Abstract
Background and aims
Expeditious endoscopic retrograde cholangiopancreatography (ERCP) in acute cholangitis with biliary decompression is associated with better outcomes. In this study, we evaluated the temporal trends of ERCP utilization and healthcare outcomes among patients hospitalized with acute cholangitis due to choledocholithiasis (CDC) from 1998 to 2012.
Methods
We identified patients with a combined diagnosis of cholangitis and choledocholithiasis from the national inpatient sample database. The temporal trends of ERCP usage and outcomes were analyzed. Based on timing of the procedure, we arbitrarily divided ERCPs into urgent (<24 h), early(24–48 h), and delayed ERCP(>48 h) groups. In addition, trends in length of stay (LOS), hospital charges, and in-hospital mortality rates were evaluated.
Results
In-patient admissions for CDC increased by 105.7%. Overall ERCP rate also increased significantly from 66.5 ± 2.3% in 1998 to 80.3 ± 0.93% in 2012, particularly after 2006–2007. There was a significant increase in proportion of urgent and early ERCPs. In the early ERCP group, there was a significant decrease in LOS (6.4 ± 0.43 days in 1998 to 5.8 ± 0.24 days in 2012) and mortality rate (2.4 ± 1.4% in 1998 to 0.33 ± 0.33% in 2012). Hospital charges increased in all ERCP groups, but most significantly in delayed ERCP group ($20,448 ± 1611 in 1998 to $90,566 ± 6122 in 2012).
Conclusion
In-patient admissions for CDC and ERCP rates have increased significantly, particularly evident after 2006–2007. This may be attributed to increasing incidence of gallstones and wider implementation of Tokyo guidelines for the management of acute cholangitis. In-hospital morality and LOS reduced significantly in early ERCP group, whereas hospital charges increased most significantly in delayed ERCP group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Prior to the advent of endoscopic retrograde cholangiopancreatography (ERCP), emergency surgical exploration of the common bile duct was commonly performed for the treatment of patients with cholangitis due to choledocholithiasis (CDC). A randomized control trial in 1992 [1] conclusively demonstrated that ERCP was safe and effective treatment of CDC, with significantly lower morbidity and mortality as compared to surgery. After this landmark study, wide spread availability and better outcomes resulted in increasing utilization of ERCP for CDC management [2].
Once the pivotal role of ERCP was established, the focus shifted on to determine the optimal time to perform ERCP in patients with CDC. Tokyo guidelines released in 2006 emphasized on elective biliary drainage in mild, early drainage in moderate, and urgent drainage in severe cases of cholangitis [3,4,5]. Studies have also analyzed the impact of timing of ERCP and a general trend of improved healthcare outcomes was noted when ERCP was performed sooner rather than later in patients with acute cholangitis [6,7,8,9,10].
In this national inpatient sample (NIS) database study, we assessed the trends of ERCP utilization in patients with CDC from 1998 to 2012 in the United States. Since the timing of ERCP was shown to impact the outcomes, we arbitrarily divided the ERCPs into three groups i.e., urgent (<24 h), early (24–48 h), and delayed ERCP (>48 h). Trends of important healthcare outcomes such as length of stay (LOS), in-hospital mortality, and inflation-adjusted costs were also analyzed for the three groups.
Methods
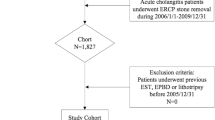
Data on hospital admissions of all patients were extracted from the NIS database from 1998 to 2012. Patients were classified as having cholangitis and choledocholithiasis by querying all available primary and secondary diagnoses for the ICD-9-CM codes corresponding to cholangitis (576.1) and choledocholithiasis (574.5). In addition, all procedural codes were queried to identify if ERCP was performed or not (51.10, 51.11, 52.13, 52.92, 51.86, 52.97, 51.88, 52.94, 51.84, 52.98, 51.87, 52.93, 51.85, 51.14, 52.14, 51.64, 52.21, 51.69, or 51.15).
