Abstract
Background
Laparoscopic Nissen fundoplication (LNF) and gastrostomy tube (GT) placement may be performed concomitantly in children with gastro-esophageal reflux disease (GERD) and failure to thrive. We aimed to evaluate the rate and risk factors for LNF failure in children undergoing concomitant LNF/GT.
Methods
A retrospective multi-institutional cohort study was conducted, reviewing patients that underwent LNF (2005–2014). Data collected included patient demographics, comorbidities, and type of GT (laparoscopy- or endoscopy-assisted). The primary outcome measure was LNF failure. Data was compared using contingency tables or Mann–Whitney tests, when appropriate. An exploratory analysis by Kaplan–Meier survival and Cox proportional hazards analysis was performed to determine predictors of time to LNF failure after LNF/GT.
Results
Of 189 children that underwent LNF, 99 (52%) had a concomitant GT (55% laparoscopy-, 45% endoscopy-assisted). LNF failed in 15% after LNF/GT and in 17% after LNF alone (p = 0.84), at a median age of 23 months (IQR 8–41). Using univariate analysis, we found that a younger age at the time of surgery (p = 0.05), prematurity (p = 0.0018), esophageal atresia (p = 0.01), and endoscopy-assisted GT (p = 0.02) were potential predictors of LNF failure after LNF/GT. After multivariate regression analysis, prematurity (p = 0.007) remained significantly associated with LNF failure after LNF/GT. No predictive factors for LNF failure after LNF alone were identified.
Conclusions
Concomitant GT insertion and LNF is a common practice, as half of the children that undergo LNF also received GT insertion. Children born preterm or with esophageal atresia comprise a fragile population at high-risk of LNF failure after LNF/GT. Prospective, multicentric studies are needed to evaluate the best GT technique to use in children undergoing LNF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastro-esophageal reflux disease (GERD) is a common condition, that affects 4–10% of the pediatric population [1,2,3]. Although the first-line treatment is medical with the use of proton-pump inhibitors, surgery can be considered when GERD symptoms fail to respond to pharmacological therapy. Laparoscopic Nissen fundoplication (LNF) has been established as a safe and effective alternative to the open approach and has become the most common anti-reflux procedure for GERD in children over 1 year of age [4, 5].
In children with swallowing difficulties and failure to thrive, it has been widely accepted that a concomitant gastrostomy tube (GT) placement can be considered [6,7,8]. In fact, a recent study reported that 94% of the children under 2 years of age that undergo LNF also had a GT placement during the same surgical procedure (LNF/GT) [9]. However, several recent studies have shown that concomitant fundoplication increases the rates of GT complications compared to GT inserted without a fundoplication [10,11,12]. Moreover, the need for a gastrostomy in children undergoing Nissen fundoplication has been recently associated with a higher risk of mortality in the first year after fundoplication [13]. However, to the best of our knowledge, no study has ever investigated LNF failure and GERD recurrence after concomitant LNF and GT placement. Moreover, various technical approaches exist for GT placement, such as laparoscopy- or endoscopy-assisted techniques, and the best option remains controversial in the pediatric population [14,15,16,17,18], and poorly studied in the context of a concomitant fundoplication.
Herein, we aimed to determine the rate of LNF failure, focusing on children undergoing concomitant LNF/GT placement for GERD and investigate risk factors for LNF failure after this procedure.
Material and methods
Patient selection and data collection
A retrospective and multi-institutional cohort study was conducted in two departments of pediatric surgery (Robert-Debré Hospital and Angers Hospital, France). Medical records of all children that underwent LNF for GERD from January 2005 to January 2014 were reviewed. We excluded from the analysis patients that underwent LNF as a redo-surgery with an initial LNF performed before January 2005. The study protocol was approved by the Institutional Review Board of Robert Debré Hospital affiliated to Paris University.
Data collected included demographics, such as gestational age at birth, gender, age and weight at surgery, and the presence of associated comorbidities such as neurological impairment, esophageal atresia, and congenital diaphragmatic hernia. Prematurity was defined as a gestational age at birth under 37 weeks of gestation.
All children that underwent LNF had symptomatic GERD unresponsive to medical treatment. Preoperative work-up included upper gastro-intestinal contrast series, endoscopy, and/or pH-metering.
