Abstract
Background
Since the introduction of laparoscopic cholecystectomy (LC), there has been continued evolution in technique, instrumentation and postoperative management. With increased experience, LC has migrated to the outpatient setting. We asked whether increased availability and experience has impacted incidence of and indications for LC.
Methods
The New York (NY) State Planning and Research Cooperative System longitudinal administrative database was utilized to identify patients who underwent cholecystectomy between 1995 and 2013. ICD-9 and CPT procedure codes were extracted corresponding to laparoscopic and open cholecystectomy and the associated primary diagnostic codes. Data were analyzed as relative change in incidence (normalized to 1000 LC patients) for respective diagnoses.
Results
From 1995 to 2013, 711,406 cholecystectomies were performed in NY State: 637,308 (89.58 %) laparoscopic. The overall frequency of cholecystectomy did not increase (1.23 % increase with a commensurate population increase of 6.32 %). Indications for LC during this time were: 72.81 % for calculous cholecystitis (n = 464,032), 4.88 % for biliary colic (n = 31,124), 8.98 % for acalculous cholecystitis (n = 57,205), 3.01 % for gallstone pancreatitis (n = 19,193), and 1.59 % for biliary dyskinesia (n = 10,110). The incidence of calculous cholecystitis declined (−20.09 %, p < 0.0001) between 1995 and 2013; meanwhile, other diagnoses increased in incidence: biliary colic (+54.96 %, p = 0.0013), acalculous cholecystitis (+94.24 %, p < 0.0001), gallstone pancreatitis (+107.48 %, p < 0.0001), and biliary dyskinesia (+331.74 %, p < 0.0001). Outpatient LC incidence catapulted to 48.59 % in 2013, from 0.15 % in 1995, increasing >320-fold. Analysis of LC through 2014 revealed increasing rates of digestive, infectious, respiratory, and renal complications, with overall cholecystectomy complication rates of 9.29 %.
Conclusion
A shifting distribution of operative indications and increasing rates of complications should prompt careful consideration prior to surgery for benign biliary disease. For what is a common procedure, LC carries substantial risk of complications, thus requiring the patient to be an active participant and to share in the decision-making process.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In just over 30 years since its introduction, LC has rapidly evolved to become the most commonly performed general surgical procedure in the USA [1–3]. This unprecedented rate of adoption resulted in nearly 80 % of cholecystectomies being performed via a laparoscopic approach in NY State by 1996. As experience and comfort with the technique grew, LC came to be accepted as the surgical standard, continuing to grow into the ambulatory and outpatient settings as well. The increased availability and decreased burden of recovery following laparoscopic day surgery have led many to consider LC to now be a routine outpatient ambulatory surgery [4, 5], a perception that could easily predispose laxity of indications. In fact, the NIH warned against this very possibility in their 1993 consensus statement titled, “Gallstones and Laparoscopic Cholecystectomy,” stating that, “the availability of laparoscopic cholecystectomy should not expand the indications for gallbladder removal.” [6] Our aim was to examine first whether these changes have led to an increased frequency of LC and second whether they have led to a shift in operative indications for LC over time.
Methods
Following Institutional Review Board and NY State approval, the NY State Planning and Research Cooperative System (SPARCS) longitudinal administrative database was used to identify patients. SPARCS captures patient-level data from all inpatient hospital discharges and ambulatory surgery visits in NY State. Using ICD-9 procedure codes: 51.2, 51.21–51.24 prior to 2008 and CPT codes: 47,562–47564, 47570, 47600, 47605, 47610, 47612, 47620 after 2008, 713,996 records were identified for cholecystectomies performed from 1995 to 2013 (Table 1). When duplicate records were identified (1349 instances), one of the multiple records was randomly retained for analysis, and when internally discordant records, i.e., overlapping dates or different admission details, were identified (1241 instances), these records were excluded. Patient demographic characteristics were abstracted, as well as operative year, operative setting: inpatient/outpatient and priority: emergent/non-emergent status. Operative indication was determined by the primary diagnosis code associated with the procedure as follows: 575.1—acalculous cholecystitis, 574.1, 575.0, 574.0—calculous cholecystitis, 575.8—biliary dyskinesia, 577.0—gallstone pancreatitis, and 574.2—biliary colic (Table 2). Rates were expressed per 1000 patients undergoing cholecystectomy. Absolute change was determined by subtracting the yearly rate at 1995 from the yearly rate at 2013. Relative change was measured as a percentage and determined by the absolute change divided by the yearly rate at 1995. US Census Bureau annual population data from 1995 to 2013 were obtained and trend analysis completed using population incidences to correct for statewide population flux over the study years [7–9]. Complications data were extracted from NY SPARCS database for post-cholecystectomy readmissions between 1995 and 2014. ICD-9 codes were categorized prior to reporting as: infectious, cardiac, respiratory, thromboembolic, hemorrhagic, digestive, bile duct injury, retained gallstone, shock (non-septic, non-cardiogenic), surgical, transfusion reaction, wound complication, renal failure, hypertension, and neurologic. The five most frequent complication categories were included in trend analysis as detailed below.
