Abstract
Background
During peroral esophageal myotomy (POEM) for the treatment of achalasia, the optimal distal gastric myotomy length is unknown. In this study, we used a functional lumen imaging probe (FLIP) to intraoperatively measure the effect of variable distal myotomy lengths on esophagogastric junction (EGJ) distensibility.
Methods
EGJ distensibility index (DI) (minimum cross-sectional area divided by intrabag pressure) was measured with FLIP after each operative step. Each patient’s myotomy was performed in four increments from proximal to distal: (1) an esophageal myotomy (from 6 cm proximal to the EGJ to 1 cm proximal to it), (2) a myotomy ablating the lower esophageal sphincter (LES) complex (from 1 cm proximal to the EGJ to 1 cm distal to it), (3) an initial gastric extension (from 1 cm distal to the EGJ to 2 cm distal), and (4) a final gastric extension (from 2 cm distal to the EGJ to 3 cm distal).
Results
Measurements were taken in 16 achalasia patients during POEM. POEM resulted in an overall increase in DI (pre 1.2 vs. post 7.2 mm2/mmHg, p < .001). Initial creation of the submucosal tunnel resulted in a threefold increase in DI (1.2 vs. 3.6 mm2/mmHg, p < .001). When the myotomy was then performed in a stepwise fashion from proximal to distal, the initial esophageal myotomy component had no effect on DI. Subsequent myotomy extension across the LES complex resulted in an increase in DI, as did the initial gastric myotomy extension (to 2 cm distal to the EGJ). The final gastric myotomy extension (to 3 cm distal) had no further effect.
Conclusions
During POEM, creation of the submucosal tunnel prior to myotomy resulted in a marked improvement in EGJ physiology. Myotomy extension across the LES complex and to 2 cm onto the gastric wall resulted in the normalization of EGJ distensibility, whereas subsequent extension to 3 cm distal to the EGJ did not increase compliance further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Achalasia is an immune-mediated disease that results in a loss of enteric neurons of the esophagus. This causes failures of both esophageal body peristalsis and relaxation of the esophagogastric junction (EGJ) in response to swallowing, resulting in symptoms of dysphagia, regurgitation, chest pain, and weight loss. As there are no effective medical therapies for achalasia, standard treatment consists of procedural interventions that aim to disrupt the lower esophageal sphincter (LES) muscular complex in order to lower EGJ pressure and allow for the transit of food boluses into the stomach [1]. There are two such surgical procedures in current practice: the gold-standard, laparoscopic Heller myotomy, and a novel operation, peroral esophageal myotomy (POEM). Both procedures create a longitudinal myotomy from the distal esophagus, across the EGJ, and onto the stomach. During a Heller myotomy, this is accomplished via a laparoscopic approach, whereas POEM is performed completely endoscopically without skin incisions. During POEM, the esophageal muscle layer is accessed through a small mucosotomy in the midesophagus and the subsequent creation of a longitudinal submucosal tunnel across the EGJ and onto the gastric wall. First performed by Inoue in 2008 [2], this novel procedure has thus far been shown to result in excellent improvement in both achalasia symptoms and EGJ physiology at short- to midterm follow-up [3, 4].
For both laparoscopic Heller myotomy and POEM, minimal data exist offering guidance as to how far the myotomy should be extended, either proximally or distally. Two studies from the University of Washington suggest that for laparoscopic Heller, a longer distal gastric myotomy (≥3 cm onto the stomach) results in both a greater reduction in EGJ pressures and improved symptomatic outcomes when compared with a shorter distal myotomy extension (1.5 cm onto the stomach) [5, 6]. However, a similar recent study by Salvador and colleagues showed no difference in outcomes between shorter and longer gastric myotomy extensions during Heller [7]. Additionally, it is not clear whether either of these results necessarily translate to POEM, as several key anatomic differences exist between the two operations: During POEM, most surgeons perform a selective myotomy of the inner, circular muscle layer, as opposed to a myotomy of both muscle layers during Heller, POEM does not involve a dissection and then closure of the esophageal hiatus, and during POEM, no antireflux procedure is performed, whereas Heller typically includes a partial fundoplication.
