Abstract
Introduction
Pancreatic pseudocysts and walled-off necrosis are well-known complications, described in 10 % of cases of acute pancreatitis. Open cystogastrostomy is usually proposed after failure of minimally invasive drainage or in the presence of septic shock. The objective of this study was to evaluate the feasibility and efficacy of laparoscopy-assisted open cystogastrostomy for treatment of symptomatic pancreatic pseudocyst with pancreatic necrosis.
Materials and methods
Between January 2011 and October 2014, all patients with pseudocyst and pancreatic necrosis undergoing open cystogastrostomy were included. Surgical procedure was standardized. The primary efficacy endpoint was the feasibility and efficacy of laparoscopy-assisted open cystogastrostomy as treatment of symptomatic pancreatic pseudocyst. Secondary endpoints included demographic data, preoperative management, operative data, postoperative data and follow-up.
Results
Laparoscopy-assisted open cystogastrostomy was performed in 11 patients [six men (54 %)], with a median age of 61 years (45–84). Nine patients received preoperative radiological or endoscopic management. First-line open cystogastrostomy was performed in two cases. Median operating time was 190 min (110–240). There was one intraoperative complication related to injury of a branch of the superior mesenteric vein. There were no postoperative deaths and two postoperative complications (18 %) including one major complication (postoperative bleeding). The median length of hospital stay after surgery was 16 days (7–35). The median follow-up was 10 months (2–45). One patient experienced recurrence during follow-up.
Conclusion
Open cystogastrostomy for necrotizing pancreatitis promotes adequate internal drainage with few postoperative complications and a short length of hospital stay. However, this technique must be performed very cautiously due to the risk of vascular injury which can be difficult to repair in the context of severe local inflammation related to pancreatic necrosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Pancreatic pseudocysts and walled-off necrosis are well-known complications, described in 10 % of cases of acute pancreatitis [1]. Pseudocyst is the consequence of inflammatory pancreatitis or pancreatic duct leak and corresponds to serous pancreatic fluid that may be infected. Walled-off necrotic pancreatic tissue is sometimes associated with variable degrees of liquefaction [1, 2].
Asymptomatic pseudocysts can generally be managed by observation. Classically, pseudocysts <6 cm in diameter resolve spontaneously [3]. In the presence of larger pseudocysts, even when asymptomatic, drainage appears to be required due to the risk of secondary complications such as infection, intraperitoneal rupture, bleeding by vessel erosion, compression of adjacent organs leading to obstructive jaundice or gastric outlet obstruction [4, 5]. In symptomatic forms, including pain and septic signs, first-line conservative treatment consists of antibiotics in the case of infection, even when a large amount of necrotic tissue is present [6]. Second-line treatment consists of minimally invasive drainage. Percutaneous drainage allows complete resolution in 84 % of cases, with a morbidity rate of 17 % [7]. Endoscopic drainage, improved by ultrasound guidance, allows a clinical success rate of 90 % with a complication rate ranging from 0 to 9 % [8, 9]. The presence of necrosis can be considered to be a risk factor for failure of endoscopic treatment, although some series have demonstrated the efficacy of minimally invasive therapy [10].
Surgical treatment is indicated only after failure of percutaneous or endoscopic drainage [11, 12]. Surgery may be directly indicated in the presence of extensive walled-off pancreatic necrosis when endoscopic treatment alone does not allow sufficient drainage or in the presence of septic shock requiring rapid and complete treatment of intra-abdominal infection.
Depending on the site of the necrosis, open cystogastrostomy and pancreatic debridement are classically performed when necrosis is located behind the posterior gastric wall. Necrosectomy is traditionally performed blindly with a risk of injury of vessels and incomplete removal of pancreatic necrosis.
The objective of this study was to evaluate the feasibility, efficacy and advantage of laparoscopy-assisted open cystogastrostomy as treatment for symptomatic pancreatic pseudocyst.
Materials and methods
Population
From January 2011 to October 2014, all patients undergoing open cystogastrostomy for pancreatic pseudocyst with the presence of pancreatic parenchymal necrosis were included in the study.
