Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) has increased in popularity in recent years as a definitive bariatric procedure. Despite its growing popularity worldwide, the surgical technique is not well standardized. There is a lack of evidence on the matter of the antrum size and its relation to gastric emptying and weight-loss outcomes. The aim of the study is to evaluate the influence of antrum size over gastric emptying and weight-loss outcomes.
Methods
Twenty-five patients were prospectively randomized according to the distance between the first firing and the pylorus: AR group (antrum resection—2 cm from the pylorus) and AP group (antrum preservation—5 cm from the pylorus). Gastric emptying (%GE) was evaluated by a gastric emptying scintigraphy before surgery, 2 months and 1 year after LSG. Antrum volume was measured using a MultiSlice CT Scan performed 2 months and 1 year after surgery. The percent of excess weight loss (%EWL) was calculated after 1 year follow-up.
Results
At 2 months after LSG the mean %GE was 69.7 ± 18 in the AR group and 72.8 ± 20 in the AP group (p = 0.69). At 1 year it was 66.5 ± 21 and 74.2 ± 16 in the AR and AP groups, respectively (p = 0.30). A significant accelerated gastric emptying was observed at 2 months (p = 0.025) and at 1 year (p = 0.013) in the AP group. Meanwhile in the AR group this increase was not significant (p = 0.12 at 2 months and p = 0.21 at 1 year). Differences regarding the %EWL between groups were no statistically significant (p = 0.74).
Conclusions
After LSG there is a global tendency to an accelerated gastric emptying, although only significant in the antrum preservation group; however, no differences were observed regarding the %EWL between groups after 1 year follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic sleeve gastrectomy (LSG) has increased in popularity in recent years as a definitive bariatric procedure. It originated as the restrictive first-stage procedure in high risk patients before duodenal switch or Roux-en-Y gastric bypass, but nowadays it has been established as a stand-alone bariatric operation due to its safety, feasibility, and remarkable results in terms of weight loss [1, 2].
LSG involves removing approximately 80% of the stomach, mainly the body and fundus, in order to reduce the gastric volume to 75–120 ml. The new narrow tube is designed to decrease appetite by reducing the distensibility of the new stomach thus increasing the intra-luminal pressure producing the sensation of satiety with minimal oral intake [2]. Although the degree of restriction performed seems to play the most important role, the mechanisms of weight loss after LSG are multifactorial; a combination of gastric restriction, hormonal factors, and changes in gastric emptying are involved [3].
To date several studies have focused on the matter of gastric emptying following LSG, showing conflicting results [4,5,6]. It is classically believed that the decrease in food intake is due in part to a delay in gastric emptying [6]. On the contrary, some studies using nuclear medicine techniques with labeled test meals have reported accelerated gastric emptying after LSG, leading to a new paradigm that may shake the previously uniform explanation of restriction as the unique weight-loss mechanism.
Melissas et al. [4, 7] support that accelerated gastric emptying may also enhance satiety signals and reduce oral intake through multiple neurohormonal pathways. Therefore, the mechanisms of weight loss that are seen after LSG are related not only to gastric restriction but also to neurohormonal changes related to gastric resection and altered gastric emptying.
Despite its growing popularity worldwide, the surgical technique is not well standardized and there are still many controversial points such as the length of the pyloric antrum [8], the diameter of the orogastric tube, and the staple line reinforcement, wherein all these techniques may contribute to the final outcome of the surgery [9]. In particular, there is a lack of evidence on the matter of the antrum size and its relation to gastric emptying and weight-loss outcomes.
The aim of this preliminary analysis of data from a randomized prospective study is to assess if LSG with or without antrum preservation (initial firing at 5 or 2 cm from the pylorus) induces changes in gastric emptying and weight-loss outcomes.
Patients and methods
Trial design
This is a preliminary analysis included in a prospective randomized clinical trial (Clinical Trials. gov ID: NCT02144545).
The aim of the study is to evaluate the influence of antrum size over gastric emptying and weight-loss outcomes.
Patients
In our institution, morbidly obese patients that are suitable candidates for bariatric surgery according to the American National Institute of Health are submitted to laparoscopic gastric bypass as standard procedure. Laparoscopic sleeve gastrectomy is proposed in patients meeting the following criteria: younger than 30 years or in the elderly (> 60 years), patients with body mass index (BMI) below 42 kg/m2 or above 55 kg/m2, and patients considered high risk.
Patients with previous gastric surgery or inflammatory bowel disease were excluded. Informed consent was obtained from all patients and the study was approved by the Ethical Committee.
