30 days after surgery are shown in Table 2. From 4419 patients, 2402 (54%) patients experienced a total of 4760 perioperative complications, 26% of patients had one complication and 28% had two or more complications (Fig. 2). The most common type of complication was an intra or post-operative blood transfusion (21%), followed by delayed gastric emptying (16%) and deep incisional SSI (13%).
Post-operative complications between patients with or without pre-operative ERCP stenting
Out of 3467 patients that underwent pre-operative ERCP stenting, 1901 (55%) experienced a perioperative complication, compared to 501 (53%) of 952 patients without stenting (RR 1.04, 95% CI 0.97–1.11, p = 0.23).
Major complications were present in 19% of patients with stent and in 16% of patients without (RR 1.16, 95% CI 0.99–1.36, p = 0.06). Minor complications were present in 36% of patients with and without a stent (RR 0.98, 95% CI 0.89–1.08, p = 0.80) (Table 2).
Post-operative mortality within 30-days was comparable among patients with a pre-operative stent (61 [1.7%]) and without (17 [1.7%) (RR 0.99, 95% CI 0.58–1.68, p = 0.96).
Secondary measures
Patients with a stent had a median comprehensive complication index of 21 (0–48) compared to patients without a stent who had a median CCI of 9 (0–47), (RR 1.05, 95% CI 0.96–1.15, p = 0.20) (eTable 5).
An exploratory analysis of all the individual complications can be found in appendix 1 (eTable 6). A slightly increased risk of sepsis in patients with a stent (10%) compared to patients without (7%) was observed, (RR 1.51, 95% 1.17–1.94), and the risk of pancreatic fistula was also 2% higher in patients with a stent compared to patients without (RR 1.45, 95% 1.01–2.08).
Pre-operative stenting was associated with a shorter length of hospital stay for patients with a stent, with a median of 8 (6, 13) days compared to a median of 9 (7, 15) days for those without stent (RR 0.89, 95% CI 0.84–0.95).
Discussion
In this cohort between 2014 and 2017, encompassing more than one-hundred centers across U.S. and Canada, the risk of peri-operative complication was compared between patients who received an ERCP stenting before pancreatoduodenectomy for pancreatic cancer, and those who did not receive stenting. Overall, major, and minor complications between patients with or without pre-operative ERCP stenting were not significantly different.
Previous studies have shown that routine pre-operative ERCP stenting in patients with pancreatic adenocarcinoma is not beneficial and poses a higher risk of post-operative complication compared to surgery alone [3,4,5, 20]. In our study, the relative risk of overall peri-operative complication in patients with pre-operative ERCP stenting was lower (RR 1.04, 95% CI 0.97–1.10, p = 0.23) than that reported by Fang et al. (rate ratio 1.66, 95% CI 1.28 to 2.16, p < 0.001). This meta-analysis included six randomized control trials from 1982 to 2010 and compared the outcomes between patients with pre-operative stenting vs. those without; all included patients presenting with obstructive jaundice [5]. Reasons for this variation may be explained by the years of the trials (1982–2010), and the increased use of percutaneous drainage in the intervention group (67% of the studies).
Our study shows an overall complication rate of 55% for patients with stent compared to 53% for patients without; this differs from that published by Scheufele et al. in 2017. They conducted a meta-analysis encompassing 25 studies (22 retrospective and 3 randomized control trials) with a sample size of 6214 patients. They included patients with obstructive jaundice and pancreatic head tumors and compared morbidity and mortality between patients with pre-operative stenting and those without. The study showed an increased incidence of post-operative complications in patients receiving pre-operative stenting compared to patients without (49% vs. 43%, respectively, [OR 1.40, 95% CI 1.14–1.72, p = 0.002]). Some of the limitations of this study are the inclusion of older retrospective studies (median year of publication 2005 [25–75th percentile, 2001–2010]), and a high ratio of retrospective studies vs. randomized control trials (22 vs. 3). Older studies may have had different practices (preferential use of plastic stent over metal stent) that lead to an increased incidence of complications compared to contemporary practices [22]. This study also reports odds ratios rather than risk ratios, which may overestimate the relative risk considering the outcome is not rare.