In this study we sought to add to the evidence base regarding the optimal myotomy length during POEM by measuring the effect of incremental distal myotomy extensions on EGJ physiology intraoperatively. To do so, we used a functional lumen imaging probe (FLIP) to serially measure EGJ distensibility, while performing the myotomy in a stepwise fashion starting at its proximal end and proceeding distally onto the stomach wall. FLIP is a novel catheter-based diagnostic tool that measures EGJ distensibility, a metric that has been shown to better correlate with postintervention symptomatic outcomes than EGJ pressure as measured by manometry [8, 9]. Additionally, we have shown that FLIP can measure stepwise changes in EGJ physiology intraoperatively during POEM and that these distensibility measurements are predictive of eventual postoperative symptoms [10, 11]. These previous results provide the framework for using FLIP as a tool for testing the efficacy of variable myotomy length in real time.
Methods
Patient selection
During the study period, patients presenting to the surgery clinic at a single institution for treatment of achalasia were counseled regarding the available options (pneumatic dilation, LHM, or POEM) and chose among them in consultation with their physicians. Patients undergoing POEM were approached regarding undergoing stepwise intraoperative FLIP measurements. Additional FLIP study eligibility criteria included age ≥18 years and a diagnosis of achalasia, types I and II only, confirmed by esophageal manometry [12]. All patients signed an informed consent for intraoperative FLIP measurements prior to their procedure, and measurements were taken according to a study protocol approved by the Northwestern Institutional Review Board.
Preoperative demographics and high-resolution manometry
Demographic and disease-specific information including age, sex, duration of symptoms, Eckardt symptom score [13], prior endoscopic treatment for achalasia, and body mass index was collected prospectively. Patients underwent preoperative high-resolution manometry to confirm the diagnosis of achalasia type I or II. Manometry data were evaluated using esophageal pressure topography [14] and interpreted according to the Chicago classification of esophageal motility disorders [12].
POEM technique
Our operative technique for POEM has been previously described in detail [15]. A standard high-definition gastroscope with a transparent dissecting cap and CO2 insufflation was used. A saline solution was first injected into the anterior esophageal wall 12 cm proximal to the EGJ to create a submucosal fluid bleb. A mucosotomy was then made overlying the bleb, and the scope was maneuvered into the submucosal space. A submucosal tunnel was then dissected to at least 3 cm beyond the EGJ. For this study, a selective myotomy of the inner, circular muscle layer was then performed in four incremental segments, advancing from proximal to distal: (1) an esophageal myotomy (from 6 cm proximal to the EGJ to 1 cm proximal to it), (2) a myotomy ablating the LES complex (from 1 cm proximal to the EGJ to 1 cm distal to it), (3) an initial gastric extension (from 1 cm distal to the EGJ to 2 cm distal), and (4) a final gastric extension (from 2 cm distal to the EGJ to 3 cm distal). The endoscope shaft markings were used to measure myotomy distances in relation to the EGJ, using the intraluminal location of the squamocolumnar junction (SCJ) to mark the EGJ. After myotomy completion, the mucosotomy was closed with endoscopic clips.
FLIP
Intraoperative measurements were taken using a commercially available FLIP system (EndoFLIP; Crospon Ltd., Galway, Ireland) and probes (EF-325N; Crospon) that have previously been described in detail [16, 17]. FLIP is a catheter-based probe that contains 17 ring electrodes at 5-mm intervals, housed within a bag that can be variably filled with saline solution. Impedance planimetry measurements are taken to calculate bag cross-sectional areas (CSA) at the level of each electrode pair. Therefore, when the catheter is placed across the EGJ, these measurements represent the 16 CSAs at 5-mm intervals along an 8-cm segment of esophagus, EGJ, and stomach, giving a representation of luminal geometry. The probe also contains a solid-state pressure transducer that measures intrabag pressure.
The EGJ distensibility index (DI) is defined as the minimum CSA (i.e., narrowest portion of the EGJ) divided by intrabag pressure. The median value of minimum CSA and intrabag pressure measurements at each distension volume were calculated using MATLAB software (MathWorks; Natick, MA) and used for subsequent analysis when determining the DI.
Intraoperative FLIP protocol
Prior to probe insertion, an automated purge sequence was used to evacuate air from the FLIP and the pressure transducer was zeroed to atmospheric pressure. After the induction of anesthesia, paralysis, and endotracheal intubation, an upper endoscopy was performed and the FLIP was advanced down the esophagus under direct endoscopic visualization. Probe position across the EGJ was confirmed endoscopically and by seeing an “hour glass” anatomic configuration on the FLIP monitor.