Patients eligible for the inclusion in the trial were prospectively randomized depending on two main criteria: the bougie size (33 vs. 42 French) and the distance between the first firing and the pylorus (2 vs. 5 cm). Four groups were obtained: Group 1 (2 cm from pylorus and 33Fr bougie), Group 2 (5 cm from pylorus and 33Fr bougie), Group 3 (2 cm from pylorus and 42Fr bougie), and Group 4 (5 cm from pylorus and 42Fr bougie).
The following main variables were analyzed preoperatively, 2 months and 1 year after LSG, and compared between the four allocated arms:
-
BMI
-
Gastric volume (MSCT)
-
Gastric emptying (Gastric emptying scintigraphy)
In the literature to date there are no data that allow us to calculate a sample size adapted to the variables evaluated. The number of morbidly obese patients operated annually in our service is 36 and the ratio of LSGs and gastric bypasses performed since the beginning of the laparoscopic bariatric surgery program (2008) is 2:1. Based on these data, we estimated that the number of patients that could be included in a study with an approximate duration of 3 years, is 100.
This is an open-label randomized trial with parallel assignment. Randomization is performed using a random number table. Patients are randomized through a closed envelope that is opened in the operation room once patient is anesthetized. The data to be analyzed are recorded in a specially designed prospective database.
The trial started in October 2013 and has not yet been concluded. Due to the reduced number of cases and because the aim of this preliminary analysis is to evaluate the role of antrum size over the gastric emptying and its relation with weight-loss outcomes, we evaluate only one of the two main criteria: distance between the first firing and the pylorus. Based on this premise, patients are grouped according to the resection of the antrum (AR) or its preservation (AP): Group AR (Groups 1–3, 2 cm from the pylorus) and Group AP (Groups 2–4, 5 cm from the pylorus).
To evaluate gastric emptying we performed a gastric emptying scintigraphy before surgery, 2 months and 1 year after LSG. We also measured the antrum volume using an MSCT Scan, performed 2 months, and 1 year after surgery. The percent of excess weight loss (%EWL) was calculated after 1 year follow-up.
Operative technique
All operations were performed laparoscopically by the same surgical team. The patient was placed in a supine position and in reverse Trendelenburg with splitting legs. Elastic and intermittent pneumatic compressing stockings were applied. The surgeon stood between the patient’s legs, the first assistant to the patient’s left, and the camera assistant to the patient’s right.
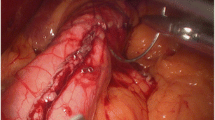
The operation was performed with five trocars. A Harmonic scalpel (UltraCision, Ethicon Endo-Surgery) was used to dissect the greater curvature of stomach and short gastric vessels. After the insertion of a gastric calibration tube (33/42Fr), the pylorus was identified and the section started to 2 cm in the AR group or 5 cm in the AP group, and extending up to the angle of His. Antrum resection was performed using endoscopic linear stapler 60 mm (Echelon Flex, Ethicon Endo-Surgery) with two sequential 3.8 mm cartridges and then 3–4 reloads of 3.5 mm for the upper stomach.
We routinely use SeamGuard (Gore, USA) to reinforce the staple line. A leak test with methylene blue was performed to demonstrate the integrity of the sleeve and a closed suction drain was placed along the staple line.
MultiSlice CT scan
Patients underwent an MSCT for evaluating the antrum volume at 2 months and 1 year after LSG. Each patient was encouraged to take the maximum oral contrast, with the aim of distending the stomach as much as possible. The solution of effervescent sodium bicarbonate and sodium amidotrizoate (Gastrografin®) diluted 3% causes gastric distention. The solution was prepared just before scanogram and helical CT range is set, in order to minimize the loss of effervescent gas. Immediately after oral intake a helical CT was acquired, without intravenous contrast and in a supine position including slices from the carina to the symphysis pubis. Slices should cover the anatomy just above the diaphragmatic hiatus to evaluate possible cranial migration of the sleeve, a complication that has been described in recent publications.
Three different pieces of equipment were used for image acquisition: Philips Brilliance 16 slice, Philips Brilliance iCT 256 slices (field of view 500 mm and max weight 204 kg in both equipments), and in extreme BMI cases Philips Big Bore 16 slices (field of view 700 mm and max weight 295 kg).
We adjusted the characteristic CT techniques (maximum field of view, Kv, and mAs) in order to achieve proper penetration of the ray beam, as we are evaluating patients, especially at baseline, with high BMIs. All cases were supervised by a senior radiologist that validated the images obtained with the aim of getting the highest 3D quality for subsequent processing. The optimal degree of gastric distension was evaluated. All data were collected in DICOM format for further 3D manipulation using Philips IntelliSpace Portal software. Volumetric reconstruction of the air-contrast distended stomach and volume values were obtained and recorded.
