Abstract
Background
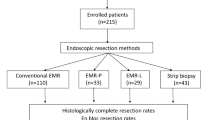
Various endoscopic techniques for rectal carcinoid tumors have been developed recently. In this study, we compared the outcomes of conventional endoscopic mucosal resection (EMR), strip biopsy, and EMR after circumferential precutting (EMR-P).
Methods
From March 2004 to July 2014, the medical records of 188 patients (190 rectal carcinoid tumors) who were treated with an endoscopic procedure for rectal carcinoid tumors were investigated retrospectively. The characteristics of the patients and tumors, the selection of the treatment method, the rate of complete resection, and the rate of complications were analyzed retrospectively.
Results
Forty-seven, 75 and 68 cases of EMR, strip biopsy and EMR-P were performed, respectively. The mean procedure time was not significantly different between the EMR, strip biopsy and EMR-P cases (5.6, 6.5 and 7.4 min, respectively, P = 0.119). En bloc resection was achieved in most of the cases (97.8, 98.7 and 95.5 % in the EMR, strip biopsy and EMR-P cases, respectively). However, histologic examination showed positive lateral or deep resection margins in 57 out of 190 cases (30.0 %). Multivariate analysis showed that the strip biopsy and EMR-P methods were independent factors for pathologic complete resection (negative in both lateral and deep resection margins), with odds ratios for margin involvement of 0.20 and 0.43 with 95 % confidence intervals from 0.08 to 0.47 and 0.19 to 0.96, respectively. In all the follow-up cases (81 of 190, 42.6 %), no local recurrence or distal metastasis was found.
Conclusions
Compared to conventional EMR, strip biopsy and EMR-P had a lower risk of incomplete resection. The procedure time and complication rate did not differ between the three groups, and no recurrence was detected during the follow-up period. Strip biopsy and EMR-P are safe and effective methods for the treatment of rectal carcinoid tumors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Rectal carcinoid tumors are one of the most common neuroendocrine tumors found in the gastrointestinal tract [1]. Recently, the incidence of rectal carcinoid tumors has increased due to the increase in detection from widespread colonoscopy screening. Most of the rectal carcinoid tumors are small in size [2]. Rectal carcinoid tumors smaller than 10 mm in size have a low risk of lymph node or distant metastasis [3–5]. Rectal carcinoid tumors that are detected early on are good candidates for endoscopic resection [4, 6, 7].
There are several methods that can be used in the resection of rectal carcinoid tumors, including conventional endoscopic mucosal resection (EMR), modified EMR such as endoscopic mucosal resection using a cap (EMR-C) and endoscopic mucosal resection after circumferential precutting (EMR-P) [8].
Recently, the endoscopic submucosal dissection (ESD) method has been widely adopted by many centers, and its use in the resection of rectal carcinoid tumors is increasing [9]. ESD is a very attractive method in terms of its high rates of en bloc and complete resection [10–16]. On the other hand, ESD has a high risk of complications, especially when the endoscopist is not well trained. Moreover, in Korea, the use of the IT-knife in the ESD procedure for rectal lesions is not covered by the national health insurance, so there are some limitations in performing ESD in rectal carcinoid tumors.
In this study, we compared conventional EMR, strip biopsy and EMR-P to determine which one is the most efficient in achieving the complete resection of rectal carcinoid tumors. We compared retrospectively the outcomes of the three different resection methods and their complication rates and procedure times.
Materials and methods
Patients
The records of 188 patients (190 lesions) with rectal carcinoid tumors who were treated with an endoscopic procedure in a tertiary medical center from March 2004 to July 2014 were reviewed retrospectively. The characteristics of the patients and tumors, the selection of the treatment method, the rate of complete resection and the rate of complications were analyzed. The study protocol was defined in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of the Seoul National University Bundang Hospital (IRB No. B-1504-294-114).
Endoscopic techniques
The resection of rectal carcinoid tumors was performed with one of the following methods: EMR or strip biopsy or EMR-P. The majority of the endoscopic procedures (178 of the 190, 93.7 %) were done by four experienced, expert endoscopists: endoscopist A (80 cases), B (39 cases), C (33 cases) and D (26 cases). The method used for resection was chosen depending on the personal preference of the endoscopist.
EMR
A single-channel endoscopy (CF-H260, Olympus Co, Tokyo, Japan) was used for the EMR of rectal carcinoid tumors. An indigo-carmine-mixed hypertonic saline solution (1 cc of epinephrine added to 100 cc of 0.9 % normal saline with a small amount of indigo-carmine) was injected into the submucosal layer to lift it off the muscle layer. After the submucosal layer was lifted off the muscle layer, the lesion was snared (with an asymmetrical polypectomy snare, MTW-Endoskopie, Wesel, Germany) and resected with an Endocut Q current generated with a VIO300D electrosurgical unit (ERBE, Tuebingen, Germany) (Fig. 1).
