Abstract
Introduction
Patients, clinicians and researchers seek an easy, reproducible and valid measure of postoperative recovery. The six-minute walk test (6MWT) is a low-cost measure of physical function, which is a relevant dimension of recovery. The aim of the present study was to contribute further evidence for the validity of the 6MWT as a measure of postoperative recovery after colorectal surgery.
Methods
This study involved a sample of 174 patients enrolled in three previous randomized controlled trials. Construct validity was assessed by testing the hypotheses that the distance walked in 6 min (6MWD) at 4 weeks after surgery is greater (1) in younger versus older patients, (2) in patients with higher preoperative physical status versus lower, (3) after laparoscopic versus open surgery, (4) in patients without postoperative complications versus with postoperative complications; and that 6MWD (5) correlates cross-sectionally with self-reported physical activity as measured with a questionnaire (CHAMPS). Statistical analysis was performed using linear regression and Spearman’s correlation. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) checklist was used to guide the formulation of hypotheses and reporting of results.
Results
One hundred and fifty-one patients who completed the 6MWT at 4 weeks after surgery were included in the analysis. All hypotheses tested for construct validity were supported by the data. Older age, poorer physical status, open surgery and occurrence of postoperative complications were associated with clinically relevant reduction in 6MWD (>19 m). There was a moderate positive correlation between 6MWD and patient-reported physical activity (r = 0.46).
Conclusions
This study contributes further evidence for the construct validity of the 6MWT as a measure of postoperative recovery after colorectal surgery. Results from this study support the use of the 6MWT as an outcome measure in studies evaluating interventions aimed to improve postoperative recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Major abdominal surgery evokes a physiologic stress and is associated with a period of disability. Patients commonly ask about the time it will take them to recover from surgery and return to their normal employment and leisure activities, and many perioperative innovations are said to “improve recovery” [1]. Yet little information is available for clinicians and researchers on how best to quantify recovery after surgery [2]. Recovery is a complex construct which comprises multiple dimensions of health (i.e., physical, mental and social) and follows a defined trajectory (a rapid deterioration of health status followed by a gradual return toward baseline) [3]. Length of stay (LOS) has been extensively used to measure recovery, as discharge from hospital presumes good pain control, ability to self-care, as well as tolerance of oral nutrition [4]. However, this measure is influenced by many nonclinical factors (e.g., surgeons’ preference and hospital tradition), and only captures the early phase of recovery. It is clear that patients are not fully recovered to their baseline status when they leave the hospital [3, 5] and full recovery takes weeks to months [6].
One key dimension of recovery is physical function, as it affects the ability to perform activities of daily living, return to work and resume social leisure life. The six-minute walk test (6MWT), which measures the total distance that a patient is able to walk in 6 min (six-minute walk distance, 6MWD), is a performance-based measure of functional walking capacity. This test was originally developed to assess exercise tolerance in patients with cardiac and respiratory diseases [7], but it is now extensively used in a variety of settings [8, 9]. As opposed to more sophisticated exercise tests [e.g., cardio-pulmonary exercise testing (CPET)], the 6MWT is simple, does not require expensive equipment or specialized personnel, and can be performed in nearly any clinical location [10]. Previous studies have demonstrated a positive correlation of the 6MWD with CPET results (i.e., VO2 max) in different surgical populations [11, 12].
A preliminary study supported the construct validity and responsiveness of the 6MWT as an indicator of recovery after colorectal surgery [13]. This study, however, relied on a limited number of patients undergoing exclusively open colorectal resection. At that time, minimally invasive surgery and standardized perioperative care protocols (i.e., enhanced recovery pathways) were not part of routine care, which significantly differs from current practice [14]. Validation of a measurement instrument is a continuous process of evidence accumulation in order to support the use of the tool in a variety of surgical populations and contexts. Therefore, the aim of the present study is to contribute further evidence for the validity of the 6MWT as a measure of postoperative recovery in patients undergoing elective colorectal surgery in the context of laparoscopy and an enhanced recovery program.
