Abstract
Background
Effective hemostasis is essential to prevent rebleeding. We evaluated the efficacy and feasibility of the Over-The-Scope Clip (OTSC) system compared to combined therapy (through-the-scope clips with epinephrine injection) as a first-line endoscopic treatment for high-risk bleeding peptic ulcers.
Methods
We retrospectively analyzed data of 95 patients from a single, tertiary center and underwent either OTSC (n = 46) or combined therapy (n = 49). The primary outcome of the present study was the efficacy of the OTSC system as a first-line therapy in patients with high-risk bleeding peptic ulcers compared to combined therapy with TTS clips and epinephrine injection. The secondary outcomes included the rebleeding rate, perforation rate, mean procedure time, reintervention rate, mean procedure cost and days of hospitalization in the two study groups within 30 days of the index procedure.
Results
All patients achieved hemostasis within the procedure; two patients in the OTSC group and four patients in the combined therapy group developed rebleeding (p = 0.444). No patients experienced gastrointestinal perforation. OTSC had a shorter median procedure time than combined therapy (11 min versus 20 min; p < 0.001). The procedure cost was superior for OTSC compared to combined therapy ($102,000 versus $101,000; p < 0.001). We found no significant difference in the rebleeding prevention rate (95.6% versus 91.8%, p = 0.678), hospitalization days (3 days versus 4 days; p = 0.215), and hospitalization costs ($108,000 versus $240,000, p = 0.215) of the OTSC group compared to the combined therapy group.
Conclusion
OTSC treatment is an effective and feasible first-line therapy for high-risk bleeding peptic ulcers. OTSC confers comparable costs and patient outcomes as combined treatments, with a shorter procedure time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over recent years, advances in endoscopic and pharmacological therapies have reduced the continued and recurrent bleeding rates in upper gastrointestinal bleeding [1]. Nevertheless, nonvariceal upper gastrointestinal bleeding is a common medical condition that account for over 300,000 hospitalizations in the USA annually, and carries considerable morbidity and mortality risks and health economic burdens [2]. Achieving endoscopic hemostasis at the time of the index endoscopy is essential to stop active bleeding, prevent rebleeding, and avoid the need for angiographic or surgical interventions, which are associated with considerable adverse events [3]. Rebleeding in particular directly increases the morbidity and mortality rates of patients with nonvariceal upper gastrointestinal bleeding [2]; thus, achieving primary hemostasis and preventing rebleeding are key goals of endoscopic therapy.
Endoscopy with combined therapy, such as including the deployment of through-the-scope (TTS) hemostatic clips, is the currently recommended first-line therapy for gastroduodenal peptic ulcer bleeding [4]. TTS clips, however, have limited hemostatic efficacy in ulcers with a fibrotic base, ulcers that are actively bleeding, and ulcers in difficult-to-access anatomical locations, such as the gastric lesser curvature, cardia, and within the posterior duodenal wall [5]. Combination therapy with TTS clips and diluted epinephrine injection or thermal therapy is superior over monotherapy for high-risk bleeding ulcers; however, patients with refractory ulcers are still referred for salvage surgery or angioembolization [6].
The Over-The-Scope Clip (OTSC) system (Ovesco® Endoscopy AG, Tubingen, Germany) is an effective rescue therapy for severe bleeding in patients who have failed to achieve hemostasis with TTS clips or combined therapy [7]. In a randomized clinical trial, the OTSC system proved to be superior to standard therapy in patients with recurrent peptic ulcer bleeding, with a 42.4% absolute difference [8]. In addition, the OTSC system is effective in treating perforated peptic ulcers < 15 mm [9]; in these cases, surgical interventions are avoided and oral feeding is resumed within a short time. Finally, OTSC treatment confers a low rebleeding rate compared to combined therapy.
A previous study showed that when used as a first-line therapy in patients with high-risk nonvariceal upper gastrointestinal bleeding, the OTSC system had a 100% hemostasis rate, with no cases of rebleeding during the 30-day follow-up period [10]. This study, however, lacked a comparison group. Consequently, we established a control study group to compare OTSC with the combined technique. Specifically, we aimed to evaluate the efficacy of the OTSC system as a first-line therapy in patients with high-risk bleeding ulcers compared to the combined treatment of TTS clips and epinephrine injection.