Statistical analysis
The linear trend in the rate of cholecystectomy with different diagnosis over years was examined using log-linear Poisson regression models. Over-dispersion was checked and corrected for when needed. Relative risks (RR) with 95 % confidence interval were reported. A RR > 1 indicates an increasing pattern, while a RR < 1 suggests a decreasing pattern. All rates were calculated per 1000 patients undergoing LC, except date in Table 5, which was calculated per 100,000 NY State population with LC surgery. All analyses were performed in SAS 9.3 (SAS Institute Inc., Cary, NC), and significance level is set at p value <0.05.
Results
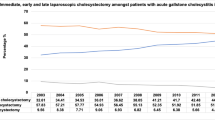
Over the 19-year period of study, from 1995 to 2013, 711,406 unique records were identified for cholecystectomies in NY State. Of these, 74,098 records (10.42 %) were performed via an open approach, while 637,308 records (89.58 %) were performed laparoscopically. Demographic and insurance payor class data are provided (Table 3). The overall increase in operative volume for cholecystectomy in NY State over this period was 410 cases (a 1.23 % increase) over the 19-year period of study. This rate of increase was not commensurate with the 6.32 % increase in population seen in NY State during this time [7–9]. Despite a stable operative volume, there has been a notable shift in operative approach with 94.37 % (31,753) of cholecystectomies being performed laparoscopically in 2013, increased from 78.10 % (25,957) in 1995. Similarly, there has been an increasing utilization of the outpatient setting for LC, with 48.59 % of LC being performed in the ambulatory context in 2013, up from 0.15 % in 1995 (Fig. 1). Interestingly, the majority of LC being performed in NY State is being done electively (58.1 %), with only 41.9 % being performed in an urgent fashion.
Not only did the technique and operative venue for LC evolve over time, but so did the distribution of operative indications. Calculous cholecystitis remained the major operative indication for LC throughout the period of study; however, its frequency has declined over time, with a relative change of −20.09 % over 19 years (p < 0.0001). At the same time, the rate of other diagnoses as operative indications has increased significantly (relative change reported), i.e., biliary colic (+54.96 %, p = 0.0013), acalculous cholecystitis (+94.24 %, p < 0.0001), gallstone pancreatitis (+107.48 %, p < 0.0001), and biliary dyskinesia (+331.74 %, p < 0.0001)) (Table 4).
In order to ensure changes in operative indications were not secondary to population flux, indications were also expressed as incidence per 100,000 NY State population (Table 5). Similar trends were seen with a declining rate of LC for calculous cholecystitis (−0.08 %, p = 0.0184) and increases in rates of LC for biliary colic (+0.78 %, p = 0.01), gallstone pancreatitis (+1.39 %, p < 0.0001), acalculous cholecystitis (+1.23 %, p = 0.001), and biliary dyskinesia (+3.97 %, p < 0.0001). Similarly, both in operations done electively and urgently there was a decrease rate of LC for calculous cholecystitis (−20.73 and −18.77 %), with increased rates of LC for biliary colic (+65.61 and 48.56 %), gallstone pancreatitis (+132.49 and +84.99 %), acalculous cholecystitis (+148.47 and +7.07 %), and biliary dyskinesia (+454.98 and +152.99). With the exception of urgent LC done for acalculous cholecystitis, p = 0.5044, the p value for all urgent and elective LC diagnoses was <0.0001.