Materials and methods
Participants and setting
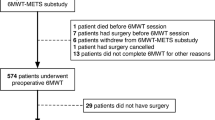
This validation study involved a sample of 174 patients enrolled in one published [15] and two recently completed randomized controlled trials (RCT) (ethics board approval codes 11-240-SDR and GEN11-004) aimed at investigating the role of nutrition and physical prehabilitation on recovery after colorectal surgery. These RCTs included adult patients scheduled for colorectal cancer resection at a university teaching hospital between September 2011 and September 2014. During this period, all patients were treated according to an enhanced recovery program as previously described [14]. Exclusion criteria were premorbid conditions that contraindicated patient exercise, and inability to speak English or French. Eligible consenting patients underwent preoperative assessment within 4 weeks of the scheduled operation completing baseline questionnaires, as well as biochemical and functional testing. Postoperative evaluations took place at 4 weeks after surgery. At both time points, patients performed the 6MWT and responded to a physical activity questionnaire [the Community Healthy Activities Model Program for Seniors (CHAMPS)]. Demographic and baseline patient characteristics including body mass index (BMI), comorbidities, American Society of Anesthesiologists (ASA) score, operative and postoperative parameters were also recorded. Patients converted from laparoscopic to open surgery were treated as open surgery patients in the analysis. Postoperative complications and hospital readmissions were recorded up to 30 days after surgery. Complication severity was graded according to the Clavien–Dindo classification [16]. Complications graded as III–V were defined as major.
Measures
Patients performed the 6MWT along a 15 m stretch of a flat corridor and were instructed to walk for 6 min at the pace that will make them feel tired. The hallway was marked with meter tacks, allowing a precise recording of the total distance covered by the patient in meters (m). Standardized encouragements were given minute-by-minute according to the guidelines by the American Thoracic Society [10]. Age- and sex-specific predicted 6MWD was calculated using the following formula: predicted distance walked in 6 min (m) = 868 − (age × 2.9) − (female × 74.7), where age is in years, and the value “1” is assigned for females and “0” assigned to males [7]. The minimal important difference (MID) for 6MWD (i.e., “the smallest change in an outcome measure perceived as beneficial by patients or physicians” [17]) has been estimated at 19 m for between-group comparisons in patients undergoing colorectal surgery [18].
The CHAMPS is a self-reported measure of physical activity. It comprises a 41-item questionnaire that was originally developed to assess the effectiveness of interventions aimed at increasing the level of physical activity in the elderly [19]. The frequency and time spent performing a range of physical and social activities during the past week are weighted according to the metabolic value of each activity. Total caloric expenditure per kilogram per week is then estimated. A previous study supported the validity of the CHAMPS as a measure of recovery of physical function after abdominal surgery [20].
Construct validity
This validity study was conducted according to the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) checklist [21]. This checklist was designed to evaluate the methodological quality of studies on measurement properties and set minimal standards for design and reporting. The COSMIN describes two types of validity that are relevant to performance-based measures: criterion-related validity (degree to which a measure is an adequate reflection of a gold standard measure of the construct of interest) and construct validity (degree to which the measure is consistent with hypotheses based on the assumption that it measures the construct of interest) [21]. As there is no gold standard measure of the construct “recovery,” this study focused on construct validity. According to the COSMIN, hypotheses tested for construct validity revolve around the degree to which the measure of interest (1) can demonstrate differences between relevant groups (i.e., groups known to differ on the construct of interest) and/or (2) is related to other measures of the same construct. It is recommended that hypotheses testing be based on the expected direction and magnitude of differences or correlations rather than on sample size-dependent statistics, such as p values [22].
Construct validity of the 6MWT as a measure of postoperative recovery was assessed by testing the hypotheses that the 6MWD at 4 weeks after surgery is greater (1) in younger patients (<75 years old) versus older patients (≥75 years old), (2) in patients with higher preoperative physical status (ASA < 2) versus lower preoperative physical status (ASA ≥ 3), (3) after laparoscopic versus open surgery, (4) in patients without postoperative complications versus with postoperative complications; and that the 6MWD (5) correlates cross-sectionally with self-reported physical activity as measured with the CHAMPS questionnaire. We hypothesized that the magnitude of differences between groups would be equal or greater than the MID of 19 m [18], and that the correlation between 6MWD and CHAMPS scores would be positive and moderate (correlation coefficient 0.2–0.5) [23]. All the hypotheses tested in this study were formulated prior to merging the databases and analyzing the data.
Statistical analysis
We conducted a complete case analysis including patients who performed the 6MWT at baseline and at 4 weeks after surgery. The characteristics of the included patients and those lost to follow-up were compared using Chi-square test or Fisher’s exact test (for categorical data) and Student’s t test or Mann–Whitney U test (for continuous data). Hypotheses 1–4 were tested using multiple linear regression where 6MWD at 4 weeks after surgery was the dependent outcome variable. Analyses were adjusted for patient baseline 6MWD to take into account preoperative functional walking capacity as a potential confounder. Linear regression coefficients were interpreted as mean difference in 6MWD between groups. Hypothesis 5 was tested using Spearman’s rank correlation. All statistical analyses were performed using STATA® version 13.1 software (StataCorp, College Station, TX, USA).