EMR-P
A submucosal cushion under the tumor was made by injecting an indigo-carmine-mixed hypertonic saline solution (1 cc epinephrine added to 100 cc of 0.9 % normal saline with a small amount of indigo-carmine) with the same single-channel endoscopy (CF-H260, Olympus Co, Tokyo, Japan) used for EMR. Then, a circumferential incision (precutting) was made 5–10 mm away from the tumor with the tip of the same snare used in the conventional EMR (asymmetrical polypectomy snare, width X = 25 mm, MTW-Endoskopie, Wesel, Germany). The flex knife and IT-knife were not used in this procedure. Next, the tumor was anchored with the snare at the mucosal incision site and finally resected. The devices used in EMR-P were not different from the devices used in conventional EMR (Fig. 2).
EMR after circumferential precutting (EMR-P). Making of a submucosal cushion under the tumor (A), then circumferential incision (precutting) 5–10 mm away from the tumor, with the tip of the same snare used in the conventional EMR (asymmetrical polypectomy snare, MTW-Endoskopie, Wesel, Germany). The flex knife and IT-knife were not used in this procedure. B Next, anchor the snare around tumor at the mucosal incision site and finally resect the tumor (C, D). This method does not need any additional device compared with conventional EMR
Strip biopsy
A two-channel endoscope (GIF-2T 290, Olympus Co, Tokyo, Japan) was used for the strip biopsy. The carcinoid tumor was cushioned with the same injection fluid used in EMR and EMR-P and then lifted with grasping forceps. Once grasped, the tumor lesion was snared and resected with the same snare used in the conventional EMR (an asymmetrical polypectomy snare, width X = 25 mm, MTW-Endoskopie, Wesel, Germany) through a separate channel of the two-channel endoscope (Fig. 3).
Evaluation of the pathology, procedure time and complications from the procedures
All the specimens were examined by an experienced pathologist for histopathologic type, size, depth of invasion, lymphovascular invasion, differentiation, deep resection margin and lateral resection margin. En bloc resection means the lesion was resected in one piece, and complete resection means an en bloc resection with negative deep and lateral margins with no lymphovascular involvement. The procedure time was defined as the time from submucosal injection to total resection of the tumor. Immediate and delayed bleeding or perforation was considered a complication related to the procedure.
Statistical analysis
Means were reported with standard deviations. Student’s t test was conducted for continuous variables, and Chi-square test was used to calculate categorical variables. Univariate analysis was done to identify variables that affect the complete resection rate, and multivariate logistic regression method was used for the prediction of complete resection. A p value of <0.05 was considered statistically significant. SPSS version 19.0 for windows (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
From March 2004 to July 2014, the medical records of 188 patients (190 rectal carcinoid tumors) who were treated with an endoscopic procedure for a rectal carcinoid tumor were investigated retrospectively. We performed 47, 75 and 68 cases of EMR, strip biopsy and EMR-P, respectively. The clinical characteristics of the patients in the three groups are presented in Table 1. The mean age was 47.4 years (range 28–78 years), and the number of male patients was 115 (60.5 %). The mean tumor size was 5.1 ± 2.4 (1.0–14.0) mm, and the mean distance from the anal verge was 7.0 ± 3.2 (1.0–22.0) cm. The three groups did not differ in gender, age and tumor size but differed in tumor location (distance from the anal verge) and in the ratio of incomplete resection (positive in either lateral or deep resection margin). The mean procedure time was 5.6, 6.5 and 7.4 min for EMR, strip biopsy and EMR-P, respectively, which did not differ significantly among the three groups (P = 0.119, Fig. 4A). Endoscopic en bloc resection was achieved in most of the cases (97.8 % in EMR, 98.7 % in strip biopsy and 95.5 % in EMR-P). However, histologic examination showed incomplete resection in 57 out of 190 cases (30.0 %, Fig. 4B, C). The rate of histopathologic complete resection in EMR, strip biopsy and EMR-P was 51.1, 82.7 and 69.4 %, respectively (P = 0.002).
