Abstract
Background
No study has shown the oncologic non-inferiority of robotic pancreatoduodenectomy (RPD) versus open pancreatoduodenectomy (OPD) for pancreatic cancer (PC).
Methods
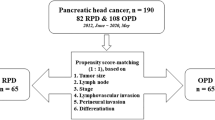
This is a single institution propensity score matched study comparing RPD and ODP for resectable PC, based on factors predictive of R1 resection (≤ 1 mm). Only patients operated on after completion of the learning curve in both procedures and for whom circumferential margins were assessed according to the Leeds pathology protocol were included. The primary study endpoint was the rate of R1 resection. Secondary study endpoints were as follows: number of examined lymph nodes (N), rate of perioperative transfusions, percentage of patients receiving adjuvant therapies, occurrence of local recurrence, overall survival, disease-free survival, and sample size calculation for randomized controlled trials (RCT).
Results
Factors associated with R1 resection were tumor diameter, number of positive N, N ratio, logarithm odds of positive N, and duodenal infiltration. The matching process identified 20 RPDs and 24 OPDs. All RPDs were completed robotically. R1 resection was identified in 11 RPDs (55.0%) and in 10 OPDs (41.7%) (p = 0.38). There was no difference in the rate of R1 at each margin as well as in the proportion of patients with multiple R1 margins. RPD and OPD were also equivalent with respect to all secondary study endpoints, with a trend towards lower rate of blood transfusions in RPD. Based on the figures presented herein, a non-inferiority RCT comparing RPD and OPD having the rate of R1 resection as the primary study endpoint requires 3355 pairs.
Conclusions
RPD and OPD achieved the same rate of R1 resections in resectable PC. RPD was also non-inferior to OPD with respect to all secondary study endpoints. Because of the high number of patients required to run a RCT, further assessment of RPD for PC would require the implementation of an international registry.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Robotic pancreatoduodenectomy (RPD) [1] is gaining momentum, as feasibility [2,3,4] and safety [5,6,7] of this minimally invasive procedure have been reported. What is still lacking is the evidence of oncologic equivalence of RPD vs. open pancreatoduodenectomy (OPD) in the treatment of pancreatic cancer (PC).
The ideal pancreatoduodenectomy for PC should achieve negative circumferential margins [8, 9], retrieve an adequate number of lymph nodes [9, 10], minimize the use of perioperative blood transfusions [11], and reduce post-operative morbidity so that adjuvant medical therapies can be timely administered [12, 13]. Unfortunately, some of these parameters do not purely reflect the quality of surgery as they are influenced also by non-surgical factors. The rate of margin positivity, for instance, depends also on the accuracy of pathology analysis [14] and the definition used to identify clear margins (i.e., 0 vs. ≤ 1 mm) [15].
The introduction of the Leeds Pathology Protocol (LEEPP) [16] provides a highly standardized method to analyze pancreatoduodenectomy specimens, making surgery the only human-dependent variable that can potentially influence the rate of R1 resection.
We herein provide a propensity score-matched analysis of RPD vs. OPD for resectable PC having margin status assessed by LEEPP as the primary endpoint.
Materials and methods
This study was designed and reported according to the STROBE guidelines [17] and was approved by the Institutional Review Board of the University of Pisa.
A retrospective case-controlled analysis of a prospectively maintained database on all pancreatic resections was performed for all patients undergoing pancreatoduodenectomy for clearly resectable PC in whom the LEEPP [16] was used for specimen analysis between February 1, 2014 and January 31, 2017. All procedures were performed at a single institution (Division of General and Transplant Surgery, University of Pisa) by the senior author (U.B.), who had completed the learning curve for both OPD [18] and RPD [4] before February 1, 2014. The same oncologic principles were followed in RPD and OPD, as previously described [2, 5].
The primary endpoint of this study was the rate of positive margins. The two study groups were matched by propensity scores based on factors predicting margin positivity.
Secondary endpoints were number of examined lymph nodes, rate of perioperative transfusions, percentage of patients receiving adjuvant chemotherapy or chemo-radiation therapy, overall survival, disease-free survival, rate of local cancer recurrence, and sample size calculation for RCTs having the rate of positive margins as the main study endpoint.
