Abstract
Background
Compared to end-to-side anastomosis with a circular stapler, the overlap method is favored for intracorporeal esophagojejunostomy because it facilitates handling of the stapler, even in narrow spaces, and wider anastomosis. However, it associates with technical difficulties during anastomosis, including difficult traction on the esophageal stump that necessitates stay sutures. Here, we introduce a new modified overlap method that employs knotless barbed sutures (MOBS) and report the outcomes of our case series.
Method
All consecutive patients who underwent intracorporeal esophagojejunostomy in 2015–2016 were included. All patients underwent surgery as follows: After esophageal transection with a linear stapler, two V-loc 90 sutures (Covidien, Mansfield, MA, USA) were sutured in the center of the stapled line. The opening was made between the two threads, and the intraluminal space was identified. The jejunum was ascended toward the esophageal stump by inserting a 45-mm-long linear staple. The anastomosis was made at the space between the right and left crura. After firing the linear stapler, the entry hole was closed bidirectionally using the pre-sutured threads.
Results
Forty patients underwent MOBS (27 by laparoscopy; 13 by robot). Mean total operative and MOBS procedural times were 180.6 and 22.4 min, respectively. Mean hospital stay was 6.9 days. Two patients had major complications (5.0 %). There were no anastomosis-related complications. Laparoscopy and robot subgroups did not differ in mean MOBS procedural times (22.2 vs. 22.7 min, p = 0.787).
Conclusion
MOBS is a safe and feasible method that is a good option for intracorporeal esophagojejunostomy after laparoscopic gastrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic gastrectomy is an alternative treatment for early gastric cancer, and recent surgical advances have focused on minimizing its surgical complications. When a laparoscopic approach for gastric cancer first evolved, a mini-laparotomy on the epigastrium was required for gastric resection and reconstruction. However, due to recent improvements in laparoscopic techniques, gastrectomy has evolved into a totally laparoscopic procedure, namely all procedures are performed intracorporeally and a mini-laparotomy is not needed [1, 2].
Compared to previous procedures, totally laparoscopic gastrectomy associates with less blood loss and faster postoperative recovery [3]. It is also especially useful for patients with obesity because the intracorporeal procedure is less affected by obesity than extracorporeal anastomosis [4]. Nevertheless, totally laparoscopic total gastrectomy is still not popular compared to totally laparoscopic distal gastrectomy. This may largely reflect the technical difficulties associated with, and the poor reliability of, intracorporeal esophagojejunostomy [5].
The overlap method is one of the most favored reconstruction methods for intracorporeal esophagojejunostomy [6]. Compared to the end-to-side anastomosis method using a circular stapler, the overlap method offers a sufficient intraluminal area and easy handling of a stapler, even in a narrow space [7]. However, it has several technical shortcomings, as follows. First, it is difficult to obtain traction on the esophageal stump during the anastomosis; sometimes, a stay suture is needed to obtain traction. Second, there is a risk of unintended stapling of the left crus during the anastomosis. Third, additional stay sutures are needed to close the common entry hole.
Here, we present a novel surgical technique that overcomes these shortcomings. We have termed this method the ‘modified overlap method using knotless barbed sutures (MOBS)’ and report here the short-term outcomes of the patients who underwent this technique in our hospital.
Materials and methods
This retrospective study was approved by the institutional review board of Ajou University School of Medicine, Suwon, Korea (Approval no.: MED-MDB-16-21) and adhered to the principles of the Declaration of Helsinki and its revisions. All patients provided written informed consent to undergo the surgery.
Patients
All consecutive patients who underwent totally laparoscopic or robotic gastrectomy for upper third gastric cancer between April 2015 and January 2016 in our academic hospital were identified by retrospective analysis of the medical records. All data, including complications, were extracted from the prospectively maintained gastric cancer database.