Definition of pancreatic pseudocysts and walled-off pancreatic necrosis
Pancreatic pseudocysts were defined by pancreatic fluid collections surrounded by a wall of fibrous granulation tissue following acute pancreatitis, pancreatic trauma or chronic pancreatitis [13]. Connor et al. [14] described walled-off pancreatic necrosis as a heterogeneous mass with solid and liquid components in a well-defined inflammatory wall of fibrous tissue on contrast-enhanced abdominal computed tomography scan. Walled-off pancreatic necrosis is usually described as appearing at least 4 weeks after onset of necrotizing pancreatitis [15].
Surgical management of pseudocysts
Initial workup
A preoperative abdominal CT scan with arterial and portal phases was always performed in order to visualize the anatomical relations between the pancreatic pseudocyst, the posterior gastric wall and vessels (arteries: gastroduodenal artery; veins: portal vein, splenomesenteric trunk and splenic vein) (Fig. 1). The indication for endoscopic or radiologic treatment as same as the indication for a surgical procedure was validated during a multidisciplinary staff meeting (comprising surgeons, endoscopists and radiologists).
Surgical procedure
Surgery was performed via a midline laparotomy except in one case (bilateral subcostal incision).
The first step consisted of anterior gastrostomy, measuring approximately 5 cm, located in the antrum. Four sutures were placed at the 4 cardinal points of the anterior gastrostomy incision, allowing better exposure of the posterior gastric wall. Exploration of the posterior gastric wall was performed to locate a retrogastric pseudocyst, by palpation, in the case of a voluminous collection with gastric bulge, or by ultrasound when there was a doubt about the exact location of the retrogastric pseudocyst. A fine needle was introduced through the posterior gastric wall to obtain a bacteriological sample and then to guide cystogastrostomy. The posterior gastric wall was opened over the fine needle using an electric scalpel as a longitudinal incision of 4–6 cm. Several 3/0 monofilament nonabsorbable sutures are placed on the edges of the posterior gastrostomy to ensure optimal hemostasis (Video 1). The posterior gastrostomy measured a total of 4–6 cm to ensure optimal drainage of the retrogastric pseudocyst.
Optimal necrosectomy was performed with the 30-degree laparoscope introduced through the cystogastrostomy, together with substantial irrigations to clean the retrogastric pseudocyst and ensure satisfactory debridement and hemostasis (Video 2). Necrosectomy was performed cautiously using a Duval clamp (Fig. 2). The laparoscope was used to guide the necrosectomy to remove a maximum of necrotic pancreatic tissue and allow visualization of intracystic vessels (Fig. 3).
At the end of necrosectomy, a nasogastric tube was introduced into the stomach, passed through the opening of the posterior gastric wall and positioned in the pseudocyst cavity (Fig. 4) to allow postoperative irrigation and aspiration (if necessary, depending on the purulent appearance of the cyst fluid). The anterior gastric wall was then sutured in two layers using 3/0 monofilament absorbable suture material as two half-running sutures on the mucosal, then serosal planes.
Drainage was ensured by two suction drains allowing aspiration and, when necessary, irrigations in contact with the anterior gastric suture. A feeding jejunostomy was systematically placed at the end of the surgical procedure [16].
Surgical variants
As explained above, surgery was sometimes a second-line procedure after failure of endoscopic treatment. A shorter surgical procedure was performed in this setting. The posterior gastrostomy and cystogastrostomy steps are no longer necessary in the presence of an endoscopic stent providing direct access to the pseudocyst immediately after anterior gastrostomy. When a double-pigtail stent (Zimmon® Biliary Stent, Cook Ireland Ltd., Limerick, Ireland) had been used prior to surgery, the double-pigtail stent provided exposure to the posterior gastric wall which was opened by enlarging the opening created by the stent. When a Diabolo covered self-expandable metallic stent (SARL COUSIN ENDOSURG, Wervicq-sud, France) had been used, necrosectomy was performed through the stent (Video 3), and the Diabolo stent was left in place at the end of the surgical procedure with a nasogastric tube inserted through the stent order to drain the pseudocystic cavity.
Postoperative management
Irrigation and aspiration through the nasogastric tube, using one to two liters of water, were performed on the first postoperative days. The feeding jejunostomy was used on the day after surgery allowing rapid renutrition.
A postoperative abdominal CT scan with oral contrast study was performed on the seventh postoperative day to ensure the absence of leakage of the anterior gastric wall suture and ensure adequate drainage of the retrogastric pseudocyst.
