Abstract
Background
Gastric cancer treatment guidelines recommend additional surgery as the standard treatment for lesions for which endoscopic submucosal dissection (ESD) is not indicated. However, the incidence of lymph-node metastasis is low in most patients.
Methods and materials
The study comprised 231 patients (231 lesions) who underwent ESD for early gastric cancer (EGC) in our hospital from September 2002 through March 2015 and were found to have lesions for which endoscopic treatment is not indicated on histopathological evaluation after ESD. The patients were divided into the additional operation group and the follow-up group, and long-term outcomes were studied retrospectively. Risk factors for metastasis and recurrence were also studied (capture rate, 98.7%).
Results
The median follow-up was 48 months. There were 174 men and 57 women with a median age of 72 years. The additional operation group comprised 118 patients, and the follow-up group comprised 113 patients. The rates of 5-year cause-specific survival and 5-year overall survival were significantly higher in the additional operation group (100 and 96.0%, respectively) than in the follow-up group (92.6 and 73.3%, respectively; p = 0.010, p < 0.001). In the follow-up group, 5 patients (4.4%) died of gastric cancer (p = 0.021). Among elderly patients 75 years or older, long-term outcomes did not differ significantly between the groups. Sixteen patients had metastasis or recurrence, and the presence of lymphatic involvement was an independent risk factor for metastasis, recurrence, or both (p = 0.003; odds ratio 10.594; 95% confidence interval 2.294–48.927).
Conclusions
In patients with EGC who are confirmed to have lesions for which endoscopic treatment is not indicated on histopathological evaluation after ESD, additional surgery should be aggressively performed if the patient can tolerate such treatment. In elderly patients aged 75 years or older and patients with serious underlying diseases, follow-up observation was suggested to be one option in patients who give informed consent after receiving an explanation of the risk of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In Japan, gastric cancer is the second leading cause of death, coming after lung cancer. Internationally as well, gastric cancer remains one of the leading causes of death [1].
There has been a remarkable increase in the use of endoscopic submucosal dissection (ESD) for the treatment of early gastric cancer (EGC). The guidelines issued by the Japan Gastroenterological Endoscopy Society (JGES) and Japanese Gastric Cancer Association (JGCA) state that ESD is absolutely indicated for the treatment of differentiated-type EGC without ulcerative findings [UL(−)] in which the depth of invasion is clinically diagnosed as T1a (tumor confined to the mucosa) and the tumor diameter is <2 cm [2, 3]. These guidelines also include the following categories of EGC with a clinical diagnosis of T1a in the expanded indications for EGC: (a) differentiated-type, without ulcerative findings [UL(−)], >2 cm in diameter; (b) differentiated-type, with ulcerative findings [UL(+)], ≤3 cm in diameter; and (c) undifferentiated-type, without ulcerative findings [UL(−)], ≤2 cm in diameter [4] (Table 1). The possibility of expanding the indications for endoscopic treatment has been considered [5,6,7,8]. On the other hand, we sometimes encounter patients who undergo ESD for EGC, but are found to have lesions for which endoscopic treatment is not indicated on histopathological evaluation after ESD.
The gastric cancer treatment guidelines recommend additional surgery as the standard treatment for such lesions. In fact, however, the incidence of lymph-node metastasis is low in most patients [3, 9]. To date, few studies have examined risk factors for metastasis and recurrence in patients who underwent ESD for lesions for which endoscopic treatment was not indicated.
We retrospectively studied long-term outcomes and risk factors for metastasis and recurrence in patients who underwent ESD for EGC and were given a diagnosis of lesions for which endoscopic treatment was not indicated on histopathological evaluation.
Among patients who are 75 years or older, the majority have multiple diseases and functional disorders that would influence daily living [10]. We therefore additionally studied long-term outcomes in patients 75 years or older.
Patients and methods
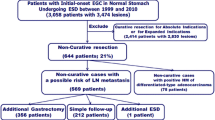
From September 2002 through March 2015, ESD was performed in 1587 consecutive patients (1984 lesions) with EGC in the Department of Gastroenterology, Kitasato University School of Medicine. After excluding patients with a gastric tube or remnant stomach, the study group comprised 1547 patients with EGC who had 1919 lesions. On histopathological examination, there were 1092 guideline lesions in 922 patients, 596 expanded-indication lesions in 553 patients, and 231 lesions for which ESD was not indicated in 231 patients (some overlap) (Table 2).
