Abstract
Background
Single-site laparoscopic percutaneous extraperitoneal closure (SLPEC) of hernia sac/processus vaginalis has been widely performed for repair of inguinal hernia/hydrocele in children. However, a variety of surgical instruments and techniques were used, and significant differences existed among the SLPEC reports.
Methods
A literature search was performed for all available studies concerning SLPEC for pediatric inguinal hernia/hydrocele in PubMed, Embase and Cochrane library. The surgical details and operative outcomes were pooled and analyzed with software StataSE 12.0.
Results
49 studies fulfilled the predefined inclusion criteria of this review and 37 studies were finally included in the meta-analysis. The mean incidence of CPPV was 29.1% (range 5.73–43.0%). The average of mean operative time was 19.56 min (range 8.30–41.19 min) for unilateral SLPEC and 27.23 min (range 12.80–48.19 min) for bilateral SLPEC. The total incidence of injury, conversion, recurrence, hydrocele formation, knot reaction, severe pain, and scrotal swelling was 0.32% (range 0–3.24%), 0.05% (range 0–0.89%), 0.70% (range 0–15.5%), 0.23% (range 0–3.57%), 0.33% (range 0–3.33%), 0.05% (range 0–4.55%), and 0.03% (range 0–1.52%), respectively. There was no development of testicular atrophy. Subgroup analyses showed an inverse correlation between the injury incidence and adoption of assisted forceps, hydrodissection, and blunt puncture device, between the conversion rate and adoption of hydrodissection, between the recurrence/hydrocele incidence and adoption of assisted forceps, hydrodissection, nonabsorbable suture and the preventive measures to avoid ligating the unnecessary subcutaneous tissues, and between the rate of knot reaction and adoption of assisted forceps, hydrodissection, and the preventive measures.
Conclusions
SLPEC was a well-developed procedure for repair of pediatric inguinal hernia/hydrocele. Adoption of assisted forceps, hydrodissection, nonabsorbable suture, and the preventive measures to avoid ligating the unnecessary subcutaneous tissues could significantly reduce the intra- and postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pediatric inguinal hernia and hydrocele are the most common surgical pathologies in children worldwild, of which a congenital patent processus vaginalis (PPV) is the main cause [1]. With the development of minimally invasive surgery, laparoscopic repair of these diseases has progressed rapidly in the past decades [2]. Among the various effective procedures, single-site laparoscopic percutaneous extraperitoneal closure (SLPEC) of the hernia sac and processus vaginalis has been widely used with a minimal risk of injury to the spermatic cord, a low recurrence rate, and satisfactory cosmetic results [3].
As for every procedure, surgical outcomes (e.g., operative time, intra- and postoperative complications, etc.) are the issues of great concern. Numerous studies have evaluated the operative outcomes in large cohort of patients who received SLPEC [3]. However, these studies might be limited by inaccuracies in data collection, which may cause underreporting of complications and heterogeneity in the outcomes. We therefore performed a systematic review and meta-analysis of SLPEC on repair of pediatric inguinal hernia and hydrocele, and summarized the surgical details and operative outcomes of this procedure.
Materials and methods
Search strategy
A search was carried out for all studies concerning laparoscopic repair of inguinal hernia and hydrocele in children, which were published in the databases of PubMed, Embase and Cochrane library. Our searches used both free-text protocol and keywords for all databases. The search strategies were as seen in Appendix. No lower date or “language” limits were set. All titles and/or abstracts were reviewed initially to select studies if they contained results of laparoscopic inguinal hernia and hydrocele repair in children. After identification of the titles and/or abstracts, the full text of all potentially relevant studies was retrieved. The reference lists of included studies were examined manually to identify any additional relevant studies. The last search was performed on July 31, 2016.
Eligibility criteria
Studies were included in the systematic review if they met the following criteria: children with inguinal hernia or hydrocele as the study participant; SLPEC or its modification as the surgical method; operative time and complications as the outcomes of interest. Editorials, letters, review articles, technical reports, and abstracts with incomplete data were excluded from meta-analysis. If data were duplicated in more than one study, only the most recent or informative one was included in the final analysis.
