Abstract
Background and aims
Peroral endoscopic myotomy (POEM) may be associated with higher rates of gastroesophageal reflux disease (GERD) than laparoscopic Heller’s myotomy with fundoplication (LHM), since POEM is not combined with a fundoplication. However, peri-esophageal anti-reflux barriers are preserved in POEM, which might prevent GERD. Hence, we sought to compare the objective esophageal pH study findings in achalasia patients after POEM and LHM.
Methods
Achalasia patients undergoing POEM from 2014 to 2015 at our institution were matched 1:3 with LHM patients using propensity score matching. Demographics, prior interventions, pre-treatment and 2-month post-treatment timed barium esophagram (TBE), high-resolution esophageal manometry (HREM) and 24-h esophageal pH study findings were compared between the two groups.
Results
Thirty-one patients in the POEM group and 88 patients in the LHM group were included. Larger proportion of POEM patients had prior interventions for achalasia as compared to LHM patients (overall: 71% vs. 44.3%; p = 0.012). Esophageal acid exposure was significantly higher in POEM as compared to LHM patients (abnormal total acid exposure: 48.4% vs. 13.6%; p < 0.001, abnormal DeMeester score 54.8% vs. 17.4%; p = 0.005 respectively). In sub-group analysis, similar results were noted on 24-h pH study after exclusion of the POEM patients with prior LHM and corresponding matches. There was no significant difference in the rate of GERD symptoms between POEM and LHM. There was no significant correlation between the post-treatment basal lower esophageal sphincter pressure and integrated relaxation pressure with abnormal acid exposure in either POEM or LHM.
Conclusions
In patients with achalasia, POEM leads to significantly higher rates of abnormal esophageal acid exposure, without an increase in the rate of GERD symptoms, when compared to LHM with fundoplication. Interestingly, prior LHM has no impact on post-POEM pH study findings. Potential of increased esophageal acid exposure and possible consequences should be discussed with all patients prior to POEM. Further studies are needed to determine the long-term effects of increased acid exposure after POEM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Most therapeutic interventions have pros and cons. Iatrogenic gastroesophageal reflux disease (GERD) is a common after-effect of any treatment in achalasia. All current treatments for achalasia aim at palliation of symptoms by lowering the lower esophageal sphincter (LES) pressure, which may in turn lead to GERD. However, very effective laparoscopic Heller myotomy (LHM) was associated with significant rates of GERD [1]. Hence, LHM is usually combined with an anti-reflux procedure such as partial fundoplication to reduce postoperative GERD. This approach has brought down the rates of GERD to below 10% and is now the standard surgical approach [1].
Peroral endoscopic myotomy (POEM) is an emerging treatment modality for achalasia and is rapidly gaining popularity as the preferred treatment. It has the advantages of being minimally invasive like an endoscopic procedure along with the precision and efficacy of a surgical myotomy. It is shown to be at least as efficacious if not more than surgical myotomy at short- and intermediate-term follow-up [2]. Since POEM is not combined with an anti-reflux procedure, it may be associated with higher rates of GERD than LHM. However, in POEM, peri-esophageal anti-reflux barriers such as suspensory ligaments and angle of His are preserved in contrast to LHM. Hence theoretically, POEM should not lead to significantly higher rates of GERD than LHM with fundoplication. Asian studies have reported lower rates of GERD after POEM [3, 4]. It is not clear whether this finding is population specific or due to preservation of anti-reflux mechanisms during POEM procedure.