Results
Of the 174 patients enrolled in the three RCTs, a total of 151 (87 %) performed the 6MWT preoperatively and 4 weeks after surgery and were included in this validity study. Patients lost to follow-up (n = 23) were older [73 (95 % CI 68–77) versus 67 (95 % CI 65–69), p = 0.019] and less likely to have received laparoscopic surgery (74 vs. 91 %, p = 0.023). No difference was found regarding other baseline and operative characteristics, including preoperative 6MWD and CHAMPS scores (Table 1). After surgery, excluded patients had higher rates of overall complications (61 vs. 31 %, p = 0.005), severe complications (35 vs. 5 %, p < 0.001) and 30-day readmissions (32 vs. 12 %, p = 0.02) (Table 2).
All the four hypotheses involving group comparisons were confirmed by the data. At 4 weeks after surgery, 6MWD was greater in younger versus older patients (mean difference 28.3 m, 95 % CI −8.1 to 64.7), in patients with higher preoperative physical status versus lower (mean difference 44.2 m, 95 % CI 15.5–72.8), after laparoscopic versus open surgery (mean difference 58.8 m, 95 % CI 11.5–106.0) and in patients without postoperative complications versus with postoperative complications (mean difference 27.1 m, 95 % CI −1.9 to 56.1) (Table 3). The hypothesis involving cross-sectional relationship between 6MWD and CHAMPS scores was also confirmed as we found a moderate positive correlation between the measures (r = 0.46).
Discussion
The present study contributes evidence for the construct validity of the 6MWT as a measure of postoperative recovery after elective colorectal resection. As we hypothesized, 6MWD at 4 weeks after surgery was able to discriminate between younger and older patients, patients with higher versus lower preoperative physical status, patients treated with laparoscopic versus open surgery and patients who experienced postoperative complications versus those with an uneventful postoperative course. The 6MWT was also found to have a moderate positive correlation with patient-reported physical activity using the CHAMPS questionnaire.
Physical function represents a crucial dimension of recovery. This dimension can be measured either through performance-based measures (e.g., 6MWT, handgrip test, 30-s sit-to-stand test) or through patient-reported outcome (PRO) measures (e.g., CHAMPS, Short-Form 36 physical component scale) [6, 24]. As walking is essential to everyday activities and integrates different components of functional capacity (i.e., balance, speed and endurance) [25], it is possible that the 6MWT captures a wider spectrum of recovery than expected. Although this test may miss the patient’s perspective and other health-related quality of life domains that are unique to PRO measures, the 6MWT has the advantage of providing an objective measure that avoids bias associated with PRO measures such as “response shift” (i.e., a change in patients’ values, internal standards and conceptualization interfering with PRO responses) [26] and “floor and ceiling effect” (i.e., PRO responses achieving maximal or minimal levels reducing sensitivity to change) [27]. In fact, a previous study suggested that performance-based measures capture postoperative functional impairment more accurately than PRO measures [6].
In this cohort, only 13 % of patients did not perform the test at 4 weeks after surgery, a relatively low rate of missing data in comparison with previous studies assessing recovery through PROs [28, 29]. Patients who failed to perform the test at 4 weeks were older, had a higher rate of open surgery and experienced more postoperative complications. This suggests that poor postoperative physical status was a common reason for patients being lost to follow-up. The exclusion of these patients from the analysis might have biased our comparisons, but toward the null hypothesis (i.e., differences in 6MWD between groups would likely be even larger if these patients were included). This strengthens our conclusions regarding the validity of the 6MWT as a measure of recovery.
Our results corroborate some of the findings of the validation study by Moriello et al. [13], which also found an association of postoperative 6MWD with age, ASA scores and presence of postoperative complications after colorectal surgery. Previous research has shown that advanced age and poor physical status are associated with a slower return to baseline functional status [6, 30]. Similarly, postoperative morbidity appears to have a detrimental effect on quality of life early after surgery and in the long-term, affecting mostly the mobility and physical function domains [29, 31]. An additional finding of the current study is the positive cross-sectional correlation between the 6MWD and self-reported physical activity as measured using the CHAMPS questionnaire. As the CHAMPS covers a wide range of lifestyle activities (e.g., household activities, cleaning, yard work) [19], this finding reinforces the idea of using the 6MWT as a proxy measure for the ability to perform activities of daily living after surgery.
