Abstract
Background and study aims
Narrow band imaging (NBI) combined with magnifying endoscopy enables us to detect superficial laryngo-pharyngeal cancers, which are difficult to detect by standard endoscopy. Endoscopic laryngo-pharyngeal surgery (ELPS) is a technique developed to treat such lesions and the purpose of this study is to evaluate the usefulness of ELPS for superficial laryngo-pharyngeal cancer.
Patients and methods
Seventy five consecutive patients with 104 fresh superficial laryngo-pharyngeal cancers are included in this study. Under general anesthesia, a specially-designed curved laryngoscope was inserted to create a working space in the pharyngeal lumen. A magnifying endoscope was inserted transorally to visualize the field and a head & neck surgeon dissected the lesion using the combination of the orally-inserted curved grasping forceps and electrosurgical needle knife in both hands. The safely, functional outcomes, and oncologic outcomes of ELPS were evaluated retrospectively.
Results
Median operation time per lesion was 35 min. Post-operative bleeding occurred in 3 cases and temporal subcutaneous emphysema occurred in 10 cases. No vocal fold impairment occurred after surgery. The median fasting period was 2 days and all patients except one have a normal diet with no limitations. Local recurrence occurred in 1 case, and the 3-year overall survival rate and the 3-year disease specific survival rate was 90 % and 100 %, respectively.
Conclusions
ELPS is a hybrid of head and neck surgery and gastrointestinal endoscopic treatment, and enjoys the merit of both procedures. ELPS makes it possible to perform minimally-invasive surgery, preserving both the swallowing and phonation functions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laryngo-pharyngeal cancer is often advanced when detected and has a relatively poor prognosis. Surgery for advanced cases impairs swallowing and/or vocal function, and chemoradiotherapy sometimes causes serious adverse effects involving severe swallowing disorders and permanent salivary gland dysfunction. Early detection of the tumor is important because it not only improves survival rate but also minimizes functional loss of swallowing and voice. We have previously reported that narrowband imaging (NBI) combined with magnifying endoscopy is useful in detecting early superficial laryngo-pharyngeal cancers, which are difficult to detect by standard endoscopy [1–3]. For such superficial lesions, we have reported endoscopic submucosal dissection (ESD) [4]. In this procedure, the cancerous lesion with safety margin is resected with minimal invasion using a knife needle inserted through a flexible gastrointestinal endoscope. Shimizu et al. [5] and Iizuka et al. [6] have also reported the usefulness of endoscopic resection for laryngo-pharyngeal cancer. However, there were limitations to the procedure including longer surgical time and technical difficulties because each procedure was performed with one “hand” through an endoscope. Here we report a technique of “endoscopic laryngo-pharyngeal surgery (ELPS)” in which a lesion is resected using two orally inserted “hands” under the assistance of a flexible gastrointestinal endoscope.
Patients and methods
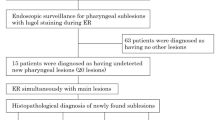
During the period from August 2009 to January 2014, 104 consecutive fresh superficial laryngo-pharyngeal cancers in 75 patients were treated with ELPS under general anesthesia at Kyoto University Hospital. Written informed consent for the treatment was obtained from all patients, and this study was approved by the institutional review board of the Graduate School of Medicine, Kyoto University.
Histological diagnosis of the lesions was made in accordance with the World Health Organization classification of tumors (head and neck tumors). Evaluation of the invasion of the tumor was also made according to the general rules for clinical studies of head and neck cancer by the Japanese Society for Head and Neck Cancer [7] and the Japanese classification of esophageal cancer by the Japan Esophageal Society [8]. If the lesion was diagnosed as carcinoma in situ or carcinoma with invasion to the subepithelial layer (not to the muscular layer), ELPS was indicated as a minimally invasive treatment. All lesions were detected by NBI with a magnifying endoscope and histologically confirmed by biopsy specimen as high-grade dysplasia/carcinoma in situ or squamous cell carcinoma.