Methods
Study design
This was an observational, analytic, retrospectively cohort study. There were analyzed a database from patients who presented with high-risk ulcer-related gastrointestinal bleeding between May 2014 and September 2018 in a single, tertiary center of Ecuador. The local Institutional Review Board of the Instituto Ecuatoriano de Enfermedades Digestivas approved the study protocol. The study was conducted in accordance with the Declaration of Helsinki. All patients provided written informed consent for the endoscopic procedure. All authors had access to the study data and have reviewed and approved the final manuscript.
Study population
An ulcer was considered to be a high-risk bleeding peptic ulcer when (a) located in a major arterial territory (gastroduodenal or left gastric artery), (b) with a large-caliber artery (> 2 mm) visible during esophagogastroduodenoscopy, and/or c) with a fibrotic base or high-risk endoscopic stigmata (Forrest classification types I and II). No patients had undergone a previous endoscopic treatment attempt for bleeding management.
Patients were excluded from the analysis if they had bleeding secondary to varices, they underwent OTSC deployment for the closure of a fistula or tissue defect, the bleeding did not meet the criteria for high-risk ulcer bleeding, or they were lost to follow-up. All endoscopic and medical records were reviewed by three physicians (R.O., J.A.-V., J.B-B).
Study outcomes
The primary outcome of the present study was the efficacy of the OTSC system as a first-line therapy in patients with high-risk bleeding peptic ulcers compared to combined therapy with TTS clips and epinephrine injection. Feasibility was defined as the successful performance of the endoscopic technique. Efficacy was defined as immediate hemostasis with hemodynamic stability achieved during the index procedure and prevention of rebleeding within 30 days after treatment.
The secondary outcomes included the rebleeding rate, perforation rate, mean procedure time, reintervention rate, mean procedure cost and days of hospitalization in the two study groups within 30 days of the index procedure. Rebleeding was defined as a drop-in hemoglobin of > 2 g/dL accompanied by clinical signs of rebleeding. Procedure time was defined as the time it took the endoscopist to complete the procedure from scope in to scope out, including the mounting of the clips (OTSC or TTS).
Endoscopic technique
The decision to use TTS clips or OTSC was based on the preference of the endoscopist in each case and device availability in the endoscopic unit. Endoscopic procedures were performed by two experienced endoscopists (C.R.-M., J.A.-V.), who trained the same length of time in both types of techniques. For the endoscopic procedure, the patient was sedated with intravenous propofol, with continuous monitoring of the vital signs. The endoscopic procedure was performed after adequate fluid resuscitation and the achievement of hemodynamic stability.
All patients were treated with proton pump inhibitors. Patients were continuously monitored after the procedure, and the decision to keep them hospitalized or to discharge them was based on the clinical scenario. Patients were followed two days either during hospitalization or through a visit at the clinic and after 30 days through a clinic visit with esophagogastroduodenoscopy as part of the institutional protocol.
OTSC therapy
The OTSC system was attached to the tip of a gastroscope (EG-i10 Pentax Medical, Montalve, NJ, USA) that was 9.8 mm in diameter with a working channel diameter of 3.2 mm. The applicator cap was mounted on the tip of the endoscope carrying the OTSC. The thread was used to release the OTSC and was fixed to the applicator cap. The hand wheel was used to wind the thread and to apply the OTSC.
A 11/6 T nontraumatic OTSC was used with a 9-mm clipping width and a 16.5-mm maximum cap outer diameter. The OTSC was deployed by rotating the handle attached to the working channel of the endoscope, as in the endoscopic band ligation technique.
Combined therapy
For combined therapy, Resolution™ hemostatic clips (Boston Scientific®, Marlborough, USA) were used for all procedures. The number of clips was based on the operator’s preference in accordance with the clinical case. Epinephrine (1:10,000 epinephrine solution) was injected via a 25-G Carr-Locke injection needle (US Endoscopy, Heisley, Ohio, USA).