FLIP measurements were taken after each step of POEM, including each of the incremental myotomy extensions, using a bag distension volume of 40 ml. Between measurements, the bag was deflated and the probe was advanced into the stomach. FLIP measurements were thus taken at six time points: (1) after the induction of anesthesia, paralysis, and endotracheal intubation, (2) after submucosal tunnel creation, (3) after esophageal myotomy, (4) after myotomy across the LES complex, (5) after initial gastric myotomy extension, and (6) after final gastric myotomy extension.
Statistical analysis
Data analysis was performed using SPSS software (version 22; IBM, Armonk, NY). For continuous variables, comparisons between time points were made using a paired t test. A two-tailed p value of <.05 was used to determine statistical significance in all cases. Values throughout are presented as mean ± standard deviation.
Results
Intraoperative FLIP measurements were taken on 16 patients undergoing POEM. Table 1 shows the patients’ preoperative demographics, disease characteristics, and manometric measurements.
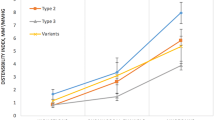
The completed POEM resulted in a significant increase in DI (mean pre 1.2 ± .8 vs. mean post 7.2 ± 2.7 mm2/mmHg, p < .001), and the stepwise changes during the procedure are shown in Fig. 1. Creation of the submucosal tunnel, prior to performing any myotomy, resulted in a threefold increase in DI (mean pre 1.2 ± .8 vs. post 3.6 ± 1.9 mm2/mmHg, p < .001). When the myotomy was performed in an incremental fashion from proximal to distal, the initial esophageal myotomy (to 1 cm proximal to the EGJ) had no effect on DI (mean pre 3.6 ± 1.9 vs. post 3.8 ± 1.8 mm2/mmHg, p = .76). Subsequent myotomy extension across the LES complex (to 1 cm distal to the EGJ) resulted in an increase in DI (mean pre 3.8 ± 1.8 vs. post 6.2 ± 2.4 mm2/mmHg, p < .001), as did the initial gastric myotomy extension (to 2 cm distal to the EGJ) (mean pre 6.2 ± 2.4 vs. post 7.0 ± 2.4 mm2/mmHg, p < .001). The final gastric myotomy extension (to 3 cm distal to the EGJ) had no further effect on DI (mean pre 7.0 ± 2.4 vs. post 7.2 ± 2.7 mm2/mmHg, p = .46).
Stepwise changes in EGJ distensibility index (DI) are shown over the subsequent steps of POEM. Creation of the submucosal tunnel increased DI. The initial esophageal myotomy had no effect on DI. Subsequent myotomy across the lower esophageal sphincter complex to 1 cm distal to the EGJ increased DI, as did an initial gastric extension to 2 cm. Final gastric extension of the myotomy to 3 cm distal to the EGJ did not further affect DI
Discussion
The major finding of this study was that two main steps of the POEM procedure, creation of the submucosal tunnel and the myotomy segment immediately across the EGJ, accounted for the majority of the increase in distensibility attributable to the operation. Extension of the myotomy 2 cm onto the stomach wall resulted in a small but significant augmentation of this effect, but further lengthening of the myotomy to 3 cm past the EGJ did not increase distensibility further.
The threefold increase in distensibility after submucosal tunnel creation is an interesting effect that we have similarly observed in prior studies [10, 18]. While it appears from these results that ablation of the submucosal layer has a significant effect on EGJ physiology, it is unclear whether this is due to the normal role the submucosa plays in maintaining the structural integrity of the EGJ, or rather a consequence of pathologic change that occurs in the submucosa as a result of achalasia. Regardless, we now consider complete ablation of the submucosal fibers across the EGJ to be an essential therapeutic component of POEM and always take independent FLIP measurements after both submucosal tunneling and myotomy creation, in order to ensure that each step has independently contributed to increasing EGJ distensibility.