Our study showed no significant differences for major complications (Clavien-Dindo ≥ 3) between patients with and without stents (19% vs. 16%, p-value = 0.06, respectively) [16]. This differs from a randomized control trial published in 2010. This study, with a cohort of 196 patients, reported higher serious complications (74% vs. 39%, p-value < 0.01) between patients with pre-operative ERCP stenting compared to patients without, respectively [4]. A possible reason for their higher rate for some of these serious complications could be the exclusive use of plastic stents and the lack of routine prophylactic antibiotics [23]. Multiple studies have shown that plastic stents compared to metal stents are associated with more complications (46% vs. 24%, respectively), such as stent occlusion, reintervention, and cholangitis [6, 9, 24,25,26,27].
Even though our study did not show statistical differences between the rate of overall and major complications between groups, pre-operative stenting was associated with shorter length of hospital stay compared to those without stenting (median of 8 [6, 13] vs. 9 [7, 15] days, respectively, p-value < 0.01). This is statistically significant, but is unlikely to be clinically significant, which might be explained due to the large sample size. As such, our study also had overall shorter length of stay compared to the randomized control trial published in 2010; the patients included in this study also seem to differ from ours, as patients with pre-operative stenting had longer length of stay compared to patients without stenting (median of 15 [10, 20] vs. 13 [11, 22] days, respectively); the longer length of stay in patients with pre-operative stenting could be attributed to their higher rate of major complications compared to patients without stenting [4].
The exploratory analysis showed a slight increased risk of sepsis in patients with stent (10%) compared to patients without (7%), (RR 1.51, 95% 1.17–1.94). This resembles a meta-analysis from 2015, which included a total of 44 studies (eight RCTs, 13 prospective studies and 23 retrospective studies), with a total population of 6286. From the 44 studies, only 7 trials reported the incidence of sepsis. Overall sepsis occurred in 10% of patients with pre-operative biliary drainage compared to 7% without (OR 1.70, CI 0.75 to 3.85; p = 0.20). Although the sepsis rates were similar between our study and the meta-analysis, our study was statistically significant. This did not seem to statistically increase the rate of major complications (19% vs. 16%), the length of stay (8 vs. 9 days, respectively), nor the mortality rate (1.7% vs. 1.7%, respectively) among groups. Although this was not studied, there is some potential for some patients to encounter delay to adjuvant treatments as a result of a septic insult [28].
A meta-analysis published in 2011, composed of 1826 patients with malignant obstructive jaundice from fourteen retrospective studies, reported no increased risk of post-operative abdominal abscess or delayed gastric emptying. Similar to this, our study did not find increased risk for these complications [29].
ACS-NSQIP registry provides well-controlled and audited recording of post-operative complications and treatments, which enabled us to calculate a score like the CCI. The CCI has been externally validated and it reduces the risk of minimizing complications [30]. Most studies that assess post-operative complications tend to report the most severe complication per patient rather than the accumulation of complications. The CCI allowed the comparison of the number and severity of multiple complications between patients with and without stenting and no significant difference between them was evident (RR 1.05, 95% CI 0.96–1.15, p = 0.20).
This study has several strengths. The large sample size obtained from over one-hundred hospitals from U.S. and Canada increases the heterogeneity of the population, permits generalizability of conclusions and gives enough power to detect small differences between groups. Data is prospectively collected and its high quality is maintained by detailed, strict clinical definitions, rather than just codes, and it has tight controls over data collection and continuous auditing [31]. By matching on propensity scores estimated using 20 pre-operative variables, the possibility of bias due to confounding was reduced.
