Abstract
Background
Training in laparoscopic surgery is important not only to acquire and improve skills but also avoid the loss of acquired abilities. The aim of this single-centre, prospective randomized study was to assess skill acquisition of different laparoscopic techniques and identify the point in time when acquired skills deteriorate and training is needed to maintain these skills.
Methods
Sixty surgical novices underwent laparoscopic surgery (LS) and single-incision laparoscopic surgery (SILS) baseline training (BT) performing two validated tasks (peg transfer, precision cutting). The novices were randomized into three groups and skills retention testing (RT) followed after 8 (group A), 10 (group B) or 12 (group C) weeks accordingly. Task performance was measured in time with time penalties for insufficient task completion.
Results
92 % of the participants completed the BT and managed to complete the task in the required time frame of proficiency. Univariate and multivariate analyses revealed that SILS (P < 0.0001) and precision cutting (P < 0.0001) were significantly more difficult. Males performed significantly better than females (P < 0.005). For LS, a deterioration of skills (comparison of BT vs RT) was not identified; however, for SILS a significant deterioration of skills (adjustment of BT and RT values) was demonstrated for all groups (A–C) (P < 0.05).
Discussion
Our data reveal that complex laparoscopic tasks (cutting) and techniques (SILS) are more difficult to learn and acquired skills more difficult to maintain. Acquired LS skills were maintained for the whole observation period of 12 weeks but SILS skills had begun to deteriorate at 8 weeks. These data show that maintenance of LS and SILS skills is divergent and training curricula need to take these specifics into account.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimally invasive surgery has become widely used and integrated in routine surgical practice. Single-incision laparoscopic surgery (SILS) technique is an example for the trend towards even less invasive surgical procedures. This represents a unique challenge for surgical training. In standard laparoscopic (LS) procedures, the ports are placed in a triangular fashion. The target organ should be 15–20 cm from the central camera port and the remaining working trocars should ideally be placed on either side of the camera port. This allows the surgeon to work at a 60°–90° angle and triangulation is the most efficient and comfortable position for a laparoscopic procedure. Furthermore, standard laparoscopic operative technique has been proven to be more intuitive when compared to SILS procedures [1]. SILS technique, on the other hand, with its one port access offers cosmetic benefits for patients and may lead to reduced postoperative pain [2]. The use of several instruments through one port results in a technically more challenging operation because the well-established principle of laparoscopic triangulation is not possible. Special manoeuvrability of the instruments is needed to facilitate the SILS procedure because all instruments are inserted in the same axis. Therefore, articulating intersecting instruments have been developed which lead to an inverse triangulation; the surgeon’s right hand holds the left-sided instrument and vice versa.
Not all skills acquired by conventional laparoscopic surgery are transferable to SILS [3]. Several case series have demonstrated the presence of a significant learning curve for trained laparoscopic surgeons acquiring SILS technique [4, 5].
The establishment of new surgical techniques is time consuming. In addition, adequate training must be guaranteed for patient’s safety. Focused training outside of operating theatres is needed, especially for SILS, to prevent longer operating times and increased rates of conversion when operating on patients. In a previously published study by our group [6], we were able to show that participants maintained their acquired SILS skills after 4 weeks without training; however, these skills were lost when retested after 12 weeks.
The aim of this study was to optimise our laparoscopic training curriculum by identifying the point in time when acquired laparoscopic skills deteriorate and training is needed to maintain these skills. We have trained and retested surgical novices not only for SILS but also for standard laparoscopic procedures to assess ideal training programmes for standard and complex laparoscopic skills and evaluate differences in skill maintenance between these different techniques.
Methods
A single-centre, prospective randomized study was conducted at The Queen Elizabeth Hospital in Adelaide between July and November 2014. The study has been approved by the Human Research Ethics Committee (TQEH/LMH/MH).
The primary endpoint was definition of the time point of skill deterioration. The aim was to assess when training needs to be repeated to avoid loss of acquired skills and if the different techniques (standard laparoscopy vs SILS) display different time periods of skill maintenance without training.
The assessment of tasks with different complexity (peg transfer vs precision cutting), gender differences, influence of non-surgical skills were secondary endpoints of our study.
Medical students and Interns at the University of Adelaide without LS or SILS exposure participated in this study. All participants had an interest in a surgical speciality and agreed to the assessment and publication of their results.
