Abstract
Background
Techniques for laparoscopic liver resection (LLR) have been developed over the past two decades. The aim of this study is to analyze the outcomes and trends of LLR.
Methods
203 patients underwent LLR between 2006 and 2015. Trends in techniques and outcomes were assessed dividing the experience into 2 periods (before and after 2011).
Results
Tumor type was malignant in 62%, and R0 resection was achieved in 87.7%. Procedures included segmentectomy/wedge resection in 64.5%. Techniques included a purely laparoscopic approach in 59.1% and robotic 12.3%. Conversion to open surgery was necessary in 6.4% cases. Mean hospital stay was 3.7 ± 0.2 days. 90-day mortality was 0% and morbidity 20.2%. Pre-coagulation and the robot were used less often, while the performance of resections for posteriorly located tumors increased in the second versus the first period.
Conclusion
This study confirms the safety and efficacy of LLR, while describing the evolution of a program regarding patient and technical selection. With building experience, the number of resections performed for posteriorly located tumors have increased, with less reliance on pre-coagulation and the robot.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since the description of laparoscopic liver resections (LLR) by Gagner et al. in 1992 [1], the volume of LLR has seen a dramatic increase. This advent of LLR has been accompanied by multiple reports describing improved postoperative benefits of reduced hospital stay, intraoperative blood loss, and postoperative complications compared to open hepatectomy [2]. Although LLR was initially described for the treatment of benign tumors and for peripherally located lesions, the techniques have developed significantly over the past two decades to broaden the applications. These include the expansion of LLR for resection of malignant tumors [3], an increased extent of resection to include major hepatectomies [4], and the introduction of robotic liver resection [5].
Despite the common benefit of smaller incisions, the techniques used for LLR are numerous, including radiofrequency assisted [6], stapler [7], hand assisted [8], and robotic assisted [5]. The usage of various techniques has introduced heterogeneity into the literature [9]. From a training point of view as well, it is unknown what techniques should be used early on during the start of a new LLR program and how the techniques should evolve over time. This is in contrast to training in conventional open liver resection where a given technique could be adapted, with minimal modification made over the career of a surgeon. It is also unknown if the perioperative outcomes of various techniques would be different.
At the authors’ institution, a LLR program was started in 2006. Earlier reports from this program have validated LLR by demonstrating improved perioperative parameters [10]. The aim of this study is to critically analyze this experience, with a focus of the evolution of our technique and its impact on perioperative outcomes.
Methods
This was an IRB-approved study. Since the beginning of the program in 2006, the patients were prospectively entered into an IRB-approved LLR database. Patients who underwent LLR between the advent of the program and December 2015 were reviewed. Patient demographics, disease characteristics, surgical technique, and perioperative outcomes were assessed by SPSS (SPSS v.17, SPSS Inc. Chicago, IL) using descriptive analysis. Trends in minimally invasive operative techniques and patient outcomes were assessed by dividing the experience into 2 periods (before and after December 2011) using student t and Chi-square tests. Additional analyses were performed by comparing the lesions based on their anterior (segments II, III, IVb, V, and VI) or posterior (segments VII, VIII, and IVa) location in the liver. Categorical values are expressed as percentages and continuous values are expressed as means ± SEM. Differences in values are deemed statistically significant when p ≤ 0.05.
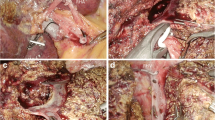
The procedures were done by a group of surgeons with experience in both advanced laparoscopic and conventional liver surgery. Laparoscopic procedures of four surgeons only (FA, CQ, JJF, and EB) were examined. The patients were candidates for LLR if they preferably presented with malignant tumors measuring <5 cm and benign tumors <8 cm. However, these criteria were expanded based on the discretion of surgeons over the course of the study. The tumors were selected for LLR if they were away from the hilum and hepatic vein-inferior vena cava junctions. The surgical techniques were described in earlier reports [10, 11]. Pre-coagulation was performed using either a bipolar (Habib, Angiodynamics, Latham, NY) or monopolar radiofrequency coagulator (Starburst XL, Angiodynamics, Latham, NY) as described before [12].
Results
There were a total of 203 study patients. Forty-seven per cent (n = 95) underwent LLR in the first (2006–2011) and 53% (n = 108) in the second period (2012–2015). Table 1 shows the demographic and clinical details of the patients. Patients in a wide range of age distribution were treated, with 60% being female. Seven percent (n = 15) of the patients had underlying cirrhosis. Two-thirds of the resections (n = 138) were done for malignancy, with colorectal cancer metastasis being the main indication (n = 84, 41.3%). The patients had an average of 1.4 tumors measuring 4.08 cm. When the two study periods were compared, there was no difference regarding patient demographics, indications and tumor characteristics, except for an increase in the percentage of lesions located in the posterior segments from 16 to 37% in the second versus the first period (p = 0.001) (Table 1).