Surgical method
The SLPEC procedure was briefly described as follows [3]: a trocar was placed at the umbilicus for the endoscope; a hernia needle with a suture was inserted percutaneously into the preperitoneal space at the corresponding skin of the internal ring; the suture was then introduced extraperitoneally in one side of the ring and extracted through the other side at the same skin incision; the suture was tied externally to obliterate the internal ring; the contralateral PPV (CPPV) was usually repaired by the same procedure; sometimes, an additional forceps and preperitoneal hydrodissection [4] (i.e., injection of isotonic saline into the preperitoneal space to separate the vas deferens and spermatic vessels from the peritoneum) was used to assist the procedure in some studies.
Data extraction
Data were extracted from each study using a predefined extraction form. The extracted data included general characteristics of the studies and patients (first author’s surname, publication year, study location, design and duration, patients number, age and gender, patient’s disease and its laterality, and length of follow-up), the surgical details (number of working ports, type of endoscope, hernia device and suture material, and whether applying an assisted forceps, hydrodissection, and preventive measures to avoid ligating the unnecessary tissues), and surgical outcomes (number of CPPVs, operative time, intra and postoperative complications) of SLPEC. Level of evidence was assessed according to the Oxford Center for Evidence-Based Medicine [5].
Statistical analysis
The outcome measures were mean operative time, and the incidence of CPPV, intra-, and postoperative complications. We assumed that the operative outcomes of SLPEC were probably influenced by the specific surgical aspects, such as the type of hernia device and suture material, application of assisted forceps and hydrodissection, and measures to avoid ligating the unnecessary tissues. Given this, subgroup analyses of the primary outcome measures were performed across a variety of the surgical details of SLPEC. The significance of differences between subgroups was evaluated by t test for continuous data and by Chi-squared or Fisher’s exact test for dichotomous data, respectively. All analyses were conducted using StataSE 12.0 software (Stata Corporation, College Station, TX), and a two-sided P < 0.05 was considered statistically significant.
Results
Selection of the studies and the level of evidence
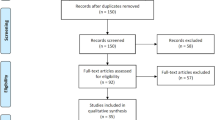
Figure 1 shows the study selection result of this systematic review and meta-analysis. From the 2262 citations initially identified, 49 studies [3, 4, 6–52] fulfilled the predefined inclusion criteria of this review. Subsequently, five duplicate publications [6, 7, 9, 11, 12], three abstracts with incomplete data [13–15], three technical reports [4, 16, 17], and one review article [3] were excluded. Finally, the remaining 37 studies [8, 10, 18–52] were included in the meta-analysis. There were 26 SLPEC case series [8, 10, 29–52] (level 4); three studies [18, 22, 24] comparing different techniques or subgroups in the context of SLPEC (level 3); eight comparative studies [19–21, 23, 25–28] of SLPEC vs. other procedures (one study [20], level 2; seven studies [19, 21, 23, 25–28], level 3).
General characteristics of the studies and patients (Table 1)
Publication dates of the included studies ranged from 2006 to 2016. Sixteen studies were conducted in China, six studies in Japan and USA each, three studies in Turkey, two studies in Egypt and India each, and one study in Russia and Poland each. Overall, these studies comprised 11,815 patients who underwent SLPEC and 1093 patients undergoing other procedures. Of these studies, number of the patients who underwent SLPEC was between 11 and 3507. The age of patients ranged from birth to 17 years. Thirteen-one studies [10, 18–21, 23–28, 30–37, 39–46, 48–52] only included patients with inguinal hernia, two studies [38, 46] only with hydrocele, and four studies [8, 22, 29, 47] with both diseases. Among the 35 studies [8, 10, 18–37, 39–45, 47–52] including inguinal hernias, there were three [20, 31, 44] and two studies [22, 32] each only included female and male patients, respectively.