Statistical analyses
Continuous variables are described as the mean (standard deviation) or median (range: minimum–maximum) if they showed a normal distribution (Kolmógorov-Smirnov test). Categorical variables are described as the frequency (%). Both types of variables were compared between the groups (OTSC vs. combined therapy) using corresponding contrast hypothesis tests. The total cost per study group is expressed in US dollars (USD): this cost included both the overall procedure cost (endoscopy, clips, and epinephrine ampoule) and the hospitalization cost. A simple cost-effectiveness ratio (SCER) formula was used to compare the relationship between the median total cost by study group and the rate of rebleeding prevention (main study outcome). The incremental cost-effectiveness ratio (ICER) was calculated when appropriate. A p value < 0.05 was considered statistically significant. Data analysis was evaluated by a biostatistician (M. P-T) and performed in R v.3.4.3 (R Foundation for Statistical Computing; Vienna, Austria).
Results
Patients demographics
From May 2014 to September 2018, 285 patients were admitted to the institution for nonvariceal upper gastrointestinal bleeding management. A total of 95 patients met the inclusion criteria and were included in the analysis; of these patients, 46 received OTSC therapy and 49 received combined treatment. The median age was 62 (18.0–95.0) years, and 32.6% of the patients were female (Fig. 1).
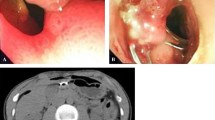
Twenty-three patients in the cohort were taking oral anticoagulants at the time of presentation; 12 in the OTSC group and 13 in the combined therapy group (p = 1.00). We found that most lesions in the study cohort were gastric ulcers (71.6%); 32/46 (69.6%) in the OTSC group and 36/49 (73.5%) in the combined therapy group. We found no statistically significant difference in the age, number of patients on oral anticoagulants, history of nonsteroidal anti-inflammatory drug use, previous red blood cell package transfusion for achieving hemodynamic stability, ulcer location, or size of ulcers. Most ulcers had an IIA Forrest classification (Fig. 2, Table 1).
Treatment costs
We found a significant difference in the number of clips required between the groups (p < 0.001). Specifically, the median number of OTSC procedures was one (range: 1–3), while the median number of TTS clips (used in combined therapy) was two (range: 1–8). In Ecuador, the cost of esophagogastroduodenoscopy with one OTSC deployment is $1016.00 and the cost of esophagogastroduodenoscopy with combined therapy consisting of TTS clips and epinephrine injection is $794.00 ($219 for one TTS clip, $175.00 for epinephrine injection).
We also found a significant difference in the median procedure cost between groups (p < 0.001), based on OTSC costing $1,020.00 (range: 1020.00–2250.00) and combined therapy costing $1010.00 (795.00–2330.00). The median duration of hospitalization in the study was 4 days (range: 1–28 days), with no statistically significant difference between the study groups (3 days for OTSC and 4 days for combined therapy; p = 0.215) (Table 2). We also found no statistically significant difference in the total cost of therapy, including the endoscopic procedure and hospitalization, between the two groups (p = 0.652). OTSC system group total cost was $2810.00 (range: 1610.00–18400.00) compared to $319,000 (range: 139,000–18000.00) for the combined therapy (Table 3). Combined therapy with TTS clips and epinephrine injection exhibited a statistically significant inferior median cost of endoscopic therapy compared to the OTSC system treatment; however, overall cost including hospitalization was not statistically different (Fig. 3).
Treatment efficacy and safety
We found no difference between the efficacies of either therapy: both approaches resulted in hemostatic and hemodynamic stability in all patients after the index procedure. No patients experienced gastrointestinal perforation within 30 days of the index procedure. No patients in the study experienced any adverse events as a consequence of the anesthesia and no patients died within 30 days of the procedure. OTSC had a 100% success rate for achieving primary hemostasis as combined therapy with TTS clips and epinephrine injection.
Rebleeding
Overall, six patients in the study experienced rebleeding (6.31%). In the OTSC group, two patients experienced rebleeding > 48 h (on days 5 and 15 of follow-up) after the index procedure. One of the affected patients was taking warfarin for atrial fibrillation, he had three antral ulcers that were successfully treated with one OTSC per ulcer but the reintroduction of warfarin initiated rebleeding on day 15 that required argon plasma coagulation. Histological analysis of the gastric ulcer isolated from the other affected patient showed a malignancy-related ulcer. The ulcer was retreated with a second OTSC, and no further rebleeding occurred.