Little data currently exist to guide surgeons as to how far to extend the gastric myotomy during laparoscopic Heller myotomy or POEM. Oelschlager and colleagues showed that during laparoscopic Heller, a myotomy extending to 3 cm onto the stomach achieved superior reductions in EGJ pressures and improved symptomatic outcomes when compared with a shorter distal myotomy to 1.5 cm5. However, Salvador and colleagues found no difference in either EGJ pressures or postoperative symptoms in Heller’s with either a short (1.5–2 cm) or a long (2.5–3 cm) distal gastric myotomy extension [7]. During POEM, most surgeons create a distal myotomy of 2–3 cm past the EGJ [2, 15], although no data currently exist regarding the efficacy of variable distal myotomy lengths specifically for POEM. The results of the current study suggest that a myotomy to 1 cm distal to the EGJ is responsible for the majority of the change in distensibility during POEM, from a baseline of 1.2 to 6.2 mm2/mmHg. Our previous work suggests that a final intraoperative distensibility in the range of 4.5–8.5 mm2/mmHg results in optimal symptomatic outcomes by relieving dysphagia while limiting iatrogenic gastroesophageal reflux (which occurs in patients with higher final distensibilities). Studies of healthy volunteers have shown similar average distensibilities in the range of 5–8 mm2/mmHg [8, 9]. In the current study, lengthening the myotomy to 2 cm onto the gastric wall resulted in a small increase in distensibility to 7.0 mm2/mmHg, while extension to 3 cm did not further increase this value. Prior studies of EGJ physiology have shown the LES high-pressure zone to span a total of approximately 4 cm from proximal to distal, with 2 cm lying caudal to the SCJ [19]. However, newer data, using three-dimensional high-resolution manometry catheters to isolate the impact of the LES from the contribution of the crural diaphragm, have demonstrated this high-pressure zone to be shorter than previously thought, with less than 1 cm distal to the SCJ [20, 21]. This correlates with our current study’s results, showing a normalization of distensibility after the creation of the myotomy to only 1 cm distal to the EGJ.
Despite our current findings, we caution against interpreting these results to mean that during POEM, a myotomy 1 cm onto the stomach wall is sufficient to achieve optimal dysphagia relief. Firstly, at this point in the operation in our study, a submucosal tunnel had already been created to at least 3 cm distal to the EGJ. As creation of the submucosal tunnel has such a significant effect on distensibility, if POEM were to be performed with a shorter tunnel to 1 cm distal to the EGJ, along with a shorter myotomy, it may be insufficient to normalize EGJ physiology. Secondly, although average EGJ distensibility had been normalized after the creation of a myotomy 1 cm distal to the EGJ, individual patients within the cohort still had a rather wide range of distensibility at this point in the operation, from 2.5 to 10.5 mm2/mmHg. As patients with a distensibility of less than 2.9 mm2/mmHg have been shown to have inferior symptomatic outcomes [9], some of the patients in our cohort clearly required a distal myotomy extension longer than 1 cm. Based on this, it appears that rather than extrapolating a fixed optimal distal myotomy length from these data, they argue for the use of FLIP as an instrument to intraoperatively assess myotomy adequacy and thus tailor distal length to individual patient physiology. FLIP has been used to this effect in one study in which myotomy length during laparoscopic Heller was tailored according to intraoperative distensibility measurements [22]. The authors found that with the use of this technique, the myotomy length could be shortened while achieving similar symptomatic outcomes as in Heller’s without FLIP guidance.
This study has some limitations. Since sequential myotomy extensions were performed in each case, every patient ended their operation with the same final 3-cm distal gastric myotomy length. As such, we are unable to subsequently assess the physiologic and symptomatic consequences of variable distal myotomy lengths. Additionally, we relied on the luminal location of the SCJ in order to measure the stepwise myotomy extensions. While these lengths should translate when the endoscope is within the submucosal tunnel during myotomy creation, bending of the endoscope shaft during this step may have caused minor variations and error in these distance measurements. Performing the distal myotomy in increments as short as 1 cm may have also introduced variability and error between patients.
In conclusion, in patients undergoing POEM, submucosal tunnel creation and performing a myotomy across the high-pressure zone of the EGJ to 1 cm distal to the SCJ resulted in the normalization of intraoperative distensibility. While subsequent extension of the distal myotomy to 2 cm onto the stomach wall further increased compliance, lengthening to 3 cm had no additional effect. These results provide further evidence that FLIP may serve as a useful tool for monitoring the effect of operations for achalasia in real time, with the goal of tailoring myotomy length to individual patient physiology and anatomy in order to achieve optimal outcomes.