The nasogastric tube was then removed, and oral feeding was resumed. Abdominal drainage was removed in the presence of normal oral feeding. The feeding jejunostomy was removed 6 weeks after surgery in the absence of complications.
Study criteria
The inclusion and exclusion criteria were as follows:
-
Inclusion criteria: pancreatic pseudocyst requiring surgery, pancreatic pseudocyst treated by surgical cystogastrostomy, and pancreatic pseudocyst with the presence of parenchymal necrosis.
-
Exclusion criteria: pancreatic surgical procedures other than PD, pancreatic pseudocyst treated exclusively by endoscopic procedures, and pancreatic pseudocyst requiring surgical management other than surgical cystogastrostomy.
Endpoints and data collection
The primary objective of the study was to assess the feasibility and efficacy of surgical cystogastrostomy for pancreatic pseudocysts. The secondary endpoints included data on surgical parameters, intraoperative and postoperative complications, recurrence rate and follow-up.
The following parameters were recorded:
-
Preoperative data: age, gender, body mass index, type 2 diabetes, median preoperative percentage of weight loss, cause of pancreatitis.
-
Preoperative management: proportion of patients in whom preoperative endoscopy or radiologic drainage was performed, number of endoscopic procedures, type of endoscopic procedure, patients with concomitant pancreatic duct leak and management.
-
Surgical data: indication for surgery, operating time, blood loss, simultaneous cholecystectomy rate and feeding jejunostomy rate.
-
Outcome data: mortality rate, complication rate according to the Dindo classification [17], reoperation rate, time to oral refeeding, total length of hospital stay (LOS) and LOS after surgery.
-
Follow-up data: median follow-up, type 2 diabetes rate, exocrine pancreatic insufficiency rate, pseudocyst recurrence rate and management.
Results
Preoperative data
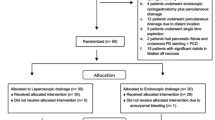
During the study period, 42 patients were managed for walled-off pancreatic necrosis following acute pancreatitis. Thirty-one patients were managed exclusively by conservative management (radiological drainage and/or endoscopy), and open cystogastrostomy was required in 11 patients (26.2 %). This group consisted of six men (54 %), with a median (range) age of 61 years (45–84). The median preoperative BMI was 24.3 kg/m2 (19.1–30.4). Three patients had type 2 diabetes (27 %), three patients were active smokers (27 %) and two patients presented chronic alcoholism (18 %).
Cause for pancreatic pseudocysts was due to a biliary cause in five cases (45 %), chronic pancreatitis in two cases, alcohol-induced acute pancreatitis in two cases, pancreatitis after endoscopic retrograde cholangiopancreatography in one case and pancreatitis secondary to hypertriglyceridemia in one case.
Preoperative management
Abdominal CT scan was performed in all patients at the time of diagnosis of pseudocyst. A pancreatic duct leak was visible on abdominal CT scan in two patients.
Nine patients had been treated preoperatively by a radiological or endoscopic technique. CT-guided percutaneous drainage had been performed in three patients. The pseudocyst had been treated endoscopically prior to surgery in seven patients. Endoscopic treatment consisted of double-pigtail stent in three cases, endoscopic cystogastrostomy in two cases and Diabolo stent in three cases. Two different types of endoscopic treatment were performed in one patient: double-pigtail stent followed by Diabolo stent. Two patients were treated by both CT-guided drainage and endoscopic treatment. A 5-mm pancreatic duct stent was placed in two patients with pancreatic duct leak. The median number of endoscopic procedures per patient was 2 (1–5). Median time to surgical management after diagnosis of pseudocyst was 44 days (32–70). Two patients had not been treated preoperatively by a radiological or endoscopic technique because of septic shock (18 %) and underwent first-line laparoscopy-assisted open cystogastrostomy.
Surgical data
Surgery was indicated due to failure of endoscopic treatment in five cases, unfeasible endoscopic treatment in four cases, spontaneous intracystic bleeding in one case, and intracystic bleeding secondary to endoscopy in one case. First-line open cystogastrostomy was performed in two cases.
Surgery was performed via a midline laparotomy in 10 cases and via bilateral subcostal laparotomy in 1 case. The median operating time was 190 min (110–240). Median blood loss was 400 ml (100–1700). Cholecystectomy was performed during the same procedure in 7 cases. A feeding jejunostomy was placed in 9 cases.