Surgical details of SLPECs (Table 2)
Twelve studies conventionally introduced two working ports in the umbilicus, of which one [18] inserted three ports for the patients with incarcerated inguinal hernia; 25 studies initially placed one umbilical port, of which nine studies [8, 19, 34, 38, 39, 42, 43, 48, 51] added another port for some patients later. The vast majority of the included studies applied an approximately 3- or 5-mm laparoscope, of which one study each utilized a rigid bronchoscope [37] and ureteroscope [49], respectively. Some studies sutured the internal ring using a specially made or modified puncture needle (e.g., Endoclose, Lapaherclosure, Tuohy needle or Kirschner pin, etc.) which had a relatively blunt tip [8, 18–21, 24, 25, 27, 33, 36, 37, 39, 41, 44, 47, 49, 50], while others used ordinary sharp needles [8, 22, 23, 26, 28–32, 34, 35, 38, 40, 42, 43, 45, 46, 48, 50–52] (e.g., taper needle, injection needle, angiocath needle, etc.). Most studies ligated the hernia sac or processus vaginalis with nonabsorbable sutures while very few studies with absorbable [28] or both materials [22, 23, 35, 37, 51].
Ten studies [10, 26, 28, 30, 35, 36, 39, 46, 48, 50] carried out hydrodissection to obtain preperitoneal dissection and avoid subsequent injury to the vas and vessels. Eleven studies adopted the “one-puncture” technique [10, 20, 24, 26, 30, 39, 40, 44, 46, 50] (i.e., withdraw of the puncture needle just to the preperitoneal space on the roof of the internal ring rather than the outside of the abdominal wall, and then reintroduction along the other side of the ring) or other measure [8] (i.e., setting a cannula outside the puncture needle) to avoid ligating the unnecessary subcutaneous tissues, such as muscles and nerves.
Operative outcomes of SLPECs (Table 3)
The mean incidence of CPPV was 29.1% (range 5.73–43.0%) after three studies [25, 26, 43] with duplicate data and 11 studies [10, 20, 21, 23, 32, 33, 36, 40, 44, 45, 47] with insufficient data excluded. The average of mean operative time was 19.56 min (range 8.30–41.19 min) for unilateral SLPEC and 27.23 min (range 12.80–48.19 min) for bilateral SLPEC after three studies [25, 43, 48] with duplicate data and five [22, 31, 32, 40, 51] studies with insufficient data excluded. The total incidence of injury and conversion was 0.32% (range 0–3.24%) and 0.05% (range 0–0.89%), respectively, after three studies [25, 26, 34] with duplicate data excluded. The most commonly injured sites were the external iliac and inferior epigastric vessels. All injuries were treated with observation or by external compression, and no sequela was left.
The overall incidence of recurrence and hydrocele occurrence was 0.70% (range 0–15.5%) and 0.23% (range 0–3.57%), respectively, after three studies [26, 27, 43] with duplicate data removed. Knot reactions with various degrees (e.g., palpable subcutaneous knots, erythema, granulomas, and abscess) were observed at the suture site of internal ring in nine studies, and the total incidence was 0.33% (range 0–3.33%) after three studies [26, 27, 34] with duplicate data and one study [52] with insufficient data removed. Severe pain was found in the ligated region in only three studies [10, 19, 51], and the total incidence was 0.05% (range 0–4.55%). Scrotal swelling was reported in only two studies [18, 38], and the total incidence was 0.03% (range 0–1.52%). There was no development of testicular atrophy.
Aspects of surgery influencing the primary operative outcomes of SLPEC (Table 4)
No comparative studies evaluated the effect of assisted forceps, preperitoneal hydrodissection, and sharpness of puncture needle on the primary operative outcomes of SLPEC (i.e., mean operative time, intra- and postoperative complications). Pooled the results of SLPEC case series [8, 10, 18–25, 28–42, 44–52] showed that an assisted forceps significantly reduced the incidence of injury (0.23% vs. 0.72%, P = 0.007) and recurrence/hydrocele (0.55% vs. 2.91%, P = 0.000), but not markedly affected mean operative time and the incidence of conversion and knot reaction. Hydrodissection significantly decreased the incidence of injury (0.82% vs. 0.23%, P = 0.005), conversion (0.27% vs. 0.03%, P = 0.024) ,and recurrence/hydrocele (1.64% vs. 0.86%, P = 0.019), but not markedly affected mean operative time and knot reaction [8, 10, 18–25, 28–42, 44–52]. Furthermore, the injury incidence was significantly higher in the group with sharp puncture needle than in that with blunt device (0.51% vs. 0.11%, P = 0.002) [8, 10, 18–25, 28–42, 44–52].