The concept of ELPS is the same as that of ESD in that both perform en bloc resection of a cancer lesion following submucosal injection, but it differs from ESD in that the resection procedure is performed by a head and neck surgeon with both hands [9]. Under general anesthesia, a curved rigid laryngoscope (Nagashima Medical Instruments Company, Ltd, Tokyo, Japan) was inserted to provide a working space in the pharyngeal lumen, and a magnifying endoscope (GIF TYPE H260Z, Q240Z, or Q260J; Olympus Medical Systems, Tokyo, Japan) was inserted transorally by a gastroenterologist to visualize the surgical field (Fig. 1). The combination of the curved laryngoscope (Fig. 2A) and the magnifying endoscope provides an excellent surgical field of the whole hypopharynx including the apex of the piriform sinus, the post-cricoid region, and the entrance of the esophagus (Fig. 2B). Tumor resection was performed by a head and neck surgeon with the assistance of a gastroenterologist. The extent of the lesion and the exact margins were determined by NBI and iodine staining. Specially designed curved forceps (Nagashima Medical Instruments Company, Ltd, Tokyo, Japan) developed by Sato et al. [9] and a curved electrosurgical needle knife (Olympus Medical Systems, Tokyo, Japan) (Fig. 3C, D and E) were orally inserted, and the margin of the lesion was marked using the needle knife (Olympus Medical Systems, Tokyo, Japan) in coagulation mode (Fig. 3A, B). A mixed solution of epinephrine (0.02 mg/mL) and saline was injected into the subepithelial layer beneath the lesion, to lift the lesion above the surrounding mucosa and to create a safety space. The space lifts the lesion to facilitate its removal and minimizes damage to the deep layers of the laryngo-pharyngeal wall. A circumferential incision into the submucosa was then created around the lesion, and the lesion was dissected from the pharyngeal wall (Fig. 3C–F). The cutting and dissection procedure was performed using the combination of the orally inserted curved grasping forceps in one hand and the orally inserted curved electrosurgical needle knife in the other hand. After resection, iodine staining was repeated as necessary to confirm complete resection and sodium thiosulfate was sprayed to reutilize the iodine irritation. The laryngo-pharyngeal mucosa was checked before extubation, and prophylactic tracheostomy was performed if severe mucosal swelling was observed. The patient was extubated immediately after surgery if there was no or mild mucosal swelling. Endoscopic examination was performed a day after the operation to check the wound. The fasting period was usually 1–2 days after surgery. If subcutaneous emphysema developed after surgery, the patient continued fasting for a week and was administered with antibiotics.
Instrumentation. A Curved laryngoscope, B surgical field visualized by the flexible gastrointestinal endoscope and the curved laryngoscope. The whole hypopharynx is clearly visualized including the post-cricoid region and the apex of the piriform sinus. C Curved forceps developed by Sato et al. [9]. D Electric needle knife developed by Sato et al. [9]. E Tip of the electric needle knife. The length of the needle can be adjusted manually. The point of the needle is designed to be rounded in shape to avoid damage to the deeper tissue
Surgical procedure. A Early hypopharyngeal cancer in the right piriform sinus. B Resection margin marked by coagulation after observation by narrowband imaging and iodine staining. C A circumferential incision into the submucosa was performed around the lesion following submucosal hydrodissection with a mixed solution of glycerol, epinephrine, and saline. D, E The tumor was resected using the electric needle knife and curved forceps. F Resected specimen
All resected specimens were cut into longitudinal slices 2 mm in width. The slices were embedded in paraffin and stained with hematoxylin–eosin. All specimens were microscopically evaluated according to the World Health Organization classification. Staging was performed according to the Union for International Cancer Control tumor–node–metastasis (UICC/TNM) classification (seventh edition).
The results of continuous number are expressed as median (range). For the evaluation of operation time, the operation time in multifocal cases was divided by the number of lesions resected in that operation and was defined as operation time per lesion. Swallowing function was evaluated using the FOSS score more than 3 months following surgery. Hoarseness was evaluated using the GRBAS scale by a speech pathologist more than 3 months after surgery, and a score of more than grade 2 was defined as hoarseness. Cause-specific and overall survival rates were estimated using the Kaplan–Meier method.
Results
Patient characteristics are shown in Table 1. Patients were predominantly male (96 %), and the median age was 68 years (range 44–85 years). Of the 75 patients, 54 (72 %) had esophageal cancer synchronously or previously, and 22 patients (29 %) had multiple head and neck cancer synchronously or previously.