The antrum was defined as the volume included between a virtual line joining the incisura angularis and the first staple, above the pylorus (Fig. 1).
Gastric emptying scintigraphy
Patients underwent a gastric empting scintigraphy before, 2 months, and 1 year after LSG. The scintigraphic analysis was performed in the morning after 12 h fasting overnight. Smoking and drugs that may interfere with gastric emptying were discontinued prior to the scintigraphic evaluation. Diabetic patients were studied early in the morning after their normal insulin dosage.
Patients were fed by a standard semi-solid meal with 99mTc (37 MBq)-sulfur colloid-labeled egg-white sandwich along with 200 cc of water. To accurately quantify solid emptying the radiotracer must be tightly bound to the solid meal.
A dual-head gamma camera was used with low-energy collimator and medium resolution. Immediately after oral intake (within first 10 min), the examination proceeded to the stomach detection measurements with the patient in a standing position. A baseline image was performed immediately after ingestion and subsequently, anterior and posterior projections were taken every 15 min for a total of 2 h.
Data were stored to a PC memory and afterwards, the individual images were used to generate an activity decline curve over time with a correction for used radionuclide degradation. We expressed the following parameter: %GE in the 60th minute—percentage of irradiated food evacuation from the stomach within a specified period (normal gastric emptying > 50%).
The antrum of the stomach is responsible for solid gastric emptying. Two phases of solid emptying have repeatedly been demonstrated [10, 11]: an initial delay before emptying begins—the lag phase—and continuous emptying, typically linear. The lag phase is presumably due to the time required for the antrum to grind food into particles small enough to pass through the pylorus and lasts for about 20–30 min. Tougas et al. [12] described a median value for percent gastric retention at 60 min of 24% after an analysis of gastric emptying in 123 volunteers from 11 centers. For this reason, we consider the %GE at 60 min a valuable parameter for the assessment of gastric emptying in our patients.
Statistical analysis
Results are expressed as mean ± standard deviation for continuous variables. Categorical variables are reported using percentages. Correlation between variables was determined by Chi-Square test and differences were established by Analysis of variance. The level of significance was set at p < 0.05. Statistical analysis of data was performed using IBM-SPSS (V22).
Results
From October 2013 to April 2015, 61 consecutive morbidly obese patients were assessed for eligibility but only 36 were enrolled in the trial and randomly allocated into four arms. Patients who did not undergo the scheduled testing during the first year were excluded from the analysis (Fig. 2).
The average age of patients was 52.7 ± 13 years, average body weight was 119.7 ± 16 kg, mean BMI was 44.2 ± 7 kg/m2, and the average of excess weight was 60.6 ± 16 kg. Demographic data of randomized patients are presented in Table 1. Preoperative data were comparable in both groups as regards sex, age, weight, BMI, and overweight.
All patients underwent the LSG procedure without complications. In order to determine whether groups are comparable regarding the bougie size, its influence was analyzed in each group. In the AR group there were 52.6% of patients with 33Fr bougie and 47.4% of patients with 42Fr bougie, while in the AP group there were 54.5% of patients with 33Fr bougie and 45.5% of patients with 42Fr bougie. There were no significant differences in either group with respect to the bougie size (p = 0.9), therefore bougie size was discarded as a confounding factor.
In relation to the antrum volume measured by MSCT, as expected we observed a significantly lower volume in the AR group at 2 months after surgery (11.8 ± 10 ml in AR group and 22.1 ± 12 ml in AP group, p = 0.04) and at 1 year (7.5 ± 5 ml vs. 29.1 ± 16 ml respectively, p = 0.001) (Fig. 3).
Scintigraphic examinations were realized within the stated periods (preoperatively, 2 months, and 1 year after LSG). In the AR group the mean preoperative percent clearance of semi-solid meal at 60 min was 55.8 ± 22 and in the AP group it was 52.7 ± 24 (p = 0.74). At 2 months it was 69.7 ± 18 in the AR group and 72.8 ± 20 in the AP group (p = 0.69). At 1 year it was 66.5 ± 21 in the AR group and 74.2 ± 16 in the AP group (p = 0.30) (Table 2).
However, if we analyze the evolution of each group (Fig. 4) we see a significant accelerated gastric emptying at 2 months (p = 0.025) and at 1 year (p = 0.013) in the AP group. Meanwhile in the AR group this increase is not significant (p = 0.12 at 2 months and p = 0.21 at 1 year).