General operative details
All surgeries were performed by a single experienced surgeon (Han SU), who has performed more than 1000 laparoscopic gastrectomies and 300 robotic gastrectomies before starting the MOBS procedure. Patients were placed in a supine reverse Trendelenburg position under general anesthesia. The five-port system was used for totally laparoscopic or robotic gastrectomy as follows. In totally laparoscopic gastrectomy, three 12-mm trocars were placed on the right and left lower abdomen and the infraumbilical area, and two 5-mm trocars were placed on the right and left upper abdomen (Fig. 1A). In robotic gastrectomy, two 12-mm trocars were placed on the left lower abdomen and the infraumbilical area, and three 8-mm trocars were placed on the right and left upper abdomen and the right lower abdomen (Fig. 1B). After the placement of the ports, the pneumoperitoneum was maintained between 10 and 13 mmHg during surgery. A liver traction was performed using a single thread as described previously [8]. An ultrasonically activated shears (Harmonic Scalpel, Ethicon, EndoSurgery, Cincinnati, OH, USA or Sonicision™, Covidien, Mansfield, MA, USA) was used for D1+ or D2 lymphadenectomy. An ultra-powered stapling system (iDrive™ and EndoGIA™, Covidien, Mansfield, MA, USA) and two 15-cm-long barbed threads (V-loc 90, Covidien, Mansfield, MA, USA) were used for the anastomosis.
Placement of the ports in the laparoscopic and robotic methods. A Three 12-mm and two 5-mm trocars were used for laparoscopic gastrectomy. B Two 12-mm and three 8-mm trocars were used for robotic gastrectomy. The left-hand trocars were placed lower than those in laparoscopic gastrectomy. This port placement can reduce the clash of robotic arms during the splenic hilar dissection and the esophagojejunostomy
Surgical procedure of MOBS
After the radical lymphadenectomy and complete gastric mobilization, a 60 mm length of purple cartilage was introduced through a 12-mm trocar (the right lower 12-mm trocar in laparoscopic surgery and the left lower 12-mm trocar in robotic surgery) and the distal esophagus was transected transversely. The resected specimen was delivered via the extended umbilical incision. The pneumoperitoneum was re-established after temporary closure of the umbilical incision using towel clips. After checking the free resection margins, an intracorporeal esophagojejunostomy was performed according to the following steps.
1. Two barbed threads are sutured on the stapled line of the esophageal stump. They are located on the middle portion of the esophageal stump 1 cm apart from each other (Fig. 2A). A too-narrow or too-wide distance between the two threads should be avoided because otherwise their locations become lateral angles of the common entry hole after firing of the linear stapler.
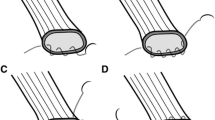
Steps of the modified overlap method using knotless barbed sutures for intracorporeal esophagojejunostomy. A Two barbed threads are sutured on the center of the stapled line of the esophageal stump about 1 cm apart from each other. B An entry hole for the anastomosis is made on the esophageal stump between the two barbed sutures using an ultrasonically activated shears. C The antero-posterior anastomosis is made using a 45-mm-long linear stapler at the space between the right and left crura. D The common entry hole is sutured bidirectionally using the pre-sutured barbed threads. E The roux and biliopancreatic limbs are separated by dividing the jejunum with a linear stapler
2. An opening is made on the esophageal stump using an ultrasonically activated shears (Fig. 2B). Theoretically, the stapled line should contain the anterior and posterior esophageal walls so that cutting the staple line means the anterior and posterior walls will be cut simultaneously. This will help the surgeons to readily identify the intraluminal space with a sufficient opening, and thus additional stay sutures to fix anterior or posterior wall are not required.
3. An anastomosis is made between the esophageal stump and the jejunum in the antero-posterior fashion (Fig. 2C). Prior to the esophagojejunostomy, sufficient esophageal stump should be prepared, especially in the posterior area of the esophageal stump. The anastomosis procedure starts with a jejunal opening that is made at the anti-mesenteric side of the jejunum and is about 15–20 cm away from the Treitz ligament. The cartilage jaw of a 45-mm-long purple-colored stapler is then introduced into the jejunum, and the jaws are closed. The stapler is then angled and ascended toward the axis of the esophageal stump. At this moment, the pre-sutured barbed threads should be pulled downward to reduce the tension on the jejunal mesentery. The staple is then slightly opened, and the anvil jaw is introduced gently into the esophagus via the space between the right and left crura.