Overall incidence of complications in cholecystectomy in our data set was 9.29 %, with digestive system complications being the leading complication category at 5.66 %, followed by infectious complications at 3.66 %, respiratory complications at 3.15 %, surgical complications at 1.71 %, renal complications at 1.01 %, and hemorrhage at 1.00 %. The top five complication categories following cholecystectomy were identified and analyzed for trends over the 20-year period.
Trends (relative risk) for the top five categories of LC complications were: digestive +47.10 %, infectious +42.21 %, respiratory +16.68 %, renal +1074.69 %, and surgical −16.27 %. Trends (relative risk) for the top five categories of open cholecystectomy complications were: digestive +169.08 %, infectious +84.75 %, respiratory +43.50 %, surgical +223.43 %, and hemorrhage +130.56 %. With the exception of surgical complications in the LC group, p = 0.7595, all identified trends were statistically significant with a p value <0.0001.
Discussion
This, along with its migration to the outpatient setting has led to the perception of LC as a low-risk, routine, and outpatient procedure. As a result, cholecystectomy is currently the fourth most common ambulatory surgery performed in the USA and the most commonly performed operation in general surgery across operative settings [2, 3]. Early on, there was concern that rates of cholecystectomy would rise after the adoption of a minimally invasive approach [4–6]; several series subsequently demonstrated increased rates of cholecystectomy beginning in the mid-1990s. Steiner et al. [10] showed a 28 % increase in volume in the state of Maryland over just an 8-year period. Meanwhile, Norwegian data demonstrated a more remarkable rise in the rate of cholecystectomy, 52.94 % over the 12 years spanning 1992–2002, with subsequent studies showing an even more impressive 72.58 % increase over the 22 years between 1990 and 2011 [5, 11]. Though an increased rate of cholecystectomy was not evidenced in our series, a universal decline in the rates of LC for calculous cholecystitis was noted, with an increase in rates of LC for all other diagnoses. One reason for this finding is very early adoption of LC in NY State, as evidenced by a 1994 study demonstrating a 28.12 % increase in volume of cholecystectomies in NY State in the four years spanning 1990–1993 [12]. Similarly, early adoption was demonstrated in a Pennsylvania HMO-based study, with a 59.26 % increase in cholecystectomy between 1988 and 1992 [13]. Thus, an increase in volume of cholecystectomy may have occurred several years prior to the start of our study.
The trends in distribution of operative indications are clearly demonstrated in our data. What is seen is a decrease in rates of LC for calculous cholecystitis and increased rates for less acute pathologies. The importance of this shifting distribution of diagnoses is its implication for assessing the risk/benefit ratio for LC. Despite conceptions that LC is a routine and low-risk procedure, several groups, including our own, have demonstrated inherent risks of the operation. Though the benefits of LC were initially tempered by concerns over bile duct injury, these concerns have not been borne out in the current era. Modern studies demonstrate that the rate of bile duct injury in LC now equals that of open cholecystectomy [14]. Together, the benefits of a laparoscopic approach with similar risk profile to conventional open surgery have made LC a more attractive option for both the physician and patient.
Though the dreaded complication of bile duct injury is felt not to be significantly different between either laparoscopic or open approaches, the risk is finite, as are the risks of other more common complications. While hemorrhage or renal complications only occur in approximately 1 % of cases, respiratory complications occur in 3.15 % of procedures, with infectious complications occurring at a rate of 3.66 % and complications involving the digestive tract affecting 5.66 % of cases. In fact, the likelihood of developing any postoperative complication following cholecystectomy is 1 in 11 operations (9.29 %). These findings are consistent with data from the Swedish GallRiks registry, which demonstrated complication rates of 6.1 % for elective cholecystectomy and 1 in 9 rate of complication for urgent cholecystectomy (11.2 %) [10]. Though LC may be a common procedure, given the rate of complication, it should not be considered routine, as there is a significant risk of postoperative complication inherent to the procedure. Even with minimally invasive surgery that drastically decreases operative mortality, increases in operative volume can easily eliminate the strides in incidence of mortality from a population standpoint. This was illustrated in 1994, when Steiner et al. reported that operative mortality for cholecystectomy had decreased significantly (33 %) in the state of Maryland; however, due to the increased rate of LC (28 %), the total number of deaths secondary to cholecystectomy did not decline. Similarly, we demonstrate significant rise in the rates of infectious, respiratory, and digestive complications in cholecystectomy, with significant increase in the rates of renal complications with LC and both hemorrhage and surgical complications with open cholecystectomy.