There was one intraoperative complication related to injury of a branch of superior mesenteric vein requiring suture using 4.0 nonabsorbable suture material (Video 3). Concomitant ligation of the gastroduodenal artery was performed in one patient (Video 4).
Outcomes
No postoperative deaths were observed in this series. Two postoperative complications (18 %) were observed: postoperative lung infection (Clavien grade 2) treated with antibiotics, and postoperative bleeding from the posterior gastrostomy requiring endoscopy with the use of local adrenalin (Clavien grade 3b).
The median total length of hospital stay was 29 days (8–102). The median length of hospital stay after open cystogastrostomy was 16 days (7–35). Five patients required postoperative monitoring in the intensive care unit (50 %). The median length of stay in the intensive care unit was 4 days (3–9).
Long-term follow-up
No death (0 %) and one case of recurrence were observed with a median follow-up of 10 months (2–45) (Fig. 5). The patients with recurrence underwent spleen-preserving distal pancreatectomy. On our follow-up, there was no need for additional endoscopic or radiological treatment. Five patients had type 2 diabetes (50 %), and one patient had exocrine pancreatic insufficiency (10 %).
Discussion
Specific management is required for pseudocysts measuring more than 60 mm in diameter, and for symptomatic or infected pseudocysts. In these situations, first-line endoscopic or radiological drainage is usually required. Endoscopic procedures include endoscopic cystogastrostomy, endoscopic retrograde cholangiopancreatography, double-pigtail stent placement, covered self-expandable metallic stent (“Diabolo”) placement [18] or natural orifice transluminal endoscopic surgery for more extensive necrosectomy [19].
Open surgical cystogastrostomy is usually proposed in patients with necrotizing pancreatitis and secondary infection of necrotic tissue, but this invasive approach is associated with higher complication and mortality rates [20, 21]. In view of the good results obtained with minimally invasive treatment, a step-up approach was proposed as first-line therapy with percutaneous or endoscopic drainage of the collection, followed by minimally invasive retroperitoneal necrosectomy in the absence of clinical improvement. In a multicenter randomized study, van Santvoort et al. [22] showed that this approach was associated with a lower rate of major complications or death (40 % for the step-up approach vs. 69 % for primary open cystogastrostomy).
Surgery is usually performed as second-line treatment or as first-line treatment in the case of multiple pseudocysts or bleeding secondary to rupture of pseudocyst or pseudoaneurysm adjacent to the pseudocyst [23]. As in our series, most cases of pseudocyst reported in the literature were primarily managed by endoscopic or radiological drainage. Many different types of surgical procedure have been proposed, such as external drainage of the pseudocyst with the risk of external pancreatic fistula, pancreatic resection [24] which is associated with higher morbidity and mortality rates, and internal drainage by creating a communication between the pseudocyst and a segment of gastrointestinal tract: duodenum, stomach and jejunum; the type of bypass depends on the site of the pseudocyst. When pseudocysts are located behind the posterior surface of the stomach, cystogastrostomy (open or laparoscopic) can usually be proposed as surgical management.
Recently, Varadarajulu et al. [25], in a prospective single-center randomized study comparing 20 patients with first-line endoscopic treatment to 20 patients with first-line open cystogastrostomy, showed that endoscopic treatment was associated with shorter hospital stays, better physical and mental health of patients, and lower cost. There was no case of recurrence in the endoscopic group compared to one case of recurrence in the surgical group. Endoscopic therapy was not possible in one patient. However, this study included patients without pancreatic parenchymal necrosis (exclusion criterion), and very good results were obtained in the surgical group that are with few complications (one major complication, 5 %) and a median length of hospital stay of 6 days for surgical patients. The length of hospital stay in our study was almost three times longer. Endoscopic treatment was also performed only once for most patients in Varadarajulu’s series. These results, better than those observed in our series, can be explained by the fact that we only included patients with pancreatic parenchymal necrosis. Most patients in our institution are treated by endoscopy only, without the need for open cystogastrostomy, in the absence of pancreatic parenchymal necrosis.