Li et al. [24] performed the SLPEC for pediatric inguinal hernia using an innovative 2-hooked device which overcame the limitations of the 1-hooked apparatus (i.e., inclusion of some upper subcutaneous tissues in the ligature). Compared to the 1-hooked apparatus, the 2-hooked device yielded a relatively low incidence of knot reaction (0 vs. 1.59%, P = 0.28) and recurrence (0 vs. 1.59%, P = 0.28), despite no statistical significance. Pooled analysis including the SLPEC case series [8, 10, 18–25, 28–42, 44–52] showed that whether or not taking the measures to avoid ligating the unnecessary subcutaneous tissues markedly affected the incidence of recurrence/hydrocele (0.05% vs. 1.15%, P = 0.000) and knot reaction (0 vs. 0.41%, P = 0.001). Grimsby et al. [22] compared the outcomes of absorbable vs. nonabsorbable sutures during SLPEC for pediatric inguinal hernias and found a significant difference of the recurrence incidence (26% vs. 4%, P = 0.004). Meta-analysis of the included 32 studies [8, 10, 18–22, 24, 25, 28–34, 36–42, 44–52] demonstrated that nonabsorbable suture remarkably reduced the incidence of recurrence/hydrocele compared with absorbable suture (0.51% vs. 19.0%, P = 0.000).
Discussion
SLPEC was a well-developed surgical procedure in the past decade, which has been wildly used as a treatment for pediatric inguinal hernias and hydroceles [3]. By systematically searching the literature, we found that there were at least 51 relevant reports concerning this procedure [3, 4, 6–52]. SLPEC has been reported to be easy and effective. The unilateral and bilateral mean operative time was about 20 and 27 min, respectively, while the overall incidence of recurrence and hydrocele was 0.70% and 0.23%, respectively. Furthermore, SLPEC also had the significant advantages of minimal invasion and cosmesis. There were only a concealed umbilical incision and a tiny puncture hole which left no obvious scars. However, significant differences existed among the SLPEC studies, and a variety of surgical instruments and techniques were used. Given this, we performed this meta-analysis to pool the surgical details and operative outcomes of SLPEC, and explore the surgical aspects affecting the primary operative outcomes.
The included studies showed that accident puncture of the external iliac [29, 34, 52] and inferior epigastric vessels [19] was the most common injury during SLPEC, which could be cured with conservative treatment (e.g., observation and external compression). A working forceps could greatly facilitate the meticulous manipulation of puncture needle and then reduce the risk of injury in abdominal cavity [53]. Application of the hydrodissection technique could add the preperitoneal safe space around the internal ring [4]. A blunt hernia needle helped prevent the accident damage to the extraperitoneal tissues [4, 19, 53] (e.g., the external iliac and inferior epigastric vessels, and spermatic cord). Therefore, all these surgical details were significantly associated with the low incidence of injury. It was rare to see conversions, which were usually caused by difficult operations of the inguinal hernias with giant hernia sac or excessive peritoneal folds [19, 28, 48]. Hydrodissection brought great convenience to perform a complete circumferential closure of the sac at the level of the internal ring, and consequently led to a significant decrease of conversion. Unexpectedly, we did not found the remarkable reduction of conversion using the assisted forceps. Although the convenience from these surgical details reduced the operation time in abdominal cavity, they also added the time of these techniques themselves. Therefore, there was no significant difference of the total operative time.
Recurrence and hydrocele formation were mainly caused by low patient number, inexperienced surgeon, leaving a peritoneal gap in the encircling suture, loosing of ligation due to inappropriate or inadequate knotting, and use of absorbable sutures [2]. Adoption of the grasping forceps and hydrodissection technique ensured the complete closure of mere hernia sac/processus vaginalis, leaving no peritoneal gaps [3]. Some preventive measures could effectively avoid ligating the unnecessary subcutaneous tissues, and thus reduce the loose knots during surgery and the knot loosening thereafter due to excessive tissues in the ligature [3]. These measures included the “one-puncture” technique [10, 20, 24, 26, 30, 39, 40, 44, 46, 50] and setting a cannula outside the puncture needle [8]. The nonabsorbable suture could avoid later split of the internal ring due to absorption of the suture material after the operation [22, 28, 51]. The current meta-analysis showed that these surgical details significantly reduced the recurrence and hydrocele formation. Various knot reactions were mostly caused by the knots which were not buried deeply. The preventive measures to avoid ligating the subcutaneous tissues (e.g., muscles and fascias) ensured that the knot could be buried below the muscular layer. Our meta-analysis showed that these techniques markedly reduced the knot reactions at the suture site of internal ring.