The decision for surgery must carefully weigh the risk and benefit of the proposed operation. Our data demonstrate a shifting distribution of operative indications and an increasing rate of peri- and postoperative complications. Taken together, this should prompt patients and physicians alike to reassess operative indications for cholecystectomy. Despite its benefits over traditional open cholecystectomy, LC, if performed for looser indications, rather than a more restrictive, defined set of indications, can still result in significant risk of morbidity. As such, not only is preoperative counseling and consent required, but the patient must be an active participant in shared decision making for elective LC for benign biliary disease.
The change in the distribution of operative indications seen may reflect a shift in disease prevalence, patient factors affecting presentation, evolving practice patterns, and even changing third-party payor policies. The ~20 % decline in calculous cholecystitis as an operative indication may reflect increased rates of operation for symptomatic cholelithiasis, thereby decreasing the prevalence of gallstones (and gallbladders) which would otherwise put patient at risk of developing calculous cholecystitis [15]. The rate of LC for the diagnoses of: Biliary colic, gallstone pancreatitis, acalculous cholecystitis, and biliary dyskinesia demonstrated a steadily rising rate, with the frequency of operation for biliary dyskinesia demonstrating the most remarkable rise among all indications.
A full discussion of the clinical phenotype of biliary dyskinesia and the relevant criteria is beyond the scope of the current study. The entity is broad and it vaguely defined, encompassing a phenotype that entails a functional disorder of the gallbladder, delineated by international consensus utilizing the Rome Foundation criteria, currently in its fourth iteration [16]. The utility of LC for treatment of biliary dyskinesia remains debated widely, with existing meta-analyses suggesting potential efficacy of LC for biliary dyskinesia, based upon the limited data available [17, 18]. Additionally, complicating the determination of efficacy is the lack of a discrete diagnostic code for functional gallbladder disease. Most studies, such as ours, utilize ICD-9 code 575.8 for other specified diseases of the gallbladder, of which approximately 81 % reflect the diagnosis of biliary dyskinesia [19]. Despite these global concerns regarding the diagnosis, our data mirror previous findings demonstrating substantial increases in the rate of cholecystectomy for biliary dyskinesia in the USA. Cholecystectomy for biliary dyskinesia is predominantly a US phenomenon, with rates disproportionately higher than other western nations. Preston et al. [20] demonstrated that operative rates for biliary dyskinesia are >340 % that of referenced nations, identifying a >200 % increase in the operative rate for biliary dyskinesia in the USA between 1991 and 2011. Thus the >330 % increase in operative rate seen in our series is consistent with prior data.
The reason(s) for the nationwide rise in biliary dyskinesia remains unclear, and while patient and physician factors may play a role, consideration must also be given to evolving practice patterns in the diagnosis and treatment of biliary pathology. The increased availability and utilization of HIDA scan as a diagnostic adjunct [21, 22] may play a role in the increased diagnosis of depressed gallbladder ejection fraction. Other considerations include changes in third-party payor reimbursement policies, such as coverage for biliary dyskinesia as an operative indication.
It is prudent to mention that due to our use of an administrative database lacking clinical data, there are inherent constraints. Without radiographic or pathologic data, patients with the diagnosis of “biliary dyskinesia” may in fact have a pathologic, instead of a functional diagnosis. Recent data suggest that up to 87 % of patients with a preoperative diagnosis of biliary dyskinesia have pathology consistent with chronic cholecystitis, while 42 % may have calculous disease in the form of small stones and sludge that is not identified on preoperative imaging evaluation [23, 24]. In comparing the rates of LC for biliary dyskinesia in the USA with international cohorts, the healthcare system of the cohort nation must also be considered. In the study by Preston et al., besides the USA, all other studied nations had a government healthcare system; inherent in this structure of healthcare delivery are queues for both diagnostics and procedures. Thus, the diagnostic disparity seen in the USA regarding biliary dyskinesia may be secondary to lower thresholds, and/or smaller preoperative queues, rather than a difference in incidence of pathology.