Timing of ERCP
ERCPs were arbitrarily divided into three groups based on the timing of ERCP: (1) ERCPs performed within 24 h of admission (urgent ERCP), (2) between 24 and 48 h after admission (Early ERCP), and (3) after 48 h of admission (Delayed ERCP). If multiple ERCPs were performed during the same hospital admission, they were classified based on when the first procedure was done.
Recorded data
In addition to ERCP details as above, demographic data including age, sex, race, and comorbidities were collected. Payer status for all the admissions was also recorded. In terms of hospital characteristics, size (small medium and large) and location (rural and urban) were reviewed. Hospital charges were defined as the amount the hospital charged for the entire hospital stay. Patients with missing information on LOS, charges, or in-hospital mortality were excluded from the analysis. The HCUP Comorbidity Software was used to generate Elixhauser comorbidities from ICD-9 CM diagnosis codes (https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp). A modified Charlson Comorbidity Index (CCI) was calculated using the NIS disease severity measure files [11]. Costs were adjusted for inflation to 2013 dollars using the gross domestic product deflator [12].
Statistical analysis
Survey procedures were used to obtain yearly discharge frequencies, mean LOS, and costs. The trend weights provided by NIS for the years 1998–2011 which are consistent with the redesigned NIS (beginning in 2012) were used (https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp). The temporal trends of ERCP usage rates in CDC patients were assessed by linear and polynomial regression. In addition, trends in LOS, hospital charges, and in-hospital mortality rates were evaluated for each ERCP group. Poisson regression was used to model rates and linear regression was used to model LOS and costs. The most appropriate functional form for the trend was assessed by examination of regression diagnostic plots. All analyses were performed using SAS (version 9.4, The SAS Institute, Cary, NC) and a p < 0.05 was considered statistically significant.
Results
From a total of 103,998 CDC patients, 77,323 underwent ERCP at any given point in time during the hospitalization over a period of 1998–2012. Out of these, urgent ERCPs (<24 h) were N = 45,733; early ERCPs (24–48 h) were N = 13,916 and delayed ERCPs (>48 h) were N = 17,674.
Patient and hospital characteristic for the years 1998 and 2012 are shown in Table 1. Average age of patients undergoing ERCP was 71.5 ± 0.69 years and 70.5 ± 0.42 years in 1998 and 2012, respectively. CDC cases increased from 17.2 to 21.9% in the 45–64 years age group, and however reduced from 51.6 to 46.8% in the 65–84 years age group, indicating a rising prevalence of CDC in younger patients in 2012. A proportionate change in ERCP rates was also noted. Females were affected more frequently than men and highest incidence was noted in Caucasians followed by Hispanics and African Americans. The ERCP rate reduced from 66.9 to 64.7% in Caucasians, whereas it increased from 8.9 to 11.9% in Hispanics from 1998 to 2012. A significantly higher CCI was noted for patients in 2012 as compared to 1998 (4.1 ± 0.06 vs. 3.5 ± 0.08). Medicare remained the primary payer for majority of the patients. Payment by Medicaid increased from 5.9 to 8.4%, whereas the rate of private insurance payment decreased from 22.6 to 16.7% from 1998 to 2012. In terms of hospital characteristics, highest rate of ERCP was noted in large hospitals and those located in urban areas.
Trends of inpatient admissions for CDC: The inpatient admissions for CDC increased by 105.7% over the span of 15-year study period, increasing from 5070 patients in 1998 to 10,340 patients in 2012 (Table 2; Fig. 1). On further assessment, it was noted that the increase from 1998 to 2004 was very modest (rising from 5070 cases in 1998 to 6006 cases in 2004). However a more significant increase was noted from 2005 to 2012 (rising from 6592 cases in 2005 to 10,430 cases in 2012).
Trends of ERCP utilization
The overall rate of ERCP increased from 66.5 ± 2.3% in 1998 to 80.3 ± 0.93% in 2012 (Table 2; Fig. 2). It was further noted that ERCP rate remained relatively stable from 1998 (66.5 ± 2.3) to 2005 (65.5 ± 2.3). However, there was a progressive increase in ERCP rate from 2006 to 2012 (69.5 ± 2.1% in 2006 to 80.3 ± 0.93% in 2012).