In the combined therapy group, four patients experienced rebleeding. Three of these patients rebled within 48 h of the index procedure, for which two required an OTSC clip, and one required argon plasma coagulation. The fourth patient rebled 7 days after the index procedure, which required argon plasma coagulation. These cases of rebleeding were not associated with oral ASA or anticoagulant treatment. Overall, both treatments were safe with a low incidence of rebleeding.
Procedure time
Regarding the median procedure time, we found a significant reduction in the median procedure time in the OTSC group (11 min, range: 10–15 min) compared to that in the combined therapy group (20 min, range: 15–40 min) (p < 0.001) (Fig. 4).
Discussion
The present study aimed to compare the efficacy of the OTSC system and combined therapy with TTS clips and epinephrine injection as a first-line endoscopic treatment for high-risk bleeding peptic ulcers. Here, we found that OTSC treatment is as effective as combined therapy with TTS clips and epinephrine injection for managing high-risk bleeding ulcers. While we found a trend toward a reduced rebleeding rate in the OTSC group compared with that of the combined therapy group, this was not significantly different between the groups. The rebleeding events that occurred in the OTSC group were not associated with OTSC deployment; instead, they were associated with either anticoagulant therapy or neoplasia. Interestingly, OTSC treatment conferred a significantly reduced median procedure time compared to combined treatment; however, OTSC system tends to cost more per endoscopic treatment. Overall, our findings confirm that OTSC-based treatment of high-risk ulcers is effective, safe, and easy to perform in high-risk patients as a first-line monotherapy.
The literature regarding the efficacy of OTSC treatment for nonvariceal gastrointestinal bleeding is scant, especially in the setting of first-line treatment. Most data regarding OTSC treatment have been derived from patients with refractory bleeding after the failure of conventional methods, and in whom the OTSC system was used as rescue therapy before surgical or radiological re-intervention [7, 8, 11]. In these cases, however, the previous treatment attempt might have influenced the effectiveness of OTSC, resulting in rebleeding [8, 12].
Recently, Brander et al. published a retrospective study of 67 patients with a high risk of gastrointestinal bleeding as an adverse outcome, including patients with peptic ulcers, nonpeptic ulcers, and other lesions in the upper and lower digestive tract. The researchers found an 81.3% success rate in managing high-risk bleeding with OTSC [11]. Only 12 gastric ulcers and 31 duodenal ulcers were included in the analysis, and at least one previous intervention had been attempted in 26.9% of cases, followed by the use of the OTSC system as rescue therapy; these issues limit the evaluation of the OTSC system as a first-line therapy and likely contribute to the reduced overall success rate compared with that found in our study (95.6%). Additionally, 18 patients experienced rebleeding in this cohort; 12/18 rebled directly from the OTSC site, and 9/12 required repeat endoscopic and radiological intervention.
In another retrospective study, Richter-Schrag et al. demonstrated that second-line endoscopic treatment with the OTSC system had a significantly higher rebleeding risk compared to first-line endoscopic treatment, with an 8.2% rebleeding rate described for first-line therapy and a 28.2% rebleeding rate described for second-line therapy (OR 5.3, p = 0.008) [13]. Thus, the use of the OTSC system as first-line endoscopic treatment determines a higher primary hemostasis success and a lower rebleeding rates over second-line endoscopic treatment with the same OTSC system, demonstrating that primary OTSC treatment is an independent predictor to prevent rebleeding [11, 13]. Moreover, failed primary endoscopic hemostasis is an independent factor for rebleeding and is associated with increased mortality in patients with nonvariceal gastrointestinal bleeding [14].
In another study, Manno et al. retrospectively evaluated 40 consecutive patients who underwent OTSC treatment as a first-line option. Primary hemostasis was achieved in all patients, with no cases of rebleeding during the 30-day follow-up period; unfortunately, this study lacked randomization and a control group [10].
