Abstract
Background
Flexible endoscopy allows use of the vessel–tissue sealer Ligasure™ (Covidien, Massachusetts, USA) to perform diverticulotomy. Few studies have used this endoscopic approach in the uncommon disorder Zenker's diverticulum. The aim of the present study was to evaluate the effectiveness and safety of flexible endoscopy treatment assisted by Ligasure™.
Methods
The single-center prospective and descriptive study included patients treated by flexible endoscopy using Ligasure™ for resection of Zenker’s diverticulum. Consecutive patients were included from March 2009 to April 2018. Patients were censored until the end of follow-up or death. Complications, symptoms before treatment, type of sedation, and number of interventions needed to resolve Zenker’s diverticulum were analyzed. Bleeding complications were considered when a case required a second endoscopy.
Results
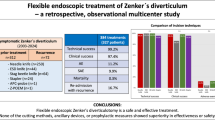
A total of 46 symptomatic patients with Zenker's diverticulum were included in the final analysis (41.3% women, median age of 73.7 ± 11 years). The median follow-up period was 37.21 ± 28 months. Of all cases, 58.7% were considered small (< 3 cm). Solid or semi-solid food-related dysphagia was present in 55.6% of patients previously to the procedure. The technique was successful in a single procedure in 78.3% of cases. However, the success rate increased to 89.1% with a second procedure, and we had a complication rate of 4.3% with this technique. Most patients (79.66%) were managed as out-patients or with short (< 24 h) admission.
Conclusion
In this large case series, treatment of Zenker's diverticulum based on flexible endoscopy assisted by Ligasure™ was a safe and effective procedure with a high success rate in a few endoscopy sessions and low complication rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Zenker’s diverticulum is an outpouching of tissue through a wall weakness situated between the thyropharyngeus muscle and the cricopharyngeal muscle, the region called Killian’s triangle. Zenker’s diverticulum occurs more commonly between 65 and 75 years of age. It is a rare disorder with an incidence of approximately 2/100,000 per year and a prevalence between 0.01 and 0.11% [1]. Dysphagia, caused by compression or incomplete opening of the upper esophageal sphincter, is the most common symptom. Other clinical manifestations include regurgitation, aspiration, presence of neck lump or malnutrition.
Treatment for Zenker’s diverticulum has changed over the years. Traditionally, open surgery approached diverticulum elimination through the excision (diverticulectomy), inversion, or suspension (diverticulopexy) [1]. However, open surgery has a high risk of severe complications, such as fistula formation or recurrent nerve paralysis [2], and requires a longer hospital stay than endoscopic treatment [3]. Thus, endoscopic myotomy began to develop as the best option for treatment [1]. The introduction of rigid endoscopy allowed diminution in adverse effects compared to open surgery.
However, some patients were not good candidates for a rigid procedure, and flexible endoscopy was introduced. This is a less invasive procedure, and patients with severe comorbidities were also candidates for the technique. For this procedure, the use of a diverticuloscope is advisable to protect the esophageal posterior wall, isolate the septum, and stabilize the instrument. A transparent hood can also be used with the same function [2].
This technique was described for the first time in 1995 in two independent studies [3, 4]. Different instruments and techniques have since been used to carry out the myotomy: needle knife, argon plasma coagulation, submucosal knife, harmonic scalpel, staple-assisted with endo-GIA™ (Medtronic, Minnesota, USA), or Ligasure™ (Covidien, Massachusetts, USA). Which technique is better is still unclear. No clinical trials have compared these alternatives, and any of them can be recommended over the other. The choice must be based on endoscopist experience and local resources [1, 2].
Flexible endoscopic myotomy assisted by Ligasure™ (forceps with double function, vessel–tissue sealer and cut, widely used in laparoscopic surgery) came into recent use. The first publications were in 2014, independently by two different authors [5, 6]. However, very little has been published about this endoscopic approach since then [5,6,7,8,9,10].
In this study, we evaluated the long-term outcomes of flexible endoscopy assisted by Ligasure™ myotomy in a large, single-center cohort of patients.
Materials and methods
Endoscopic technique
All procedures were performed by three expert endoscopists (C.S., M.A.S., and J.D.) using a standard video gastroscope (GIFQ 180 or 160Z, Olympus Optical Co., Tokyo, Japan) in a tertiary hospital. Before the procedure, patients received prophylactic antibiotic therapy.