4. After firing the stapler, the common entry hole is closed bidirectionally by hand sewing using the pre-sutured barbed threads (Fig. 2D). Since the pre-sutured barbed threads are located at lateral angles to the common entry hole, they function both as a landmark and the stay sutures during the closure of the common entry hole.
5. After completing the esophagojejunostomy, the roux limb and the biliopancreatic limb are separated by dividing the jejunum with a 60-mm-long tan-colored stapler (Fig. 2E). A side-to-side jejunojejunostomy is made with two 60-mm-long tan-colored staplers at the roux limb about 45–50 cm away from the esophagojejunostomy without mesentery division. The mesenteric defect between the roux and biliopancreatic limbs is then repaired using another barbed suture. The final appearance after the Roux-en-Y reconstruction is shown in Fig. 3.
Postoperative care
All patients were managed according to standardized clinical protocols after surgery, namely sips of water were allowed on the second postoperative day, a semi-fluid diet was permitted on the third, and a semi-pureed diet was allowed on the fourth. Discharge was recommended on the sixth postoperative day but was delayed if the patient had any medical problem or complication.
Statistical analysis
All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were expressed as number and percentage, while continuous variables were expressed as mean and SD. The patients were divided according to whether the surgical approach was laparoscopic or robotic, and the two groups were compared in terms of various variables using Chi-squared test, Fisher’s exact test, or Student’s t test. p values of <0.05 were considered to indicate statistical significance.
Results
In total, 40 patients underwent intracorporeal esophagojejunostomy with the MOBS method during the study period. Their demographic and clinical characteristics and surgical outcomes are summarized in Tables 1 and 2, respectively. The mean age was 60.6 years, and the patients were predominantly male (77.5 %). The mean body mass index was 23.6 kg/m2, and 23 patients had comorbidities at the time of the operation. Of the 40 patients, 27 (67.4 %) underwent laparoscopic gastrectomy and 13 (32.6 %) underwent robotic gastrectomy. In 35 (87.5 %), three (7.5 %), and two (5.0 %) patients, total gastrectomy, completion total gastrectomy, and proximal gastrectomy with double tract reconstruction was performed, respectively. The mean operative time and estimated blood loss were 180.6 min and 109.6 ml, respectively. The mean MOBS procedural time (defined by the time from suturing the barbed threads on the esophageal stump to the jejuna transection after esophagojejunostomy) was 22.4 min. The mean length of hospital stay was 6.9 days. Postoperative complications occurred in five patients (12.5 %). Two were major complications (grade ≥IIIa) (5.0 %). The latter two patients received percutaneous drainage for liver abscess (S5) and exhibited multifocal intra-abdominal fluid collection (subhepatic and pelvic area), respectively. However, there were no anastomosis-related complications such as leakage.
When the patients who underwent laparoscopic surgery were compared to the patients who underwent robotic surgery, the robot subgroup tended to have longer operation times (171.1 vs. 200.3 min). However, this trend did not achieve statistical significance (p = 0.065). Further differences in perioperative variables were also not observed (Table 3). Interestingly, the laparoscopic and robot groups also did not differ in terms of MOBS procedural time (22.2 vs. 22.7 min, p = 0.787). Moreover, as shown in Fig. 4, the MOBS procedural times of the 40 patients did not fluctuate sharply, unlike the total operation times.
Regarding long-term anastomotic complications, the follow-up endoscopy was conducted at postoperative 12 months (Fig. 5). Because the MOBS procedure was performed since April 2015, the anastomotic status was evaluated in 21 patients. Until now, there was no anastomotic stenosis, but one patient who had undergone laparoscopic proximal gastrectomy with double tract reconstruction showed mild esophagitis due to alkaline reflux.
Discussion
Although the first laparoscopic total gastrectomy for gastric cancer was reported in 1999, the procedure is still not widely accepted because of its technical difficulties and lack of information regarding its long-term outcomes [9]. In particular, the laparoscopic esophagojejunostomy method has not yet been standardized and its safety remains a challenging issue.