Definition of clearly resectable PC
Patients with resectable PC were identified based on NCCN guidelines [19], but patients with tumors showing a vein contact ≤ 180° without vein contour irregularity were excluded. On practical grounds, only patients with clear margins all around PC, as shown by contrast-enhanced computed tomography (C-ECT), were considered to have a clearly resectable PC.
Selection criteria for RPD
Patients were selected for RPD when generally suitable for laparoscopy, when body mass index was < 35 kg/m2, and when the robotic system was timely available [5,6,7].
Inclusion criteria
All patients included in this study were initially selected for RPD. As reported previously [6], at our Institution several patients suitable for RPD have actually to undergo OPD because the robotic system is not timely available (i.e., ≤ 4 weeks from the initial surgical consultation). Although several patients with borderline resectable PC [20, 21] underwent RPD and OPD during the study period, they were not included in this study.
Pathological examination of resected specimens
All specimens were analyzed according to the principles established by the LEEPP [16]. Briefly, margins were stained in the fresh specimen that, after fixation in 10% buffered formalin, was serially sliced in < 5-mm-thick slices in a plane perpendicular to the duodenal axis. Each axial slice was examined in a single large slide, so that circumferential margins could be accurately assessed. Seven margins were assessed: anterior surface, posterior surface, vein bed, SMA groove, pancreatic neck, proximal duodenum/stomach, and common bile duct. All resected lymph nodes were also analyzed.
Definition of primary and secondary outcome measures
Margins were defined positive (R1) if tumor cells were detected ≤ 1 mm of any margin. A subgroup named R1-direct (0 mm), in which cancer cells were immediately present at resection margins, was also identified to allow comparison with series using this definition to identify R1 status [22].
The number of examined lymph nodes corresponded to the overall number of nodes analyzed at pathology.
The rate of perioperative transfusions corresponded to the percentage of patients receiving blood transfusions during the hospital stay.
The rate of patients receiving adjuvant medical therapies corresponded to the percentage of patients undergoing adjuvant chemotherapy or chemo-radiation therapy.
The rate of local cancer recurrence corresponded to the percentage of patients with local tumor regrowth in the surgical bed.
Overall survival time was defined as the time from surgery to death from any reasons.
Disease-free survival time was defined as the time from to diagnosis of tumor recurrence.
Sample size calculation for RCTs was performed according to a on a non-inferiority study design.
Definition of other outcome measures
All perioperative events occurring within 90 days of surgery were recorded.
Occurrence and severity of post-operative pancreatic fistula (POPF) [23], delayed gastric emptying [24], and post-pancreatectomy hemorrhage [25] were defined according to the International Study Group on Pancreatic Surgery. Grade B and grade C POPF were considered clinically relevant.
Post-operative complications were classified according to Clavien–Dindo [26] and were considered severe when graded IIIb and higher [27]. In patients with more than one complication, the highest grade was considered. The comprehensive complication index was also calculated [28].
Statistics and matching strategy
Categorical variables are presented as rates and proportions. Continuous variables are reported as mean ± SD if normally distributed or as median and interquartile range (IQR) if not.
ROC curves were used to calculate the cut-off value of the tumor size at CT scan.
Relationship between outcome (R1) and surgical approach (OPD and RPD) was evaluated by linear logistic regression (Chi-Square test, Odd ratio), before and after matching.
Overall survival and disease-free survival were calculated by using Kaplan–Meier curves and compared between the two surgical approach groups (OPD and RPD) by using Log-rank test, after matching.
According to the recommendations by Lonjon et al. [29], propensity score matching was applied to achieve a balanced exposure groups at baseline (i.e., minimal confounding). All significant predictors of outcome (R1) were identified by using univariate logistic regression in the overall population and were used as covariates to perform a propensity score analysis in order to balance them into the two treatment groups. Linear propensity score values were used to conduct a “full matching” between two surgical approach groups (OPD and RPD).