Necrosectomy is traditionally performed according to a blind approach with a risk of injury to the vessels and incomplete removal of pancreatic necrosis. In our experience, the blind technique was associated with one additional early postoperative death due to intraoperative injury of vessels. We therefore modified our technique in favor of open cystogastrostomy. The present series comprises 11 cases of laparoscopy-assisted open cystogastrostomy. The median operating time of 190 min was acceptable. Outcomes were acceptable with only one major complication (postoperative bleeding at the posterior gastrostomy) requiring endoscopy, and the length of hospital stay was acceptable with a median length of hospital stay of 16 days. Nevertheless, surgical cystogastrostomy is associated with certain risks, as one case of injury of a branch of the superior mesenteric vein during necrosectomy was observed in our series explaining the high intraoperative blood loss (1700 ml). Gastroduodenal artery injury can also be observed as in our series, as this artery has a retropancreatic course and may therefore be situated in the middle of the necrosis (Video 4) and can be easily injured during necrosectomy. Prophylactic ligation was performed in our case to prevent pseudoaneurysm formation. Laparoscopy-assisted open cystogastrostomy with placement of a transgastric retroperitoneal drainage tube was associated with complete resolution of all complex pancreatic pseudocysts with only one case of recurrence in this series. The patient with recurrence was the first patient in this series to be treated by open cystogastrostomy, and recurrence may have been due to an excessively short posterior gastrostomy. This technique can also avoid vascular injury, as the artery and vein may be weakened by local inflammation due to pancreatic necrosis (Video 4). Globally, our results are similar to those reported in the literature [12].
Laparoscopic cystogastrostomy has been described previously, but requires extensive experience. Simo et al. [Simo] published their experience based on 22 patients. Mean operating time was acceptable at 220 min. Seven patients required conversion to an open procedure (31 %). No recurrence was observed in 20 patients with a mean follow-up of 3.4 months. The main problem associated with laparoscopic cystogastrostomy for debridement of pancreatic necrosis is the possibility of incomplete removal of necrosis, as reported in the series by Simo et al. [26]. The advantage of our technique is that optimal debridement can be performed under laparoscopic control with optimal control of vessels to avoid injury during necrosectomy. Our technique can also be performed by all surgeons and does not require an extensive experience of laparoscopy. For this reason, we prefer to perform open cystogastrostomy with concomitant use of laparoscopy to ensure removal of a maximum of pancreatic necrosis.
Conclusion
Open cystogastrostomy for necrotizing pancreatitis promotes adequate internal drainage of the heterogeneous pancreatic pseudocyst, resulting in a postoperative complication rate and a short length of hospital stay. However, this technique requires particular attention to the risk of vascular injury, which can be difficult to repair in the context of severe local inflammation related to pancreatic necrosis.
References
Klöppel G (2000) Pseudocysts and other non-neoplastic cysts of the pancreas. Semin Diagn Pathol 17:7–15
Baron TH, Thaggard WG, Morgan DE, Stanley RJ (1996) Endoscopic therapy of organized pancreatic necrosis. Gastroenterology 111:755–764
Bradley EL, Clements JL Jr, Gonzalez AC (1979) The natural history of pancreatic pseudocysts: a unified concept of management. Am J Surg 137:135–141
O’Malley VP, Cannon JP, Postier RG (1985) Pancreatic pseudocysts: cause, therapy, and results. Am J Surg 150:680–682
Gluck M, Ross A, Irani S, Lin O, Hauptmann E, Siegal J, Fotoohi M, Crane R, Robinson D, Kozarek RA (2010) Endoscopic and percutaneous drainage of symptomatic walled-off pancreatic necrosis reduces hospital stay and radiographic resources. Clin Gastroenterol Hepatol 8:1083–1088
Regimbeau JM, Dupont H (2004) Should patients with acute severe pancreatitis be given antibiotic prophylaxis? Ann Chir 129:596–598
Pitchumoni CS, Agarwal N (1999) Pancreatic pseudocysts. When and how should drainage be performed? Gastroenterol Clin North Am 28:615–639
Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Moriyasu F (2006) EUS-guided simultaneous internal and external drainage of pancreatic infected pseudocysts. Dig Endosc 18:71–74
Will U, Wanzar C, Gerlach R, Meyer F (2011) Interventional ultrasound-guided procedures in pancreatic pseudocysts, abscesses and infected necroses—treatment algorithm in a large single-center study. Ultraschall Med 32:176–183
Seifert H, Wehrmann T, Schmitt T, Zeuzem S, Caspary WF (2000) Retroperitoneal endoscopic debridement for infected peripancreatic necrosis. Lancet 356:653–655
Evans KA, Clark CW, Vogel SB, Behrns KE (2008) Surgical management of failed endoscopic treatment of pancreatic disease. J Gastrointest Surg 12:1924–1929
Boutros C, Somasundar P, Espat NJ (2010) Open cystogastrostomy, retroperitoneal drainage, and G-J enteral tube for complex pancreatitis-associated pseudocyst: 19 patients with no recurrence. J Gastrointest Surg 14:1298–1303
Bradley EL III (1993) A clinically based classification system for acute pancreatitis. Summary of the international symposium on acute pancreatitis, Atlanta, GA, September 11 through 13, 1992. Arch Surg 128:586–590
Connor S, Raraty MG, Howes N, Evans J, Ghaneh P, Sutton R, Neoptolemos JP (2005) Surgery in the treatment of acute pancreatitis-minimal access pancreatic necrosectomy. Scand J Surg. 94:135–142
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS, Acute Pancreatitis Classification Working Group (2013) Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 62:102–111
Delany HM, Carnevale NJ, Garvey JW (1973) Jejunostomy by a needle catheter technique. Surgery 73:786–790
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Bourgeois M, Fumery M, Coron E, Giovannini M, Crinquette JF, Branche J, Antonietti M, Iwanicki-Caron I, Barange K, Yzet T, Brazier F, Bartoli E, Regimbeau JM, Dupas JL, Nguyen Khac E, Delcenserie R (2014) Su1709 Covered Self Expandable Metallic Stent (“Diabolo”) for the treatment of pancreatic fluid collections. Gastrointest Endosc 79(suppl):AB375
Puli SR, Graumlich JF, Pamulaparthy SR, Kalva N (2014) Endoscopic transmural necrosectomy for walled-off pancreatic necrosis: a systematic review and meta-analysis. Can J Gastroenterol Hepatol 28:50–53
Connor S, Alexakis N, Raraty MG, Ghaneh P, Evans J, Hughes M, Garvey CJ, Sutton R, Neoptolemos JP (2005) Early and late complications after pancreatic necrosectomy. Surgery 137:499–505
Rau B, Bothe A, Beger HG (2005) Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery 138:28–39
van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, van Goor H, Schaapherder AF, van Eijck CH, Bollen TL, van Ramshorst B, Nieuwenhuijs VB, Timmer R, Laméris JS, Kruyt PM, Manusama ER, van der Harst E, van der Schelling GP, Karsten T, Hesselink EJ, van Laarhoven CJ, Rosman C, Bosscha K, de Wit RJ, Houdijk AP, van Leeuwen MS, Buskens E, Gooszen HG, Dutch Pancreatitis Study Group (2010) A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 362:1491–1502
Kianmanesh R, Benjelloun M, Scaringi S, Leroy C, Jouet P, Castel B, Sabaté JM, Coffin B, Flamant Y, Msika S (2008) Fissure syndrome of a gastrointestinal artery pseudoaneurysm in contact with a pseudocyst of the pancreas: rare, but serious complication of chronic pancreatitis. Gastroenterol Clin Biol 32:69–73
Martin RF, Hein AR (2013) Operative management of acute pancreatitis. Surg Clin North Am 93:595–610
Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM (2013) Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 145:583.e1–590.e1
Simo KA, Niemeyer DJ, Swan RZ, Sindram D, Martinie JB, Iannitti DA (2014) Laparoscopic transgastric endolumenal cystogastrostomy and pancreatic debridement. Surg Endosc 28:1465–1472
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Olivier Gerin, Flavien Prevot, Abdennaceur Dhahri, Richard Delcenserie, Lionel Rebibo and Jean-Marc Regimbeau have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MPG 23338 kb)
Supplementary material 2 (MPG 23258 kb)
Supplementary material 3 (MPG 24528 kb)
Supplementary material 4 (MPG 16104 kb)
Rights and permissions
About this article
Cite this article
Gerin, O., Prevot, F., Dhahri, A. et al. Laparoscopy-assisted open cystogastrostomy and pancreatic debridement for necrotizing pancreatitis (with video). Surg Endosc 30, 1235–1241 (2016). https://doi.org/10.1007/s00464-015-4331-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4331-6