Trends of ERCP timing
Rate of urgent and early ERCP increased over the study period, while there was no significant change in delayed ERCP rate (Table 2; Fig. 3). Rate of early ERCP remained relatively stable from 1998 (38.6 ± 2.1%) to 2006 (38.9 ± 1.9%); however, a progressive rise was noted since 2006–2007, approaching a rate of almost 50% by 2012.
Trends of length of stay
LOS has declined significantly in the early ERCP group (6.4 ± 0.43 days in 1998 to 5.8 ± 0.24 in 2012) (Table 3; Fig. 4). LOS was shortest among the urgent ERCP group and longest among the delayed ERCP groups. This trend was maintained all throughout the study period without a significant change.
Trends of in-hospital mortality rate
In-hospital mortality rates have declined significantly in the early ERCP group (2.4 ± 1.4% in 1998 to 0.33 ± 0.33% in 2012). A trend towards reduced mortality in the urgent ERCP group and increased mortality in the delayed ERCP group was noted over the study period; however, it did not reach statistical significance (Table 3; Fig. 5).
Trends of hospital costs
Discussion
Gallbladder disease from gallstones constitutes a significant health problem in the United States with approximately 20 million Americans estimated to have gallbladder disease [13]. This translates into a healthcare economic burden of approximately $6.2 billion/year [14]. An aging population, use of ultrasonographic survey, rising incidence of obesity, and metabolic syndrome have resulted in a higher prevalence of gall bladder disease in the United States [15,16,17,18,19]. In western countries, most cases of choledocholithiasis result from passage of gallstones into the common bile duct (CBD) from gall bladder [20]. Hence, increasing prevalence of gallstones has likely resulted in higher incidence of choledocholithiasis. This has subsequently resulted in rising incidence of acute cholangitis due to choledocholithiasis. Prior to 2006, standard diagnostic criteria for acute cholangitis did not exist. An international consensus meeting was held in Tokyo in 2006, where criteria were laid out for diagnosing acute cholangitis based on a systematic literature review and the consensus of experts [3,4,5]. These guidelines were widely implemented since its inception, likely resulting in higher identification of acute cholangitis cases. In our study, the inpatient admissions for CDC have nearly doubled over the span of 15 years, increasing from 5070 patients in 1998 to 10,340 patients in 2012. On further assessment, it was noted that the increase from 1998 to 2004 was very modest (rising from 5070 cases in 1998 to 6006 cases in 2004). However, a sharp increase was noted from 2005 to 2012 (rising from 6592 cases in 2005 to 10,430 cases in 2012). Apart from increasing prevalence of gall bladder disease, this finding can most likely be explained by increasing implementation of Tokyo guidelines released in 2006–2007 with more number of cases of acute cholangitis being diagnosed (Table 2; Fig. 1).
It has been estimated that approximately 500,000 ERCPs are performed annually in the United States [21]. The use of ERCP as a diagnostic tool has steadily declined with the advent of less-invasive imaging modalities like endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP). However, the use of ERCP as a therapeutic modality continues to rise. In a study by Jamal et al. [19], the age adjusted rate for therapeutic ERCPs in men and women was 13.74 and 15.61/100,000 in 1988–1990, respectively, which increased to 38.76 and 43.75 in 2000–2002. In a population-based study from Mayo Clinic, utilization of therapeutic ERCP increased from 58 to 104.8 ERCPs/100,000 persons/year from 1997 to 2006. In this study, ERCP was performed for a biliary indication in 80% of the cases and the most common indication for ERCP was choledocholithiasis (47%) [22]. Similarly, in a population-based study from Canada, the rate of therapeutic ERCP increased from 0.42/10,000 in 1987 to 12.79/10,000 in 2009, where the most common indications for ERCP were choledocholithiasis, cholangitis, and bile leak [23]. Hence, it can be noted from above studies that the rate of therapeutic ERCPs has increased significantly over the years and that the majority of ERCPs are being performed for biliary indications like choledocholithiasis and cholangitis.