We focused on patients who underwent concomitant GT placement during the same surgical intervention as the LNF. Regarding gastrostomy placement, indication and technique for this procedure were collected. Several conditions led to the indication of a GT insertion: inability to feed due to vomiting or neurologic impairment, oesophageal dysmotility, or failure to thrive due to other conditions, such as cardiac and respiratory comorbidities. In our institutions, three techniques of gastrostomy placement were used: laparoscopy-assisted or endoscopy-assisted (either with a “pull” or a “push” technique).
Operative techniques
Laparoscopic Nissen fundoplication
The laparoscopic technique consisted in using a trans-ombilical 30° optical port, as well as two operative ports placed in the right and the left flank on the mid-clavicular line. An additional port was placed in the right upper quadrant to lift the liver and expose the hiatal area. Without performing any hiatal dissection or short gastric vessels section, a complete Nissen wrap was performed. The crural opening posterior to the esophagus was closed using non-absorbable sutures.
Laparoscopy-assisted gastrostomy
The laparoscopy-assisted technique was a modified Stamm gastrostomy procedure [7, 19]. At the end of the LNF, a 3–0 non-absorbable multifilament suspension suture was inserted under laparoscopic control on the anterior gastric wall, to fix the stomach to the abdominal wall. The stomach was then grasped along the greater curvature and exteriorized through a left-upper quadrant trocar. After placement of a 3–0 non-absorbable multifilament purse-string suture on the anterior gastric wall under laparoscopic control, the gastrostomy was then performed either with fine scissors or cautery under direct vision inside the purse-string suture. Once the stomach was secured against the abdominal wall, the GT or button was then inserted. Finally, the suspension suture is exteriorized and ligated on the abdominal wall.
Endoscopy-assisted gastrostomy
At the end of the LNF procedure, the pneumoperitoneum was exsufflated and a gastroscope was introduced through the patient’s mouth into the stomach, in order to help identifying a suitable location for the GT.
In the “pull” technique, the stomach was punctured percutaneously, and a pull suture was introduced into the stomach cavity through the conducting needle. The suture was then grasped with an endoscopic biopsy forceps, and pulled out through the esophagus and the mouth, as described by Gauderer et al. [20]. The gastrostomy tube was then fixed to the suture and pulled in through the mouth and esophagus, into the stomach and eventually externalized through the abdominal wall. The tip of the catheter was maintained in the stomach by a retention disk.
In the “push” technique, the MIC-KEY Introducer Kit (Kimberly-Clark Corp, Roswell, GA, United States) was used according to the manufacturer’s procedure as previously described by Göthberg and Björnsson [21]. The stomach was first punctured under endoscopic control with 3 T-fasteners with resorbable sutures. Gastropexy was carried out by traction on these three sutures, that were fastened with accompanying external suture locks. A needle was then used to puncture the stomach between the anchors, followed by the insertion of a guide wire through this needle into the stomach. The orifice was then dilated using a conus-like dilator surrounded by a plastic shaft. After removing the guide wire and the dilator, a balloon gastrostomy catheter was inserted through the plastic shaft. Subsequently, the GT balloon was filled with water, the plastic shaft was peeled off, and the catheter was pulled against the abdominal wall.
Primary outcome
The primary outcome of this study was LNF failure. We defined failure as vomiting or other clinical signs of GERD, endoscopic and/or radiological signs of relapse of GERD after LNF. When required, redo LNF was performed using the same initial technique. Children were followed up by the pediatric surgeon at 1, 3, and 12 months after fundoplication. No explorations were systematically carried out if the child was asymptomatic and subsequent follow-up was performed by a pediatrician.
Statistical analysis
The results of the descriptive analysis were expressed as numbers and percentages for qualitative variables and as median and interquartile range (IQR) for quantitative variables. Comparison was carried out regarding the outcome of LNF. Chi-square test or Fisher’s exact test for qualitative variable and Student’s t-test or Mann–Whitney’s test for quantitative variables were used, when appropriate. Statistical significance was assigned to p < 0.05.
All variables with a p-value < 0.20 on univariate analysis were assessed for a possible association with LNF failure using a multivariate Cox regression (Stata 12.1; StataCorp, College Station, TX, USA). Kaplan–Meier survival analysis was used to determine predictors of time to LNF failure.
Results
Patient characteristics
During our study period, 189 children underwent LNF at our institutions. A concomitant gastrostomy tube insertion was carried out in 52% (n = 99) of these children (Fig. 1).