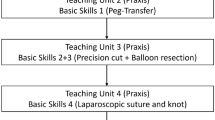
Training was conducted as a single afternoon session including an introduction tutorial on LS and SILS techniques, equipment handling, and a repetition of the course tasks. Before starting the training, participants completed a questionnaire assessing age, gender, previous exposure to surgery and non-surgical skills such as computer games, use of chopsticks and musical instruments. Previous experience was rated subjectively on a 5-point Likert scale, with 1 indicating no experience and 5 indicating very experienced.
Students were randomized into three groups (A, B and C) by picking a sealed envelope. The training curriculum was identical in all groups apart from the duration of time between baseline training (BT) and retention testing (RT). Group A returned to RT after 8 weeks, group B after 10 weeks and group C after 12 weeks of BT completion. Between BT and RT, participants had no access to the simulation facilities or exposure to LS/SILS procedures. BT was conducted by the first author (SME) and RT by a different author (TR) who had no information about the participant’s randomisation to exclude investigator related bias.
The setup and tasks have been described in detail in our previous study [6]. Briefly, Fundamentals of Laparoscopic Surgery (FLS) box trainers (modified for SILS) were used for both laparoscopic methods (LS, SILS) and tasks (peg transfer, precision cutting). Participants needed to reach previously defined [6] proficiency levels at baseline training (<240 s for peg transfer, <420 s for precision cutting) and both tasks were scored for efficiency (time) and precision. Penalties were applied for specific errors or lack of precision.
Statistics were conducted by senior statistician SH. A sample size of n = 20 for each group was calculated to be adequate. The data were analysed using a linear mixed effects model, with subject treated as a random factor. A log transformation was applied to the outcome measure (time) to normalise the distribution of this measure in order to meet the assumptions of a linear mixed effect model. The data were transformed back to the original scale prior to reporting with the effects representing the ratio of two geometric means. Multivariate analysis commenced with a saturated model which included all variables with a P value of <0.20. Non-significant variables were systematically removed from the model until a model containing only significant variables remained. All analyses were completed using SAS 9.3 (SAS Institute Inc, Cary, NC, USA).
A subgroup analysis was performed on the retest data to determine whether subsequent performance depended on the length of the retest interval. The effects task (cutting vs peg) and equipment (SILS vs LS) were evaluated separately to assess trends in performance over retest were dependent on these measures. This was accomplished by assessing retest by task and retest by equipment interactions.
Results
General findings
Sixty medical students were enrolled and randomized into three groups. 92 % of the participants completed the BT and managed to complete the task in the required time frame of proficiency. There were no significant differences in the demographic characteristics of the groups. There was also no statistically significant difference in the distribution of the potential confounders (e.g. previous laparoscopic experience) between the two groups (data not shown).
Comparison of training periods (BT vs RT) and techniques (LS vs SILS)
For LS, a deterioration of skills was not identified. The participants performed significantly better at RT in all groups: mean time to completion was 1.64, 1.93, and 1.86 times higher at baseline compared to retest after 8, 10, and 12 weeks, respectively.
For SILS, however, a significant deterioration of skills was demonstrated for all groups (A-C) (P < 0.05) (Fig. 1; Table 1).
Multivariate analysis
In general, the completion of tasks took longer at baseline when compared to the retest (MR = 1.20; P < 0.01), and when the technique [(SILS) (MR = 1.55; P < 0.0001)] or the task [cutting (MR = 1.42: P < 0.0001)] were more complex. Females took significantly longer (12 %) to complete the tasks than males (MR = 1.12; P < 0.01).
The multivariate analysis revealed that technique, task and gender are significant and independent predictors of time to complete the tasks (Table 2).
Discussion
Previous experience with the introduction of laparoscopic surgical techniques strongly suggests that well-structured, specific training programmes are a requirement to facilitate the development of technical skills in order to ensure optimal clinical outcomes [3]. Multiple papers have described SILS training programmes in varied detail, most without specific measurement of clinical outcomes and without specific consideration of time interval between SILS cases [7–10]. Whilst a number of studies have investigated potential differences in skill acquisition between LS and SILS techniques [11, 12], there is limited data investigating skill retention. An understanding of temporal skill degradation is imperative to designing a programme that optimises the maintenance of these skills to ensure that the achieved optimal clinical outcomes are perpetuated. Thus, the aim of this study was to assess skill acquisition of different laparoscopic techniques and clearly identify the point in time when acquired skills deteriorate and training is needed to maintain these skills.