Post-matching covariance analysis and sensitivity analysis were then evaluated using Rosenbaum test.
For the statistical significance of the test a power = 80%, p < 0.05, two-tailed significance level was used.
Sample size calculation for a non-inferiority randomized controlled trial, comparing OPD and RPD and having R1 as the primary endpoint, was performed based on the results obtained in the current series. Sample size was estimated using the Farrington & Manning Score test at α = 0.025, power = 90%, and non-inferiority margin difference of 10% the actual group reference proportion.
Statistical analysis were carried out using JMP® 9.0.1 software package for Mac, Copyright© SAS Institute Inc., SAS campus Drive, Cary, NC, USA, SPSS Statistics for Mac, Version 20.0., IBM Corp., Armonk, NY, USA, R Package, R Core Team (2014): A language and Environment for Statistical Computing, R Foundation for Statistical Computing, Vienna AT, available at http://www.r-project.org/ and PASS 2005 software package (Hintze J 2004, NCSS and PASS, Number Cruncher Statistical System, Kaysville, Utah. http://www.NCSS.COM).
Results
During the study period, a total of 268 pancreatoduodenectomies were performed at our Division. These procedures included 175 OPD (85 with either a venous or an arterial resection) and 93 RPD (9 with a vein resection). A diagnosis of PC, excluding malignant intraductal papillary mucinous neoplasms, was eventually proven in 131 patients. When 67 patients requiring associated vascular procedures and/or receiving neoadjuvant therapies were excluded, 64 were left who could have been potentially eligible for RPD based on purely anatomic parameters. After excluding 14 additional patients, who were not considered candidate for RPD because of non-oncologic reasons based on our general selection criteria [5], a total of 50 pancreatoduodenectomies were left that met the inclusion criteria for this study (RPDs = 24; OPDs = 26). No RPD was converted to OPD, laparoscopy, or hand assistance.
Outcomes in the unmatched cohorts
Patients undergoing RPD and OPD were similar with respect to mean preoperative Ca19.9 (428 ± 647 vs. 1266 ± 4300 U/L), mean neutrophil-to-lymphocyte ratio (3 ± 2 vs. 3 ± 2), mean platelet-to-lymphocyte ratio (174 ± 65 vs. 185 ± 72), mean tumor diameter (3 ± 0.73 vs. 3 ± 0.74 cm), percentage of T3 tumors (91.6 vs. 100%), rate of lymph node positivity (91.7 vs. 80.8%), proportion of moderately differentiated tumors (75.0 vs. 76.9%), presence of perineural infiltration (95.8 vs. 84.6%), and duodenal infiltration (37.5 vs. 50.0%). The groups were also similar with respect to the mean number of examined lymph nodes (45.0 ± 15.0 vs. 42.0 ± 17.0), the mean number of positive lymph nodes (7.0 ± 7.0 vs. 4.0 ± 6.0), the lymph node ratio (0.16 ± 0.16 vs. 0.11 ± 0.16), and the log odds of positive lymph nodes (LOODS) (− 2.02 ± 1.31 vs. − 2.55 ± 1.33).
R1 resection (≤ 1 mm) occurred in similar percentages between the two groups (54.2 vs. 38.5%). No difference was noted in the site of R1: anterior margin (4.1 vs. 15.3%), posterior margin (33.3 vs. 15.3%), vein margin (25.0 vs. 19.2%), and SMA margin (20.8 vs. 7.6%). No patient had R1 histology at the pancreatic neck, the bile duct, and the duodenal margin. Multiple R1 margins were present in 20.8% of RPDs and in 15.3% of OPDs.
A summary of operative data and post-operative morbidity is provided in Table 1.
Factors predictive of R1
As reported in Table 2, 19 preoperative and 7 post-operative variables were assessed to define the factors associated with R1 resection.
Tumor diameter, measured at either preoperative contrast-enhanced computed tomography (C-ECT) or specimen pathology, number of positive lymph nodes, lymph node ratio, logarithm odds of positive lymph nodes (LOODS), and duodenal infiltration were associated with a higher probability of R1 resection.