Surgical approach was dominated by a purely laparoscopic approach in 59% (n = 120), followed by a hand-assisted approach in 28.6% (n = 58) and robotic resection in 12% (n = 25) of patients. The majority of resections were minor resections (91.1%, n = 185), with 6.4% (n = 13) conversion to open. Major hepatectomy was defined as the resection of three or more segments of the liver. The causes for conversion included bleeding in six patients, technical difficulties without being able to make progress laparoscopically in six patients, and diaphragmatic injury in one patient. The majority of the procedures were performed without inflow occlusion (94%, n = 190), and perioperative blood transfusions were done in 20 cases (9.9%). An R0 resection was achieved in 87.7% of the malignant cases (n = 123). The average hospital stay was 3.7 days, with 7.4% (n = 15) of patients being admitted to the intensive care unit postoperatively. The morbidity was 20.2%, with 0% 90-day mortality. Most of the complications were Clavien–Dindo [13] Class I (46.3%, n = 19), followed by class II (39%, n = 16), class III (9.8%, n = 4), and class IV (4.9%, n = 2). There was no difference between the 2 study periods regarding operative or perioperative parameters, except for a decrease in the utilization of pre-coagulation from 50 to 4% in the second period (p < 0.001) (Table 2).
When resections performed for posterior versus anterior tumors were compared, it was seen that operative time was longer (249.2 ± 16.2 vs. 199.7 ± 7.2 min, p = 0.007), with a higher, but statistically insignificant rate of conversion to open rate (11% vs. 5%, p = 0.118), similar hospital stay (3.6 ± 0.3 vs. 3.9 ± 0.3 days, p = 0.496) and morbidity (17% vs. 22%, p = 0.521). Anteriorly positioned tumors include those in segments II, III, IVb, V, and VI, while posteriorly positioned tumors include those located in segments VII, VIII, and Iva.
Discussion
This study describes the results of a LLR program at a tertiary center over a span of 10 years. In selected patients with resections performed predominantly for malignant tumors, R0 resection, morbidity, and mortality rates were comparable to the laparoscopic and open series in the literature [14–17]. One of our objectives was to see if any trends could be detected over time. According to the analyses, our surgical approach evolved from an initially pre-coagulation dependent technique to a more precise dissection with individual ligation/division of parenchymal structures over time. The acquisition of advanced laparoscopic skills that helped mimic open liver resection eventually enabled the program to expand the indications to more patients with posteriorly located tumors. As LLR requires the development of skills not acquired in open liver resection, surgeons use a variety of new techniques in laparoscopic surgery. There are also certain patient selection criteria involved, as the resection of each segment poses a different degree of challenge, which in magnitude is more much significant compared to that in open surgery. The result of this technical transformation can be seen in the literature with a heterogeneity of techniques reported [5–8]. To the best of our knowledge, this study is a unique attempt to define this transformation in LLR and to give an algorithm to surgeons interested in developing a successful laparoscopic program.
The first part of our experience can be characterized as a period when image quality in laparoscopic surgery was not as advanced as the current era, and although there were numerous options of energy devices for vessel ligation and division, none of them was the “ideal device” for hepatic parenchymal transection. Furthermore, the lack of articulation with rigid instruments made the control of bleeding difficult. At this point in time, the use of pre-coagulation and hand-assistance helped us perform laparoscopic resections more comfortably, while we became more familiar with instrumentation and acquired advanced skills for LLR. Once we developed the experience to perform most open liver resection maneuvers laparoscopically and put together a set of appropriate instrumentation that also included laparoscopic vascular clamps, we were able to transform our laparoscopic technique closer to open and hence reduce the need for pre-coagulation and expand the indications to more difficult segments of the liver.
The robot was used more frequently in the first part of the study. The marketed benefits of the robot, such as 3-D view and articulation [18], are useful in only certain parts of the procedure, and in the earlier robotic technology, there was not an articulating vessel sealer available. Since LLR is a very dynamic procedure, with the angle of exposure and type of surgical task changing very rapidly, as well as unpredictable occurrence of bleeding, we felt that the robot was inferior to the laparoscopic technique for liver resection. Therefore, it was used less often in the second part of the study. We believe that the role of the robot is limited to the resection of tumors where rigid instruments have a restricted reach (i.e., tumors located at the dome of the liver; i.e. segments 4A, 8 and 7) and to hilar dissection. Since the completion of this study, an articulating vessel sealer has become available with the robot. We are currently investigating whether this new tool may make the robot again attractive for liver resection.