Our participants were trained in conventional and single-incision laparoscopic surgery and acquired both skills. The final score [time to completion of the task including penalty] for BT was calculated by assessing all attempts the students needed to reach the level of proficiency, whilst RT scores were gathered via assessment of three consecutive runs of the tasks. Thus, similar results at BT and RT represent the loss of acquired skills.
In previous studies of our group and others [6, 13–15], the deterioration of acquired laparoscopic skills without training has been demonstrated. For conventional laparoscopic surgery, Bonrath et al. [13] reported that a time period of 11 weeks between initial training and retesting resulted in significantly deteriorated skills. Recently we published our results for maintenance of acquired skills for SILS, demonstrating that acquired skills of surgical novices were well maintained after 4 weeks but significantly deteriorated after 12 weeks without training [6]. The data presented in this study further characterise the timeline of loss of attained skills in the absence of regular training, suggesting that whilst SILS skills are maintained for a period of 4 weeks there is a significant decline in ability demonstrable at 8 weeks and beyond. Subsequently, we recommend a maximum period of 4 weeks without training for maintenance of acquired SILS skills in laparoscopic novices.
Interestingly, there was no deterioration of skills identified within any group for LS techniques during the 12-week study period. This contrast to the results described above by Bonrath et al. [13] may be attributable to a potential synergistic effect of SILS training on LS skills, as suggested by results reported in previous studies. Santos et al. [1] observed that participants trained exclusively in SILS techniques performed equally well as those trained exclusively in LS techniques when assessed with LS tasks. They also observed that the reverse situation did not yield equal performance, with those trained in SILS techniques producing superior results in SILS tasks. Our participants received an augmented training programme including both SILS and LS skills, a feature that clearly differentiates our study design from previous studies. It is possible that this extended period of LS skill retention observed is attributable to a consolidatory or synergistic effect of SILS training.
The results of different studies to identify the ideal time point of laparoscopic training vary widely. For example, Stefanidis et al. [16] tried to identify the ideal training interval for proficiency-based laparoscopic suturing but failed to demonstrate an association between intertraining interval and change in performance during proficiency-based laparoscopic simulator training. In contrast, several studies showed a significant loss of skills when acquired skills were not retrained, e.g. loss of skills after 2 weeks [15], 11 weeks [13], 12 weeks [6] or 6 months [17]. These studies have to be considered with caution because some of the study designs have tested limited time points, such as baseline training and retesting at one single time point without assessing the performance status in the interim.
Our model is not ideal either. Probably it does not adequately represent the real-life situation in surgery because our students did not have any exposure to laparoscopic or SILS simulation or actual surgery between the initial training and retesting. In addition, there is growing evidence that spaced training (multiple training sessions with interruptions) is superior to massed training (training in one compact training session) [17, 18]. Nevertheless, we have chosen this setup because we wanted to imitate the scenario of being trained for a short time, e.g. 1-day training course abroad, and not being able to train and/or perform the acquired surgical skills in the operating theatre for some weeks. Taken together, the model clearly provides evidence for the need of re-training once surgeons have been away from training for some time (e.g. research, maternity/sick leave). Surgical trainees should be aware of the fact that continuous training in minimally invasive surgery is very important and train as much as possible to keep and improve acquired skills.
The finding that males showed significantly better results compared to females is in concordance with existing studies demonstrating that females seem to have inferior visual-spatial abilities when compared to males in laparoscopic suturing [19] and that males are able to complete tasks on the Minimally Invasive Surgical Trainer-Virtual Reality (MIST-VR) in less time than females [20].
In conclusion, our data reveal that once acquired, complex laparoscopic skills such as cutting and complex techniques such as SILS are more difficult to maintain than simpler laparoscopic skills. Acquired LS skills were shown to be maintained throughout the entire 12-week observation period, in contrast to SILS skills which were shown to have deteriorated significantly at an 8-week interval. We recommend that that the future development of SILS training curricula involves establishing continuous training programmes for novices and inexperienced surgeons based on these results.