There are conflicting data on rates of abnormal esophageal pH study, GERD symptoms and endoscopic esophagitis after POEM. Several studies have shown that GERD is not a major problem after POEM [5,6,7,8]. Shiwaku et al. reported that the GERD symptoms and reflux esophagitis were present in a small minority of patients only [3]. However, studies have shown poor correlation between GERD symptoms and objective pH study findings after POEM [9, 10]. There are limited data on comparison of comprehensive pH study findings after POEM and LHM. Bhayani et al. showed that the abnormal pH study after POEM and LHM was comparable [11]. However, only less than half of the LHM and only about three quarters of the POEM patients underwent esophageal pH testing in that study. A recent meta-analysis by Repici et al. showed higher rates of GERD after POEM compared to LHM [12]. However, some of these studies did not classify achalasia into various subtypes based on high-resolution manometry (HREM). Hence, primary objective of our study was to compare the abnormal esophageal acid exposure and DeMeester score by a 2-month post-treatment 24-h pH study among POEM and LHM patients. Secondary objective was to compare the abnormal acid exposure and DeMeester scores by achalasia subtype, GERD symptoms, pre- and post-treatment HREM and timed barium esophagram (TBE) parameters between the two groups.
Methods
Study population
The institutional review board of the Clevelan d Clinic approved this study. All patients with achalasia who underwent POEM by authors MS and SR at our institution between January 2014 and December 2015 and had a 2-month post-treatment esophageal pH study completed were included in the study.
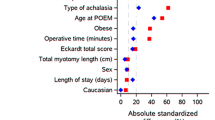
Matching to LHM group
Patients who underwent POEM were compared to those who had LHM with Dor fundoplication at our institution between January 2005 and December 2015. Propensity score matching was used to match patients who underwent POEM to those who underwent LHM on a 1:3 basis. A logistic regression model was used to estimate the propensity score; POEM was modeled as the outcome with age, gender, body mass index (BMI) and type of achalasia as the independent variables. The probability of having POEM done was used as the propensity score, and a greedy matching algorithm was used to find the best matches for each patient. The standardized differences in all covariates before and after matching were evaluated to assess the success of the matching. Five LHM patients had to be excluded as we found that they had no pH testing done within 2 months so for analysis, 26 POEM patients have three matches each, and five have only two each.
Study variables
The study variables included patient demographics such as age, gender and race, BMI, disease characteristics such as type of achalasia, duration of symptoms, prior therapeutic interventions for achalasia, TBE, HREM and 24 pH study findings. Data were collected by retrospective chart review.
Patient evaluation
Prior to contemplating POEM or LHM, all patients underwent multidisciplinary evaluation by a gastroenterologist and a thoracic surgeon and had TBE, HREM and an esophagogastroduodenoscopy (EGD). Based on HREM, achalasia was classified into various subtypes in both the groups. After POEM, all patients were prescribed proton pump inhibitors (PPI) for acid control. Two months after POEM or LHM, per our standard protocol, patients undergo transnasal catheter based 24 h esophageal pH study off PPIs and other acid reducing medications. Abnormal values on pH study were defined as: DeMeester score > 14.72, total acid exposure time > 5.5%, postprandial state > 6.8%, upright position > 8.2%, supine position > 3%, symptom index (SI) > 50%, symptom sensitivity index (SSI) > 10% and significant symptom association probability (SAP) as > 95%. The presence or absence of GERD symptoms was recorded at the time of clinical follow-up at 2 months after POEM or LHM.
POEM procedure
All POEM procedures were performed under general anesthesia with carbondioxide insufflation in an operating room using standard steps as described by Inoue et al. [13]. The steps were (1) a2-cm mucosotomy and creation of a submucosal tunnel starting approximately 10–12 cm proximal to the LES and extending distally to about 2–4 cm into the gastric side. The submucosal tunnel was usually created on anterior esophageal wall except in post-LHM patients in whom it was created on the posterior esophageal wall; (2) myotomy of the circular muscle fibers starting 3–4 cm distally from the mucosotomy and extending 2–4 cm into the gastric wall; and (3) closure of the mucosotomy with endoscopic clips. Next day, patients underwent a soluble contrast swallow radiograph to exclude transmural perforations. If the swallow study was unremarkable, patients were started on clear liquid diet, placed on twice daily PPI for 2 months, and were advised to advance diet gradually over the next 1–2 weeks.
LHM with fundoplication
In our patients, LHM was performed with anterior approach and thoracic esophagus was mobilized and full-thickness myotomy was performed along distal 4–6 cm of esophagus and extended 2–4 cm on to the gastric wall. Subsequently a partial anterior fundoplication (Dor fundoplication) was performed. Patients undergo a barium swallow study next day to exclude perforation, and if negative a liquid diet was be initiated and gradually advanced over the next few days.