The cut-off value of C-ECT tumor diameter was 26.0 mm (AUC 0.78; p = 0.0013).
Comparison of matched cohorts (margin status)
Using the six parameters shown to predict the development of R1 in the current series a propensity score analysis was performed. A linear value of propensity score was defined from propensity score analysis and was used as covariate in a logistic regression analysis to define the OR for R1 in RPD and OPD. The adjusted value of the “crude” effect size varied from 1.89 (0.26–5.97) in the unmatched cohorts, to 1.71 (0.52–5.81) in the matched cohorts. Rosembaum sensitivity analysis showed that the results of our propensity score matching were not sensitive to hidden biases (the lower bound of the p value overlapped the significance level within a Gamma change of 0.6).
The matching process identified 20 RPD and 24 OPD. The baseline characteristics of these groups are presented in Table 3.
No patient in either groups had direct margin positivity. R1 resection (≤ 1 mm) was identified in 11 RPD (55.0%) and 10 OPD (41.7%) (p = 0.38). There was no difference in the rate of R1 at the SMA margin and the vein margin, as well as in the proportion of patients with multiple R1 margins (Table 4).
Comparison of matched cohorts (secondary study endpoints)
A summary of results concerning the secondary endpoints of this study is provided in Table 5.
No difference was identified in the mean number of examined lymph nodes, and in the percentage of patients receiving adjuvant chemotherapy and/or radiation therapy. Local recurrence developed in similar proportions of patients after RPD (15.0%) and OPD (8.3%). RPD was associated with a trend towards fewer overall and intraoperative blood transfusions, and with a lower number of transfused blood units per patient.
Based on the results of this study, a non-inferiority RCT comparing RPD and OPD having the rate of R1 resection as the primary study endpoint requires 3355 pairs (α = 0.025, power = 90%, non-inferiority margin of 10% corresponding to a value of 0.038).
Discussion
Surgery is clearly not enough to cure most patients with resectable PC, but remains the only chance for cure. Probably a realistic view of the current role of resection in the treatment of PC is to achieve an R0 resection along with removal of an adequate number of lymph nodes, obtained at the price of a low post-operative morbidity so that as many patients as possible can receive full course adjuvant therapies.
In the early stages of the development of RPD, many surgeons have preferred to select patients with tumor types not requiring extensive retroperitoneal dissection, such as periampullary cancers [30, 31]. This strategy permitted the development of RPD, but made evidence on oncologic suitability of RPD for PC scarce and poorly standardized. This study was specifically designed to provide this piece of information by matching two groups of patients diagnosed with PC and undergoing RPD or OPD. The rate of R1 resection was identified as the main treatment endpoint, because this parameter is probably the single most reliable factor showing the oncologic adequacy of resection for PC [22].
The first important information from this study is the safety of RPD in PC. As expected, because of favorable gland texture and duct size, the rate of clinically relevant POPF was lower than reported in series of RPD including mixed tumor types [2, 5, 6]. Although the stringent selection criteria adopted in this study limited the number of procedures available for analysis, these results are in accordance with our previous study where we found few clinically relevant POPF in patients stratified at low or negligible risk for POPF [7]. Since hard gland texture and enlarged pancreatic duct are typically associated with PC, lower rates of POPF are indeed expected to occur in this setting [32] and clearly underscore the need to define the oncological suitability of RPD for PC.
Our study provides also the initial evidence that RPD vs. OPD can achieve the same rate of R1 resections in PC. The rate of R1 resections that was recorded in this study is slightly inferior to the figures reported in the literature using the LEEPP [14, 16]. This difference is probably caused by the lack of borderline resectable PC in this series. However, equivalence in the rate of R1 resections between RPD and OPD unambiguously shows that RPD allows the surgeon to follow the same dissection planes validated in OPD. On practical grounds, RPD does not limit the ability of the surgeon to follow the periadventitial plane along the right side of the SMA, that is considered key to limit the rate of R1 resections in pancreatoduodenectomy for PC [33]. Actually, following a dissection plane close to the right side of the SMA, with early ligation of the inferior pancreaticoduodenal artery [34], makes dissection drier and easier and is therefore particularly convenient in the setting of a minimally invasive procedure such as RPD.