References
Santos BF, Enter D, Soper NJ, Hungness ES (2011) Single-incision laparoscopic surgery (SILS) versus standard laparoscopic surgery: a comparison of performance using a surgical simulator. Surg Endosc 25(2):483–490
Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST (2011) The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg 254(6):933–940
Pucher PH, Sodergren MH, Singh P, Darzi A, Parakseva P (2013) Have we learned from lessons of the past? A systematic review of training for single incision laparoscopic surgery. Surg Endosc 27(5):1478–1484
Alevizos L, Brinkman W, Fingerhut A, Jakimowicz J, Leandros E (2012) Novice surgeons versus experienced surgeons in laparoendoscopic single-site (LESS) surgery: a comparison of performances in a surgical simulator. World J Surg 36(5):939–944
Santos BF, Reif TJ, Soper NJ, Hungness ES (2011) Effect of training and instrument type on performance in single-incision laparoscopy: results of a randomized comparison using a surgical simulator. Surg Endosc 25(12):3798–3804
Varley M, Choi R, Kuan K, Bhardwaj N, Trochsler M, Maddern G, Hewett P, Mees ST (2015) Prospective randomized assessment of acquisition and retention of SILS skills after simulation training. Surg Endosc 29(1):113–118
Khandelwal S, Wright AS, Figueredo E, Pellegrini CA, Oelschlager BK (2011) Single-incision laparoscopy: training, techniques, and safe introduction to clinical practice. J Laparoendosc Adv Surg Tech A 21(8):687–693
Muller EM, Cavazzola LT, Grossi JVM, Mariano MB, Morales C, Brun M (2010) Training for laparoendoscopic single-site surgery (LESS). Int J Surg 8(1):64–68
Wu AS, Podolsky ER, Huneke R, Curcillo PG (2010) Initial surgeon training for single port access surgery: our first year experience. Jsls 14(2):200–204
Stroup SP, Bazzi W, Derweesh IH (2010) Training for laparoendoscopic single-site surgery and natural orifice transluminal endoscopic surgery. BJU Int 106(6 Pt B):934–940
Lewis T, Aggarwal R, Kwasnicki R, Darzi A, Paraskeva P (2012) Does previous laparoscopic experience improve ability to perform single-incision laparoscopic surgery? Surg Endosc 26(5):1214–1219
Fransen SA, Mertens LS, Botden SM, Stassen LP, Bouvy ND (2012) Performance curve of basic skills in single-incision laparoscopy versus conventional laparoscopy: is it really more difficult for the novice? Surg Endosc 26(5):1231–1237
Bonrath EM, Weber BK, Fritz M, Mees ST, Wolters HH, Senninger N, Rijcken E (2012) Laparoscopic simulation training: testing for skill acquisition and retention. Surgery 152(1):12–20
Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB, Scott DJ (2005) Skill retention following proficiency-based laparoscopic simulator training. Surgery 138(2):165–170
Gallagher AG, Jordan-Black JA, O’Sullivan GC (2012) Prospective, randomized assessment of the acquisition, maintenance, and loss of laparoscopic skills. Ann Surg 256(2):387–393
Stefanidis D, Walters KC, Mostafavi A, Heniford BT (2009) What is the ideal interval between training sessions during proficiency-based laparoscopic simulator training? Am J Surg 197(1):126–129
Akdemir A, Zeybek B, Ergenoglu AM, Yeniel AO, Sendag F (2014) Effect of spaced training with a box trainer on the acquisition and retention of basic laparoscopic skills. Int J Gynaecol Obstet 127(3):309–313
Spruit EN, Band GP, Hamming JF (2015) Increasing efficiency of surgical training: effects of spacing practice on skill acquisition and retention in laparoscopy training. Surg Endosc 29(8):2235–2243
Donnon T, DesCoteaux JG, Violato C (2005) Impact of cognitive imaging and sex differences on the development of laparoscopic suturing skills. Can J Surg 48(5):387–393
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2003) Impact of hand dominance, gender, and experience with computer games on performance in virtual reality laparoscopy. Surg Endosc 17(7):1082–1085
Acknowledgments
The authors thank the Royal Australasian College of Surgeon (RACS) for loan of the two FLS box trainers and their substantial support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mr. Ellis, Dr Varley, Mr Howell, Dr Trochsler, Prof Maddern, Prof Hewett, Dr Runge and Dr Mees have no conflicts of interest or financial ties to disclose.
Additional information
Tina Runge and Soeren Torge Mees have contributed equally to the study.
Rights and permissions
About this article
Cite this article
Ellis, S.M., Varley, M., Howell, S. et al. Acquisition and retention of laparoscopic skills is different comparing conventional laparoscopic and single-incision laparoscopic surgery: a single-centre, prospective randomized study. Surg Endosc 30, 3386–3390 (2016). https://doi.org/10.1007/s00464-015-4619-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4619-6