Abstract
Introduction
Pre-operative esophagogastroduodenoscopy (EGD) is becoming routine practice in patients undergoing bariatric surgery. Many patients with morbid obesity have obstructive sleep apnea (OSA), which can worsen hypoxia during an EGD. In this study, we report our outcomes using the SuperNO2VA™ device, a sealed nasal positive airway pressure mask designed to deliver high-fraction inhaled oxygen and titratable positive pressure compared to conventional nasal cannula.
Methods
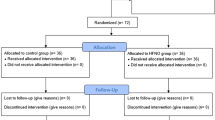
Between June 2016 and August 2017, we conducted a prospective observational study that included 56 consecutive patients who presented for EGD prior to bariatric surgery. Airway management was done using either the SuperNO2VA™ (N = 26) device or conventional nasal cannula (N = 30). Patient demographics, procedure details, and outcomes were compared between the two groups.
Results
The SuperNO2VA™ group had a lower median age compared to the control group (38.5 vs. 48.5 years, p = 0.04). These patients had a higher body mass index (BMI) (47.4 vs. 40.5, IQR, p < 0.0001), higher ASA class (p = 0.03), and were more likely to have OSA (53.9% vs. 26.7%, p = 0.04). Desaturation events were significantly lower in the SuperNO2VA™ group (11.5% vs. 46.7%, p = 0.004) and the median lowest oxygen saturation was higher in the SuperNO2VA™ group (100% vs. 90.5%, p < 0.0001).
Discussion
This is the first study to report on the use of the SuperNO2VA™ device in bariatric patients undergoing pre-operative screening EGD. The use of the SuperNO2VA™ device offers a clinical advantage compared to the current standard of care. Our data demonstrate that patients with higher BMI, higher ASA classification, and OSA were more likely to have the SuperNO2VA™ device used; yet, paradoxically, these patients were less likely to have issues with desaturation events. Use of this device can optimize care in this challenging patient population by minimizing the risks of hypoventilation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In preparation for bariatric surgery, pre-surgical esophagogastroduodenoscopy (EGD) is quickly becoming a routine practice. Some surgeons consider it mandatory for all Roux en-Y Gastric Bypass (RYGB) patients because the remnant stomach will no longer be easily accessible for future screening. Specific endoscopic findings that are detected pre-operatively, such as a large hiatal hernia, Barrett’s esophagus, Helicobacter pylori infection, or gastric lesions may also change the operative management of certain patients [1].
While simple endoscopic procedures do not require an anesthesia provider, it is generally recommended an anesthesiologist be present for higher-risk patients [2, 3]. Patients with morbid obesity undergoing pre-operative EGD pose a unique problem to physicians. Outside of the operating room, EGD presents a challenge to airway providers and a risk to patients, with hypoxemia occurring in up to 54% of patients [4,5,6,7]. This risk of hypoxemia is further exacerbated by morbid obesity and obstructive sleep apnea; both have been reported as independent risk factors with odds ratios two to nine times that of normal weight patients [4, 7]. This is likely secondary to increased risk for upper airway obstruction and hypoventilation, poor functional residual capacity, and increased oxygen consumption seen in these patients [5]. The presence of an anesthesia provider is an important part of managing these patients and has been shown to impact periprocedural outcomes; transient hypoxic episodes occur up to 19% when managed by anesthesiologist compared to 25–69% when managed by non-anesthesia providers [4, 6].
The current standard of care during sedation employs passive oxygenating devices, such as nasal cannula or supplemental oxygen facemask, along with continuous capnography monitoring, but the incidence of hypoxemia and other respiratory adverse events remains high [8]. Positive pressure ventilation (PPV) allows for maintenance of upper airway patency alongside delivery of high oxygen concentrations and ventilatory support, however current technology is limited during intra-oral procedures (e.g., EGD).
In this study, we employed the use of the SuperNO2VA™ (Vyaire Medical, Mettawa, IL); a sealed nasal positive airway pressure mask designed to deliver a high fraction of inhaled oxygen (FiO2) and titratable positive pressure when connected to standard anesthesia equipment (anesthesia machine or Mapleson circuit) as an alternative to the current standard of care in mitigating the risk of hypoxemia in this patient population.
Methods
During the period between June 6, 2016 and August 22, 2017, a prospective observational study was performed where data for 56 consecutive patients presenting for EGD prior to bariatric surgery were collected. At the discretion of the anesthesia team, without provocation from the surgical team, airway management was performed using either the SuperNO2VA™ device (n = 26), or conventional oxygen device (nasal cannula, n = 30). Consent for retrospective chart review was obtained on all bariatric patients and approved by the Institutional Review Board at New York Presbyterian, Weill Cornell Medical College. Patient sex, ethnicity, age, presence of obstructive sleep apnea (OSA), Mallampati score, and American Society of Anesthesiologists (ASA) classification were retrieved for each patient by reviewing the medical record (Table 1).