The 231 patients with the 231 lesions for which ESD was not indicated on histopathological examination were divided into two groups: those who additionally underwent surgery (additional operation group) and those who were followed up (follow-up group). In principle, additional surgery was recommended for patients who could tolerate surgery. In elderly patients, patients with poor performance status, and patients with underlying disease, the treatment policy was decided on the basis of the background characteristics of each patient after weighing the potential risks and benefits of additional surgery and follow-up observation.
Long-term outcomes and risk factors for metastasis and recurrence were clinicopathologically studied retrospectively (capture rate, 98.7%). The clinicopathological variables studied were sex, age, tumor location (upper/middle/lower), macroscopic type, ulceration, tumor size, histological type, depth of invasion, lymphatic involvement, vascular involvement, horizontal margin/vertical margin, antithrombotic therapy, underlying disease, and outcomes (5-year cause-specific survival and 5-year overall survival). Patients 75 years or older more often have multiple underlying diseases and functional disorders that influence their activities of daily living (ADL) than younger patients [10, 11]. We therefore additionally studied long-term outcomes in patients 75 years or older.
Patients underwent esophagogastroduodenoscopy (EGD) and abdominal computed tomographic scanning (CT) as pretreatment examinations. Endoscopic ultrasonography was performed as required if it was difficult to diagnose the depth of invasion.
Endoscopic submucosal dissection
The circumference of the lesion was marked with a needle knife. After injecting glycerol solution into the submucosa, an initial cut was made with a needle knife outside the marking. An IT Knife (Olympus Medical Systems, Tokyo, Japan) was inserted into this cut and operated to cut around the lesion [12]. The marked lesion was separated from the surrounding normal mucosa. Then, the submucosal layer was dissected using the IT Knife, and the lesion was finally removed. An IT Knife was used to perform ESD until the end of March 2007, and an IT Knife2 (Olympus Medical Systems) was then used from April 2007 onward [13].
Histopathological evaluation
The tissue specimens were fixed in formalin, cut into 2-mm-wide strips perpendicular to the lesion base, and embedded in paraffin. A pathologist examined the sections to determine the histopathological diagnosis according to the Japanese Classification of Gastric Carcinoma [3]. Tumor size, depth of invasion, presence of ulceration, lymphatic and vascular involvement, and tumor involvement of the horizontal and vertical margins were assessed. The depth of invasion was defined as follows: M, mucosal invasion; SM1, minute submucosal invasion (<500 µm below the muscularis mucosae); and SM2, submucosal invasion (≥500 µm below the muscularis mucosae). En bloc resection was defined as the endoscopic resection of an entire lesion in a single procedure. Complete resection was defined as the endoscopic resection of an entire lesion in a single procedure, with no histopathological evidence of tumor at the resection margin. Incomplete resection was defined as tumor-positive margins on histopathological examination. Endoscopically resected lesions with margins that could not be evaluated histopathologically because of electrosurgical or mechanical damage were classified as not assessable. Lesions for which ESD was not indicated were defined as lesions that did not histopathologically meet the JGCA criteria or the expanded criteria.
Follow-up
In the additional operation group, patients were promptly referred to the Department of Gastrointestinal Surgery to undergo laparoscopy-assisted distal gastrectomy with D2 lymph-node dissection, total gastrectomy, or proximal gastrectomy. During the first 2 years after surgery, medical examinations were performed every 3 months, computed tomography (CT) was performed every 6 months, and esophagogastroduodenoscopy (EGD) was performed every year. From 3 years after surgery onward, medical examinations, CT, and EGD were performed at 1-year intervals. Patients were followed up for 5 years.
In the follow-up group, patients underwent EGD 2 months after ESD. During the first 3 years after surgery, medical examinations, EGD, and CT were performed at 6-month intervals. From 4 years after treatment onward, medical examinations, EGD, and CT were performed at 1-year intervals. Patients were followed up for 5 years.
Statistical analysis
Patients with lesions for which endoscopic treatment was not indicated were divided into two groups: the additional operation group and the follow-up group. Clinicopathological characteristics were compared between the groups with the use of the Chi-square test.
Survival time was calculated as the interval between the date of the first session of ESD and the date of death or the last date on which the patient was confirmed to be alive for survivors. Survival curves were calculated using the Kaplan–Meier method. The log-rank test was used to compare survival. All p values reported are two-sided, and p values of less than 0.05 were considered to indicate statistical significance. Risk factors for metastasis or recurrence with p values of <0.05 on univariate analysis were included in multivariate logistic regression analysis.