Compared to patients that underwent LNF alone, children that underwent LNF/GT were younger (17 vs 47 months, p = 0.0011), with a lower weight at surgery (8.2 vs 12.5 kg, p = 0.0001) (Table 1). Moreover, there was a higher proportion of neurologically impaired children in the LNF/GT group compared to LNF alone (65% vs 43%, p = 0.0036). On the other hand, there was a higher proportion of children born with esophageal atresia in the LNF alone group compared to the LNF/GT group (13% vs 4%, p = 0.03). Other comorbidities included prematurity (n = 29, 15%), and congenital diaphragmatic hernia (n = 4, 2%). Children undergoing LNF alone were more likely to have none of these four comorbidities than children undergoing LNF/GT (38% vs 22%, p = 0.03). Overall, 37 children (20%) weighed less than 6 kg at the time of the surgery.
All Nissen fundoplications were performed laparoscopically, without any conversions. Regarding the 99 children that underwent LNF/GT, a laparoscopy-assisted approach was used for GT insertion in 55% of cases. In the remaining 45% (n = 45), an endoscopy-assisted GT insertion was performed. Of the latter, the majority (82%) was placed using the “pull” technique, whereas the “push” technique was used in only 18% of the cases.
The median duration of follow-up was 46 months (IQR 27–68 months) after LNF/GT and 44 months (IQR 23–81 months) after LNF alone (p = 0.67).
Fundoplication failure
The overall rate of fundoplication failure was 16% (n = 30/189), with a median time to failure of 23 months (IQR 8–41 months). There was no difference between patients that underwent LNF/GT and those that underwent LNF alone in terms of failure rate (15% vs 17%, p = 0.84) or time to failure (20 vs 23 months, p = 0.34).
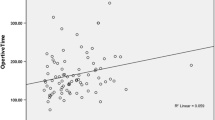
Regarding patients that underwent LNF/GT, 15% presented with LNF failure, with a median time to failure of 20 months (IQR 6–26 months). On Kaplan–Meier survival analysis, 77.4% of patients had success of LNF by 5 years (Fig. 2). After LNF failure, 40% (n = 6) underwent a redo-surgery, at a median time of 26 months after the initial surgery (IQR 7–64 months). The remaining 9 children did not undergo a second intervention, either because the symptoms were considered mild (n = 4, 45%), the children were assessed as having a high surgical risk (n = 4, 45%) or died before a redo-surgery could be performed (n = 1, 11%).
Kaplan–Meier estimates of patients remaining symptom-free of GERD after LNF/GT. A Kaplan–Meier showing time to symptom from LNF, censored at time of symptom or last follow-up. Median (IQR) symptom-free of GERD after LNF/GT: 20 months (6–26). B Kaplan–Meier showing time to symptom from LNF based on history of prematurity, censored at time of symptom or last follow-up. Log-rank p < 0.05. C Kaplan–Meier showing time to symptom from LNF based on endoscopic procedure for gastrostomy insertion, censored at time of symptom or last follow-up. Log-rank p < 0.05
Regarding patients that underwent LNF alone, 17% presented with LNF failure, with a median time to failure of 23 months (IQR = 18–45 months). Only three patients underwent redo-surgery (20%), at a median time of 24 months after the initial surgery (IQR 10–39 months).
After redo-surgery (n = 9), none of children presented with GERD recurrence, after a median follow-up of 47 months after redo-surgery (IQR 14–56 months).
Risk factors for LNF failure after LNF-GT
Using univariate comparison (Table 2), we found that a younger age at the time of surgery (p = 0.05), prematurity (p = 0.0018), esophageal atresia (p = 0.01), and an endoscopy-assisted GT insertion (p = 0.02) were potential predictors of LNF failure.
LNF failure occurred in 57% of children born prematurely (vs. 8% of children born at term, p = 0.0018) and 75% of children born with esophageal atresia (vs. 13% of children born without esophageal atresia, p = 0.01).
The risk of LNF failure was significantly higher after endoscopy-assisted GT insertion (24%) than after surgical placement (7%, p = 0.02). Both endoscopy-assisted techniques had similar LNF failure rates (38% for “push” technique vs. 22% for “pull”-technique, p = 0.4).