In our institution, pre-bariatric surgery EGD procedures are performed in the endoscopy suite, which is not outfitted with an anesthesia machine. Wall oxygen was used for both groups; for the control group, oxygen flow via nasal cannula was set at the discretion of the anesthesia team. For the SuperNO2VA™ group, the SuperNO2VA™ was secured over the nose and connected to a Mapleson F circuit (Jackson Rees modification of Ayre’s T-Piece; Fig. 1) connected to wall oxygen at 10 L/min. Pressure relief valve closure on the Mapleson circuit was titrated at the discretion of the anesthesia team throughout the procedure to generate nasal positive pressure. If deemed necessary by the anesthesia team, the procedure was interrupted at any time, removing the endoscope and bag-mask ventilating the patient with conventional full-face bag-valve-mask.

Image taken from https://www.vyaire.com/
The SuperNO2VA™ nasal positive airway pressure device. Artistic render of the SuperNO2VA™ device connected to a Mapleson circuit used for upper endoscopy.
For both groups, sedative dosing and airway intervention was determined by the anesthesia team to achieve deep sedation. Sedation-related adverse events were recorded live by a research assistant during the procedure, including the incidence and number of hypoxemic events (SpO2 < 90% for greater than 15 s), lowest SpO2 during the procedure, number of procedure interruptions requiring bag-mask ventilation, and morbidity. Additional patient data collected from the medical record included baseline SpO2, post-operative SpO2, procedure length, and length of stay in the post-anesthesia care unit (PACU).
Patient baseline demographic and clinical characteristics were analyzed and reported as frequencies or proportions for categorical data, means ± standard deviation (SD) for continuous parametric variables, and medians [interquartile ranges (IQR)] for continuous non-parametric variables. Differences in pre-operative and post-operative characteristics between groups were evaluated. Categorical variables were compared using Pearson’s Chi-square test (gender, ethnicity, Mallampati score, ASA class, presence of comorbidities, and/or OSA) and the Mann–Whitney U test was used to compare median age and BMI.
Results
Demographic information differed between the two groups (Table 1). The SuperNO2VA™ group had a higher percentage of males (50% vs. 23.3%, p = 0.04), a lower median age (38.5 vs. 48.5 years, p = 0.04), and differed in ethnicity (p = 0.01) from the control group. The SuperNO2VA™ group also had a higher mean BMI (47.4 vs. 40.5, IQR, p < 0.0001), percentage of patients with OSA (53.9% vs. 26.7%, p = 0.04), and ASA classification (p = 0.03).
There was no difference in baseline SpO2 between the two groups (Table 2). The incidence of desaturation events was significantly lower in the SuperNO2VA™ group (11.5% vs. 46.7%, p = 0.004) and the median lowest O2 was higher in the SuperNO2VA™ group (100% vs. 90.5%, p < 0.0001). Procedural interruptions to allow for bag-mask ventilation differed between the two groups (0 in SuperNO2VA™ group, 3 in Control group) but this did not reach statistical significance (p = 0.24). There was no difference in the length of procedure time between the two groups, post-op SpO2, or time spent in the post-anesthesia care unit. One complication was observed in the control group which was hypoxia requiring admission overnight.
Discussion
In this prospective observational study, when used at the discretion of the anesthesia team, the SuperNO2VA™ device allowed for better oxygenation of bariatric patients undergoing EGD and reduced the number of clinically significant hypoxemic events. Interestingly, these results were collected on patients with higher BMI, ASA Classification, and history of OSA compared to the control group. The efficacy is likely due to the beneficial effects of PPV, namely, improved upper airway patency and positive end-expiratory pressure (PEEP) allowing for enhanced alveolar patency and gas exchange. In the recent past, introduction of high-flow nasal oxygen during anesthesia has been reported with some success compared to standard care but is ineffective in the setting of upper airway obstruction or apnea, commonly encountered during EGD, making it a sub-optimal device for use in morbidly obese patients [9, 10]. The lack of positive pressure limits its utility on this patient population, where PPV allows for better oxygenation via improved alveolar ventilation.
The SuperNO2VA™ is the first of its kind on the market; it was first developed in 2017 and focuses on providing non-invasive positive airway pressure. It differs from nasal continuous positive pressure (CPAP): it has a low-profile mask with minimal dead space to facilitate endotracheal intubation, CO2 sample tubing within the mask, and high-flow oxygen up to 15 L/min. The positive pressure of this device maintains functional residual capacity, minimizes hypoventilation, pre-oxygenates, and maintains oxygen reserves. Ventilation may also be spontaneous, assisted, or controlled using this device.