Equivalence in the number of examined lymph nodes further demonstrates that RPD does not limit the surgeon ability to clear as much lympho-neural tissue as required. It is also worth to note that RPD was associated with a trend towards reduced need for perioperative blood transfusions and a lower number of blood units transfused per patient. The rate of perioperative blood transfusions is a quality indicator in pancreatoduodenectomy [11]. Ability to receive adjuvant chemotherapy, possibility to sustain full course treatment and/or receive combination therapy, and rate of local recurrence were all similar in matched cohorts of RPD and OPD. Based on the data obtained from our study, we have estimated that a non-inferiority RCT having margin status as the primary endpoint requires 3355 pairs. Considering that the enrolment of this number of patients would be hardly feasible, even in a multicenter study, we suggest that the role of RPD for PC should be further evaluated in the context of an international registry.
An important piece of information that is lacking in the current literature, and that it is not provided by this study, is the oncologic value of RPD vs. laparoscopic pancreatoduodenectomy (LPD). A recently published systematic review and network meta-analysis [35] shows that RPD achieves higher rates of margin negative resections when compared to either LPD or OPD. Considering that at nearly all institutions performing minimally invasive pancreatoduodenectomy, a single approach was adopted or different approaches were implemented sequentially (e.g., starting with laparoscopic resection with open reconstruction and developing into pure LPD), it is unlikely that a study comparing LPD to RPD will be published from a single institution. Data from research consortia, such as the E-MIPS (European Consortium on Minimally Invasive Pancreatic Surgery; http://www.e-mips.org), or from registries could instead provide this important comparison.
The main limitations of this study are the retrospective nature, the limited sample size, and the yet limited duration of the follow-up period that does not allow us to present meaningful data on long-term survival. A further limitation of this study is the exclusion of patients who received neoadjuvant therapies. This decision was based on several considerations. First, although neoadjuvant therapies are increasingly used in borderline resectable and locally advanced pancreatic cancer [36], there is no clear evidence that these treatments should be implemented also in immediately resectable pancreatic cancer [19, 37, 38]. Second, neoadjuvant therapies are expected to influence margin status after resection [9]. Since margin status was the primary endpoint in this study, including patients who received neoadjuvant therapies could have introduced a confounding variable.
In conclusion, we have shown that RPD achieves the same local radicality of OPD in resectable PC. These results are not obtained at the expenses of higher morbidity or mortality, decreased probability of receiving adjuvant treatments, and increased rate of local recurrence. Running a RCT having R1 rate as the primary endpoint is barely feasible at the present time, because of the magnitude of estimated sample size. Implementation of an international registry could be the next step in the assessment of RPD for PC.
References
Montagnini AL, Røsok BI, Asbun HJ, Barkun J, Besselink MG, Boggi U, Conlon KC, Fingerhut A, Han HS, Hansen PD, Hogg ME, Kendrick ML, Palanivelu C, Shrikhande SV, Wakabayashi G, Zeh H, Vollmer CM, Kooby DA (2017) Standardizing terminology for minimally invasive pancreatic resection. HPB 9:182–189
Boggi U, Signori S, De Lio N, Perrone VG, Vistoli F, Belluomini M, Cappelli C, Amorese G, Mosca F (2013) Feasibility of robotic pancreaticoduodenectomy. Br J Surg 100:917–925