Statistical analysis
Data are presented as median (25th, 75th percentiles) for continuous variables or frequency (percent) for categorical factors. All analyses were done using SAS version 9.4 (The SAS Institute, Cary, NC), and a p value < 0.05 was considered statistically significant.
Paired analysis
A paired univariable analysis was done to compare patients who underwent POEM and those who had LHM. Univariable conditional logistic regression analysis with POEM as the outcome was done to assess differences in patient demographics and pre-treatment characteristics while accounting for the matching. To assess differences in total acid exposure, acid exposure in upright and supine positions, type of symptoms, PPI use and GERD symptoms, models were built with each factor as the dependent variable (outcome) with type of treatment as the predictor. Conditional logistic regression was used to compare binary factors between the groups; this was done for outcomes observed in > 5 patients. In addition, mixed linear regression was used for the continuous variables using a natural logarithm transformation and a variance component correlation matrix to model the intra-cluster correlation.
Unpaired analysis
Standard unpaired methods were used to compare acid exposure during postprandial state, DeMeester score and the symptom scores because of the high number of missing values; Kruskal–Wallis tests were used for % time and scores, while Pearson’s Chi-square tests were used for the abnormal/normal variables. We also used these tests when comparing pH findings in the achalasia subtypes.
Results
Among a total of 66 POEM patients, 34 patients did not have a pH study performed at 2 months and one patient could not be matched. The remaining 31 patients, who underwent POEM along with a 2-month post-treatment 24-h esophageal pH study, were included in the final analysis. They were matched to 93 patients who underwent LHM, of which five were excluded since they did not have a pH study done at 2 months. Hence, a total of 88 LHM patients were included in the final analysis. There were no significant differences between patients in the two groups in terms of age, gender, race, BMI, subtype of achalasia and duration of symptoms (Table 1). Larger proportion of POEM patients had prior achalasia interventions compared to LHM patients (overall: 71% vs. 44.3%; p = 0.012, pneumatic dilatation: 35.5% vs. 18.2%; p = 0.041; LHM: 32.3% vs. 0%; p = 0.003 respectively).
Esophageal pH study findings
Abnormal esophageal acid exposure was significantly higher among POEM patients compared to LHM patients (48.4% vs. 13.6%, p < 0.001). This was true for all the parameters evaluated including total reflux time, upright reflux, supine reflux, postprandial reflux and DeMeester scores (Table 2; Fig. 1). However, there was no significant difference in the rate of GERD symptoms between POEM and LHM (28% vs. 14.9%, p = 0.38).
Subgroup analysis after excluding POEM patients with prior LHM
Table 3 presets the comparison of esophageal pH study findings after excluding the POEM patients with prior LHM and their corresponding matches. This subgroup of POEM patients had significantly higher total, supine, upright and postprandial acid reflux and DeMeester scores compared to LHM patients. These results are similar to those seen in the whole sample, suggesting that prior LHM has little impact on abnormal esophageal acid exposure and GERD symptoms in POEM patients. This can also be seen in the adjusted p values shown in Table 2.
Subtype of achalasia and esophageal pH study findings
In the POEM group, the subtypes of achalasia were type I in 13 patients, type II in 15 patients and type III in 3 patients. In the LHM group, the distribution was type I in 38 patients, type II in 43 and type III in 7 patients. Type of achalasia was not found to be associated with abnormal esophageal acid exposure in either POEM or LHM groups (Tables 4, 5). Since there were only three type III achalasia patients in POEM group, they were excluded from the final analysis due to a very small number.
Correlation between the pH study findings with LES pressures and myotomy length
Tables 6, 7 and 8 present the correlations between the esophageal pH study findings with post-POEM mean basal LES pressure, LES-IRP and myotomy length, respectively. Myotomy length was only available in the POEM patients and not in LHM group. There was no evidence to suggest any significant correlation.
