Abstract
The factors affecting the survival of patients with aspiration pneumonia (AP) remain unclear. This study aimed to determine whether factors, including oral status, swallowing function, and oral intake level, were related to survival outcomes in older patients hospitalized for AP. The study enrolled patients with AP who were admitted to our hospital between February 2017 and November 2019. Patients were divided into two groups based on the 90-day mortality after the first swallowing function evaluation: survivors and deceased. The data were compared between the two groups. A total of 29 patients were diagnosed with AP. Of these patients, 13 died within 90 days. The numbers of patients who could not use removable dentures and required sputum suctioning and had cough reflex at rest were significantly higher in the deceased than in the survivors. The salivary pooling and pharyngeal clearance scores evaluated by videoendoscopy, International Dysphagia Diet Standardisation Initiative Functional Diet Scale score determined after swallowing function evaluation, and consciousness level were significantly worse in the deceased than in the survivors. There were significant differences in patients’ oral status, swallowing function, oral intake level, and consciousness level between the survivors and deceased.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Pneumonia is one of the leading causes of death in Japan. In 2019, 95,498 people died from non-aspiration pneumonia (non-AP), accounting for 6.9% of total deaths, and 40,354 people died from aspiration pneumonia (AP), accounting for 2.9% of total deaths, according to a report from the Ministry of Health, Labor, and Welfare [1]. Teramoto et al. [2] reported that the prevalence of AP in community-acquired pneumonia and hospital-acquired pneumonia was high and increased with age (from nearly 20% in those aged 50–59 years to 80% in patients aged ≥ 70 years). Patients with AP exhibit frequent recurrence of pneumonia and higher mortality than non-AP patients [3] because AP is considered to arise through repeated aspiration due to declines in swallowing and/or airway protective functions. In Japan with its aging population, understanding the pathophysiology of AP in older adults is a critical medical issue.
The occlusal contact points between the maxilla and mandible in the molar regions are lost because of decreased numbers of teeth associated with dental caries and periodontal disease. Loss of these contact points reduces chewing efficiency and limits food intake. According to a Japanese longitudinal study, the percentage of people who had no occlusal contact points in the posterior region at all was 26.3% in their 70 s, compared with 10.9% in their 60 s and 1.1% in their 50 s [4]. Recent studies have shown that recovery of occlusal support by wearing dentures contributes to improvements in not only food intake, but also bolus formation and propulsion [5, 6]. These findings suggest that older adults exhibit worsening oral conditions and increasing risk of dysphagia as they continue to age.
Clinical and biological indicators such as age, respiratory rate, body temperature, serum total protein level, serum albumin level, serum creatinine level, and C-reactive protein (CRP) level have been identified as factors related to survival in older patients with AP [7,8,9]. However, there are few studies on the relationships between survival and oral status, swallowing function, and oral intake level [10,11,12,13].
This study aimed to determine whether oral status, swallowing function, and oral intake level were related to survival outcomes in older patients hospitalized for AP.
Materials and Methods
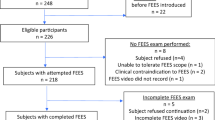
Study Design and Subjects
This was a retrospective study conducted from February 2017 to November 2019. All participants were inpatients at Minamiuonuma City Yukiguni Yamato Hospital and referred to the Department of Dentistry after being diagnosed with AP by their attending physicians. AP’s diagnosis was based on the Clinical Practice Guidelines for Nursing and Healthcare-associated Pneumonia [14]. The patients underwent an assessment of oral health status and swallowing function by dentists responsible for dysphagia rehabilitation. All of these dentists were well trained and had > 5 years of clinical experience in dental practice and dysphagia rehabilitation. The exclusion criteria were as follows: (1) patients with history of head and neck cancer and neurologic impairment except for dementia (e.g., Parkinson disease, amyotrophic lateral sclerosis) because these diseases significantly affect swallowing function and can be a confounding factor and (2) patients with end-stage cancers or serious life-threatening diseases other than AP. The study received approval from the Ethics Committee of Minamiuonuma City Yukiguni Yamato Hospital (R2-001) and was performed in accordance with the Declaration of Helsinki.
Baseline Characteristics
Baseline data on age, sex, prehospital residence (home or nursing home), survival duration after first evaluation of swallowing function, presence or absence of dementia diagnosis before hospitalization, and history of AP and cerebrovascular diseases were collected from medical records.
Oral Status
Oral status was evaluated by number of remaining teeth, use of dentures, and distribution of occlusal support in the molar region using the Eichner index (EI) [15]. A Residual root tooth not involved in occlusion was counted as missing tooth. The EI was determined by existing contact points between natural teeth in the maxilla and mandible in the bilateral premolar and molar regions and categorized into three types: Class A, contact in four occlusal supporting zones; Class B, contact in one to three supporting zones or contact in the anterior region only; and Class C, no occlusal contact at all. The number of teeth and EI was expressed both with and without dentures. Patients who corresponded to Class B/C and Class A in the EI were classified as the denture-required group and denture-non-required group, respectively. The denture-required group was further subdivided into two groups: denture-usage group and denture-non-usage group. The denture-non-usage group included those who did not own dentures or owned dentures but could not use them.