The endoscopic technique consisted of introducing a flexible diverticuloscope (ZDO-22-30, Cook Endoscopy, Limerick, Ireland) over the gastroscope and placing each flap in the esophageal and diverticular lumen to expose the septum before performing the diverticulotomy. Diverticulotomy consists of a cricopharyngeal muscle myotomy using Ligasure™. The Ligasure™ was introduced through the diverticuloscope parallel to the gastroscope and situated in the middle of the septum (Fig. 1). After reaching this adequate position, Ligasure™ blades were opened and closed, catching the septum. Next, it was coagulated, sealed (pressing vessel–tissue sealer button), and finally cut in the middle to 3 mm from the bottom of the diverticulum. This procedure could be repeated if some muscle fibers remained uncut. The dissection was considered complete when muscle layer fibers were observed (Fig. 2). At the end of the procedure, one or two endoclips were placed at the base of the dissection to increase the cut length and prevent microperforation or bleeding (Fig. 3).
Population
Forty-six patients with Zenker’s diverticulum were prospectively and consecutively included from March 2009 to April 2018. Demographic data, symptoms before treatment, type of sedation, complications, length of hospital stay, and number of interventions needed were collected prospectively. The size and characteristics of the diverticulum were estimated endoscopically or radiographically previously to the procedure. We have defined a small diverticulum as < 3 cm and large diverticulum as ≥ 3 cm, similarly to the previous published manuscripts [11, 12]. Dysphagia was scored according to the Dakkak and Bennett scale [13].
The outcomes and side effects of the treatment were evaluated by follow-up visits. Patients were censored until the end of the follow-up period or death. Bleeding complications were considered when cases required a second endoscopy. Success has been defined as improvement in the patient’s symptoms, and achievement of residual diverticulum length less than 3 mm assessed among one or two endoscopic approaches.
The local Institutional Review Board approved data collection. Patient consent for data analysis was waived because individual patients were not identified.
Statistical analysis
Data were expressed as mean (± standard deviation) or percentage depending on the type of data. Correlations between categorical data were considered significant when p < 0.05. Statistical analysis was performed using SPSS software (version 22.0).
Results
A total of 46 patients were treated with flexible endoscopy assisted by Ligasure™ at our center. The mean age was 73.7 ± 11 years (Table 1) with a male predominance (n = 27 males, 58.7%). Preoperative symptoms were complete dysphagia in 6.7% (n = 3), dysphagia for liquid food in 35.6% (n = 16), dysphagia for semi-solid food in 20% (n = 9), and dysphagia for solid food in 35.6% (n = 16). One patient was treated without dysphagia (Fig. 4). The mean diverticulum size was 2.58 ± 1.16 cm. According to length, 58.7% (n = 27) were small diverticulum and 41.3% (n = 19) were large diverticulum. Patients were followed for 37.21 ± 28 months, and two patients were lost to follow-up.
Sedation was performed by the endoscopist in 95.7% (n = 44) of patients, and only two patients required an anesthesiologist. The success rate was 78.3% (n = 36) in a single endoscopic session, and 10 patients required at least one more session. Success rate increased to 89.1% (41 patients) after a second endoscopic approach (Fig. 5). Only 2 patients (4.3%) developed complications: one case of significant bleeding (with need for endoscopic therapy), and one case of significant desaturation related to sedation. Of all procedures (n = 64), 79.66% (n = 47) were managed as out-patients or with a short (< 24 h) admission. In six endoscopies, the patient was re-admitted because of other reasons not related to the technique.
No significant differences in complication rates were observed based on gender (p = 0.339), number of interventions (p = 0.45), or diverticulum size (p = 0.54). No significant differences were found between number of interventions according to diverticula size (p = 0.94) or symptoms (p = 0.17).
Discussion
Treatment of Zenker’s diverticulum has evolved from open surgery to a less invasive approach based on flexible endoscopy. Flexible endoscopy can be carried out in most patients, especially those with poor neck extension or jaw retraction in whom the use of a rigid endoscope is not possible. Also this technique is less invasive and can be performed in comorbid or elderly patients who are not candidates for open surgery [2]. This procedure can be performed without general anesthesia, reducing anesthetic risk and complication rates [14].
For the flexible endoscopy approach, we use a soft diverticuloscope because it provides better exposure of the septum and a more stable position, resulting in fewer adverse events [15].
Diverticulotomy and cricopharyngeal myotomy are the keys to treatment of Zenker's diverticulum and can be achieved by different tools, such as the Zimmon needle (Cook endoscopy, Winston-Salem, NC), argon plasma coagulation, needle knife, submucosal dissection knives, hook knife, or endoscopic forceps. However, which technique is better is still unclear.