This study has some limitations. Having data collected anonymously from many centers impeded making more inquiries regarding important data (e.g. the type of stent used [plastic/metallic], number of pre-operative ERCPs, number of stents used and low vs. high-volume ERCP centers). This prevented comparing post-operative complications between types of stent. Data regarding complications post-ERCP stenting, and pre-surgery, were not captured, which increases the chance of underestimating the resultant number of complications from pre-operative ERCP stenting. Even though post-operative complications were available for analysis, ACS-NSQIP does not provide a standardized post-operative complication classification and the treatment provided to treat these complications is not reported. As in all non-randomized studies, confounding by indication might affect certain results. In this study, confounding by indication can occur with obstructive jaundice and ERCP stenting. The indication for stenting (obstructive jaundice) might precipitate the outcome, rather than the exposure (stenting) itself. To adjust for this, a matched population was used and all patients without jaundice were excluded [32]. To keep anonymity within centers, ACS-NSQIP registry does not provide specific characteristics from each center, which prevented comparing outcomes between community vs. academic hospitals and low vs. high-volume ERCP centres.
Conclusion
This study observed a similar risk of overall post-operative complication in pancreatoduodenectomy patients that received pre-operative ERCP stenting compared to patients that did not receive stenting. Contemporary ERCP stenting to alleviate biliary tract obstruction appears safe and affords the opportunity to consider pre-operative chemotherapy and improved pre-operative clinical status.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- CCI:
-
Comprehensive complication index
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- GGE:
-
Generalized estimating equations
- IPMN:
-
Intraductal papillary mucinous neoplasm
- OR:
-
Odds ratio
- RR:
-
Risk ratio
- SIRS:
-
Systemic inflammatory response syndrome
References
Wang AY, Yachimski PS (2018) Endoscopic management of pancreatobiliary neoplasms. Gastroenterology 154(7):1947–1963
Sauvanet A, Boher JM, Paye F, Bachellier P et al (2015) Severe jaundice increases early severe morbidity and decreases long-term survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. J Am Coll Surg 221(2):380–389
Lee PJ, Podugu A, Wu D, Lee AC et al (2018) Preoperative biliary drainage in resectable pancreatic cancer: a systematic review and network meta-analysis. HPB 20(6):477–486
van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ et al (2010) Preoperative biliary drainage for cancer of the head of the pancreas. N Engl J Med 362(2):129–137
Fang Y, Gurusamy KS, Wang Q, Davidson BR et al (2013) Meta-analysis of randomized clinical trials on safety and efficacy of biliary drainage before surgery for obstructive jaundice. Br J Surg 100(12):1589–1596
Boulay BR, Parepally M (2014) Managing malignant biliary obstruction in pancreas cancer: choosing the appropriate strategy. World J Gastroenterol 20(28):9345–9353
Abrams RA, Lowy AM, O’Reilly EM, Wolff RA et al (2009) Combined modality treatment of resectable and borderline resectable pancreas cancer: expert consensus statement. Ann Surg Oncol 16(7):1751–1756
Tsuboi T, Sasaki T, Serikawa M, Ishii Y et al (2016) Preoperative biliary drainage in cases of borderline resectable pancreatic cancer treated with neoadjuvant chemotherapy and surgery. Gastroenterol Res Pract. https://doi.org/10.1155/2016/7968201
Decker C, Christein JD, Phadnis MA, Mel Wilcox C et al (2011) Biliary metal stents are superior to plastic stents for preoperative biliary decompression in pancreatic cancer. Surg Endosc 25(7):2364–2367
Abbott DE (2014) Pancreatic adenocarcinoma. Complex Gen Surg Oncol A 2:129–141
Fink AS, Campbell DA, Mentzer RM, Henderson WG et al (2002) The National surgical quality improvement program in non-veterans administration hospitals: Initial demonstration of feasibility. Ann Surg 236(3):344–354