Zureikat AH, Moser AJ, Boone BA, Bartlett DL, Zenati M, Zeh HJ (2013) 250 robotic pancreatic resections: safety and feasibility. Ann Surg 258:554–559
Napoli N, Kauffmann EF, Palmeri M, Miccoli M, Costa F, Vistoli F, Amorese G, Boggi U (2016) The learning curve in robotic pancreaticoduodenectomy. Dig Surg 33:299–307
Napoli N, Kauffmann EF, Menonna F, Perrone VG, Brozzetti S, Boggi U (2016) Indications, technique, and results of robotic pancreatoduodenectomy. Updates Surg 68:295–305
Boggi U, Napoli N, Costa F, Kauffmann EF, Menonna F, Iacopi S, Vistoli F, Amorese G (2016) Robotic-assisted pancreatic resections. World J Surg 40:2497–2506
Napoli N, Kauffmann EF, Menonna F, Costa F, Iacopi S, Amorese G, Giorgi S, Baggiani A, Boggi U (2018) Robotic versus open pancreatoduodenectomy: a propensity score matched analysis based on factors predictive of postoperative pancreatic fistula. Surg Endosc 32:1234–1247
Sabater L, García-Granero A, Escrig-Sos J, Gómez-Mateo Mdel C, Sastre J, Ferrández A, Ortega J (2014) Outcome quality standards in pancreatic oncologic surgery. Ann Surg Oncol 21:1138–1146
Merkow RP, Bilimoria KY, Bentrem DJ, Pitt HA, Winchester DP, Posner MC, Ko CY, Pawlik TM (2014) National assessment of margin status as a quality indicator after pancreatic cancer surgery. Ann Surg Oncol 21:1067–1074
Tomlinson JS, Jain S, Bentrem DJ, Sekeris EG, Maggard MA, Hines OJ, Reber HA, Ko CY (2007) Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg 142:767–774
Ball CG, Pitt HA, Kilbane ME, Dixon E, Sutherland FR, Lillemoe KD (2010) Peri-operative blood transfusion and operative time are quality indicators for pancreatoduodenectomy. HPB 12:465–471
Wu W, He J, Cameron JL, Makary M, Soares K, Ahuja N, Rezaee N, Herman J, Zheng L, Laheru D, Choti MA, Hruban RH, Pawlik TM, Wolfgang CL, Weiss MJ (2014) The impact of postoperative complications on the administration of adjuvant therapy following pancreaticoduodenectomy for adenocarcinoma. Ann Surg Oncol 21:2873–2881
Nussbaum DP, Adam MA, Youngwirth LM, Ganapathi AM, Roman SA, Tyler DS, Sosa JA, Blazer DG (2016) Minimally invasive pancreaticoduodenectomy does not improve use or time to initiation of adjuvant chemotherapy for patients with pancreatic adenocarcinoma. Ann Surg Oncol 23:1026–1033
Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess H, Schirmacher P, Büchler MW (2008) Most pancreatic cancer resections are R1 resections. Ann Surg Oncol 15:1651–1660
Sugiura T, Uesaka K, Mihara K, Sasaki K, Kanemoto H, Mizuno T, Okamura Y (2013) Margin status, recurrence pattern, and prognosis after resection of pancreatic cancer. Surgery 154:1078–1086
Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A (2006) Redefining the R1 resection in pancreatic cancer. Br J Surg 93:1232–1237
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2007) The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457
Fisher WE, Hodges SE, Wu MF, Hilsenbeck SG, Brunicardi FC (2012) Assessment of the learning curve for pancreaticoduodenectomy. Am J Surg 203:684–690
Tempero MA, Malafa MP, Al-Hawary M, Asbun H, Bain A, Behrman SW, Benson AB 3rd, Binder E, Cardin DB, Cha C, Chiorean EG, Chung V, Czito B, Dillhoff M, Dotan E, Ferrone CR, Hardacre J, Hawkins WG, Herman J, Ko AH, Komanduri S, Koong A, LoConte N, Lowy AM, Moravek C, Nakakura EK, O’Reilly EM, Obando J, Reddy S, Scaife C, Thayer S, Weekes CD, Wolff RA, Wolpin BM, Burns J, Darlow S (2017) Pancreatic adenocarcinoma, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 15:1028–1061
Kauffmann EF, Napoli N, Menonna F, Vistoli F, Amorese G, Campani D, Pollina LE, Funel N, Cappelli C, Caramella D, Boggi U (2016) Robotic pancreatoduodenectomy with vascular resection. Langenbecks Arch Surg 401:1111–1122