Though the lack of pathologic data limits determination of the patient’s true diagnosis, the reported encounter diagnosis does reflect the motivation for surgery, providing insight into trends in operative indications. Additional limitations include the inability to capture cholecystectomies that were initiated using a laparoscopic approach and later converted to an open approach. As a result, certain diagnoses, namely calculous cholecystitis may be underreported. However, in a separate analysis of open cholecystectomies during the study period, this concern is not borne out. As with the LC population, a similar decline in calculous cholecystitis is demonstrated in the open cholecystectomy group (−28.59 %, p < 0.0001), with increased rates of: gallstone pancreatitis (+31.14 %, p < 0.0001), acalculous cholecystitis (+128.14 %, p = 0.0020), biliary colic (+143.93 %, p < 0.0001), and biliary dyskinesia (+888.38 %, p < 0.0001).
As the composition of our population continues to change, a better understanding of the distribution of pathology is useful in determining the timing and role for cholecystectomy in the management of benign biliary pathology. With further population-based analyses of healthcare utilization and societal costs, determining the optimal timing for and clarifying the indications for cholecystectomy will become of increased health and economic import.
References
Centers for Disease Control and Prevention. National Center for Health Statistics. (2016) Health data interactive. www.cdc.gov/nchs/hdi.htm. Accessed 11 Mar 2016
National Center for Health Statistics (2015). Health, United States, 2014: with special feature on adults aged 55–64. Hyattsville, MD. Accessed 11 Mar 2016
Wier LM, Steiner CA, Owens PL (2015) Surgeries in hospital-owned outpatient facilities, 2012. HCUP statistical brief #188. February 2015. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb188-Surgeries-HospitalOutpatient-Facilities-2012.pdf. Accessed 11 Mar 2016
Pulvirenti E, Toro A, Gagner M, Mannino M, Di Carlo I (2013) Increased rate of cholecystectomies performed with doubtful or no indications after laparoscopy introduction: a single center experience. BMC Surg. doi:10.1186/1471-2482-13-17
Talseth A, Lydersen S, Skjedlestad F, Hveem K, Edna TH (2014) Trends in cholecystectomy rates in a defined population during and after the period of transition from open to laparoscopic surgery. Scand J Gastroenterol. doi:10.3109/00365521.2013.853828
NIH Consensus Conference (1993) Gallstones and laparoscopic cholecystectomy. JAMA 269(8):1018–1024
Table 1. Annual Estimates of the Resident Population for the United States, Regions, States, and Puerto Rico: April 1, 2010 to July 1, 2014 (NST-EST2014-01); Source: U.S. Census Bureau, Population Division; Release Date: December 2014; Accessed 20 June 2016. https://www.census.gov/popest/data/state/totals/2014/tables/NST-EST2014-01.csv
Table 2. Intercensal Estimates of the Resident Population by Sex and Age for New York: April 1, 2000 to July 1, 2010 (ST-EST00INT-02-36); Source: U.S. Census Bureau, Population Division; Release Date: October 2012; Accessed 20 June 2016. https://www.census.gov/popest/data/intercensal/state/tables/ST-EST00INT-02/ST-EST00INT-02-36.csv
Table CO-EST2001-12-00 – Time Series of Intercensal State Population Estimates: April 1, 1990 to April 1, 2000; Source: Population Division, U.S. Census Bureau; Release Date: April 11, 2002; Accessed 20 June 2016. https://www.census.gov/popest/data/intercensal/st-co/files/CO-EST2001-12-00.pdf
Steiner CA, Bass EB, Talamini MA, Pitt HA, Steinberg EP (1994) Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med 330(6):403–408