Lesion characteristics are shown in Table 2. Of the 104 lesions resected, the number of lesions in the oropharynx, hypopharynx, and larynx was 28 (27 %), 74 (71 %), and 2 (2 %), respectively. In the oropharynx, the number of lesions in the anterior wall, posterior wall, superior wall, and lateral wall was 4 (14 %), 14 (50 %), 5 (18 %), and 5 (18 %), respectively. In the hypopharynx, the number of lesions in the piriform sinus, post-cricoid, and posterior wall was 59 (80 %), 3 (4 %), and 12 (16 %), respectively. In the larynx, two lesions were in the supraglottic area. Multifocal superficial cancer was resected in 16 operations. Regarding the TNM classification, 72 lesions were pathologically diagnosed as Tis, 18 lesions as T1, 11 lesions as T2, and three lesions as T3. No case, except for one N2a case, had neck lymph node metastasis at the initial treatment. No case had distant metastasis.
Operation data are shown in Table 3. Tumor resection was performed by ELPS in 98 lesions, by a combination of ELPS and ESD in five lesions and by a combination of ELPS and microlaryngoscopic surgery in one lesion. The five lesions which needed the combination of ELPS and ESD included two lesions which had spread to the cervical esophagus. For the resection of these two lesions, a gastroenterologist performed the resection of the esophageal portion with ESD, and then the operation was handed over to a head and neck surgeon who resected the hypopharyngeal portion, resulting in en bloc resection of the whole lesion. Median operation time per lesion was 35 min (range 6–206 min).
Postoperative course and functional outcomes are summarized in Table 4. Prophylactic tracheostomy was performed in three cases during operation, and the median fasting period was 2 days (range 1–22 days). Regarding adverse effects, postoperative bleeding occurred in three cases, one of which needed emergency tracheostomy. Subcutaneous emphysema occurred in ten cases after the procedure, and all were controlled conservatively. No vocal fold impairment occurred after surgery, and no hoarseness occurred. All patients except one have a normal diet with no limitations, and the average FOSS score was 1.0.
During the median follow-up period of 29 months (range 4–59 months), local recurrence occurred in one case, which was controlled by repeating the same procedure. Postoperative neck lymph node metastasis developed in two cases, and both were controlled by neck dissection followed by radiation therapy. Seven patients died of other diseases, and the causes of death were esophageal cancer in four cases, lung cancer in one case, myelodysplastic syndromes in one case, and aspiration pneumonia in one case because of the preexisting unilateral vocal fold paralysis and esophageal stenosis due to the surgery and radiation therapy for the esophageal cancer. The 3-year overall survival rate was 90 %, and the 3-year disease-specific survival rate was 100 % (Fig. 4).
Discussion
The present study demonstrates that ELPS for laryngo-pharyngeal cancer is a feasible treatment option with no severe adverse events. This technology also provided a good prognosis.
NBI enables us to detect superficial laryngo-pharyngeal cancer which has been barely visible by conventional methods. This has provided a breakthrough in diagnosis, and we have applied it to this issue to create a strategy for such early stage cancer because the conventional treatment strategy, including open surgery and chemoradiotherapy, seems to be overtreatment [4].
Transoral surgery is becoming popular as a minimally invasive treatment for laryngo-pharyngeal cancer, since Steiner et al. reported an excellent local control rate while preserving swallowing and voice function [10–12]. To date, several methods have been reported as a minimally invasive transoral surgical approach, such as transoral laser microsurgery (TLM), transoral robotic surgery (TORS) [13–15], transoral videolaryngoscopic surgery (TOVS) [16], and ESD [4, 5], and the merits and demerits of each procedure are becoming evident. It has been reported that TLM for laryngo-pharyngeal cancer results in an excellent organ preservation rate [11, 12]. However, because of the limitation of the surgical field, the tumor has to be divided into piecemeal specimens during resection of a large-size tumor [17], which may increase the potential for local recurrence. TORS is an innovative treatment option which is quickly spreading worldwide. TORS is performed using the da Vinci surgical system and has several merits, such as precise movement, a wide and 3D field of view using a 3D rigid endoscope, and a maximum of four arms (two robotic arms and two arms operated by an assistant) [13, 14]. However, high cost is a big issue regarding robotic surgery. In addition, because of the size of the robotic arm, there are limitations to the exposure and procedure especially in the hypopharynx. Pharyngeal ESD is a technique performed by a gastroenterologist under the assistance of an otolaryngologist. A gastroenterologist resects the mucosa containing the lesion at the subepithelial level using a coagulator and forceps inserted through a flexible endoscope, and, if necessary, an otolaryngologist assists the procedure by retracting the mucosa with orally inserted forceps. ESD is safe and achieves a good local control rate for early laryngo-pharyngeal cancer [4, 5]. However, ESD also has limitations, such as its technical difficulty because of the one-arm procedure through the endoscope and the relatively longer surgical time because of the one-handed operation.