The current review still had some limitations. Firstly, there were various hernia devices applied in the studies, of which most were designed by the authors themselves. Even though for the same device, the detailed use methods might vary among the different studies. These aspects probably affected the surgical outcomes of SLPEC. Therefore, the SLPEC methods required to be unified and standardized. Next, population composition of the patients and surgery experience of the operator [47, 48] might be significantly related to the operative time. Murase et al. [18] reported a markedly longer operative time for incarcerated inguinal hernia than for reducible hernia. Yamoto et al. [47] reported a shorter operative time for the girls and the surgeons with more experience. Chang et al. [48] found that female patients, reducible hernias, maturity, surgery volume, and weight >5 kg would decrease the operative time. Accordingly, these nonsurgical factors should also be considered when assessing the perioperative outcomes of SLPEC. Finally, some hernia recurrence and hydrocele formation probably developed very late. Shalaby et al. [54] reported a cohort of 38 children with 42 recurrent hernias, of which the time interval between surgery and recurrence ranged from 1 day to 2.5 years. Consequently, a relatively long-term follow-up was necessary to accurately evaluate the postoperative complications.
References
Lloyd DA, Rintala RJ (1998) Inguinal hernia and hydrocele. In: O’Neill JA Jr, Rowe MI, Grosfeld JC et al (eds) Pediatric surgery. Mosby, St. Louis, pp 1071–1086
Saranga Bharathi R, Arora M, Baskaran V (2008) Minimal access surgery of pediatric inguinal hernias: a review. Surg Endosc 22:1751–1762
Chang YT (2010) Technical refinements in single-port laparoscopic surgery of inguinal hernia in infants and children. Diagn Ther Endosc 2010:392847
Bharathi RS, Arora M, Baskaran V (2008) How we “SEAL” internal ring in pediatric inguinal hernias. Surg Laparosc Endosc Percutan Tech 18:192–194
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence. Available at: http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf. Accessed 18 October 2016
Shalaby R, Ismail M (2016) The use of epidural needle for single incision laparoscopic pediatric hernia repair: a novel technique. Surg Endosc 30:S152
Peng Y, Li C, Lin W, Xu L (2015) Application of a laparoscopic, single-port, double-needle technique for pediatric hydroceles with multiple peritoneal folds: a trial from a single-center 5-year experience. Urology 85:1466–1470
Liu W, Wu R, Du G (2014) Single-port laparoscopic extraperitoneal repair of pediatric inguinal hernias and hydroceles by using modified Kirschner pin: a novel technique. Hernia 18:345–349
Liu L, Li S, Li M, Yu Z (2013) Single-port laparoscopic assisted percutaneous extraperitoneal closure using an innovated apparatus for inguinal hernia in children. J Laparoendosc Adv Surg Tech A 23:A112
Muensterer OJ, Georgeson KE (2011) Multimedia manuscript: inguinal hernia repair by single-incision pediatric endosurgery (SIPES) using the hydrodissection-lasso technique. Surg Endosc 25:3438–3439
Shen W, Li W, Pan J (2010) A modified single-port technique for the minimally invasive treatment of pediatric inguinal hernias with high ligation of the vaginal process: the initial experience. J Endourol 24:A296
Chang YT, Wang JY, Lee JY, Chiou CS, Hsieh JS (2008) One-trocar laparoscopic transperitoneal closure of inguinal hernia in children. World J Surg 32:2459–2463
Yusheng N, Jie C (2016) Single-hole laparoscopic treatment in pediatric patients with inguinal hernia (908 cases analyze). Hernia 20:S96