After multivariate logistical regression analysis and a stepwise selection of variables (Table 3), only prematurity remained independently associated with LNF failure. The likelihood of being symptom-free from GERD at 5 years after surgery is displayed in Fig. 2 for the entire cohort of children undergoing LNF/GT and in the setting of prematurity or endoscopy-assisted gastrostomy.
Risk factors for LNF failure after LNF alone
Using univariate comparison, none of the factors studied were predictive of LNF failure in children undergoing LNF alone (Table 4).
Discussion
Our study demonstrated that more than half of the children that undergo LNF in our institutions also receive a GT placement during the same surgery. Overall, 15% of children that undergo concomitant LNF/GT will suffer from GERD recurrence, or LNF failure. Moreover, we found that prematurity was independently associated with LNF failure in children that underwent concomitant LNF/GT.
In our cohort, 52% of the children that underwent laparoscopic Nissen fundoplication had a gastrostomy tube placement during the same procedure, similar to the rate reported by Hernandez et al. of 40% [22]. To the best of our knowledge, no study has focused on the long-term results of this combined surgery. Moreover, the concomitant indication for a LNF and GT usually implies underlying comorbidities, comprising a distinct and fragile population compared to patients undergoing LNF alone [6]. In our cohort, 78% of the children undergoing LNF/GT had at least one major comorbidity (prematurity, neurological impairment, esophageal atresia, or congenital diaphragmatic hernia). Optimizing surgical procedures for these fragile patients is crucial in order to avoid unnecessary procedures and redo surgeries.
We found an overall rate of 15% of LNF failure after LNF/GT, similar to rates that have been previously reported for LNF, between 5 and 15%, and the 17% rate of failure after LNF alone in our cohort [22,23,24]. However, after univariate and multivariate analysis, we found several risk factors potentially predictive of LNF failure after LNF/GT. Although a younger age or low weight at surgery has previously been reported as a risk factor for LNF failure [23], we found for the first time that prematurity is predictive of LNF failure after LNF/GT. This could be due to the multifactorial etiology of GERD in preterm infants, and the persistence of pro-GERD factors, such as chronic lung disease.
In our cohort, 75% of the children born with esophageal atresia and undergoing LNF/GT presented with GERD recurrence. This is in accordance with previous studies, that have consistently reported high failure rates of fundoplication in children born with esophageal atresia [22, 24, 25]. This is believed to be due to persistent anatomic anomalies and functional disturbances of the repaired esophagus that differ considerably from a normal esophagus, and may not be as responsive to fundoplication. The insertion of a GT at the time of LNF may result in additional strain to the wrap, predisposing to LNF failure. In our study, esophageal atresia was significantly associated with LNF failure upon univariate analysis but was not an independent predictive factor of LNF failure after multivariate logistical regression analysis, despite an odds ratio of 10. This can be explained by the fact that patients with esophageal atresia represent less than 5% of our cohort.
Interestingly, although the majority of our cohort undergoing LNF/GT were neurologically impaired, this comorbidity was not found to be predictive of LNF failure, suggesting that concomitant LNF/GT is a safe option in children with neurological impairment and GERD.
At univariate analysis, we found higher rates of LNF failure after endoscopy-assisted GT insertion techniques (24%) compared to laparoscopically-assisted GT (7%, p = 0.02). However, after multivariate logistical regression analysis, endoscopic GT insertion was no longer associated with LNF failure. Determining the best technique for GT placement remains controversial in children. Several studies have found that laparoscopy-assisted gastrostomy results in less gastrostomy-related complications than endoscopic techniques in children [14,15,16,17,18]. Laparoscopy is considered as an effective tool to avoid complications related to GT positioning, that occur in partly due to the blind placement technique that is conventionally used, resulting in a suboptimal fixation of the stomach to the abdominal wall. Moreover, compared to open and endoscopy-assisted GT placement, the laparoscopic approach has been associated with a lower need for subsequent fundoplication after GT [26]. Finally, the introduction of the endoscope and the insufflation of air to expand the stomach immediately after the wrap has been performed could cause an over-stretching of the wrap, resulting in LNF failure. Despite the frequent association of a concomitant LNF/GT, no guidelines have been established on the technique to use when performing a gastrostomy during the same procedure as LNF and prospective, randomized and multicentric studies should be performed in order to investigate the best GT technique to be used.