ACS-NSQIP history. https://www.facs.org/quality-programs/acs-nsqip/about/history. Accessed 5 July 2018
ACS NSQIP participant use data file. https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed 3 July 2018
Bernard AC, Davenport DL, Chang PK, Vaughan TB et al (2009) Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg 208(5):931-937.e2
von Elm E, Altman DG, Egger M, Pocock SJ et al (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240(2):205–213
Slankamenac K, Graf R, Barkun J, Puhan MA et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258(1):1–7
Austin PC (2008) Assessing balance in measured baseline covariates when using many-to-one matching on the propensity-score. Pharmacoepidemiol Drug Saf 17(12):1218–1225
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28(25):3083–3107
Edge SB, Compton CC (2010) The american joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474
Zins M, Matos C, Cassinotto C (2018) Pancreatic adenocarcinoma staging in the era of preoperative chemotherapy and radiation therapy. Radiology 287(2):374–390
Scheufele F, Schorn S, Demir IE, Sargut M et al (2017) Preoperative biliary stenting versus operation first in jaundiced patients due to malignant lesions in the pancreatic head: a meta-analysis of current literature. Surg (United States) 161(4):939–950
Gavazzi F, Ridolfi C, Capretti G, Angiolini MR et al (2016) Role of preoperative biliary stents, bile contamination and antibiotic prophylaxis in surgical site infections after pancreaticoduodenectomy. BMC Gastroenterol 16(1):1–11
Tol JAMG, Van Hooft JE, Timmer R, Kubben FJGM et al (2016) Metal or plastic stents for preoperative biliary drainage in resectable pancreatic cancer. Gut 65(12):1981–1987
Sung JY, Leung JWC, Shaffer EA, Lam K et al (1993) Bacterial biofilm, brown pigment stone and blockage of biliary stents. J Gastroenterol Hepatol 8(1):28–34
Adams MA, Anderson MA, Myles JD, Khalatbari S et al (2012) Self-expanding metal stents (SEMS) provide superior outcomes compared to plastic stents for pancreatic cancer patients undergoing neoadjuvant therapy. J Gastrointest Oncol 3(4):309–313
Boulay BR, Gardner TB, Gordon SR (2010) Occlusion rate and complications of plastic biliary stent placement in patients undergoing neoadjuvant chemoradiotherapy for pancreatic cancer with malignant biliary obstruction. J Clin Gastroenterol 44(6):452–455
Chen Y, Ou G, Lian G, Luo H et al (2015) Effect of preoperative biliary drainage on complications following pancreatoduodenectomy: a meta-analysis. Medicine (United States) 94(29):1–9
Qiu YD, Bai JL, Xu FG, Ding YT (2011) Effect of preoperative biliary drainage on malignant obstructive jaundice: a meta-analysis. World J Gastroenterol 17(3):391–396
de la Plaza LR, Ramia Ángel JM, Bellón Caneiro JM, Arteaga Peralta V et al (2018) Clinical validation of the Comprehensive Complication Index as a measure of postoperative morbidity at a surgical department: a prospective study. Ann Surg. 268(5):838–844
Lawson EH, Louie R, Zingmond DS, Brook RH et al (2012) A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 256(6):973–981
Partap U, Allcock SH, Parker E, Gurdasani D et al (2018) Association between early life antibiotic use and childhood overweight and obesity: a narrative review. Glob Health Epidemiol. https://doi.org/10.1017/gheg.2018.16
Acknowledgements
Will acknowledge in all reports that the source of the data is the participating hospital(s) that submitted data to the ACS NSQIP and will include the following disclosure on any presentation or published material. The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. The source of the data herein this publication is from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) and the participating hospitals.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Garcia-Ochoa, Skaro, Leslie, Hawel and Mr. McArthur have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Garcia-Ochoa, C., McArthur, E., Skaro, A. et al. Pre-operative stenting and complications following pancreatoduodenectomy for pancreatic cancer: an analysis of the ACS-NSQIP registry. Surg Endosc 35, 6604–6611 (2021). https://doi.org/10.1007/s00464-020-08160-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08160-9