Conventional hemostasis therapies, such as contact thermal devices, TTS clips, epinephrine injection, and combined treatment, have proven to be effective in most patients with peptic ulcer bleeding. Mechanical, thermal or combined therapy does, however, fail in 5–20% of patients [15, 16]. In patients with high-risk lesions, bleeding might be difficult to manage due to the size, anatomical site, or presence of a fibrous base or large vessel. In this patient group, we propose that the OTSC system might be useful for reducing the procedure and anesthesia time and avoiding rebleeding and the need for reintervention.
In our cohort of patients treated with the OTSC system as a first-line therapy, only two patients (4.34%) experienced rebleeding. In one case, the rebleeding was associated with oral anticoagulant therapy: switching to heparin and argon plasma coagulation resolved the rebleeding. In the other case, rebleeding was associated with a malignant ulcer in which the OTSC migrated, and the deployment of a second OTSC was required to overcome the rebleeding. We consider that the adequate reintroduction of oral anticoagulants with close monitoring is essential in patients treated for ulcers with a high risk of rebleeding. In addition, in cases of ulcers with a high suspicion of neoplasia, endoscopists should attempt to avoid shallow placement or premature clip deployment to avoid OTSC therapy failure.
Technically, we consider that TTS clips might have a limited application compared to OTSCs due to the relatively small size of the TTS clip scope. This small size results in a restricted amount of tissue being compressed during deployment, inadequate hemostasis for large-size vessels, and the requirement for more than one clip to achieve hemostasis [5]. Indeed, despite the high-quality evidence available for TTS clips and combined therapy with epinephrine injection in treating peptic ulcer bleeding [6], we found that the OTSC system as a monotherapy is as effective as the combined therapy, with a significantly decreased median procedure time.
Finally, a previous cost-effectiveness analysis suggested that OTSC treatment in patients with recurrent peptic ulcer bleeding is associated with a lower cost compared to TTS clips if rebleeding after OTSC treatment is low [17]. In our study, we found no difference in the overall cost of the endoscopic procedure and hospitalization between patients treated with OTSCs or combined therapy. A multicenter clinical trial is currently underway to assess the efficacy of the OTSC system in comparison with combined therapy for the treatment of upper nonvariceal gastrointestinal bleeding with a high risk of recurrence; we anticipate that the data from this trial will address various remaining issues regarding primary treatment of high risk of rebleeding peptic ulcers.
The present study carries limitations inherent with its nonrandomized retrospective design, which can lead to selection bias. In addition, procedures were performed by two endoscopists in a single tertiary center, limiting the generalizability of these findings. However, considering the limited data available evaluating the efficacy of the OTSC system as an initial therapy for high-risk bleeding ulcers, we consider that our findings are novel and open the discussion of considering the OTSC system as a first-line or a rescue therapy in patients at a high risk of gastrointestinal bleeding. Multicenter, controlled randomized clinical trials comparing these two endoscopic techniques are now necessary to demonstrate the real clinical impact of using the OTSC system as a first-line therapy in the management of high-risk bleeding ulcers.