A recent study comparing outcomes and costs of robotic and open hepatectomy demonstrated that higher perioperative costs were associated with robotic hepatectomy, however, it also was associated with a shorter LOS and significantly lower postoperative and direct hospital costs [19]. The cost of the robot, which was not calculated in this study, will need to be considered especially in the current era with a move towards more accountable health care organizations.
As reported in this study, posteriorly located tumors were not initially the main indication for LLR. With building experience though, the number of LLRs performed for these tumors has increased. Our results show that LLR for posterior hepatic tumors can be performed with a similar morbidity, albeit with a longer operative time compared to anterior tumors. As these are technically more difficult, the surgical team should be ready for conversion to open, which occurred 11% of the time, compared to 5% for anterior resections. Other groups have also reported on laparoscopic management of posterior hepatic tumors [20–22]. Although some groups have advocated transcostal trocars to facilitate resection of certain tumors, we have not required to do so. Hand-assistance or robotic instrumentation has helped us to perform these posterior resections.
In a recent review and meta-analysis of over 9000 laparoscopic liver resections, Ciria et al. have reported a mortality of 0.4% and a morbidity of 18.3%. In this series of minor and major resections, mean EBL was 375 ml, while perioperative blood transfusion was required in 8.3% of cases. Mean operative time was 216.7 min and hospital stay was 7.9 days [14]. Our experience compares favorably with these results.
Recent studies have documented that major liver resections are also being safely performed laparoscopically. Dagher et al. in a multicentric study of 210 major hepatectomies demonstrated the safety and feasibility of laparoscopic major hepatectomy. In this study, 64.8% of the procedures were right hepatectomies. Conversion to open surgery was required in 12.4, and 4.3% of patients received blood transfusions. Perioperative mortality was 1%, liver specific morbidity 8.1%, and general morbidity 13.8%. Median postoperative LOS was 6 days [4]. In the current study, 9% of our cohort underwent major liver resections. In our opinion, with building experience, a left hepatectomy should be attempted first, as it is a more straight-forward laparoscopic procedure. Right hepatectomy is the last frontier in a LLR program. The potential difficulties are related to the body habitus of the patients, where, either because of the size of the tumor or size of the liver, adequate exposure might not be possible. We use a hand-access port at the upper midline routine in these cases, which is also either used for specimen extraction or included in the Makuuchi incision, if converted to open.
In our study, other than demonstrating differences in patient selection and techniques, we did not demonstrate differences in other perioperative parameters. This is related to the fact that the procedures were performed by multiple surgeons, who were each incorporated into the study at different time points, limiting the ability to show improvements in these parameters over time. Nevertheless, the team approach has enabled the maintenance of the safety and oncologic metrics evenly throughout the course of the study.
In summary, this single-center, multi-surgeon study demonstrates the safety and feasibility of LLR while describing how our technique changed with experience. We believe that a review of how our program evolved over time can help other surgeons in building or expanding their LLR program. At our institution, LLR has become the procedure of choice over the open counterpart for minor liver resections. We are further expanding the program to perform more major resections and approach more challenging tumors laparoscopically.