A novel and relevant finding of this study is that the 6MWT was able to capture differences in recovery between patients undergoing laparoscopic versus open surgery at 4 weeks postoperatively. Previous evidence suggests that patients treated with laparoscopy have reduced pain scores, faster recovery of bowel function and earlier hospital discharge in comparison with conventional open surgery [32]. However, the benefits of laparoscopy have appeared to be limited to the very early phase of recovery, as studies using PRO measures [e.g., SF-36 and the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30 questionnaire] have failed to show any significant difference in recovery by 2 weeks after surgery [28, 33, 34]. This could also reflect the use of questionnaires that are not sensitive enough to detect differences in recovery. The 6MWT specifically targets physical function, which may be the domain of recovery that is most influenced by open surgery, as it involves lengthier incisions, greater tissue trauma and greater physiological stress in comparison with laparoscopy [35]. This would explain why the 6MWT remains sensitive to differences between these approaches even in the longer term.
Strengths and limitations
Strengths of this study include the adoption of accepted guidelines to test the measurement properties of the 6MWT [21] and the use of MIDs to formulate hypotheses involving group comparisons. Moreover, our sample size was relatively large in comparison with previous studies [12, 13] allowing us to test multiple hypotheses. As this study involved patients undergoing colorectal resection in a referral center for laparoscopic surgery and enhanced recovery, our results contribute evidence for the validity of the 6MWT in the context of modern surgical and perioperative care.
The main limitation of this study was the lack of a gold standard measure of postoperative recovery to test criterion validity; thus, we needed to rely on construct validity. In addition, because we used secondary data from three previous RCTs, the hypotheses tested for construct validity were not formulated prior to data collection as recommended by the COSMIN checklist [21]. To limit potential bias related to selective reporting, we formulated our hypotheses before the databases were merged and reported all the hypotheses tested. Another potential limitation of this study is the relatively low proportion of patients receiving open surgery in this series. To reduce the possible patient selection bias (i.e., open surgery patients may have different baseline walking capacity compared to laparoscopic patients), the analysis was carried out adjusting for baseline 6MWD values. Nonetheless, the sensitivity of the 6MWT to detect differences in recovery after open and laparoscopic colorectal surgery should be further assessed in a larger cohort of patients including a greater number of open procedures. Finally, the results of this validity study are only generalizable to patients who were accounted for in the selection criteria of the RCTs. It is also important to note that the 6MWT remains a test of functional exercise capacity that does not account for other relevant domains for recovery such as pain, cognitive and gastrointestinal function. These domains should be measured using other validated instruments.
Conclusions
The present study contributes further evidence for the construct validity of the 6MWT as a measure of recovery after colorectal resection. Older age, poorer physical status, complications and open surgery are associated with shorter 6MWD at 4 weeks after surgery. We also found a positive cross-sectional correlation between 6MWD and patient-reported physical activity. These findings should encourage the adoption of this test as an outcome measure in studies evaluating interventions aimed to improve postoperative recovery.
References
Kehlet H (2011) Fast-track surgery-an update on physiological care principles to enhance recovery. Langenbecks Arch Surg 396:585–590
Feldman LS, Lee L, Fiore J Jr (2015) What outcomes are important in the assessment of Enhanced Recovery After Surgery (ERAS) pathways? Can J Anaesth 62:120–130
Lee L, Tran T, Mayo NE, Carli F, Feldman LS (2014) What does it really mean to “recover” from an operation? Surgery 155:211–216
Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM, Feldman LS (2014) Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg 101:159–170
Tran TT, Kaneva P, Mayo NE, Fried GM, Feldman LS (2014) Short-stay surgery: What really happens after discharge? Surgery 156:20–27
Lawrence VA, Hazuda HP, Cornell JE, Pederson T, Bradshaw PT, Mulrow CD, Page CP (2004) Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 199:762–772
Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB (1985) The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 132:919–923
Grady MV, Mascha E, Sessler DI, Kurz A (2012) The effect of perioperative intravenous lidocaine and ketamine on recovery after abdominal hysterectomy. Anesth Analg 115:1078–1084
Unver B, Kahraman T, Kalkan S, Yuksel E, Karatosun V (2013) Reliability of the six-minute walk test after total hip arthroplasty. Hip Int 23:541–545