There are several methods that are used for reconstruction after laparoscopic total gastrectomy. They are classified into two major categories. One is the extracorporeal method in which a conventional open purse-string clamp, and a circular stapler is used through a mini-laparotomy on the epigastrium. This is quite similar to the conventional open procedure and was favored by many gastric surgeons in the early phase of laparoscopic gastrectomy. However, this method has some disadvantages, including poor visualization due to the narrow operative field and a limited angle of the direct view, excessive tension placed on the organs during the anastomosis, and difficulties in applying the purse-string clamp. These problems are even more pronounced for obese patients [7, 10].
As laparoscopic experience accumulates, the laparoscopic technique is moving toward a less invasive yet highly sophisticated procedure. The totally laparoscopic procedure has been adopted for total gastrectomy, so has intracorporeal esophagojejunostomy: All procedures from transection of the esophagus to closure of the entry hole are performed under a laparoscopic view without mini-laparotomy. Based on recently published reports, it seems that most surgeons perform intracorporeal esophagojejunostomy using circular or linear staplers. In terms of which method is superior, a recent review suggested that the circular stapler method associates with a significantly higher risk of leakage and stenosis of the esophagojejunostomy: The rates of leakage for the circular and linear stapler methods were 4.7 and 1.1 %, respectively (p < 0.001), while the rates of stenosis were 8.3 and 1.8 %, respectively (p < 0.001) [7]. However, the study was not a systematic review; rather, it was a literature review that included 23 retrospective studies and only two prospective studies from 2007 to 2013. Thus, definitive evidence for the superiority of the linear stapler method over the circular stapler method, or vice versa, is still lacking. Further research that clarifies which reconstruction method is optimal for intracorporeal esophagojejunostomy is required.
At present, the overlap method is one of the most favored linear stapler methods. It was first introduced by Inaba et al. [6] in 2010 and has several advantages over conventional end-to-side anastomosis using a circular stapler. In particular, stapler handling is easier, even in a narrow space, and stapling can be performed regardless of the diameter of the esophagus. Recently, several studies reported that the overlap method has favorable outcomes. In 2014, Morimoto et al. [11] reported the surgical outcomes of 77 patients who underwent the overlap method. They showed that the mean time needed to perform anastomosis was 36.3 (range 24–52) min and that the only anastomotic complication was a single case of stenosis (1.3 %). Similarly, in 2015, Kitagami et al. [12] reported the outcomes of their 100 consecutive cases where the overlap method was used. The mean anastomotic time was 32 (range 24–53) min, and there were no anastomosis-related complications. Notably, in 2013, Nagai et al. [13] reported the outcomes of a series of 94 patients who underwent laparoscopic total gastrectomy with esophagojejunostomy using a linear stapler device. In the first 37 cases, two anastomotic leakages occurred. By contrast, no anastomotic complications occurred in the 57 patients who underwent the modified method.
The overlap method that is currently being used has several technical shortcomings, namely difficulties obtaining traction on the esophageal stump that necessitate the use of an additional stay suture, the risk of unintended stapling of the left crus, and the need for an additional stay suture when closing the common entry hole. To overcome these problems, we applied two knotless barbed sutures on the middle of the esophageal stump. These sutures served both as stay sutures and as a landmark of the lateral angles of the common entry hole during the anastomosis. When these threads are pulled out as described in the present study, it becomes easy to retract the esophageal stump downwards and make an opening on it. They even reduce the mesentery tension during esophagojejunostomy. After making the anastomosis, we close the common entry hole with these threads bidirectionally: An additional stay suture, which is usually required in the conventional overlap method, is not required. Moreover, these threads are located at the lateral angles of the common entry hole, which means that the closure sutures can be placed securely. The present study showed that this technique was feasible in terms of operative time and complications. The mean procedural time for MOBS (i.e., the time from suturing the barbed threads on the esophageal stump to the jejunal transection after esophagojejunostomy) was 22.4 (range 13–43) min, which is shorter than the times for the overlap method that were reported previously. Moreover, there were no cases of anastomosis-related complications in our 40 patients. In addition, the MOBS procedural time was not affected by whether the laparoscopic or the robotic approach was used; it also did not fluctuate sharply between patients, unlike the total operative time.