References
Gagner M, Rheault M, Dubuc J (1992) Laparoscopic partial hepatectomy for liver tumor (abst). Surg Endosc 6:99
Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP (2011) Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 13:295–308. doi:10.1111/j.1477-2574.201100295.x
Parks KR, Kuo YH, Davis JM, O’Brien B, Hagopian EJ (2014) Laparoscopic versus open liver resection: a meta-analysis of long-term outcome. HPB (Oxford) 16:109–118. doi:10.1111/hpb.12117
Dagher I, O’Rourke N, Geller DA, Cherqui D, Belli G, Gamblin TC, Lainas P, Laurent A, Nguyen KT, Marvin MR, Thomas M, Ravindra K, Fielding G, Franco D, Buell JF (2009) Laparoscopic major hepatectomy: an evolution in standard of care. Ann Surg 250:856–860. doi:10.1097/SLA.0b013e3181bcaf46
Ho C, Wakabayashi G, Nitta H, Ito N, Hasegawa Y, Takahara T. Surg Endosc (2013) 27: 732. doi:10.1007/s00464-012-2547-2
Agcaoglu O, Aliyev S, Karabulut K, El-Gazzaz G, Aucejo F, Pelley R, Siperstein AE, Berber E (2013) Complementary use of resection and radiofrequency ablation for the treatment of colorectal liver metastases: an analysis of 395 patients. World J Surg 37:1333–1339. doi:10.1007/s00268-013-1981-1
Buell JF, Gayet B, Han HS, Wakabayashi G, Kim KH, Belli G, Cannon R, Saggi B, Keneko H, Koffron A, Brock G, Dagher I (2013) Evaluation of stapler hepatectomy during a laparoscopic liver resection. HPB (Oxford) 15:845–850. doi:10.1111/hpb.12043
Hasegawa Y, Koffron AJ, Buell JF, Wakabayashi G (2015) Approaches to laparoscopic liver resection: a meta-analysis of the role of hand-assisted laparoscopic surgery and the hybrid technique. J Hepatobiliary Pancreat Sci 22:335–341. doi:10.1002/jhbp.214
Alkhalili E, Berber E (2014) Laparoscopic liver resection for malignancy: a review of the literature. World J Gastroenterol 20:13599–13606. doi:10.3748/wjg.v20.i37.13599
Tsinberg M, Tellioglu G, Simpfendorfer CH, Walsh RM, Vogt D, Fung J, Berber E (2009) Comparison of laparoscopic versus open liver tumor resection: a case-controlled study. Surg Endosc 23:847–853. doi:10.1007/s00464-008-0262-9
Berber E, Akyildiz HY, Aucejo F, Gunasekaran G, Chalikonda S, Fung J (2010) Robotic versus laparoscopic resection of liver tumours. HPB (Oxford) 12:583–586. doi:10.1111/j.1477-2574.201000234.x
Akyildiz HY, Morris-Stiff G, Aucejo F, Fung J, Berber E (2011) Techniques of radiofrequency-assisted precoagulation in laparoscopic liver resection. Surg Endosc 25:1143–1147. doi:10.1007/s00464-010-1330-5
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. doi:10.1097/SLA.0b013e3181b13ca2
Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G (2016) Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann Surg 263:761–777. doi:10.1097/SLA.0000000000001413
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 236:397–406; discussion 406-7, doi:10.1097/01.SLA.000002900366466.B3
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250:831–841. doi:10.1097/SLA.0b013e3181b0c4df
Hallet J, Beyfuss K, Memeo R, Karanicolas PJ, Marescaux J, Pessaux P (2016) Short and long-term outcomes of laparoscopic compared to open liver resection for colorectal liver metastases. Hepatobiliary Surg Nutr 5:300–310. doi:10.21037/hbsn.2016.02.01
Giulianotti PC, Coratti A, Sbrana F, Addeo P, Bianco FM, Buchs NC, Annechiarico M, Benedetti E (2011) Robotic liver surgery: results for 70 resections. Surgery 149:29–39. doi:10.1016/j.surg.2010.04.002
Sham JG, Richards MK, Seo YD, Pillarisetty VG, Yeung RS, Park JO (2016) Efficacy and cost of robotic hepatectomy: is the robot cost-prohibitive? J Robot Surg. doi:10.1007/s11701-016-0598-4
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK, Jang JY, Choi H, Jang JS, Kwon SU (2016) Comparison of laparoscopic liver resection for hepatocellular carcinoma located in the posterosuperior segments or anterolateral segments: a case-matched analysis. Surgery 160:1219–1226
Teo JY, Kam JH, Chan CY, Goh BK, Wong JS, Lee VT, Cheow PC, Chow PK, Ooi LL, Chung AY, Lee SY (2015) Laparoscopic liver resection for posterosuperior and anterolateral lesions-a comparison experience in an Asian centre. Hepatobiliary Surg Nutr 4:379–390. doi:10.3978/j.issn.2304-3881.2015.06.06
Kazaryan AM, Rosok BI, Marangos IP, Rosseland AR, Edwin B (2011) Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc 25:3881–3889. doi:10.1007/s00464-011-1815-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Eren Berber, MD, is a consultant to Ethicon (Ethicon Inc.; Somerville, NJ) and Aesculap (Aesculap Inc. USA; Center Valley, PA). He received honoraria from Ethicon for these activities. Drs. Elshamy, Takahashi, Akyuz, Yazici, Yigitbas, Hammad, Aucejo, Quintini, Fung have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Elshamy, M., Takahashi, H., Akyuz, M. et al. Evolution of a laparoscopic liver resection program: an analysis of 203 cases. Surg Endosc 31, 4150–4155 (2017). https://doi.org/10.1007/s00464-017-5468-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5468-2