Results
Table 3 shows the clinicopathological characteristics of the additional operation group and the follow-up group. The median follow-up was 48 months (range 1–154). There were 174 men and 57 women, with a median age of 72 years (range 40–90). The additional operation group comprised 118 patients, and the follow-up group comprised 113 patients. The mean age was significantly higher in the follow-up group (77 years) than in the additional operation group (69 years; p < 0.001).
Tumor characteristics, location, macroscopic type, histological type, lymphatic involvement, horizontal margin, and vertical margin did not differ significantly between the additional operation group and the follow-up group. However, ulceration was significantly more common in the follow-up group (31.9%, 36/113) than in the additional operation group (17.8%, 21/118; p = 0.0132). The median tumor size was significantly greater in the follow-up group (25 mm; range 5–84 mm) than in the additional operation group (20 mm; range 2–95 mm; p = 0.036). The depth of invasion was the mucosa (M) in 13 lesions (11.0%), the first layer of the submucosa (SM1: invasion depth 500 µm below the muscularis mucosae) in 19 lesions (16.1%), the second layer of the submucosa (SM2: invasion depth 500 µm or more from the muscularis mucosae) in 85 lesions (72.0%), and the muscularis propria (MP) in 1 lesion (5.9%) in the additional operation group and the mucosa (M) in 35 lesions (31.0%), the first layer of the submucosa (SM1) in 19 lesions (16.8%), the second layer of the submucosa (SM2) in 57 lesions (50.4%), and the muscularis propria (MP) in 2 lesions (17.7%) in the follow-up group. The depth of invasion was significantly deeper in the additional operation group (p = 0.001). There was a significant trend toward a higher incidence of vascular involvement in the additional operation group (38.1%, 45/118) than in the follow-up group (24.8%, 28/113; p = 0.029). The additional operation group had a significantly deeper depth of invasion and a significantly higher proportion of patients with vascular involvement. The follow-up group had a significantly higher incidence of ulceration and a significantly longer tumor diameter.
Antithrombotic therapy was given to 14 patients (11.9%) in the additional operation group and 24 patients (21.2%) in the follow-up group. Underlying disease was present in 12 patients (10.2%) in the additional operation group and 88 patients (77.9%) in the follow-up group. The proportion of patients with underlying disease was significantly higher in the follow-up group (p < 0.001).
Follow-up was performed in 25 patients (22.1%) who could tolerate surgery but refused to undergo operation and in 88 patients (77.9%) in whom additional surgery was precluded by factors such as advanced age, poor performance status, and underlying disease. The main underlying diseases were cardiovascular disease, cerebrovascular disease, and respiratory disease in addition to various other diseases (Table 4).
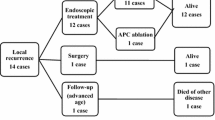
In the additional operation group, lymph-node metastasis was found at surgery in 10.2% (12/118) of the patients, but no patient had local recurrence, lymph-node metastatic recurrence, or distant metastatic recurrence. In the follow-up group, local recurrence was found in 2.7% (3/113) of the patients, abdominal lymph-node recurrence in 0.9% (1/113), and distant metastatic recurrence in 2.7% (3/113). Among the 3 patients with local recurrence, 1 underwent additional surgery, 1 underwent additional argon plasma coagulation, and 1 was observed. The patient who underwent additional argon plasma coagulation died of died of gastric cancer 15 months after ESD. The patient with abdominal lymph-node recurrence underwent additional surgery 14 months after ESD, but had multiple bone metastases 25 months after ESD and died of died of gastric cancer 36 months after ESD. Distant metastatic recurrence developed in the thoracic vertebrae, peritoneum, or lung in 1 patient each. The patient with thoracic vertebral metastasis died of gastric cancer 15 months after ESD, the patient with peritoneal metastatic recurrence died of gastric cancer 30 months after ESD, and the patient with pulmonary metastatic recurrence died of gastric cancer 52 months after ESD. No patient died of gastric cancer in the additional operation group; 5 patients (4.4%) died of gastric cancer in the follow-up group (p = 0.021).
The 5-year cause-specific survival rate was significantly higher in the additional operation group (100%) than in the follow-up group (92.6%, p = 0.010) (Fig. 1A). The 5-year overall survival rate was also significantly higher in the additional operation group (96.0%) than in the follow-up group (73.3%, p < 0.001) (Fig. 1B).