Many studies have demonstrated the success and complication rates with different tools. The success rate and complication rate for the Zimmon needle are 84% and 2.2%, respectively [16]. The needle knife approach was evaluated in a recent meta-analysis and had a high success rate of 88% and low complication rate of 13% that decreased to 10% when a diverticuloscope was used [17]. Submucosal dissection knives, which include Dual-knife (Olympus endotherapy, Tokyo, Japan) and the HybridKnife (Erbe elektromedizin GmbH, Tuebingen, Germany), were evaluated by Laquière et al. with a success rate and complication rate of 92.3% and 0%, respectively [18]. Rouquette et al. analyzed myotomy assisted by hook knife, with a success rate of 91.7% and complication rate of 7.1%, similar to other studies [19]. Using stag beetle knife (Sumimoto Bakelite, Tokyo, Japan), Goelder et al. had a success rate of 90.4% in one treatment session [20]. No clinical trials have been designed to compare different alternatives, as this is difficult because Zenker’s diverticulum is an uncommon disorder with few affected patients.
In our study, the success rate was high with few endoscopic sessions. 78.3% in the first session and 89.1% with a second session. Overall and individual success rates were evaluated, based on dysphagia symptoms and residual diverticulum wall after one or two endoscopic sessions. We consider success as an improvement in dysphagia symptoms and a residual diverticulum wall length less than 3 mm. We adopted a conservative attitude during the first cricopharyngeal muscle myotomy in order to prevent oesophagus damage. Probably it could be the main factor for the persisting symptoms after the first procedure in a small percentage of patients and the need for a second endoscopic approach. We have a long-term follow-up period of 37 months approximately.
Complication rate is low (4.3%). Only two patients experienced an adverse event. We did not observe any perforation or severe complications. The complication rate in our study was lower than previously described in a review involving flexible endoscopic techniques [21]. Significant bleeding was detected in 2.2%, compared to 6.6% in this review. Bleeding was treated by placing endoclips after finding the bleeding source. Perforation could be prevented using the diverticuloscope and endoclips at the end of the procedure [16]. We also think that the vessel–tissue sealer function of Ligasure™ could protect from perforation.
Most patients can be managed as out-patients or with a short admission less than 24 h using this technique (79.66%), which permits the patient early feeding and reduces the risk of long hospitalization (malnutrition, morbidity, or nosocomial infection), especially in elderly people.
Very little has been published about flexible endoscopy diverticulotomy and cricopharyngeal myotomy assisted by Ligasure™. Many case series in the literature have had smaller sample sizes and shorter follow-up period compared to our study [6, 7, 9, 10, 22]. Globally, Yuan et al. [14] analyzed available data for endoscopic treatment (with a lot of heterogeneity), showing a success rate of 63–100%. Recently, Díez-Redondo et al. [8] published a similar study using Ligasure™ with a clinical success rate of 96.7% and 84% asymptomatic patients at 34.6 months of follow-up. Nielsen et al. described a resolution of symptoms in 93% of patients [6].
No significant differences have been found between complication rates according to diverticulum length or the number of re-interventions needed. Similarly, we did not find differences between the need for re-intervention and diverticulum length or symptoms, which suggests that the effectiveness of the technique is independent from other diverticulum characteristics. Treatment success has correlated with the length of the septotomy and the size of Zenker’s diverticulum in other studies [23]. These differences could be explained by our smaller sample, because some authors described some differences in relapse depending on the size of the diverticulum [11].
Limitations of our study are a lack of comparison with another flexible endoscopy approach and the low patient number, which were too few to draw robust conclusions. However, this is similar to other articles. The strengths of our study are the large sample size relative to this uncommon disorder, the long follow-up period, and the prospective and consecutive data collection.
In conclusion, treatment of Zenker’s diverticulum based on flexible endoscopy assisted by Ligasure™ is an effective and safe procedure with a high success rate over a few endoscopy sessions and low complication rate. This procedure can be recommended as a solid alternative to endoscopic treatment of Zenker’s diverticulum.