Comparison of the endoscopic treatment methods for rectal carcinoid tumors. Operative time did not differ significantly in the three groups (EMR, strip biopsy, EMR-P group) (A). Lateral resection margin involvement rate was not significantly different between three groups (B). Deep resection margin involvement rate was different between three groups (P < 0.001 for EMR vs. strip biopsy, P = 0.008 for EMR vs. EMR-P, C)
Univariate analysis showed that male gender and resection technique influenced the complete resection of a carcinoid tumor (Table 2). There was no significant difference in the margin status between the four major operators (P > 0.05). Compared to EMR, strip biopsy and EMR-P were independent factors of complete resection with adjusted odds ratios (ORs) of 0.20 and 0.43, and 95 % confidence intervals (CIs) for margin involvement of 0.08–0.47 and 0.19–0.96, respectively (P < 0.001, Table 3).
There were no perforations or acute bleeding that required an emergency operation. However, delayed bleeding occurred in two patients: one in the EMR group and one in the strip biopsy group. All bleeding cases were controlled with conservative treatment.
Follow-up data were available for 81 of the 190 (42.6 %) patients: 25 of the 47 (53.2 %) in the EMR group, 34 of the 75 (45.3 %) in the strip biopsy group and 22 of the 68 (32.4 %) in the EMR-P group. Endoscopic examinations and CT scans showed that there were no local recurrences or metastasis in any of the patients in any of the groups during a median follow-up period of 12.1 months (range 3.7–55.3 months).
Discussion
The incidence of rectal carcinoid tumors is rising due to the increase in detection from widespread colonoscopy screening. Most of the carcinoid tumors are found in a small sized, asymptomatic state during endoscopic screening [2]. Rectal carcinoid tumors confined to the submucosal layer and a size <10 mm in diameter without atypical features and lymphovascular invasion are known to have a low risk of metastasis [3–5]. These tumors can be managed by endoscopic resection [4, 6, 7].
There are several endoscopic techniques that can achieve complete resection of rectal carcinoids. These include conventional EMR, endoscopic mucosal resection using band ligation (EMR-L), EMR-C, strip biopsy and ESD [8]. Many studies have compared the rate of complete resection of these modalities and their associated complications [8, 17–21]. Most of them [modified EMR (EMR-C and EMR-L) or ESD] have shown a superiority over the conventional EMR method in terms of the histologically complete resection rate.
Recently, ESD has become a familiar procedure at many centers, and the ESD technique is now widely used in many colorectal endoscopic resection procedures. ESD is also becoming a popular procedure in the endoscopic resection of rectal carcinoid tumors [9]. There have been many reports emphasizing the high success rate of en bloc and complete resection with the ESD procedure [10–16]. In one prospective study, compared with EMR, ESD resulted in a higher histologically complete resection rate (90.3 vs. 71.0 % for ESD and EMR, respectively, P = 0.035) and had a similar complication rate (P > 0.05) [13]. A recent meta-analysis showed that ESD is a better treatment modality than that of EMR for rectal carcinoid tumors in terms of the complete resection rate (complete resection rate of 52–84.6 % in the EMR group and 77.8–100 % in the ESD group) [11]. However, the ESD technique is more difficult to learn than that of conventional EMR, and if the endoscopist is not well skilled, there could be a higher chance for complications. Moreover, in Korea, using the IT-knife in rectal carcinoid resection is not covered by the national health insurance, which limits the adoption of the ESD procedure in the treatment of rectal carcinoid tumors. In such circumstances, performing an effective resection of rectal carcinoid tumors with the EMR technique is inevitable.
In this study, we compared three different EMR methods to determine which one would be the best to treat early rectal carcinoid tumors: conventional EMR, EMR-P and strip biopsy. EMR-P and strip biopsy were effective treatment modalities without any severe complications. Our results show that there was no significant difference between conventional EMR and strip biopsy and EMR-P in terms of the procedure time, procedure-related complications and success rate for en bloc resection (all P > 0.05, Table 1). In addition, both strip biopsy and EMR-P were superior to conventional EMR in terms of the pathologic complete resection rate (OR 0.20, 95 % CI 0.08–0.47 comparing strip biopsy with EMR; OR 0.43, 95 % CI 0.19–0.96 comparing EMR-P with EMR, Table 3). According to our data, there was neither local recurrence nor distant metastasis during the follow-up, regardless of the procedure techniques used, which was consistent with other previous studies.
Although ESD seems to be a highly effective technique to achieve en bloc and complete resection, our study shows that modified EMR such as EMR-P and strip biopsy also have reliable success rates for en bloc and complete resection. Several studies have insisted that modified EMR techniques are easier and safer than that of ESD and that they are not inferior to ESD in terms of the complete resection rate [17, 19, 22, 23]. For example, in one study, the complete resection rates in the ESD and EMR-L groups were 80.6 % (25 of 31) and 82.8 % (24 of 29), respectively (P = 0.833) [19]. Similarly, another study reported that the complete resection rate was 84.6 % (22 of 26) for strip biopsy and 77.8 % (7 of 9) for ESD [17]. Recently, one meta-analysis reported that modified EMR is as efficient as ESD [21]. However, all the studies included in this meta-analysis were retrospective ones with small sample sizes, and the quality of the studies was relatively low. Additionally, there was heterogeneity between the studies which could influence the results. Therefore, further studies are necessary to clarify this issue.