A Overall survival. The 5-year overall survival rate was significantly higher in the additional operation group (96.0%) than in the follow-up group (73.3%, p = 0.010). B Cause-specific survival. The 5-year cause-specific survival rate was significantly higher in the additional operation group (100%) than in the follow-up group (92.6%, p = 0.010)
Table 5 shows the clinicopathological characteristics of patients 75 years or older. The additional operation group comprised 22 patients, and the follow-up group comprised 67 patients. The median age was 77 years (range 75–81) in the additional operation group and 79 years (range 75–90) in the follow-up group and was significantly higher in the follow-up group (p < 0.001). The proportion of patients with underlying disease was significantly greater in the follow-up group (p < 0.001).
Among elderly patients 75 years or older, the 5-year cause-specific survival rate did not differ significantly between the additional operation group (100%) and the follow-up group (91.2%, p = 0.283) (Fig. 2A). The 5-year overall survival rate was slightly lower in the follow-up group (62.8%) than in the additional operation group (81.8%, p = 0.232) (Fig. 2B).
A Overall survival. Among elderly patients 75 years or older, the 5-year overall survival rate was slightly lower in the follow-up group (62.8%) than in the additional operation group (81.8%, p = 0.232). B Cause-specific survival. Among elderly patients 75 years or older, the 5-year cause-specific survival rate did not differ significantly between the additional operation group (100%) and the follow-up group (91.2%, p = 0.283)
Among 231 patients who were histopathologically confirmed to have lesions for which ESD was not indicated, 16 patients (12 in the additional operation group and 4 in the follow-up group) had lesions associated with metastasis or recurrence (Table 6). A univariate analysis showed that depth of invasion, lymphatic involvement, and vertical margin were significant risk factors for metastasis or recurrence. A multivariate logistic regression analysis showed that lymphatic involvement was an independent risk factor for metastasis or recurrence (p = 0.003; odds ratio 10.594; 95% confidence interval 2.294–48.927) (Table 7).
Discussion
Japan has become an aging society, and the number of elderly patients with various underlying diseases is increasing. In patients in good general condition whose underlying diseases are controlled, we strongly recommend that additional surgery be performed. However, additional surgery is not feasible in some patients because of poorly controlled underlying disease or poor general condition. In the present study, we assessed long-term outcomes and risk factors for metastasis and recurrence in patients who underwent ESD for EGC and were given a diagnosis of lesions for which ESD was not indicated on histopathological evaluation.
In this study, we performed ESD for EGC and studied patients who were histopathologically confirmed to have lesions for which ESD was not indicated. Both the 5-year cause-specific survival and the 5-year overall survival were significantly better in the additional operation group than in the follow-up group (100% vs. 92.6% and 96.0% vs. 73.3%, respectively; p = 0.010). In the additional operation group, lymph-node metastasis was found at surgery in 10.2% of the patients. Cure is usually difficult to achieve in patients in whom metastasis or recurrence develops after ESD. Additional surgery is therefore recommended for patients found to have lesions for which ESD is not indicated according to the gastric cancer treatment guidelines [3].
Hoteiya et al. [14] divided patients who underwent non-curative resection of EGC into two groups: an additional surgery group and a follow-up group. Although many patients in the follow-up group were elderly and died of other diseases, overall survival did not differ significantly between the groups.
In our study as well, patients in the follow-up group were older than those in the additional operation group. In about 80% of patients in the follow-up group, surgery was not performed because of elderly, poor performance status, and cardiovascular and other underlying diseases. In addition, a subanalysis of patients 75 years or older showed no significant difference in either the 5-year cause-specific survival rate or the 5-year overall survival rate between the additional operation group and the follow-up group.
Kusano et al. [15] divided patients 75 years or older who underwent non-curative endoscopic resection of EGC into two groups: an additional surgery group and a follow-up group. They found no significant difference in the 5-year overall survival or the 5-year recurrence-free survival between the groups. The majority of patients who are 75 years or older have multiple underlying diseases and functional disorders that would influence ADL. In Japan, the proportion of people who regularly attend hospitals for at least one chronic disease is nearly 70% among people who are 75–84 years of age, which is higher than that in other age groups [10, 11, 16, 17]. Sumiyoshi et al. [18] reported that ESD is an effective treatment in terms of short- and long-term outcomes even in elderly patients with EGC who are 75 years or older and recommended that such patients be closely followed up after treatment. Elderly patients aged 75 years or older and those with serious underlying disease should not only undergo additional surgery for the lesions for which ESD was not indicated, but should also carefully receive other treatments in accordance with their general condition.