ELPS is a hybrid of head and neck surgery and gastrointestinal endoscopic treatment and has several advantages as a specialized technique for superficial laryngo-pharyngeal cancer. First, the flexible gastrointestinal endoscope together with the curved laryngoscope provides an excellent surgical field. The endoscope has a wide-view angle with high resolution and in combination with the curved laryngoscope makes it possible to view the whole hypopharynx including a post-cricoid lesion and the apex of the piriform sinus. The endoscope magnifies an object up to 70 times and enables to detect morphological change of mucosal structure and microvessels. Second, three arms, an endoscopic channel and both hands, can be used for the procedure, which enables quick and precise surgery. The main procedure is performed by a head and neck surgeon who uses both hands to manipulate an orally inserted curved electrosurgical needle knife and curved forceps, while a gastroenterologist can assist the surgery when necessary. Indeed, the operation time (35 min) in our study was shorter compared to that of ESD (50 min [5]–65.3 min [18]) for pharyngeal cancer previously reported in the literature. Third, ELPS is a less invasive surgical method compared to TLM, TOVS, or TORS, as the subepithelial injection contributes to preservation of deeper structures, such as the intrinsic laryngeal muscles, their fascia, recurrent laryngeal nerves, and internal branches of the superior laryngeal nerve, which are all important for voice and swallowing. Fourth, the surgery is cost-effective compared to other methods, especially in comparison with TORS. Finally, the most important advantage is that ELPS is a collaborative surgery involving a head and neck surgeon and a gastroenterologist. ELPS can therefore cope even with lesions which have spread to the cervical esophagus by combining this technique with ESD during surgery, which is impossible for TLM, TOVS, and TORS.
The limitation of ELPS is the indication. ELPS is not suitable for laryngeal cancer except for supraglottic lesions in the anterior side of epiglottis, because of the surgical field. Intubation tube disturbs surgical filed of laryngeal lumen, and ELPS for the areas is impossible without tracheostomy. Also, it is unclear if ELPS is effective for invasive cancer which invades pharyngeal constrictor muscle. Another limitation of this study is that it is a retrospective study. A prospective, randomized controlled trial should be conducted in the future to compare functional and oncological results with other treatment methods, such as ESD.
In conclusion, ELPS is a hybrid of head and neck surgery and gastrointestinal endoscopic treatment and enjoys the merit of both procedures. ELPS makes it possible to perform minimally invasive surgery, thus preserving both the swallowing and phonation functions as well as the organs. Early detection of superficial laryngo-pharyngeal cancer with NBI and treatment with ELPS offers a new treatment strategy for head and neck cancer.