TBE and HREM findings
Table 9 presents the comparison of HREM and TBE findings among the POEM and LHM patients. There was no significant difference in the pre-treatment HREM and TBE parameters except for greater height and width of barium column at 1 min in LHM patients compared to POEM patients. Post-treatment HREM and TBE parameters were similar except for greater height of barium column at 1 min in LHM patients compared to POEM patients. Despite pre- and post-treatment differences in TBE, there was no evidence to suggest any difference between the groups in terms of pre-/post-change in HREM or TBE parameters, suggesting that POEM and LHM were equally efficacious. Eckardt scores were not available in LHM patients to be compared with POEM patients.
Discussion
The main findings of our study were: significantly higher rates of abnormal esophageal acid exposure were seen after POEM compared to LHM with fundoplication in patients with achalasia. Subtype of achalasia, mean basal LES pressure or LES-IRP did not impact the pH study findings in both the treatment modalities. There was no significant difference in the rate of GERD symptoms between POEM and LHM. Our study findings imply that the potential of increased esophageal acid exposure and its possible consequences cannot be ignored and should be discussed with all patients prior to POEM.
High rates of abnormal esophageal acid exposure after POEM found in our study are similar to previous studies specifically from the western hemisphere. In a multicenter study from mostly Europe and USA by Kumbari et al., abnormal DeMeester score was found in 57.8% of patients and erosive esophagitis in 23.2% of patients after POEM [14]. However in that study, about 60% of patients with abnormal DeMeester scores did not have GERD symptoms [14]. Our study also found that only about 50% of patients with abnormal acid exposure reported GERD symptoms after POEM (28% with GERD symptoms vs. 55% with abnormal DeMeester score). This phenomenon—a disconnection between the degree of abnormal acid exposure and GERD symptoms—is likely due to pathologic esophageal denervation in patients with achalasia or burnout effect. Chronic esophageal acid exposure can be harmful and potentially lead to serious consequences, such as peptic strictures, Barrett’s esophagus and esophageal adenocarcinoma. Hence, we advocate that all patients with abnormal esophageal pH study irrespective of symptoms are placed on long-term acid suppression with PPIs.
Our study compared abnormal esophageal acid exposure after POEM and LHM with fundoplication, the two most precise and durable options for LES myotomy in achalasia. A recent meta-analysis by Repici et al. also found higher rates of abnormal pH study in POEM compared to LHM [12]. Some of the studies included in the meta-analysis did not have classification of achalasia into subtypes based on Chicago classification [15]. Also, some of these studies reported effect of single treatment modality rather than comparative effect. Another meta-analysis by Schlottmann F et al. found that patients undergoing POEM were more likely to develop GERD symptoms (OR 1.69, 95% CI 1.33–2.14, p < 0.0001) and have erosive esophagitis (OR 9.31, 95% CI 4.71–18.85, p < 0.0001), and abnormal esophageal acid exposure (OR 4.30, 95% CI 2.96–6.27, p < 0.0001) [16]. Our study results are consistent with the findings in those two meta-analyses. We have also matched our patients by propensity score matching with resultant homogeneity of patient populations in the two groups. In our study, subtype of achalasia, basal LES pressures or LES-IRP was not found to be associated with abnormal pH study in both POEM and LHM patients. Familiari et al. analyzed clinical, procedural and functional factors, associated with GERD and esophagitis after POEM [10]. These factors correlated minimally with GERD after POEM.
The major strength of our study was comprehensive objective assessment of incidence of GERD in age/sex and type of achalasia matched cases (POEM) and controls (LHM) by propensity matching method. Achalasia was also divided into various subtypes based on HREM findings according to Chicago classification [15]. Propensity matching is considered a strong statistical method next only to randomized controlled studies (RCT). However, there are several limitations that need to be mentioned. Most importantly, patients were not randomized to treatment methods. This may have resulted in differences in characteristics between the two groups though the baseline data were similar. Since we started POEM procedures in the 2014, patients who met the eligibility criteria were offered POEM preferably. As a result, the selection bias and our initial inexperience with POEM during possible learning curve may have created additional unrecognized differences between the treatment groups. Standard GERD symptom scores or quality of life questionnaires were not used in our study, which might have resulted in some variability in symptom assessment and reporting. Esophagogastroduodenoscopy (EGD) was not routinely performed post-intervention to assess for endoscopic esophagitis in our patients. Pre- and post-treatment Eckardt scores were not available in LHM patients. However, POEM and LHM were noted to be equally efficacious based on the assessment of the pre- and post-treatment HREM and TBE parameters.