There was no difference in the complete resection rate between the operators; however, their preference was different for the procedure used. For example, endoscopist A (80 cases) in this study performed more EMR-P (49 cases) cases than strip biopsy (7 cases) cases, with a complete resection rate of 77.6 and 57.1 %, respectively, showing superior results in the EMR-P cases (P = 0.013). On the other hand, endoscopist B (39 cases) had more cases of strip biopsy (22 cases) than cases of EMR-P (15 cases) with a complete resection rate of 90.9 and 46.7 %, respectively, showing that strip biopsy was more effective (P = 0.008). Endoscopist D (26 cases) did not use the EMR-P method. We suggest that the optimal method for rectal carcinoid resection should be chosen based on the skill of the operator and his/her preference.
Our study has some limitations. The sample size was not large enough to allow for definitive conclusions. Second, because this was a retrospective study, the sample size of each technique could not be randomized equally. Additionally, all the cases did not undergo regular controlled follow-up visits. As a result, only 42.6 % of all the cases were evaluated for local recurrence or distant metastasis. In this study, a total of 57 cases had positive lateral or deep margins in their histologic findings, and 15 out of 57 incomplete resection cases did not have regular follow-up visits. However, 42 incomplete resection cases had regular checkups at our center, and they did not show any remnant lesions in the follow-up endoscopic evaluations 3–12 months after the procedure. As mentioned above, rectal neuroendocrine tumors with sizes smaller than 1 cm are known to have very little chance of lymph node metastasis [3–5]. Therefore, the limitation of having 15 cases without follow-up visits would not have a great effect on the final conclusion.
In conclusion, EMR-P or strip biopsy is an effective treatment method for rectal carcinoid tumor resection. While ESD is an effective method that achieves complete resection of rectal carcinoid tumors, it has a steep learning curve making it difficult to become skillful in the ESD technique, and when the endoscopist is not proficient in the procedure, severe complications can occur. Additionally, the procedure time is generally longer in the ESD procedure than in EMR. It may be more efficient to perform EMR-P or strip biopsy for rectal carcinoid tumor resection rather than ESD because modified EMR methods have similar success rates and fewer complications compared to the ESD technique.
References
Modlin IM, Sandor A (1997) An analysis of 8305 cases of carcinoid tumors. Cancer 79(4):813–829
Scherubl H, Kloppel G (2009) Rectal carcinoids on the rise-update. Z Gastroenterol 47(4):365–371
Shields CJ, Tiret E, Winter DC, International Rectal Carcinoid Study G (2010) Carcinoid tumors of the rectum: a multi-institutional international collaboration. Ann Surg 252(5):750–755
Al Natour RH, Saund MS, Sanchez VM, Whang EE, Sharma AM, Huang Q, Boosalis VA, Gold JS (2012) Tumor size and depth predict rate of lymph node metastasis in colon carcinoids and can be used to select patients for endoscopic resection. J Gastrointest Surg 16(3):595–602
Fujimoto Y, Oya M, Kuroyanagi H, Ueno M, Akiyoshi T, Yamaguchi T, Muto T (2010) Lymph-node metastases in rectal carcinoids. Langenbecks Arch Surg 395(2):139–142
Lin HH, Lin JK, Jiang JK, Lin CC, Lan YT, Yang SH, Wang HS, Chen WS, Lin TC, Liang WY, Chang SC (2014) Clinicopathological analysis of colorectal carcinoid tumors and patient outcomes. World J Surg Oncol 12:366
Kwaan MR, Goldberg JE, Bleday R (2008) Rectal carcinoid tumors: review of results after endoscopic and surgical therapy. Arch Surg 143(5):471–475
Choi HH, Kim JS, Cheung DY, Cho YS (2013) Which endoscopic treatment is the best for small rectal carcinoid tumors? World J Gastrointest Endosc 5(10):487–494