Laboratories ATSCoPSfCPF (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166:111–117
Lee L, Schwartzman K, Carli F, Zavorsky GS, Li C, Charlebois P, Stein B, Liberman AS, Fried GM, Feldman LS (2013) The association of the distance walked in 6 min with pre-operative peak oxygen consumption and complications 1 month after colorectal resection. Anaesthesia 68:811–816
Sinclair RC, Batterham AM, Davies S, Cawthorn L, Danjoux GR (2012) Validity of the 6 min walk test in prediction of the anaerobic threshold before major non-cardiac surgery. Br J Anaesth 108:30–35
Moriello C, Mayo NE, Feldman L, Carli F (2008) Validating the six-minute walk test as a measure of recovery after elective colon resection surgery. Arch Phys Med Rehabil 89:1083–1089
Kolozsvari NO, Capretti G, Kaneva P, Neville A, Carli F, Liberman S, Charlebois P, Stein B, Vassiliou MC, Fried GM, Feldman LS (2013) Impact of an enhanced recovery program on short-term outcomes after scheduled laparoscopic colon resection. Surg Endosc 27:133–138
Gillis C, Li C, Lee L, Awasthi R, Augustin B, Gamsa A, Liberman AS, Stein B, Charlebois P, Feldman LS, Carli F (2014) Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 121:937–947
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7:541–546
Antonescu I, Scott S, Tran TT, Mayo NE, Feldman LS (2014) Measuring postoperative recovery: What are clinically meaningful differences? Surgery 156:319–327
Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL (2001) CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc 33:1126–1141
Feldman LS, Kaneva P, Demyttenaere S, Carli F, Fried GM, Mayo NE (2009) Validation of a physical activity questionnaire (CHAMPS) as an indicator of postoperative recovery after laparoscopic cholecystectomy. Surgery 146:31–39
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC (2010) The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res 19:539–549
Mokkink LB, Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, Bouter LM, de Vet HC (2010) The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol 10:22
Kraemer HC, Morgan GA, Leech NL, Gliner JA, Vaske JJ, Harmon RJ (2003) Measures of clinical significance. J Am Acad Child Adolesc Psychiatry 42:1524–1529
Tveter AT, Dagfinrud H, Moseng T, Holm I (2014) Health-related physical fitness measures: reference values and reference equations for use in clinical practice. Arch Phys Med Rehabil 95:1366–1373
Robinett CS, Vondran MA (1988) Functional ambulation velocity and distance requirements in rural and urban communities. A clinical report. Phys Ther 68:1371–1373
Ring L, Hofer S, Heuston F, Harris D, O’Boyle CA (2005) Response shift masks the treatment impact on patient reported outcomes (PROs): the example of individual quality of life in edentulous patients. Health Qual Life Outcomes 3:55
Mayo NE, Feldman L, Scott S, Zavorsky G, Kim DJ, Charlebois P, Stein B, Carli F (2011) Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery 150:505–514
Antonescu I, Carli F, Mayo NE, Feldman LS (2014) Validation of the SF-36 as a measure of postoperative recovery after colorectal surgery. Surg Endosc 28:3168–3178
Brown SR, Mathew R, Keding A, Marshall HC, Brown JM, Jayne DG (2014) The impact of postoperative complications on long-term quality of life after curative colorectal cancer surgery. Ann Surg 259:916–923
Finlayson E, Zhao S, Boscardin WJ, Fries BE, Landefeld CS, Dudley RA (2012) Functional status after colon cancer surgery in elderly nursing home residents. J Am Geriatr Soc 60:967–973
Sharma A, Sharp DM, Walker LG, Monson JR (2007) Predictors of early postoperative quality of life after elective resection for colorectal cancer. Ann Surg Oncol 14:3435–3442
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev (3):CD003145
Dowson H, Cowie A, Ballard K, Gage H, Rockall T (2008) Systematic review of quality of life following laparoscopic and open colorectal surgery. Colorectal Dis 10:751–768
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, Group MCt (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Veenhof AA, Vlug MS, van der Pas MH, Sietses C, van der Peet DL, de Lange-de Klerk ES, Bonjer HJ, Bemelman WA, Cuesta MA (2012) Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg 255:216–221
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Julio F. Fiore Jr. is supported by a postdoctoral fellowship by Mitacs/Covidien. Liane S. Feldman is the recipient of an investigator-initiated research grant from ConMed. The Steinberg-Bernstein Centre for Minimally Invasive Surgery and Innovation is supported by an unrestricted educational grant from Covidien. Nicolò Pecorelli, Benjamin Mappin-Kasirer, Petru Niculiseanu, Chelsia Gillis, Rashami Awasthi, Francesco Carli have no conflicts of interests or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Pecorelli, N., Fiore, J.F., Gillis, C. et al. The six-minute walk test as a measure of postoperative recovery after colorectal resection: further examination of its measurement properties. Surg Endosc 30, 2199–2206 (2016). https://doi.org/10.1007/s00464-015-4478-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4478-1