In the present study, we examined risk factors for metastasis or recurrence in patients who underwent ESD for EGC. Our results showed that lymphatic involvement was an independent risk factor for metastasis or recurrence. Various studies have investigated risk factors for lymph-node metastasis and found that SM2 invasion, lymphatic involvement, vascular involvement, and poorly differentiated cancer are risk factors [19,20,21,22,23]. Ishii et al. [9] reported that SM2 invasion and moderate lymphatic involvement (ly2) or marked lymphatic involvement (ly3) were predictors of lymph-node metastasis in patients who underwent additional operation after endoscopic treatment for cT1aN0M0 EGC. Sekiguchi et al. [24] scored surgically resected specimens of EGC according to tumor size, depth of invasion, histological type, the presence or absence of an ulceration, and lymphovascular involvement and found that the score was related to the risk of lymph-node metastasis. They reported that lymphovascular involvement is a strong risk factor for lymph-node metastasis. In our study, 14% (14/94) of patients with lymphatic involvement had lymph-node metastasis or peritoneal dissemination. Additional surgery should thus be aggressively performed in patients with lymphatic involvement.
In principle, we recommend additional surgery for patients who can tolerate surgery and have a histopathological diagnosis of lesions for which ESD is not indicated. However, in elderly patients and patients with concomitant diseases, the background characteristics of the individual patient, including the prognosis of underlying disease, the expected decrease in QOL associated with surgery, the risks of metastasis and recurrence, and requests made by the patients and their family members, were evaluated and whether to perform additional surgery or follow-up observation was decided after weighing the potential benefits against the risks. Therefore, selection bias may have appreciably affected the choice of treatment strategy. However, we believe that long-term outcomes of additional surgery and follow-up observation reflected the situation in actual clinical practice.
Our study had several important limitations. It was a retrospective study and performed at a single center. Another important limitation of our study was that the patients’ requests and ability to tolerate surgery were considered in the assignment to treatment groups. Therefore, further prospective studies of larger numbers of patients with lesions for which ESD is not indicated are needed to confirm our results.
Conclusions
In patients with EGC who are histopathologically confirmed to have lesions for which ESD is not indicated, surgery should be aggressively performed if such treatment can be tolerated. In elderly patients 75 years or older and those with serious underlying diseases, follow-up observation was suggested to be a feasible option provided that informed consent is obtained from the patients after they are provided with an explanation of the risk of recurrence.
Change history
07 December 2017
In Table 1, the second item in the right-hand column “Extra-indication” should be changed to “Out of indication”. The correct version of Table 1 is displayed.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:359–386
Ono H, Yao K, Fujishiro M, Oda I, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Ichinose M, Matsui T (2016) Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer. Dig Endosc 28:3–15
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver.4) Gastric cancer 2016 (Published online)
Nakata B, Tendo M, Okuyama M, Nakahara K, Ishizu H, Masuda G, Lee T, Hori T, Ohsawa M, Sato H, Ishikawa T (2016) Additional surgical resection after endoscopic mucosal dissection for early gastric cancer: a medium-sized hospital’s experience. Int J Surg 36:335–341
Gotoda T, Yanagisawa A, Sasako M, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y (2000) Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer 3:219–225
Oda I, Gotoda T, Hamanaka H, Eguchi T, Saito Y, Matsuda T, Bhandari P, Emura F, Saito D, Ono H (2005) Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time and complications from a large consecutive series. Dig Endosc 17:54–58
Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, Ohnita K, Mizuta Y, Shiozawa J, Kohno S (2009) Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut 58:331–336
Tanabe S, Ishido K, Matsumoto T, Kosaka T, Oda I, Suzuki H, Fujisaki J, Ono H, Kawata N, Oyama T, Takahashi A, Doyama H, Kobayashi M, Uedo N, Hamada K, Toyonaga T, Kawara F, Tanaka S, Yoshifuku Y (2017) Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: multicenter collaborative study. Gastric Cancer 20:45–52