References
Dzeletovic I, Ekbom DC, Baron TH (2012) Flexible endoscopic and surgical management of Zenker's diverticulum. Expert Rev GastroenterolHepatol 6:449–465
Law R, Katzka DA, Baron TH (2014) Zenker's diverticulum. ClinGastroenterolHepatol 12:1773–1782
Verdonck J, Morton RP (2015) Systematic review on treatment of Zenker's diverticulum. Eur Arch Otorhinolaryngol 272:3095–3107
Ishioka S, Sakai P, MalufFilho F, Melo JM (1995) Endoscopic incision of Zenker's diverticula. Endoscopy 27:433–437
Mulder CJ, den Hartog G, Robijn RJ, Thies JE (1995) Flexible endoscopic treatment of Zenker's diverticulum: a new approach. Endoscopy 27:438–442
Nielsen HU, Trolle W, Rubek N, Homoe P (2014) New technique using LigaSure for endoscopic mucomyotomy of Zenker's diverticulum: diverticulotomy made easier. Laryngoscope 124:2039–2042
Andersen MF, Trolle W, Anthonsen K, Nielsen HU, Homoe P (2017) Long-term results using LigaSure 5 mm instrument for treatment of Zenker's diverticulum. Eur Arch Otorhinolaryngol 274:1939–1944
Diez Redondo P, Nunez Rodriguez H, de Benito SM, Torres Yuste R, Perez-Miranda M (2019) Endoscopic treatment of Zenker's diverticulum with Ligasure: simple, safe and effective. EndoscInt Open 7:E203–E208
Gonzalez N, Viola M, Costa X, Gamba A (2014) Endoscopictreatment of Zenker's diverticulumbyLigaSurescalpel. Endoscopy 46(Suppl 1):E229–E230
Moreira da Silva BA, Germade A, Perez Citores L, Maestro Antolin S, Santos F, Sanchez Barranco F, Perez Millan A, IgeaArisqueta F (2017) Endoscopic diverticulotomy using Ligasure. GastroenterolHepatol 40:80–84
Ishaq S, Sultan H, Siau K, Kuwai T, Mulder CJ, Neumann H (2018) New and emerging techniques for endoscopic treatment of Zenker's diverticulum: state-of-the-art review. Dig Endosc 30:449–460
Mazza M, Bergamini AN, Parise P, Cossu A, Adamenko O, Elmore U, Rosati R (2017) Treatment of Zenker's diverticulum with endoscopic stapled esophago-divertisculostomy (ESD): analysis of long-term outcome. SurgLaparoscEndoscPercutan Tech 27:445–448
Dakkak M, Bennett JR (1992) A new dysphagia score with objective validation. J ClinGastroenterol 14:99–100
Yuan Y, Zhao YF, Hu Y, Chen LQ (2013) Surgical treatment of Zenker's diverticulum. Dig Surg 30:207–218
Costamagna G, Iacopini F, Tringali A, Marchese M, Spada C, Familiari P, Mutignani M, Bella A (2007) Flexible endoscopic Zenker's diverticulotomy: cap-assisted technique vs. diverticuloscope-assisted technique. Endoscopy 39:146–152
Huberty V, El Bacha S, Blero D, Le Moine O, Hassid S, Deviere J (2013) Endoscopic treatment for Zenker's diverticulum: long-term results (with video). GastrointestEndosc 77:701–707
Li LY, Yang YT, Qu CM, Liang SW, Zhong CQ, Wang XY, Chen Y, Spandorfer RM, Christofaro S, Cai Q (2018) Endoscopic needle-knife treatment for symptomatic esophageal Zenker's diverticulum: a meta-analysis and systematic review. J Dig Dis 19:204–214
Laquiere A, Grandval P, Arpurt JP, Boulant J, Belon S, Aboukheir S, Laugier R, Penaranda G, Curel L, Boustiere C (2015) Interest of submucosal dissection knife for endoscopic treatment of Zenker's diverticulum. SurgEndosc 29:2802–2810
Rouquette O, Abergel A, Mulliez A, Poincloux L (2017) Usefulness of the Hook knife in flexible endoscopic myotomy for Zenker's diverticulum. World J GastrointestEndosc 9:411–416
Goelder SK, Brueckner J, Messmann H (2016) Endoscopic treatment of Zenker's diverticulum with the stag beetle knife (sb knife)—feasibility and follow-up. Scand J Gastroenterol 51:1155–1158
Ishaq S, Hassan C, Antonello A, Tanner K, Bellisario C, Battaglia G, Anderloni A, Correale L, Sharma P, Baron TH, Repici A (2016) Flexible endoscopic treatment for Zenker's diverticulum: a systematic review and meta-analysis. GastrointestEndosc 83(1076–1089):e1075
Noguera-Aguilar J, Dolz-Abadia C, Vilella A, Munoz-Perez JM, Canaval-Zuleta HJ, Salvatierra-Arrieta L (2014) Transoralendoluminal approach to Zenker's diverticulum using Ligasure. Early clinical experience. Rev EspEnferm Dig 106:137–141
Costamagna G, Iacopini F, Bizzotto A, Familiari P, Tringali A, Perri V, Bella A (2016) Prognostic variables for the clinical success of flexible endoscopic septotomy of Zenker's diverticulum. GastrointestEndosc 83:765–773
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Enrique Alfaro, Pablo Cañamares, Carlos Sostres, Miguel Ángel Simón, and Julio Ducons have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alfaro, E., Cañamares, P., Sostres, C. et al. Flexible endoscopy assisted by Ligasure™ for treatment of Zenker’s diverticulum: an effective and safe procedure. Surg Endosc 35, 5124–5129 (2021). https://doi.org/10.1007/s00464-020-08001-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08001-9