In conclusion, POEM leads to higher rates of abnormal esophageal acid exposure compared to LHM. Since POEM is very rapidly disseminating and emerging as the preferred treatment modality for achalasia, these findings are timely and relevant. We suggest that the potential for increased esophageal acid exposure and its possible consequences should be discussed with all patients prior to POEM. Patients with abnormal pH study should be placed on long-term acid suppression regimen with PPIs and also on an endoscopic surveillance program, as suggested by several experts [17]. Further studies are needed to identify both patient-related and procedural technique-related factors that contribute to GERD after POEM and its prevention. Studies on long-term effects of GERD after POEM are also warranted.
References
Richards WO, Torquati A, Holzman MD et al (2004) Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 240(3):405–412 (discussion 412-5)
Awaiz A, Yunus RM, Khan S et al (2017) Systematic review and meta-analysis of perioperative outcomes of peroral endoscopic myotomy (POEM) and laparoscopic heller myotomy (LHM) for achalasia. Surg Laparosc Endosc Percutan Tech 27(3):123–131
Shiwaku H, Inoue H, Yamashita K et al (2016) Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first over 100 patients with short-term follow-up. Surg Endosc 30(11):4817–4826
Inoue H, Sato H, Ikeda H et al (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221(2):256–264
Swanstrom LL, Kurian A, Dunst CM et al (2012) Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 256:659–667
von Renteln D, Inoue H, Minami H et al (2012) Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 107(3):411–417
Minami H, Isomoto H, Yamaguchi N et al (2014) Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc 26:43–51
Familiari P, Gigante G, Marchese M et al (2016) Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first 100 patients with short-term follow-up. Ann Surg 263(1):82–87
Jones EL, Meara MP, Schwartz JS et al (2016) Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 30(3):947–952
Familiari P, Greco S, Gigante G et al (2016) Gastroesophageal reflux disease after peroral endoscopic myotomy: analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc 28(1):33–41
Bhayani NH, Kurian AA, Dunst CM et al (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259(6):1098–1103
Repici A, Fuccio L, Maselli R et al (2018) GERD after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc 87(4):934–943e18. https://doi.org/10.1016/j.gie.2017.10.022
Inoue H, Minami H, Kobayashi Y et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42(4):265–271
Kumbhari V, Familiari P, Bjerregaard NC et al (2017) Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy 49(7):634–642
Kahrilas PJ, Bredenoord AJ, Fox M et al (2015) International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2):160–174
Schlottmann F, Luckett DJ, Fine J et al (2018) Laparoscopic heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: a systematic review and meta-analysis. Ann Surg 267(3):451–460
Kahrilas PJ, Katzka D, Richter JE (2017) Clinical practice update: the use of per-oral endoscopic myotomy in achalasia: expert review and best practice advice from the AGA Institute. Gastroenterology 153(5):1205–1211
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Madhusudhan R. Sanaka, Dr. Prashanthi N. Thota, Dr. Malav P. Parikh, Dr. Umar Hayat, Dr. Niyati M. Gupta, Dr. Scott Gabbard, Rocio Lopez, Dr. Sudish Murthy and Dr. Siva Raja have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Sanaka, M.R., Thota, P.N., Parikh, M.P. et al. Peroral endoscopic myotomy leads to higher rates of abnormal esophageal acid exposure than laparoscopic Heller myotomy in achalasia. Surg Endosc 33, 2284–2292 (2019). https://doi.org/10.1007/s00464-018-6522-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6522-4