Conclusions
Our results suggest that MOBS is a safe, feasible, and stable method for intracorporeal esophagojejunostomy. This novel technique would be a good alternative option for totally laparoscopic or robotic total gastrectomy.
References
Hur H, Han SU (2013) Totally laparoscopic surgery for gastric cancer. J Gastric Cancer 13:1–2
Woo J, Lee JH, Shim KN, Jung HK, Lee HM, Lee HK (2015) Does the difference of invasiveness between totally laparoscopic distal gastrectomy and laparoscopy-assisted distal gastrectomy lead to a difference in early surgical outcomes? A prospective randomized trial. Ann Surg Oncol 22:1836–1843
Zhang YX, Wu YJ, Lu GW, Xia MM (2015) Systematic review and meta-analysis of totally laparoscopic versus laparoscopic assisted distal gastrectomy for gastric cancer. World J Surg Oncol 13:116
Kim MG, Kim KC, Kim BS, Kim TH, Kim HS, Yook JH, Kim BS (2011) A totally laparoscopic distal gastrectomy can be an effective way of performing laparoscopic gastrectomy in obese patients (body mass index ≥30). World J Surg 35:1327–1332
Lee JH, Ahn SH, Park DJ, Kim HH, Lee HJ, Yang HK (2012) Laparoscopic total gastrectomy with D2 lymphadenectomy for advanced gastric cancer. World J Surg 36:2394–2399
Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, Uyama I (2010) Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 211:e25–e29
Umemura A, Koeda K, Sasaki A, Fujuwara H, Kimura Y, Iwaya T, Akiyama Y, Wakabayashi G (2015) Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg 38:102–112
Oh DK, Hur H, Kim JY, Han SU, Cho YK (2010) V-shaped liver retraction during a laparoscopic gastrectomy for gastric cancer. J Gastric Cancer 10:133–136
Azagra JS, Goergen M, De Simone P, Ibanez-Aguirre J (1999) Minimally invasive surgery for gastric cancer. Surg Endosc 13:351–357
Chen K, Pan Y, Cai JQ, Wu D, Yan JF, Chen DW, Yu HM, Wang XF (2016) Totally laparoscopic versus laparoscopic-assisted total gastrectomy for upper and middle gastric cancer: a single-unit experience of 253 cases with meta-analysis. World J Surg Oncol. doi:10.1186/s12957-016-0860-2
Morimoto M, Kitagami H, Hayakawa T, Tanaka M, Matsuo Y, Takeyama H (2014) The overlap method is a safe and feasible for esophagojejunostomy after laparoscopic-assisted total gastrectomy. World J Surg Oncol. doi:10.1186/1477-7819-12-392
Kitagami H, Morimoto M, Nakamura K, Watanabe T, Kurashima Y, Nonoyama K, Watanabe K, Fujihata S, Yasuda A, Yamamoto M, Shimizu Y, Tanaka M (2015) Technique of Roux-en-Y reconstruction using overlap method after laparoscopic total gastrectomy for gastric cancer: 100 consecutively successful cases. Surg Endosc. doi:10.1007/s00464-015-4724-6
Nagai E, Ohuchida K, Nakata K, Miyasaka Y, Maeyama R, Toma H, Shimizu S, Tanaka M (2013) Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery 153:732–738
Acknowledgments
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (1320270). The funding source had no role in the design of this article and will not have any role during its execution or publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Sang-Yong Son, Long-Hai Cui, Ho-Jung Shin, Cheulsu Byun, Hoon Hur, Sang-Uk Han, Yong Kwan Cho have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Son, SY., Cui, LH., Shin, HJ. et al. Modified overlap method using knotless barbed sutures (MOBS) for intracorporeal esophagojejunostomy after totally laparoscopic gastrectomy. Surg Endosc 31, 2697–2704 (2017). https://doi.org/10.1007/s00464-016-5269-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5269-z