Yehya A, Shalaby R, Abdalrazek A, Ibrahem R (2014) Single incision laparoscopic hernia repair in children; a preliminary report. Surg Endosc 28:S93
Gu Q, Li L, Ye H, Li X, Bai D, Zhang J (2013) The single port laparoscopic techniques for inguinal herniaandhydrocele in children. J Laparoendosc Adv Surg Tech A 23:A101
Granberg C, Gargollo P, Minkes R, Snodgrass W, Jacobs M (2012) Single-trocar laparoscopic herniorrhaphy in children. J Urol 187:e223
Harrison MR, Lee H, Albanese CT, Farmer DL (2005) Subcutaneous endoscopically assisted ligation (SEAL) of the internal ring for repair of inguinal hernias in children: a novel technique. J Pediatr Surg 40:1177–1180
Murase N, Uchida H, Seki T, Hiramatsu K (2016) A feasibility of single-incision laparoscopic percutaneous extraperitoneal closure for treatment of incarcerated inguinal hernia in children: our preliminary outcome and review of the literature. Nagoya J Med Sci 78:19–25
Xu Q, Liu SQ, Niu JH, Luo RX, Zhang J, Zhang PF, Li XL, Peng F (2016) A new technique for extraperitoneal repair of inguinal hernia. J Surg Res 204:452–459
Obata S, Ieiri S, Jimbo T, Souzaki R, Hashizume M, Taguchi T (2016) Feasibility of single-incision laparoscopic percutaneous extraperitoneal closure for inguinal hernia by inexperienced pediatric surgeons: single-incision versus multi-incision randomized trial for 2 years. J Laparoendosc Adv Surg Tech A 26:218–221
Kozlov Y, Novozhilov V (2015) Technology of single-incision laparoscopic surgery in treatment of inguinal hernia in small babies. J Laparoendosc Adv Surg Tech A 25:526–530
Grimsby GM, Keays MA, Villanueva C, Bush NC, Snodgrass WT, Gargollo PC, Jacobs MA (2015) Non-absorbable sutures are associated with lower recurrence rates in laparoscopic percutaneous inguinal hernia ligation. J Pediatr Urol 11(275):e1–e4
Timberlake MD, Herbst KW, Rasmussen S, Corbett ST (2015) Laparoscopic percutaneous inguinal hernia repair in children: review of technique and comparison with open surgery. J Pediatr Urol 11(262):e1–e6
Li S, Liu L, Li M (2014) Single-port laparoscopic percutaneous extraperitoneal closure using an innovative apparatus for pediatric inguinal hernia. J Laparoendosc Adv Surg Tech A 24:188–193
Uchida H, Kawashima H, Tanaka Y, Masuko T, Deie K, Iwanaka T (2013) Single-incision laparoscopic percutaneous extraperitoneal closure may be an alternative to standard minimally invasive surgical techniques for pediatric inguinal hernia. J Laparoendosc Adv Surg Tech A 23:A100–A101
Chang YT, Lin JY, Lee JY, Tsai CJ, Chiu WC, Chiu CS (2012) Comparative mid-term results between inguinal herniotomy and single-port laparoscopic herniorrhaphy for pediatric inguinal hernia. Surg Laparosc Endosc Percutan Tech 22:526–531
Uchida H, Kawashima H, Goto C, Sato K, Yoshida M, Takazawa S, Iwanaka T (2010) Inguinal hernia repair in children using single-incision laparoscopic-assisted percutaneous extraperitoneal closure. J Pediatr Surg 45:2386–2389
Bharathi RS, Dabas AK, Arora M, Baskaran V (2008) Laparoscopic ligation of internal ring-three ports versus single-port technique: are working ports necessary? J Laparoendosc Adv Surg Tech A 18:891–894
Thomas DT, Göcmen KB, Tulgar S, Boga I (2016) Percutaneous internal ring suturing is a safe and effective method for the minimal invasive treatment of pediatric inguinal hernia: experience with 250 cases. J Pediatr Surg 51:1330–1335
Cui Z, Liu Y, Zhang W, Sun F (2016) Single-port laparoscopic percutaneous double ligation for pediatric inguinal hernias: report of a new technique and early results. Hernia 20:579–584
Erginel B, Akin M, Yildiz A, Karadag CA, Sever N, Dokucu AI (2016) Percutaneous internal ring suturing as a first choice laparoscopic inguinal hernia repair method in girls: a single-center study in 148 patients. Pediatr Surg Int 32:697–700