Our study shows similar findings with the overall rate of ERCP for CDC increasing from 66.5 ± 2.3% in 1998 to 80.3 ± 0.93% in 2012. It was further noted that the ERCP rate remained relatively stable from 1998 (66.5 ± 2.3) to 2005 (65.5 ± 2.3); however, it increased progressively from 2006 onwards (69.5 ± 2.1% in 2006 to 80.3 ± 0.93% in 2012). This increased utilization of ERCP can again be attributed to the increasing prevalence of gall bladder disease [15,16,17,18,19] and higher number of cases of acute cholangitis being diagnosed after implementation of Tokyo guidelines in 2006–2007 [3,4,5]. Also since the inception of laparoscopic cholecystectomy, there has been a significant increase in pre-operative or post-operative ERCPs for treatment of choledocholithiasis with a concomitant reduction in the cases of direct operative exploration of the CBD [24].
In our study, rates of ERCP within 24 h (urgent) and between 24 and 48 h (early) have been on the rise. On further assessment, a significantly higher increase was noted in urgent ERCPs (11% increase, from 38.6 ± 2.1% in 1998 to 49.5 ± 1.2% in 2012) as compared to early ERCPs (3% increase, from 11.8 ± 1.09 in 1998 to 14.4 ± 0.81 in 2012). Chak et al. [6] reported that in patients with cholangitis, the length of stay (LOS) was significantly lower when ERCP was performed within 24-h admission. In another study by Khashab et al. [7] (n = 90), it was noted that delayed ERCP (greater than 72 h) was associated with prolonged hospital stay, increased cost of hospitalization, and worse composite end points (death, persistent organ failure and/or intensive care unit stay). Delaying ERCP for more than 48 h was associated with increased 30-day readmission rates in another study [10]. LOS, 30-day mortality and 30-day readmission rates are important healthcare metrics used to assess quality of care and provider reimbursement. It is possible that based on above outcomes, physicians are considering earlier ERCPs in the management of patients with acute cholangitis.
Assessing the severity of acute cholangitis is also of paramount importance as it guides the treatment and dictates the timing of the biliary drainage. First ever guidelines for severity assessment of acute cholangitis were put forth in 2006–2007 and patients were classified as having mild (grade I), moderate (grade II), or severe (grade III) disease based on the response to initial treatment and the presence or absence of end organ dysfunction. Mild cases respond well to medical treatment and biliary drainage can be performed electively, whereas early biliary drainage is required for those with moderate cholangitis. Patients with acute cholangitis and organ failure are classified as having severe cholangitis and require urgent biliary drainage [3,4,5].
In our study, we further noted that the rate of ERCP within 24 h remained relatively stable from 1998 (38.6 ± 2.1%) to 2006 (38.9 ± 1.9%). However, a progressive rise was noted since 2006, approaching a rate of almost 50% by 2012 (Fig. 3). This can be attributed to the implementation of Tokyo guidelines published in 2006–2007, which likely resulted in improved severity-based classification of patients and performance of earlier ERCPs in those with moderate or severe cholangitis.
The LOS has declined significantly for patients undergoing ERCP between 24 and 48 h. It reduced from 6.4 ± 0.43 days in 1998 to 5.8 ± 0.24 days in 2012. LOS was shortest when ERCP was performed within 24 h and longest when performed after 48 h. This trend was maintained all throughout the study period without a significant change (5.1 ± 0.19 days for ERCP <24 h and 9.7 ± 0.59 for ERCP >48 h in 2012).
In-hospital mortality rate has decreased from 2.4 ± 1.4% in 1998 to 0.33 ± 0.33% in 2012, among patients with ERCP between 24 and 48 h. A trend towards reduced mortality was seen in patients who underwent urgent ERCP group (<24 h) and increased mortality in delayed ERCP group (>48 h). Urgent intervention in all patients with acute cholangitis is neither necessary nor always feasible. However, it is important to realize that patients with severe disease could have a rapid downhill clinical course and endoscopic biliary drainage in patients with septicemic shock entails a high mortality rate of 4.7–10% [1, 25,26,27].