Enochsson L, Thulin A, Osterberg J, Sandblom G, Persson G (2013) The swedish registry of gallstone surgery and endoscopic retrograde cholangiopancreatography (GallRiks): a nationwide registry for quality assurance of gallstone surgery. JAMA Surg 148(5):471–478. doi:10.1001/jamasurg.2013.1221
Nenner RP, Imperato PJ, Rosenberg C, Ronberg E (1994) Increased cholecystectomy rates among Medicare patients after the introduction of laparoscopic cholecystectomy. J Commun Health 19(6):409–415
Legorreta AP, Silber JH, Costantino GN, Kobylinski RW, Zatz SL (1993) Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. JAMA 270(12):1429–1432
Halbert C, Pagkratis S, Yang J, Meng Z, Altieri MS, Parikh P, Pryor A, Talamini M, Telem DA (2015) Beyond the learning curve: incidence of bile duct injuries following laparoscopic cholecystectomy normalize to open in the modern era. Surg Endosc. doi:10.1007/s00464-015-4485-2
Stinton LM, Shaffer EA (2012) Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 6(2):172–187. doi:10.5009/gnl.2012.6.2.172
Cotton PB, Elta GH, Carter CR, Pasricha PJ, Corazziari ES (2016) Rome IV. Gallbladder and sphincter of Oddi disorders. Gastroenterology. doi:10.1053/j.gastro.2016.02.033 [Epub ahead of print]
Ponsky TA, Desagun R, Brody F (2005) Surgical therapy for biliary dyskinesia: a meta-analysis and review of the literature. J Laparoendosc Adv Surg Tech A 15:439–442
Gurusamy KS, Junnarkar S, Farouk M, Davidson BR (2009) Cholecystectomy for suspected gallbladder dyskinesia. Cochrane Database Syst Rev 21(1):CD007086. doi:10.1002/14651858.CD007086
Bielefeldt K (2013) The rising tide of cholecystectomy for biliary dyskinesia. Aliment Pharmacol Ther 37(1):98–106. doi:10.1111/apt.12105 [Epub 2012 Oct 28]
Preston JF, Diggs BS, Dolan JP, Gilbert EW, Schein M, Hunter JG (2015) Biliary dyskinesia: a surgical disease rarely found outside the United States. Am J Surg. doi:10.1016/j.amjsurg.2015.01.003
Richmond BK, DiBaise J, Ziessman H (2013) Utilization of cholecystokinin cholescintigraphy in clinical practice. J Am Coll Surg. doi:10.1016/j.jamcollsurg.2013.02.034
Ziessman HA (2012) Sincalide cholescintigraphy–32 years later: evidence-based data on its clinical utility and infusion methodology. Semin Nucl Med. doi:10.1053/j.semnuclmed.2011.10.002
Dave RV, Pathak S, Cockbain AJ, Lodge JP, Smith AM, Chowdhury FU, Toogood GJ (2015) Management of gallbladder dyskinesia: patient outcomes following positive 99 m technetium (Tc)-labelled hepatic iminodiacetic acid (HIDA) scintigraphy with cholecystokinin (CCK) provocation and laparoscopic cholecystectomy. Clin Radiol. doi:10.1016/j.crad.2014.12.006
Shaffer E (2003) Acalculous biliary pain: new concepts for an old entity. Dig Liver Dis 35(Suppl 3):S20–S255
Acknowledgments
We would like to acknowledge statistical consultation and support from the Biostatistical Consulting Core at the School of Medicine, Stony Brook University. Additionally, we would also like to acknowledge input and guidance in study planning from Stony Brook University’s Surgical Outcome Analysis Research (SOAR) Collaborative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Vamsi Alli, Jie Yang, Andrew Bates, and Mark Talamini and Ms. Jianjin Xu have no conflicts of interest. Dr. Aurora Pryor serves as a consultant for Apollo, Intuitive and Freehold Medical, is an investigator with Baronova and Obalon, and serves as a speaker for Ethicon and Gore. Dr. Dana Telem serves as a consultant for Medtronic, Gore and Ethicon and receives research support from Cook and Surgiquest.
Rights and permissions
About this article
Cite this article
Alli, V.V., Yang, J., Xu, J. et al. Nineteen-year trends in incidence and indications for laparoscopic cholecystectomy: the NY State experience. Surg Endosc 31, 1651–1658 (2017). https://doi.org/10.1007/s00464-016-5154-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5154-9