Surprisingly, after conducting a univariate analysis in children undergoing LNF alone, we could not identify any risk factors predictive of LNF failure. In particular, none of the comorbidities identified as potentially predictive of failure after LNF/GT, such as young age at surgery, prematurity, and esophageal atresia, were associated with failure after LNF alone. Although the design of this study does not allow us to demonstrate the superiority of one technique over another, performing LNF without a GT may be a safer option in children with these comorbidities.
We acknowledge that this study has limitations, related to its retrospective design. We could not accurately evaluate the impact of the different GT techniques on LNF failure, as the populations varied strongly in terms of gestational age, weight and age at surgery, rendering the different populations not comparable.
Conclusions
Our study showed that concomitant GT insertion and LNF is a common practice, as almost half of the children that undergo LNF also receive a GT during the same procedure. Children born prematurely or with esophageal atresia comprise a fragile population at high-risk of LNF failure after LNF/GT. Prospective, multicentric studies are needed to evaluate the best GT technique to use in children undergoing LNF.
References
Martigne L, Delaage P-H, Thomas-Delecourt F, Bonnelye G, Barthélémy P, Gottrand F (2012) Prevalence and management of gastroesophageal reflux disease in children and adolescents: a nationwide cross-sectional observational study. Eur J Pediatr 171:1767–1773. https://doi.org/10.1007/s00431-012-1807-4
Okimoto E, Ishimura N, Morito Y, Mikami H, Shimura S, Uno G, Tamagawa Y, Aimi M, Oshima N, Kawashima K, Kazumori H, Sato S, Ishihara S, Kinoshita Y (2015) Prevalence of gastroesophageal reflux disease in children, adults, and elderly in the same community. J Gastroenterol Hepatol 30:1140–1146. https://doi.org/10.1111/jgh.12899
Singendonk M, Goudswaard E, Langendam M, van Wijk M, van Etten-Jamaludin F, Benninga M, Tabbers M (2019) Prevalence of gastroesophageal reflux disease symptoms in infants and children: a systematic review. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000002280
Fox D, Morrato E, Campagna EJ, Rees DI, Dickinson LM, Partrick DA, Kempe A (2011) Outcomes of laparoscopic versus open fundoplication in children’s hospitals: 2005–2008. Pediatrics 127:872–880. https://doi.org/10.1542/peds.2010-1198
Ru W, Wu P, Feng S, Lai X-H, Chen G (2016) Laparoscopic versus open Nissen fundoplication in children: a systematic review and meta-analysis. J Pediatr Surg 51:1731–1736. https://doi.org/10.1016/j.jpedsurg.2016.07.012
Stringel G, Delgado M, Guertin L, Cook JD, Maravilla A, Worthen H (1989) Gastrostomy and Nissen fundoplication in neurologically impaired children. J Pediatr Surg 24:1044–1048
Sampson LK, Georgeson KE, Winters DC (1996) Laparoscopic gastrostomy as an adjunctive procedure to laparoscopic fundoplication in children. Surg Endosc 10:1106–1110
Thatch KA, Yoo EY, Arthur LG, Finck C, Katz D, Moront M, Prasad R, Vinocur C, Schwartz MZ (2010) A comparison of laparoscopic and open Nissen fundoplication and gastrostomy placement in the neonatal intensive care unit population. J Pediatr Surg 45:346–349. https://doi.org/10.1016/j.jpedsurg.2009.10.073
Rosales A, Whitehouse J, Laituri C, Herbello G, Long J (2018) Outcomes of laparoscopic nissen fundoplications in children younger than 2-years: single institution experience. Pediatr Surg Int 34:749–754. https://doi.org/10.1007/s00383-018-4281-x
Berman L, Sharif I, Rothstein D, Hossain J, Vinocur C (2015) Concomitant fundoplication increases morbidity of gastrostomy tube placement. J Pediatr Surg 50:1104–1108. https://doi.org/10.1016/j.jpedsurg.2014.07.013
Thomas C, Forrest A, Klingberg H, Moore D, Abu-Assi R, Barry SC, Khurana S (2016) Does gastrostomy placement with concurrent fundoplication increase the risk of gastrostomy-related complications? J Pediatr Gastroenterol Nutr 63:29–33. https://doi.org/10.1097/MPG.0000000000001063