Inflation-adjusted hospital charges for CDC patients undergoing ERCP have been on the increase for all ERCP groups. The most striking rise was seen in delayed ERCP group, where the inflation-adjusted cost increased by 343.9% over the study period. Based on the above results, it may be inferred that delaying for ERCP for >48 h showed a trend towards increased morbidity and mortality, which further translated into significantly higher LOS and hospital costs. Although the severity of disease and available resources dictates the timing of ERCP drainage, the time frame of 24–48 h for biliary drainage can be thought to represent a “sweet spot.” This allows for initial diagnosis, severity assessment and reassessment, resuscitation, and hemodynamic stabilization within first 24 h. This strategy also helps in decreasing LOS, hospital costs, 30-day readmission rates, and importantly in-hospital mortality.
This is a retrospective study and thus subject to the inherent limitations of retrospective design. The NIS database uses administrative ICD-9 codes and does not control for errors during data entry. This study included very specific patient population-those with acute cholangitis secondary to choledocholithiasis, and hence does not take into account, cholangitis due to other etiologies, such as benign or malignant strictures. However choledocholithiasis represents the most common cause of cholangitis and hence this study can be considered to be applicable to most patients in the community. These data do not include outpatient encounters; however, it is unlikely to affect the generalizability of our results, since patients with CDC are rarely managed on an outpatient basis.
Strengths of our study include data from NIS, which is one of the largest inpatient medical databases in the United States, allowing for recruitment of a large number of patients and higher study power. Selection, participation, and reporting bias are minimal given the large sample size. NIS is representative of entire US population and hence the findings from our study can be generalized to the common patient population in the country.
In conclusion, our study has longitudinally analyzed the important health care metrics in CDC patients undergoing ERCP over a span of 15 years. It also evaluated the outcomes in a broader frame of timing of ERCP, (<24, 24–48, and >48 h) rather than simple dichotomous timing (early vs. late) as in some previous studies. We found that the prevalence of CDC has doubled during the study period. This was accompanied by an increase in overall ERCP rates and especially urgent ERCP in <24 h and early ERCP between 24 and 48 h. The rise in CDC and ERCP rate was particularly evident after 2006–2007, correlating with release of first Tokyo guidelines for management of acute cholangitis. In terms of healthcare outcomes, ERCP within 24–48 h resulted in significant reduction in LOS and in-hospital mortality. Inflation-adjusted hospital charges increased for all ERCP groups; however, the most striking increase occurred in ERCP >48 h group, where costs increased by 343.9% over the study period. Updated guidelines [28] for management of acute cholangitis are recently published in 2013 and its impact on above outcomes remains to be seen.
References
Lai EC, Mok FP, Tan ES et al (1992) Endoscopic biliary drainage for severe acute cholangitis. NEJM 326(24):1582–1586
McNabb-Baltar J, Trinh QD, Barkun AN (2013) Biliary drainage method and temporal trends in patients admitted with cholangitis: a national audit. Can J Gastroenterol 27(9):513–518
Wada K, Takada T, Kawarada Y et al (2007) Diagnostic criteria and severity assessment of acute cholangitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg 14(1):52–58
Miura F, Takada T, Kawarada Y et al (2007) Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg 14(1):27–34
Takada T, Kawarada Y, Nimura Y et al (2007) Background: Tokyo guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Surg 14(1):1–10. doi:10.1007/s00534-006-1150-0
Chak A, Cooper GS, Lloyd LE et al (2000) Effectiveness of ERCP in cholangitis: a community-based study. Gastrointest Endosc 52(4):484–489
Khashab MA, Tariq A, Tariq U et al (2012) Delayed and unsuccessful endoscopic retrograde cholangiopancreatography are associated with worse outcomes in patients with acute cholangitis. Clin Gastroenterol Hepatol 10(10):1157–1161