Swallowing Function
Swallowing function was evaluated by the following findings at rest and mealtimes: necessity of sputum suctioning at rest and existence of cough reflex and wet hoarseness at rest and mealtimes. The 10-item Eating Assessment Tool (EAT-10) [16], repetitive saliva-swallowing test (RSST) [17, 18], and fiberoptic endoscopic evaluation of swallowing (FEES) were also conducted. These assessments were performed by medical staff within the dysphagia rehabilitation team at the hospital. The EAT-10 is a short 10-item self-administered questionnaire. Each item is rated on a five-point scale (0–4), giving a summed score ranging from 0 to 40 (higher score implies more abnormality). The Japanese version of the tool translated by Wakabayashi et al. [19] was used in this study. A sum of ≥ 3 is considered abnormal. For the RSST, the patient’s hyoid bone and laryngeal movements were palpated, and the number of saliva-swallowing movements in 30 s was counted and recorded. For the FEES, we adopted the Hyodo scoring method [20]. This method has four parameters: (1) salivary pooling at the vallecula and piriform sinuses; (2) glottal closure reflex induction by touching the epiglottis or arytenoid with the endoscope; (3) swallowing reflex initiation assessed by “white-out” timing (white-out defined as period when endoscopic image is obscured by pharyngeal closure); and (4) pharyngeal clearance after swallowing blue-dyed water. Three milliliters of moderately thickened liquid was used as the test material in all cases and thus used for scoring. The moderately thickened liquid was equivalent to “code 0t” in the Japanese Dysphagia Diet 2013, developed by the Japanese Society of Dysphagia Rehabilitation Dysphagia Diet Committee [21], and is recommended for swallowing function evaluation in patients with severe dysphagia. It was equivalent to “level 2” or “level 3” in the International Dysphagia Diet Standardisation Initiative [22]. The four parameters were each scored as 0–3 on a 4-point scale: 0, normal; 1, mildly impaired; 2, moderately impaired; 3, severely impaired. The Hyodo score was expressed as the sum of the scores for the four parameters and ranged from 0 to 12. Because the patients in the present study were aged, enrolled immediately after onset of AP, and had a risk of vasovagal syncope and laryngospasm [23], evaluation of the glottal closure reflex by touching the epiglottis or arytenoid was not performed in most cases and was therefore excluded from the evaluation items. The FEES findings were scored by one trained dentist who was blind to patient’s clinical information and had > 5 years of clinical experience in swallowing rehabilitation.
Oral Intake Level
Oral intake level was evaluated by the existence and necessity of liquid thickening, meal assistance, and posture adjustment, as well as the Functional Oral Intake Scale (FOIS) score [24]. The FOIS scores ranged from 1 (nothing by mouth) to 7 (total oral diet with no restrictions). The FOIS score on the day of hospitalization was determined by interviews with the patient, their family members, and nurses at their nursing home. Recommended diet and viscosity of thickened liquid for the patients were determined by comprehensive discussions between physicians and dentists considering the patient’s general condition, oral status, and swallowing function and scored by International Dysphagia Diet Standardisation Initiative Functional Diet Scale (IDDSI-FDS) [25]. The IDDSI-FDS scores range from 0 (no recommend for oral intake) to 8 (no need to adjust food type or thicken liquid).
Clinical and Biological Status
The patient’s consciousness level at the first swallowing function evaluation was assessed by the number of digits in the Japan Coma Scale (JCS) [26]. The scale is composed of four main categories: JCS-0, JCS-one, JCS-two, and JCS-three digit codes corresponding to alert, awake without stimuli, arousable with some stimuli (but reverting to previous status if stimuli stop), and unarousable by any forceful stimuli, respectively. The body mass index, serum total protein level, and serum albumin level on the day of hospitalization were used as indicators of nutritional status, and the white blood cell count and CRP level were used as indicators of inflammatory status.
Statistical Analyses
Patients were divided into two groups based on the 90-day mortality after the first swallowing function evaluation in accordance with previous studies [13, 27, 28]: survivors and deceased. In the oral intake level analysis, data were compared before and after swallowing function evaluation. Data were reported as percentage for categorical variables and median with interquartile range (IQR: 25%–75%) for continuous or ordinal variables. Non-parametric tests were used because the Shapiro–Wilk normality test showed that none of the data were normally distributed. The significance of differences between the two groups was evaluated by the Mann–Whitney U test for continuous or ordinal variables and Fisher’s exact test for categorical variables. For each test, a value of p < 0.05 was considered significant. All statistical analyses were conducted using SPSS version 22.0 software (IBM Japan, Tokyo, Japan).