Li C, Xu L, Peng Y, Liang X, Lin W (2016) Effects of single-port laparoscopic percutaneous extraperitoneal closure on the orientation of the vas deferens and testicular perfusion and volume: Experience from a single center. J Pediatr Urol 12(170):e1–e5
Ordorica-Flores R, Figueroa-Portillo R, Pérez-Escamirosa F, Lorias-Espinoza D, Minor-Martínez A, Olivares-Clavijo H, Zalles-Vidal C, Nieto-Zermeño J (2016) Pediatric inguinal hernia repair with a single-incision approach using an Endo Close™ suturing device. Surg Endosc 30(11):5134–5135
Li B, Nie X, Peng Y, Gong D, Xie Z, Mo Y, Xie H, Xu L (2016) Modified single-port laparoscopic herniorrhaphy for pediatric inguinal hernias: based on 3507 cases in China. Surg Endosc 20:S53
Ahmed H, Youssef MK, Salem EA, Fawzi AM, Desoky EA, Eliwa AM, Sakr AM, Shahin AM (2016) Efficacy of laparoscopically assisted high ligation of patent processus vaginalis in children. J Pediatr Urol 12(50):e1–e5
Shalaby R, Ismail M, Shehata S, Gamaan I, Yehya A, Elsayaad I, Akl M, Shams A (2015) Shalaby technique for efficient single incision laparoscopic pediatric inguinal hernia repair. J Pediatr Surg 50:1995–2000
Yilmaz E, Afsarlar CE, Senel E, Cavusoglu YH, Karaman I, Karaman A, Ozguner IF (2015) A novel technique for laparoscopic inguinal hernia repair in children: single-port laparoscopic percutaneous extraperitoneal closure assisted by an optical forceps. Pediatr Surg Int 31:639–646
Wang Z, Xu L, Chen Z, Yao C, Su Z (2014) Modified single-port minilaparoscopic extraperitoneal repair for pediatric hydrocele: a single-center experience with 279 surgeries. World J Urol 32:1613–1618
Li S, Li M, Wong KK, Liu L, Tam PK (2014) Laparoscopically assisted simple suturing obliteration (LASSO) of the internal ring using an epidural needle: a handy single-port laparoscopic herniorrhaphy in children. J Pediatr Surg 49:1818–1820
Qi S (2013) Treatment of inguinal hernia in children with an umbilical single-incision laparoscopic percutaneous extraperitoneal closure using a syringe needle. J Laparoendosc Adv Surg Tech A 23:A103–A104
Xu C, Xiang B, Jin SG, Luo QC, Zhong L (2013) Transumbilical two-port laparoscopic percutaneous extraperitoneal closure: a new technique for inguinal hernia repair in children. J Laparoendosc Adv Surg Tech A 23:392–396
Kumar A, Ramakrishnan TS (2013) Single port laparoscopic repair of paediatric inguinal hernias: our experience at a secondary care centre. J Minim Access Surg 9:7–12
Li B, Nie X, Xie H, Gong D (2012) Modified single-port laparoscopic herniorrhaphy for pediatric inguinal hernias: based on 1,107 cases in China. Surg Endosc 26:3663–3668
Kimura T, Yamauchi K, Ihara Y, Sawai T, Kosumi T, Yonekura T (2012) Single-site laparoscopic herniorrhaphy using needle instruments for inguinal hernias in children: a novel technique. Surg Today 42:100–103
Kastenberg Z, Bruzoni M, Dutta S (2011) A modification of the laparoscopic transcutaneous inguinal hernia repair to achieve transfixation ligature of the hernia sac. J Pediatr Surg 46:1658–1664
Wang DJ, Qiu JG, Fang YQ, Si TJ, Luo JB, Gao X (2011) Laparoscopic extraperitoneal repair of symptomatic hydrocele in children: a single-center experience with 73 surgeries. J Endourol 25:1221–1225
Yamoto M, Morotomi Y, Yamamoto M, Suehiro S (2011) Single-incision laparoscopic percutaneous extraperitoneal closure for inguinal hernia in children: an initial report. Surg Endosc 25:1531–1534
Chang YT, Lee JY, Tsai CJ, Chiu WC, Chiou CS (2011) Preliminary experience of one-trocar laparoscopic herniorrhaphy in infants and children. J Laparoendosc Adv Surg Tech A 21:277–282