Finally, in this preliminary analysis, we did not find differences regarding the %EWL between groups at 1 year after surgery (54.9 ± 15 in the AR group and 57.7 ± 23 in the AP group, p = 0.74).
Discussion
Nowadays sleeve gastrectomy is established worldwide as a stand-alone bariatric procedure. Many publications have documented significant weight loss in spite of a lack of standardization regarding the surgical technique. The degree of antral resection is a common controversial issue among the most experienced surgeons. Some authors support antral preservation and start their resections 6 cm or more from the pylorus with the aim of preserving the contractile function and thus improving gastric emptying. Other surgeons performed a radical resection close to the pylorus to increase the restrictive effect and to achieve better weight-loss outcomes [13, 14].
To date several studies have focused on the matter of the antrum size in relation to gastric emptying, showing conflicting results. Braghetto et al. [5] showed an accelerated gastric emptying to liquids and solids in 20 patients 2–3 months after LSG with 2 cm of antral length compared to a normal weight control group. Melissas et al. [4] also found a significantly accelerated gastric emptying for solid meals at 6 months after LSG with 7 cm of antral length. On the contrary, in a prospective analysis of 21 patients undergoing antrum preservation and a scintigraphic examination before and 3 months after LSG, Bernstine et al. [6] did not find significant changes in gastric emptying.
Baumann et al. [15] introduced a new study tool to evaluate gastric motility in patients with antrum preservation. They performed MRI in five patients before, 6 days, and 6 months after LSG. They showed for the first time that gastric emptying after an antrum preserving sleeve gastrectomy was directly linked to the function of an accelerated antrum since the sleeve itself showed no propulsive peristalsis. This is discordant with respect to other studies that showed an accelerated gastric emptying after antrum complete resection [5].
Regarding the weight-loss outcomes depending on the antrum size, two recent studies report better weight-loss outcomes with the section close to pylorus. Obeidat et al. [14] reported in a sample of 110 patients that the radical antral resection safely potentiated the restrictive effect with significantly better weight loss in the first 2 postoperative years, compared to patients undergoing antrum preservation. In the same way Abdallah et al. [16] reported significantly better weight loss by increasing the size of the resected antrum. On the contrary, our study doesn’t find significant differences with respect to weight-loss outcomes (%EWL) between groups at 1 year of follow-up (54.9 ± 15 in AR group and 57.7 ± 23 in AP group, p = 0.74).
Our study focuses particularly on the postoperative volume antrum to determine differences in gastric emptying after LSG at 2 or 5 cm from the pylorus and its influence on the %EWL at 1 year postoperatively. A similar study by Michalsky et al. [17] found that four patients undergoing radical resection of the antrum had an increase in gastric emptying 3 months after LSG but did not find differences regarding the weight-loss outcomes after 12-month monitoring compared to patients with antrum preservation, without studying the gastric emptying in this sample of patients.
In our study we report a significantly higher antrum volume in the AP group compared to patients with antrum resection, this is basically a reflection of our adherence to intraoperative measures and these volumes remain practically invariable at 1 year after LSG (Fig. 2).
Regarding the gastric emptying we observe a tendency to an accelerated gastric emptying after LSG independently of the antrum size. This increase is only significant in the AP group, although the difference compared to the AR group at 2 months and at 1 year is not significant. Otherwise, current outcomes do not show evidence that the antrum size and variations in gastric emptying cause a difference in weight-loss outcomes between groups. However, our sample size is small and the follow-up interval is too short to draw clear conclusions.
In general terms, we think that surgically manipulating the pyloric antrum area with its resection, more or less wide, results in an increase of gastric emptying in the vast majority of patients, and in concordance with studies by Braghetto et al. and Melissas et al. we think that changes in the acceleration of stomach evacuation ability, along with the restrictive and hormonal effect, may be behind the weight-loss mechanism in patients undergoing LSG.
Some limitations of the current study should be considered. This is a preliminary study forming part of a prospective analysis of four groups: Group 1 (2 cm from pylorus and 33Fr bougie), Group 2 (5 cm from pylorus and 33Fr bougie), Group 3 (2 cm from pylorus and 42Fr bougie), and Group 4 (initial firing at 5 cm and 42Fr bougie). With the complete information that will be obtained from these four groups we expect to be able to clarify the most debated issues about LSG, and to analyze gastric emptying, presence of gastroesophageal reflux, and weight-loss outcomes in the long term.