With the use of a bite block and presence of the endoscope in the oropharynx, a patency in the oral cavity sometimes led to a pharyngeal pressure leak from the mouth when using the SuperNO2VA™. This mild gas leak is mostly inconsequential as fresh gas flows greater than 10 L/min, but in some patients it may disrupt positive pressure generation or preclude mask ventilation. Infrequently, we employed a technique of sub-mental pressure where the base of the tongue was manually engaged in the soft tissue of the sub-mental space and driven towards the hard palate. This created a seal around the endoscope against the palate and preferentially occluded the oral cavity internally, allowing for nasal positive pressure and PEEP generation (Fig. 2A, B). This technique can be particularly useful in the setting of apnea or desaturation, where rescue mask ventilation is possible without interrupting the procedure or removing the endoscope. Although rescue ventilation was not necessary for any patients in the SuperNO2VA™ arm of this trial, our experience tells us that this is common with nasal cannula and the SuperNO2VA™ may eliminate or greatly reduce the need to remove the endoscope altogether during airway management. A larger sample size would be valuable to identify this clinical advantage compared to standard care.

Images taken online from https://www.vyaire.com/us/resources/video-gallery?video=283460058
Sub-mental pressure technique. When gas leak from the mouth is significant (A), the clinician may press firmly in the sub-mental space, manually driving the tongue cephalad creating a seal around the endoscope into the hard palate, occluding the oral cavity internally (B).
Although these results are encouraging and support improved patient outcomes in this high-risk population, there are limitations to this study. First, as an observational trial, there were demographic differences between the two study groups. Although the SuperNO2VA™ group may seem clinically more difficult, the sample size was small. These results may have been insufficient to reach statistical significance for certain secondary endpoints, namely, the number of procedural interruptions, and PACU length of stay, which was trending positively in the SuperNO2VA™ arm and have substantial impact on clinical and economic outcomes.
Conclusions
In this prospective observational study, using the SuperNO2VA™ in the bariatric population undergoing EGD as part of their pre-operative assessment appears to offer a clinical advantage to the standard of care currently used, with improved oxygenation during the procedure and decreased incidence of hypoxemia. Trends illustrate additional improvements in the number of procedural interruptions necessary for bag-mask ventilation, and length of stay in the PACU. Despite not all outcomes reaching statistical significance, our study demonstrates the utility of such a device in optimizing care in a challenging population, by mitigating the risks of hypoventilation.
References
De Palma GD, Forestieri P (2014) Role of endoscopy in the bariatric surgery of patients. World J Gastroenterol 20(24):7777–7784. https://doi.org/10.3748/wjg.v20.i24.7777
Early DS, Lightdale JR, Vargo JJ et al (2018) Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc 87(2):327–337. https://doi.org/10.1016/j.gie.2017.07.018
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 96(4):1004–1017
Coté GA, Hovis RM, Ansstas MA et al (2010) Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol 8(2):137–142. https://doi.org/10.1016/j.cgh.2009.07.008
Yilmaz M, Aydin A, Karasu Z, Günşar F, Ozütemiz O (2002) Risk factors associated with changes in oxygenation and pulse rate during colonoscopy. Turk J Gastroenterol 13(4):203–208
Friedrich-Rust M, Welte M, Welte C et al (2014) Capnographic monitoring of propofol-based sedation during colonoscopy. Endoscopy 46(3):236–244. https://doi.org/10.1055/s-0033-1359149
Mehta PP, Kochhar G, Albeldawi M et al (2016) Capnographic monitoring in routine EGD and colonoscopy with moderate sedation: a prospective, randomized, controlled trial. Am J Gastroenterol 111(3):395–404. https://doi.org/10.1038/ajg.2015.437
Committee on Standards and Practice Parameters. Standards for basic anesthetic monitoring. https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring. Accessed 28 Jan 2019
Schumann R, Natov NS, Rocuts-Martinez KA et al (2016) High-flow nasal oxygen availability for sedation decreases the use of general anesthesia during endoscopic retrograde cholangiopancreatography and endoscopic ultrasound. World J Gastroenterol 22(47):10398–10405. https://doi.org/10.3748/wjg.v22.i47.10398
Patel A, Nouraei SAR (2015) Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 70(3):323–329. https://doi.org/10.1111/anae.12923
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Dimou, Dakin, Turnbull, Pomp, Samuels, Afaneh, and Ms. Huynh have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dimou, F., Huynh, S., Dakin, G. et al. Nasal positive pressure with the SuperNO2VA™ device decreases sedation-related hypoxemia during pre-bariatric surgery EGD. Surg Endosc 33, 3828–3832 (2019). https://doi.org/10.1007/s00464-019-06721-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06721-1