Navaneethan U, Njei B, Hasan M et al (2015) Su1618 timing of ERCP and outcomes of patients with acute cholangitis and choledocholithiasis: a nationwide population based study. Gastrointest Endosc 81(5):AB354
Parikh ND, Issaka R, Lapin B et al (2014) Inpatient weekend ERCP is associated with a reduction in patient length of stay. Am J Gastroenterol 109(4):465–470
Navaneethan U, Gutierrez NG, Jegadeesan R et al (2013) Delay in performing ERCP and adverse events increase the 30-day readmission risk in patients with acute cholangitis. Gastrointest Endosc 78(1):81–90
Fineberg SJ, Ahmadinia K, Patel AA et al (2013) Incidence and mortality of cardiac events in lumbar spine surgery. Spine 38(16):1422–1429
Everhart JE, Khare M, Hill M et al (1999) Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 117(3):632–639
Everhart JE, Ruhl CE (2009) Burden of digestive diseases in the United States: overall and upper gastrointestinal diseases. Gastroenterology 136:376–386
Stinton LM, Shaffer EA (2012) Epidemiology of Gallbladder Disease: Cholelithiasis and Cancer Gut Liver 6(2):172–187
Barbara L, Sama C, Morselli-Labate AM et al (1987) A population study on the prevalence of gallstone disease: The Sirmione study. Hepatology 7:913–917
Ford ES, Giles WH, Dietz WH (2002) Prevalence of the metabolic syndrome among US adults: findings from the third national health and nutrition examination survey. JAMA 287:356–359
Friedman GD, Kannel WB, Dawber TR (1966) The epidemiology of gallbladder disease: observations in the Framingham study. J Chronic Dis 19:273–292
Jamal M, Yoon EJ, Saadi A et al (2007) Trends in the utilization of endoscopic retrograde cholangiopancreatography (ERCP) in the United States. Am J Gastroenterol 102(5):966–975
Arain M, Freeman L (2017) Choledocholithiasis: clinical manifestations, diagnosis, and management. https://www.uptodate.com/contents/choledocholithiasis-clinical-manifestations-diagnosis-and-management/contributors
Andriulli A, Loperfido S, Napolitano G et al (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102(8):1781–1788
Coelho-Prabhu N, Shah ND, Van-Houten H et al (2013) Endoscopic retrograde cholangiopancreatography: utilisation and outcomes in a 10-year population-based cohort. BMJ Open 3:e002689
Moffatt DC, Yu BN, Yie W et al (2014) Trends in utilization of diagnostic and therapeutic ERCP and cholecystectomy over the past 25 years: a Population-based study. Gastrointest Endosc 79(4):615–622
Barwood NT, Valinsky LJ, Hobbs MS et al (2002) Changing methods of imaging the common bile duct in the laparoscopic cholecystectomy era in Western Australia: implications for surgical practice. Ann Surg 235:41–50
Leung JWC, Chung SCS, Sung JJY et al (1989) Urgent endoscopic drainage for acute suppurative cholangitis. Lancet 1:1307–1309
Hui CK, Lai KC, Yuen MF et al (2001) Acute cholangitis-predictive factors for emergency ERCP. Aliment Pharmacol Ther 15(10):1633–1637
Lee JG (2009) Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol. 6(9):533–541
Okamoto K, Takada T, Strasberg S et al (2013) TG13 management bundles for acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20:55–59
Author contribution
Malav P. Parikh contributed to the study concept and design, acquisition of data, literature review, initial paper writing, paper review, and approval of final version. Niyati M. Gupta contributed to the literature review, manuscript review, and approval of final version. Rocio Lopez contributed to acquisition of data, statistical analysis, interpretation of data, and approval of final version. Prashanthi N. Thota contributed to the literature review, manuscript review, and approval of final version. Madhusudhan R. Sanaka contributed to the literature review, manuscript review, and approval of final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Malav P. Parikh, Dr. Niyati M. Gupta, Rocio Lopez, Dr. Prashanthi N. Thota, and Dr. Madhusudhan R. Sanaka have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Parikh, M.P., Gupta, N.M., Thota, P.N. et al. Temporal trends in utilization and outcomes of endoscopic retrograde cholangiopancreatography in acute cholangitis due to choledocholithiasis from 1998 to 2012. Surg Endosc 32, 1740–1748 (2018). https://doi.org/10.1007/s00464-017-5856-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5856-7