Yap BKY, Nah SA, Chen Y, Low Y (2017) Fundoplication with gastrostomy vs gastrostomy alone: a systematic review and meta-analysis of outcomes and complications. Pediatr Surg Int 33:217–228. https://doi.org/10.1007/s00383-016-4028-5
Milford K, Numanoglu A, Sultan TA, Klopper J, Cox S (2019) Predictors of multiple readmissions or death in the first year after Nissen fundoplication in children. Pediatr Surg Int 35:501–507. https://doi.org/10.1007/s00383-018-04429-2
Merli L, De Marco EA, Fedele C, Mason EJ, Taddei A, Paradiso FV, Catania VD, Nanni L (2016) Gastrostomy placement in children: percutaneous endoscopic gastrostomy or laparoscopic gastrostomy? Surg Laparosc Endosc Percutan Tech 26:381–384. https://doi.org/10.1097/SLE.0000000000000310
Petrosyan M, Khalafallah AM, Franklin AL, Doan T, Kane TD (2016) Laparoscopic gastrostomy is superior to percutaneous endoscopic gastrostomy tube placement in children less than 5 years of age. J Laparoendosc Adv Surg Tech A 26:570–573. https://doi.org/10.1089/lap.2016.0099
McSweeney ME, Smithers CJ (2016) Advances in pediatric gastrostomy placement. Gastrointest Endosc Clin N Am 26:169–185. https://doi.org/10.1016/j.giec.2015.09.001
Kim J, Lee M, Kim SC, Joo CU, Kim SJ (2017) Comparison of percutaneous endoscopic gastrostomy and surgical gastrostomy in severely handicapped children. Pediatr Gastroenterol Hepatol Nutr 20:27–33. https://doi.org/10.5223/pghn.2017.20.1.27
Sandberg F, Viktorsdóttir MB, Salö M, Stenström P, Arnbjörnsson E (2018) Comparison of major complications in children after laparoscopy-assisted gastrostomy and percutaneous endoscopic gastrostomy placement: a meta-analysis. Pediatr Surg Int 34:1321–1327. https://doi.org/10.1007/s00383-018-4358-6
Reiner DS, Leitman IM, Ward RJ (1991) Laparoscopic Stamm gastrostomy with gastropexy. Surg Laparosc Endosc 1:189–192
Ponsky JL, Gauderer MW (1981) Percutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy. Gastrointest Endosc 27:9–11
Göthberg G, Björnsson S (2016) One-step insertion of low-profile gastrostomy in pediatric patients vs pull percutaneous endoscopic gastrostomy: retrospective analysis of outcomes. JPEN J Parenter Enteral Nutr 40:423–430. https://doi.org/10.1177/0148607114567202
Lopez-Fernandez S, Hernandez F, Hernandez-Martin S, Dominguez E, Ortiz R, De La Torre C, Martinez L, Tovar JA (2014) Failed Nissen fundoplication in children: causes and management. Eur J Pediatr Surg 24:79–82. https://doi.org/10.1055/s-0033-1351664
Rothenberg SS (2013) Two decades of experience with laparoscopic nissen fundoplication in infants and children: a critical evaluation of indications, technique, and results. J Laparoendosc Adv Surg Tech A 23:791–794. https://doi.org/10.1089/lap.2013.0299
Koivusalo AI, Pakarinen MP (2018) Outcome of surgery for pediatric gastroesophageal reflux: clinical and endoscopic follow-up after 300 fundoplications in 279 consecutive patients. Scand J Surg 107:68–75. https://doi.org/10.1177/1457496917698641
Tovar JA, Fragoso AC (2013) Gastroesophageal reflux after repair of esophageal atresia. Eur J Pediatr Surg 23:175–181. https://doi.org/10.1055/s-0033-1347911
Ponsky TA, Gasior AC, Parry J, Sharp SW, Boulanger S, Parry R, Ostlie DJ, St Peter SD (2013) Need for subsequent fundoplication after gastrostomy based on patient characteristics. J Surg Res 179:1–4. https://doi.org/10.1016/j.jss.2012.03.064
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Louise Montalva, Aurora Mariani, Françoise Schmitt, Cécile O. Muller, Jérôme Viala, Alexis Mosca, Matthieu Peycelon, and Arnaud Bonnard have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Montalva, L., Mariani, A., Schmitt, F. et al. Concomitant gastrostomy tube insertion during laparoscopic Nissen fundoplication for gastro-esophageal reflux disease: analysis of risk factors for fundoplication failure. Surg Endosc 35, 4251–4258 (2021). https://doi.org/10.1007/s00464-020-07913-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07913-w