Saito Y, Otake Y, Sakamoto T, Nakajima T, Yamada M, Haruyama S, So E, Abe S, Matsuda T (2013) Indications for and technical aspects of colorectal endoscopic submucosal dissection. Gut Liver 7(3):263–269
Hamada Y, Tanaka K, Tano S, Katsurahara M, Kosaka R, Noda T, Aoki M, Toyoda H, Takei Y, Katayama N (2012) Usefulness of endoscopic submucosal dissection for the treatment of rectal carcinoid tumors. Eur J Gastroenterol Hepatol 24(7):770–774
Zhong DD, Shao LM, Cai JT (2013) Endoscopic mucosal resection vs endoscopic submucosal dissection for rectal carcinoid tumours: a systematic review and meta-analysis. Colorectal Dis 15(3):283–291
Moon SH, Hwang JH, Sohn DK, Park JW, Hong CW, Han KS, Chang HJ, Oh JH (2011) Endoscopic submucosal dissection for rectal neuroendocrine (carcinoid) tumors. J Laparoendos Adv Surg Tech A 21(8):695–699
Park HW, Byeon JS, Park YS, Yang DH, Yoon SM, Kim KJ, Ye BD, Myung SJ, Yang SK, Kim JH (2010) Endoscopic submucosal dissection for treatment of rectal carcinoid tumors. Gastrointest Endosc 72(1):143–149
Zhou PH, Yao LQ, Qin XY, Xu MD, Zhong YS, Chen WF, Ma LL, Zhang YQ, Qin WZ, Cai MY, Ji Y (2010) Advantages of endoscopic submucosal dissection with needle-knife over endoscopic mucosal resection for small rectal carcinoid tumors: a retrospective study. Surg Endosc 24(10):2607–2612
Zhou PH, Yao LQ, Xu MD, Chen WF, Zhong YS, Gao WD, He GJ, Qin XY (2007) Endoscopic submucosal dissection for rectal carcinoid tumors. Zhonghua Wei Chang Wai Ke Za Zhi 10(4):319–322
Onozato Y, Kakizaki S, Ishihara H, Iizuka H, Sohara N, Okamura S, Mori M, Itoh H (2007) Endoscopic submucosal dissection for rectal tumors. Endoscopy 39(5):423–427
Onozato Y, Kakizaki S, Iizuka H, Sohara N, Mori M, Itoh H (2010) Endoscopic treatment of rectal carcinoid tumors. Dis Colon Rectum 53(2):169–176
Kim YJ, Lee SK, Cheon JH, Kim TI, Lee YC, Kim WH, Chung JB, Yi SW, Park S (2008) Efficacy of endoscopic resection for small rectal carcinoid: a retrospective study. Korean J Gastroenterol 51(3):174–180
Choi CW, Kang DH, Kim HW, Park SB, Jo WS, Song GA, Cho M (2013) Comparison of endoscopic resection therapies for rectal carcinoid tumor: endoscopic submucosal dissection versus endoscopic mucosal resection using band ligation. J Clin Gastroenterol 47(5):432–436
Kim KM, Eo SJ, Shim SG, Choi JH, Min BH, Lee JH, Chang DK, Kim YH, Rhee PL, Kim JJ, Rhee JC, Kim JY (2013) Treatment outcomes according to endoscopic treatment modalities for rectal carcinoid tumors. Clin Res Hepatol Gastroenterol 37(3):275–282
He L, Deng T, Luo H (2015) Efficacy and safety of endoscopic resection therapies for rectal carcinoid tumors: a meta-analysis. Yonsei Med J 56(1):72–81
Niimi K, Goto O, Fujishiro M, Kodashima S, Ono S, Mochizuki S, Asada-Hirayama I, Konno-Shimizu M, Mikami-Matsuda R, Minatsuki C, Yamamichi N, Koike K (2012) Endoscopic mucosal resection with a ligation device or endoscopic submucosal dissection for rectal carcinoid tumors: an analysis of 24 consecutive cases. Dig Endosc 24(6):443–447
Zhao ZF, Zhang N, Ma SR, Yang Z, Han X, Zhao YF, Gao F, Gong ZJ, Yang L (2012) A comparative study on endoscopy treatment in rectal carcinoid tumors. Surg Laparosc Endosc Percutan Tech 22(3):260–263
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hyun Joo Lee, Seong Beom Kim, Cheol Min Shin, A. Young Seo, Dong Ho Lee, Nayoung Kim, Young Soo Park and Hyuk Yoon have no conflicts of interest or financial ties to disclose.
Additional information
Hyun Joo Lee and Seong Beom Kim have equally contributed to this work.
Rights and permissions
About this article
Cite this article
Lee, H.J., Kim, S.B., Shin, C.M. et al. A comparison of endoscopic treatments in rectal carcinoid tumors. Surg Endosc 30, 3491–3498 (2016). https://doi.org/10.1007/s00464-015-4637-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4637-4