Boggi U, Del Chiaro M, Croce C, Vistoli F, Signori S, Moretto C, Amorese G, Mazzeo S, Cappelli C, Campani D, Mosca F (2009) Prognostic implications of tumor invasion or adhesion to peripancreatic vessels in resected pancreatic cancer. Surgery 146:869–881
Strobel O, Hank T, Hinz U, Bergmann F, Schneider L, Springfeld C, Jäger D, Schirmacher P, Hackert T, Büchler MW (2017) Pancreatic cancer surgery: the new R-status counts. Ann Surg 265:565–573
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, International Study Group on Pancreatic Fistula Definition (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW (2007) Postpancreatectomy hemorrhage (PPH)—An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Petermann D, Demartines N, Schäfer M (2013) Severe postoperative complications adversely affect long-term survival after R1 resection for pancreatic head adenocarcinoma. World J Surg 37:1901–1908
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Lonjon G, Porcher R, Ergina P, Fouet M, Boutron I (2017) Potential pitfalls of reporting and bias in observational studies with propensity score analysis assessing a surgical procedure: a methodological systematic review. Ann Surg 265:901–909
Cirocchi R, Partelli S, Trastulli S, Coratti A, Parisi A, Falconi M (2013) A systematic review on robotic pancreaticoduodenectomy. Surg Oncol 22:238–246
Boggi U, Amorese G, Vistoli F, Caniglia F, De Lio N, Perrone V, Barbarello L, Belluomini M, Signori S, Mosca F (2015) Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc 29:9–23
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr (2013) A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg 216:1–14
Butler JR, Ahmad SA, Katz MH, Cioffi JL, Zyromski NJ (2016) A systematic review of the role of periadventitial dissection of the superior mesenteric artery in affecting margin status after pancreatoduodenectomy for pancreatic adenocarcinoma. HPB 18:305–311
Ishizaki Y, Sugo H, Yoshimoto J, Imamura H, Kawasaki S (2010) Pancreatoduodenectomy with or without early ligation of the inferior pancreatoduodenal artery: comparison of intraoperative blood loss and short-term outcome. World J Surg 34:2939–2944
Ricci C, Casadei R, Taffurelli G, Pacilio CA, Ricciardiello M, Minni F (2018) Minimally invasive pancreaticoduodenectomy: what is the best “choice”? A systematic review and network meta-analysis of non-randomized comparative studies. World J Surg 42:788–805
Ferrone CR, Marchegiani G, Hong TS, Ryan DP, Deshpande V, McDonnell EI, Sabbatino F, Santos DD, Allen JN, Blaszkowsky LS, Clark JW, Faris JE, Goyal L, Kwak EL, Murphy JE, Ting DT, Wo JY, Zhu AX, Warshaw AL, Lillemoe KD, Fernández-del Castillo C (2015) Radiological and surgical implications of neoadjuvant treatment with FOLFIRINOX for locally advanced and borderline resectable pancreatic cancer. Ann Surg 261:12–17
Belli C, Cereda S, Anand S, Reni M (2013) Neoadjuvant therapy in resectable pancreatic cancer: a critical review. Cancer Treat Rev 39:518–524
Casadei R, Di Marco M, Ricci C, Santini D, Serra C, Calculli L, D’Ambra M, Guido A, Morselli-Labate AM, Minni F (2015) Neoadjuvant chemoradiotherapy and surgery versus surgery alone in resectable pancreatic cancer: a single-center prospective, randomized, controlled trial which failed to achieve accrual targets. J Gastrointest Surg 19:1802–1812
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Emanuele F Kauffmann, Niccolò Napoli, Francesca Menonna, Sara Iacopi, Carlo Lombardo, Juri Bernardini, Gabriella Amorese, Andrea Cacciato Insilla, Niccola Funel, Daniela Campani, Carla Cappelli, Davide Caramella, and Ugo Boggi have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kauffmann, E.F., Napoli, N., Menonna, F. et al. A propensity score-matched analysis of robotic versus open pancreatoduodenectomy for pancreatic cancer based on margin status. Surg Endosc 33, 234–242 (2019). https://doi.org/10.1007/s00464-018-6301-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6301-2