Shen W, Ji H, Lu G, Chen Z, Li L, Zhang H, Pan J (2010) A modified single-port technique for the minimally invasive treatment of pediatric inguinal hernias with high ligation of the vaginal process: the initial experience. Eur J Pediatr 169:1207–1212
Chang YT, Wang JY, Lee JY, Chiou CS (2009) A simple single-port laparoscopic-assisted technique for completely enclosing inguinal hernia in children. Am J Surg 198:e13–e16
Ozgediz D, Roayaie K, Lee H, Nobuhara KK, Farmer DL, Bratton B, Harrison MR (2007) Subcutaneous endoscopically assisted ligation (SEAL) of the internal ring for repair of inguinal hernias in children: report of a new technique and early results. Surg Endosc 21:1327–1331
Patkowski D, Czernik J, Chrzan R, Jaworski W, Apoznański W (2006) Percutaneous internal ring suturing: a simple minimally invasive technique for inguinal hernia repair in children. J Laparoendosc Adv Surg Tech A 16:513–517
Tatekawa Y (2012) Laparoscopic extracorporeal ligation of hernia defects using an epidural needle and preperitoneal hydrodissection. J Endourol 26:474–477
Shalaby R, Ismail M, Gouda S, Yehya AA, Gamaan I, Ibrahim R, Hassan S, Alazab A (2015) Laparoscopic management of recurrent inguinal hernia in childhood. J Pediatr Surg 50:1903–1908
Acknowledgements
This work was supported by the Natural Science Foundation of Ningbo Municipal Science and Technology Bureau-2016A610177.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Furan Wang has no conflicts of interest or financial ties to disclose.
Appendix
Appendix
PubMed
(“hernia, inguinal“[mh] OR hydrocele[mh] OR “inguinal hernia” OR “inguinal hernias” OR hydrocele OR hydroceles) AND (child[mh] OR infant[mh] OR adolescent[mh] OR child OR children OR infant OR infants OR baby OR babies OR pediatric OR pediatrics OR paediatric OR paediatrics OR adolescent OR adolescents) AND (laparoscopy[mh] OR laparoscopes[mh] OR laparoscopy OR laparoscopic OR coelioscopy OR coelioscopic OR celioscopy OR celioscopic OR peritoneoscopy OR peritoneoscopic OR endoscopy OR endoscopic OR laparoendoscopy OR laparoendoscopic OR minilaparoscopy OR minilaparoscopic OR laparoscope OR laparoscopes).
Embase
(‘inguinal hernia’/exp OR hydrocele/exp OR ‘inguinal hernia’ OR ‘inguinal hernias’ OR hydrocele OR hydroceles) AND (child/exp OR infant/exp OR adolescent/exp OR baby/exp OR child OR children OR infant OR infants OR baby OR babies OR pediatric OR pediatrics OR paediatric OR paediatrics OR adolescent OR adolescents) AND (laparoscopy/exp OR laparoscope/exp OR laparoscopy OR laparoscopic OR coelioscopy OR coelioscopic OR celioscopy OR celioscopic OR peritoneoscopy OR peritoneoscopic OR endoscopy OR endoscopic OR laparoendoscopy OR laparoendoscopic OR minilaparoscopy OR minilaparoscopic OR laparoscope OR laparoscopes).
Cochrane library
(“hernia, inguinal“[mh] OR hydrocele[mh] OR “inguinal hernia” OR “inguinal hernias” OR hydrocele OR hydroceles) AND (child[mh] OR infant[mh] OR adolescent[mh] OR child OR children OR infant OR infants OR baby OR babies OR pediatric OR pediatrics OR paediatric OR paediatrics OR adolescent OR adolescents) AND (laparoscopy[mh] OR laparoscopes[mh] OR laparoscopy OR laparoscopic OR coelioscopy OR coelioscopic OR celioscopy OR celioscopic OR peritoneoscopy OR peritoneoscopic OR endoscopy OR endoscopic OR laparoendoscopy OR laparoendoscopic OR minilaparoscopy OR minilaparoscopic OR laparoscope OR laparoscopes).
Rights and permissions
About this article
Cite this article
Chen, Y., Wang, F., Zhong, H. et al. A systematic review and meta-analysis concerning single-site laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia and hydrocele. Surg Endosc 31, 4888–4901 (2017). https://doi.org/10.1007/s00464-017-5491-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5491-3