References
Lau JY, Barkun A, Fan D, Kuipers EJ, Yang Y, Chan FK (2013) Challenges in the management of acute peptic ulcer bleeding. Lancet 381:2033–2043
Elmunzer BJ, Young SD, Inadomi JM, Schoenfeld P, Laine L (2008) Systematic review of the predictors of recurrent hemorrhage after endoscopic hemostatic therapy for bleeding peptic ulcers. Am J Gastroenterol 103:2625–2632
Nykänen T, Peltola E, Kylänpää L, Udd M (2017) Bleeding gastric and duodenal ulcers: case-control study comparing angioembolization and surgery. Scand J Gastroenterol 52:523–530
Fujishiro M, Iguchi M, Kakushima N, Kato M, Sakata Y, Hoteya S, Kataoka M, Shimaoka S, Yahagi N, Fujimoto K (2016) Guidelines for endoscopic management of non-variceal upper gastrointestinal bleeding. Dig Endosc 28:363–378
Gralnek IM, Khamaysi I (2018) Is the over-the-scope clip device a first-line or rescue therapy for patients at high risk for gastrointestinal bleeding? Clin Gastroenterol Hepatol 16:627–629
Gralnek I, Dumonceau J-M, Kuipers E, Lanas A, Sanders D, Kurien M, Rotondano G, Hucl T, Dinis-Ribeiro M, Marmo R, Racz I, Arezzo A, Hoffmann RT, Lesur G, de Franchis R, Aabakken L, Veitch A, Radaelli F, Salgueiro P, Cardoso R, Maia L, Zullo A, Cipolletta L, Hassan C (2015) Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47:a1–46
Skinner M, Gutierrez JP, Neumann H, Wilcox CM, Burski C, Mönkemüller K (2014) Over-the-scope clip placement is effective rescue therapy for severe acute upper gastrointestinal bleeding. Endosc Int Open 2:E37–40
Schmidt A, Gölder S, Goetz M, Meining A, Lau J, von Delius S, Escher M, Hoffmann A, Wiest R, Messmann H, Kratt T, Walter B, Bettinger D, Caca K (2018) Over-the-scope clips are more effective than standard endoscopic therapy for patients with recurrent bleeding of peptic ulcers. Gastroenterology 155:674–686
Wei JJ, Xie XP, Lian TT, Yang ZY, Pan YF, Lin ZL, Zheng GW, Zhuang ZH (2019) Over-the-scope-clip applications for perforated peptic ulcer. Surg Endosc. https://doi.org/10.1007/s00464-019-06717-x
Manno M, Mangiafico S, Caruso A, Barbera C, Bertani H, Mirante VG, Pigò F, Amardeep K, Conigliaro R (2016) First-line endoscopic treatment with OTSC in patients with high-risk non-variceal upper gastrointestinal bleeding: preliminary experience in 40 cases. Surg Endosc 30:2026–2029
Brandler J, Baruah A, Zeb M, Mehfooz A, Pophali P, Wong Kee Song L, AbuDayyeh B, Gostout C, Mara K, Dierkhising R, Buttar N (2018) Efficacy of over-the-scope clips in management of high-risk gastrointestinal bleeding. Clin Gastroenterol Hepatol 16:690–696
Asokkumar R, Soetikno R, Sanchez-Yague A, Kim Wei L, Salazar E, Ngu J (2018) Use of over-the-scope-clip (OTSC) improves outcomes of high-risk adverse outcome (HR-AO) non-variceal upper gastrointestinal bleeding (NVUGIB). Endosc Int Open 06:E789–E796
Richter-Schrag H-J, Glatz T, Walker C, Fischer A, Thimme R (2016) First-line endoscopic treatment with over-the-scope clips significantly improves the primary failure and rebleeding rates in high-risk gastrointestinal bleeding: a single-center experience with 100 cases. World J Gastroenterol 22:9162–9171
Han YJ, Cha JM, Park JH, Jeon JW, Shin HP, Joo KR, Lee JI (2016) Successful endoscopic hemostasis is a protective factor for rebleeding and mortality in patients with nonvariceal upper gastrointestinal bleeding. Dig Dis Sci 61:2011–2018
Laine L, Jensen DM (2012) Management of patients with ulcer bleeding. Am J Gastroenterol 107:345–360
Barkun AN, Martel M, Toubouti Y, Rahme E, Bardou M (2009) Endoscopic hemostasis in peptic ulcer bleeding for patients with high-risk lesions: a series of meta-analyses. Gastrointest Endosc 69:786–799
Yu JX, Kaltenbach TR, Keyes E, Soetikno RM (2019) 340 Over the scope clips for recurrent peptic ulcer bleeding is cost effective as compared to the through the scope clips. Gastrointest Endosc 89:AB72
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Robles-Medranda is a key-opinion leader for Pentax Medical and Boston Scientific. Drs. Oleas, Alcívar-Vásquez, Puga-Tejada, Baquerizo-Burgos, and Pitanga-Lukashok declare no conflict of interest relevant to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Robles-Medranda, C., Oleas, R., Alcívar-Vásquez, J. et al. Over-The-Scope Clip system as a first-line therapy for high-risk bleeding peptic ulcers: a retrospective study. Surg Endosc 35, 2198–2205 (2021). https://doi.org/10.1007/s00464-020-07625-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07625-1