References
Triadafilopoulos G, Boeckxstaens GE, Gullo R, Patti MG, Pandolfino JE, Kahrilas PJ, Duranceau A, Jamieson G, Zaninotto G (2012) The Kagoshima consensus on esophageal achalasia. Dis Esophagus 25:337–348
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Teitelbaum EN, Soper NJ, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Hirano I, Hungness ES (2014) Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg Endosc 28:3359–3365
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259:1098–1103
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138:490–495 discussion 5–7
Wright AS, Williams CW, Pellegrini CA, Oelschlager BK (2007) Long-term outcomes confirm the superior efficacy of extended Heller myotomy with Toupet fundoplication for achalasia. Surg Endosc 21:713–718
Salvador R, Caruso V, Costantini M, Parise P, Nicoletti L, Cavallin F, Zanatta L, Bardini R, Ancona E, Zaninotto G (2014) Shorter myotomy on the gastric site (≤2.5 cm) provides adequate relief of dysphagia in achalasia patients. Dis Esophagus. doi:10.1111/dote.12226
Pandolfino JE, de Ruigh A, Nicodeme F, Xiao Y, Boris L, Kahrilas PJ (2013) Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil 25:496–501
Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 143:328–335
Teitelbaum EN, Boris L, Arafat FO, Nicodeme F, Lin Z, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodeme F, Lin Z, Hungness ES (2015) Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 29:522–528
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Eckardt VF (2001) Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Clouse RE, Staiano A, Alrakawi A, Haroian L (2000) Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol 95:2720–2730
Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, Soper NJ (2013) Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 17:228–235
McMahon BP, Frokjaer JB, Kunwald P, Liao D, Funch-Jensen P, Drewes AM, Gregersen H (2007) The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol 292:G377–G384
Perretta S, McAnena O, Botha A, Nathanson L, Swanstrom L, Soper NJ, Inoue H, Ponsky J, Jobe B, Marescaux J, Dallemagne B (2013) Acta from the EndoFLIP(R) Symposium. Surg Innov 20:545–552
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Boris L, Nicodeme F, Lin Z, Hungness ES (2014) An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc 28:2840–2847
Ayazi S, Hagen JA, Zehetner J, Ross O, Wu C, Oezcelik A, Abate E, Sohn HJ, Banki F, Lipham JC, DeMeester SR, Demeester TR (2009) The value of high-resolution manometry in the assessment of the resting characteristics of the lower esophageal sphincter. J Gastrointest Surg 13:2113–2120
Kwiatek MA, Pandolfino JE, Kahrilas PJ (2011) 3D-high resolution manometry of the esophagogastric junction. Neurogastroenterol Motil 23:e461–e469
Nicodeme F, Lin Z, Pandolfino JE, Kahrilas PJ (2013) Esophagogastric Junction pressure morphology: comparison between a station pull-through and real-time 3D-HRM representation. Neurogastroenterol Motil 25:e591–e598
Ilczyszyn A, Hamaoui K, Cartwright J, Botha A. (2015) Intraoperative distensibility measurement during laparoscopic Heller’s myotomy for achalasia may reduce the myotomy length without compromising patient outcome. Dis Esophagus. doi:10.1111/dote.12343
Acknowledgments
This work was supported by R01 DK56033 (PJK) and R01 DK092217 (JEP) from the Public Health Service. The authors would like to acknowledge Rowena Martinez, RN, and Colleen Krantz, RN, for their help in coordinating the clinical aspects of this study.
Disclosures
Nathaniel Soper is on the scientific advisory boards of TransEnterix and Miret Surgical, which are unrelated to this study. Eric Hungness receives an honorarium for educational activities from Baxter, which is unrelated to this study. Ezra Teitelbaum, Joel Sternbach, Rym El Khoury, John Pandolfino, Peter Kahrilas, and Zhiyue Lin have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teitelbaum, E.N., Sternbach, J.M., El Khoury, R. et al. The effect of incremental distal gastric myotomy lengths on EGJ distensibility during POEM for achalasia. Surg Endosc 30, 745–750 (2016). https://doi.org/10.1007/s00464-015-4269-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4269-8