References
Muto M, Katada C, Sano Y, Yoshida S (2005) Narrow band imaging: a new diagnostic approach to visualize angiogenesis in superficial neoplasia. Clin Gastroenterol Hepatol 3(7 Suppl 1):S16–S20
Muto M, Minashi K, Yano T, Saito Y, Oda I, Nonaka S, Omori T, Sugiura H, Goda K, Kaise M, Inoue H, Ishikawa H, Ochiai A, Shimoda T, Watanabe H, Tajiri H, Saito D (2010) Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: a multicenter randomized controlled trial. J Clin Oncol 28:1566–1572
Muto M, Nakane M, Katada C, Sano Y, Ohtsu A, Esumi H, Ebihara S, Yoshida S (2004) Squamous cell carcinoma in situ at oropharyngeal and hypopharyngeal mucosal sites. Cancer 101:1375–1381
Muto M, Satake H, Yano T, Minashi K, Hayashi R, Fujii S, Ochiai A, Ohtsu A, Morita S, Horimatsu T, Ezoe Y, Miyamoto S, Asato R, Tateya I, Yoshizawa A, Chiba T (2011) Long-term outcome of transoral organ-preserving pharyngeal endoscopic resection for superficial pharyngeal cancer. Gastrointest Endosc 74:477–484
Shimizu Y, Yamamoto J, Kato M, Yoshida T, Hirota J, Ono Y, Nakagawa M, Nakagawa S, Oridate N, Asaka M (2006) Endoscopic submucosal dissection for treatment of early stage hypopharyngeal carcinoma. Gastrointest Endosc 64:255–259
Iizuka T, Kikuchi D, Hoteya S, Yahagi N, Takeda H (2009) Endoscopic submucosal dissection for treatment of mesopharyngeal and hypopharyngeal carcinomas. Endoscopy 41:113–117
Japan Society for Head and Neck Cancer (2012) General rules for clinical studies on head and neck cancer. 5th edn. Kanehara, Tokyo, Japan
Japan Esophageal Society (2008) Japanese classification of esophageal cancer. 10th edn. Kanehara, Tokyo, Japan
Sato Y, Omori Y, Tagawa M (2006) Surgical treatment for hypopharyngeal superficial cancer: endoscopic laryngo-pharyngal surgery. Nihon Jibiinkoka Gakkai Kaiho 109:581–586
Steiner W (1988) Experience in endoscopic laser surgery of malignant tumors of the upper aero-digestive tract. Adv Otorhinolaryngol 39:135–144
Steiner W, Ambrsch P, Hess CF, Kron M (2001) Organ preservation by transoral laser microsurgery in piriform sinus carcinoma. Otolaryngol Head Neck Surg 124:58–67
Steiner W, Fierek O, Ambrosch P, Hommerich CP, Kron M (2003) Transoral laser microsurgery for squamous carcinoma of the base of tongue. Arch Otolaryngol Head Neck Surg 129:36–43
O’Malley BW Jr, Weinstein GS, Hockstein NG (2006) Transoral roboti surgery for tongue base neoplasms. Laryngoscope 116:1465–1472
Weinstein GS, O’Malley BW Jr, Snyder W, Hockstein NG (2007) Transoral robotic surgery: supraglottic partial laryngectomy. Ann Otol Rhinol Laryngol 116:19–23
Park YM, Byeon HK, Chung HP, Choi EC, Kim SH (2013) Comparison study of transoral robotic surgery and radical open surgery for hypopharyngeal cancer. Acta Otolaryngol 133:641–648
Tomifuji M, Araki K, Yamashita T, Shiotani A (2014) Transoral videolaryngoscopic surgery for oropharyngeal, hypopharyngeal, and supraglottic cancer. Eur Arch Otorhinolaryngol 271:589–597
Okami K, Ebisumoto K, Sakai A, Sugimoto R, Maki D, Saito K, Kaneda S, Iida M, Ogura G, Nakamura N, Nishiyama K (2013) Transoral en bloc resection of superficial laryngeal and pharyngeal cancers. Head Neck 35:1162–1167
Iizuka T, Kikuchi D, Hoteya S, Takeda H, Kaise M (2012) A new technique for pharyngeal endoscopic submucosal dissection: peroral countertraction (with video). Gastrointest Endosc 76:1034–1038
Acknowledgments
This study was supported in part by Grants-in-aid for research from the Ministry of Health, Labor, and Welfare of Japan and the Ministry of Education, Culture, Sports, Science, and Technology of Japan. The authors disclose no financial relationship relevant to this publication.
Disclosures
Ichiro Tateya, Manabu Muto, Shuko Morita, Shin’ichi Miyamoto, Tomomasa Hayashi, Makiko Funakoshi, Ikuo Aoyama, Hirokazu Higuchi, Shigeru Hirano, Morimasa Kitamura, Seiji Ishikawa, Yo Kishimoto, Mami Morita, Juichi Ito have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tateya, I., Muto, M., Morita, S. et al. Endoscopic laryngo-pharyngeal surgery for superficial laryngo-pharyngeal cancer. Surg Endosc 30, 323–329 (2016). https://doi.org/10.1007/s00464-015-4213-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4213-y