References
Shi X, Karmali S, Sharma AM, Birch DW (2010) A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg 20:1171–1177
Lee CM, Cirangle PT, Jossart GH (2007) Vertical gastrectomy for morbid obesity in 216 patients: report of two-year results. Surg Endosc 21:1810–1816
Papailou J, Albanopoulos K, Toutouzas KG, Tsigris C, Nikiteas N, Zografos G (2010) Morbid obesity and sleeve gastrectomy: how does it work? Obes Surg 20:1448–1455
Melissas J, Koukouraki S, Askoxylakis J, Stathaki M, Daskalakis M, Perisinakis K, Karkavitsas N (2007) Sleeve gastrectomy—a restrictive procedure? Obes Surg 17:57–62
Braghetto I, Davanzo C, Korn O, Csendes A, Valladares H, Herrera E, Gonzalez P, Papapietro K (2009) Scintigraphic evaluation of gastric emptying on obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg 19:1515–1521
Bernstine H, Yehoshua RT, Groshar D, Beglaibter N, Shikora S, Rosenthal RJ, Rubin M (2009) Gastric emptying is nor affected by sleeve gastrectomy–scintigraphic evaluation of gastric emptying after sleeve gastrectomy without removal of the gastric antrum. Obes Surg 19:293–298
Melissas J, Daskalakis M, Koukouraki S, Askoxylakis I, Metaxari M, Dimitriadis E, Stathaki M, Papadakis JA (2008) Sleeve gastrectomy—a “food limiting” operation. Obes Surg 18:1251–1256
Nakane Y, Michiura T, Inoue K, Sato M, Nakai K, Yamamichi K (2002) Length of the antral segment in pylorus-preserving gastrectomy. Br J Surg 89:220–224
Ferrer-Márquez M, Belda-Lozano R, Ferrer-Ayza M (2012) Technical controversies in laparoscopic sleeve gastrectomy. Obes Surg 22:182–187
Camilleri M, Malagelada JR, Brown ML, Becker G, Zinsmeister AR (1985) Relation between antral motility and gastric emptying of solids and liquids in humans. Am J Physiol 249:G580–G585
Siegel JA, Urbain JL, Adler LP, Charkes ND, Maurer AH, Krevsky B, Knight LC, Fisher RS, Malmud LS (1988) Biphasic nature of gastric emptying. Gut 29:85–89
Tougas G, Eaker EY, Abell TL, Abrahamsson H, Boivin M, Chen J, Hocking MP, Quigley EM, Koch KL, Tokayer AZ, Stanghellini V, Chen Y, Huizinga JD, Rydén J, Bourgeois I, McCallum RW (2000) Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol 95:1456–1462
Baltasar A, Serra C, Pérez N, Bou R, Bengochea M, Ferri L (2005) Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg 15:1124–1128
Obeidat F, Shanti H, Mismar A, Albsoul N, Al-Qudah M (2005) The magnitude of antral resection in laparoscopic sleeve gastrectomy and its relationship to excess weight loss. Obes Surg 25:1928–1932
Baumann T, Kuesters S, Grueneberger J, Marjanovic G, Zimmermann L, Schaefer AO, Hopt UT, Langer M, Karcz WK (2011) Time-resolved MRI after ingestion of liquids reveals motility changes after laparoscopic sleeve gastrectomy—preliminary results. Obes Surg 21:95–101
Abdallah E, El Nakeeb A, Yousef T, Abdallah H, Abd Ellatif M, Lofty A, Youssef M, Elganash A, Moatamed A, Morshed M, Farid M (2014) Impact of extent of antral resection on surgical outcomes of sleeve gastrectomy for morbid obesity (a prospective randomized study). Obes Surg 24:1587–1594
Michalsky D, Dvorak P, Belacek J, Kasalicky M (2013) Radical resection of the pyloric antrum and its effect on gastric emptying after sleeve gastrectomy. Obes Surg 23:567–573
Acknowledgements
Authors appreciate research contributions by European Association for Endoscopic Surgery (EAES Research Grant Project 2011) and the Karl Storz EAES Award (Amsterdam, 2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Meritxell Garay, Carmen Balagué, Carlos Rodríguez-Otero, Berta Gonzalo, Anna Domenech, Juan Carlos Pernas, Ignasi J. Gich, Sonia Fernández-Ananín and Eduardo M. Targarona have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Garay, M., Balagué, C., Rodríguez-Otero, C. et al. Influence of antrum size on gastric emptying and weight-loss outcomes after laparoscopic sleeve gastrectomy (preliminary analysis of a randomized trial). Surg Endosc 32, 2739–2745 (2018). https://doi.org/10.1007/s00464-017-5972-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5972-4