Ishii S, Yamashita K, Kato H, Nishizawa N, Ushiku H, Mieno H, Moriya H, Hosoda K, Katada N, Kikuchi S, Tanabe S, Koizumi W, Saegusa M, Watanabe M (2016) Predictive factors for lymph node metastasis in additional gastrectomy after endoscopic resection of cT1aN0 gastric cancer. Surg Today 46:1031–1038
Kakushima N, Fujishiro M, Kodashima S, Muraki Y, Tateishi A, Yahagi N, Omata M (2007) Technical feasibility of endoscopic submucosal dissection for gastric neoplasms in the elderly Japanese population. J Gastroenterol Hepatol 22:311–314
Chinda D, Sasaki Y, Tatsuta T, Tsushima K, Wada T, Shimoyama T, Fukuda S (2015) Perioperative complications of endoscopic submucosal dissection for early gastric cancer in elderly Japanese patients 75 years of age or older. Intern Med 54:267–272
Ohkuwa M, Hosokawa K, Boku N, Ohtu A, Tajiri H, Yoshida S (2001) New endoscopic treatment for intramucosal gastric tumors using an insulated-tip diathermic knife. Endoscopy 33:221–226
Ono H, Hasuike N, Inui T, Takizawa K, Ikehara H, Yamaguchi Y, Otake Y, Matsubayashi H (2008) Usefulness of a novel electrosurgical knife, the insulation-tipped diathermic knife-2, for endoscopic submucosal dissection of early gastric cancer. Gastric Cancer 11:47–52
Hoteya S, Iizuka T, Kikuchi D, Ogawa O, Mitani T, Matsui A, Furuhata T, Yamashita S, Yamada A, Kaise M (2016) Clinicopathological outcomes of patients with early gastric cancer after non-curative endoscopic submucosal dissection. Digestion 93:53–58
Kusano C, Iwasaki M, Kaltenbach T, Conlin A, Oda I, Gotoda T (2011) Should elderly patients undergo additional surgery after non-curative endoscopic resection for early gastric cancer? Long-term comparative outcomes. Am J Gastroenterol. 106:1064–1069
Centers for Disease Control and Prevention (2003) Public health and aging: trends in aging—United States and worldwide. JAMA 289:1371–1373
Fried L, Barron J (2005) Older adults. Handbook of urban health: populations, methods, and practice. Springer, New York
Sumiyoshi T, Kondo H, Fujii R, Minagawa T, Fujie S, Kimura T, Ihara H, Yoshizaki N, Hirayama M, Oyamada Y, Okushiba S (2017) Short- and long-term outcomes of endoscopic submucosal dissection for early gastric cancer in elderly patients aged 75 years and older. Gastric Cancer 20:489–495
Fidler IJ (1995) Clitical factors in the biology of human cancer metastasis. Am Surg 61:1065–1066
Hoteya S, Yamashita S, Kikuchi D, Nakamura M, Fujimoto A, Matsui A, Nishida N, Mitani T, Kuroki Y, Iizuka T, Yahagi N (2011) Endoscopic submucosal dissection for submucosal invasive gastric cancer and curability criteria. Dig Endosc 23:30–36
Kim H, Kim JH, Park JC, Lee YC, Noh SH, Kim H (2011) Lymphovascular invasion is an important predictor of lymph node metastasis in endoscopically resected early gastric cancers. Oncol Rep 25:1589–1595
Sunagawa H, Kinoshita T, Kaito A, Shibasaki H, Kaneko K, Ochiai A, Ohtsu A, Nishida T (2016) Additional surgery for non-curative resection after endoscopic submucosal dissection for gastric cancer: a retrospective analysis of 200 cases. Surg Today 47:202–209
Fujii H, Ishii E, Tochitani S, Nakaji S, Hirata N, Kusanagi H, Narita M (2015) Lymph node metastasis after endoscopic submucosal dissection of a differentiated gastric cancer confined to the mucosa with an ulcer smaller than 30 mm. Dig Endosc 27:159–161
Sekiguchi M, Oda I, Taniguchi H, Suzuki H, Morita S, Fukagawa T, Sekine S, Kushima R, Katai H (2016) Risk stratification and predictive risk-scoring model for lymph node metastasis in early gastric cancer. J Gastroenterol 51:961–970
Funding
No research support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Authors Takafumi Yano, Kenji Ishido, Satoshi Tanabe, Takuya Wada, Mizutomo Azuma, Natsuko Kawanishi, Sakiko Yamane, Akinori Watanabe, Chikatoshi Katada, and Wasaburo Koizumi have no conflicts of interest or financial ties to disclose.
Informed consent
Informed consent was obtained from all patients in accordance with our institutional protocol.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00464-017-5953-7.
Rights and permissions
About this article
Cite this article
Yano, T., Ishido, K., Tanabe, S. et al. Long-term outcomes of patients with early gastric cancer found to have lesions for which endoscopic treatment is not indicated on histopathological evaluation after endoscopic submucosal dissection. Surg Endosc 32, 1314–1323 (2018). https://doi.org/10.1007/s00464-017-5809-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5809-1