Results
During the study period, a total of 29 patients were diagnosed with AP. No patients met the exclusion criteria. The mean age ± standard deviation of the patients was 89.4 ± 5.0 years, and 14 patients (48.3%) were men. Thirteen patients (44.8%) died within 90 days after the first swallowing function evaluation. The median survival in the deceased was 30.0 (IQR 22.0–59.0) days. The median duration of hospitalization in the survivors was 35.5 (IQR 13.5–52.5) days. The median times from day of hospitalization to first evaluation of oral status/swallowing function and from first evaluation of oral status/swallowing function to FEES were 4.5 (IQR 3.0–7.5) days and 2.0 (IQR 0.0–5.5) days in the survivors, and 5.0 (IQR 3.0–7.5) days and 2.0 (IQR 0.0–7.0) days in the deceased, respectively, with no significant differences between the two groups (p = 0.740 in the former; p = 0.768 in the latter). The patients’ baseline data are shown in Table 1. There were no significant differences in baseline characteristics between the two groups.
The patients’ oral statuses are shown in Table 2. No patients were categorized as Class A in the EI. All patients required use of dentures. There were significantly more patients in the survivors who were able to use their dentures compared with the deceased (p = 0.038), and the number of teeth after wearing their dentures tended to be higher (p = 0.086). There were significant differences in the ratio of Class A and Class B/C in the EI between the survivors and deceased (p = 0.007).
The patients’ swallowing functions are shown in Table 3. The numbers of patients who required sputum suctioning (p = 0.001) and had cough reflex (p = 0.030) at rest were significantly higher in the deceased than in the survivors. Many patients in both groups were unable to follow our instructions and perform the EAT-10 and RSST. Only 3 of 16 (18.8%) patients in the survivors and 1 of 13 (7.7%) patients in the deceased were able to perform the EAT-10. All patients in both groups scored more than the cut-off value of 3 in the EAT-10. The RSST could be performed by 10 of 16 (62.5%) patients in the survivors and 6 of 13 (46.2%) patients in the deceased. In the RSST, 8 of 10 (80.0%) patients in the survivors and 5 of 6 (83.3%) patients in the deceased scored less than the cut-off value of 3. In both groups, most patients required posture adjustment during the FEES. The median reclining angle was 60.0 (IQR 47.5–72.5) degrees in the survivors and 50.0 (IQR 40.0–60.0) degrees in the deceased, with no significant difference between the two groups. The salivary pooling score (p = 0.004), pharyngeal clearance score (p = 0.003), and total score (p = 0.000) were significantly higher in the deceased than in the survivors.
The comparison of oral intake levels between the survivors and the deceased are shown in Table 4. The number of patients who used a thickener before swallowing function evaluation was significantly higher in the deceased than in the survivors (p = 0.029). After the swallowing function evaluation, the numbers of patients judged to require meal assistance (p = 0.018) and posture adjustment (p = 0.018) were significantly higher in the deceased than in the survivors. There were no patients with tube feeding at the time of hospitalization (FOIS score: ≥ 4) in both groups. There was no difference in the median FOIS scores between the two groups, while the median IDDSI-FDS score was significantly lower in the deceased than in the survivors (p = 0.000).
The comparison of oral intake levels before and after swallowing function evaluation are shown in Table 5. Significantly more patients were judged to need a thickener in the survivors (p = 0.033) and posture adjustment in the deceased (p = 0.037) after assessment of swallowing function compared with before the assessment.
The patients’ clinical and biological statuses are shown in Table 6. In the survivors, 6 (37.5%), 8 (50.0%), and 2 (12.5%) of 16 patients showed JCS-0, JCS-one, and JCS-two digit codes, respectively. In the deceased, 8 (61.5%) and 5 (38.5%) of 13 patients showed JCS-one and JCS-two digit codes, respectively. No patients showed JCS-three digit codes in both groups. The JCS-digit code was significantly higher in the deceased than in the survivors (p = 0.013). There were no significant differences in nutritional and inflammation indicators.
Discussion
In this study, we investigated factors related to survival outcomes in older patients hospitalized for AP. There were significant differences in the patients’ oral status, swallowing function, oral intake level, and conscious level between the survivors and the deceased.
More patients were unable to use removable dentures in the deceased compared with the survivors. This result suggests that the ability to use dentures and the recovery of occlusal support may be related to the survival of older patients with AP. In a study on healthy older adults aged 50–79 years, 96.4% of those who lost occlusal support had dentures [4]. However, 12 of 13 patients in the deceased were unable to use dentures at the time of hospitalization in the present study. Because the patients had lost multiple teeth and corresponded to Class B or C in the EI, they might have used dentures in the past. We speculate that they would have been unable to use their dentures before hospitalization because of impairment in the cognitive and/or oral functions allowing use of their dentures. Central nervous system (CNS) diseases, such as cerebrovascular disease, reduce the neuroplastic capacity of the orofacial sensorimotor function [29], and severe dementia leads to orofacial apraxia [30]. These findings suggest that it is difficult for older adults with CNS diseases, including dementia, to adapt to changes in their oral conditions, such as wearing and using dentures. Taji et al. [31] investigated the relationship between mental status in dementia patients and denture acceptance using the Mini-Mental Status Examination (MMSE). They reported that the MMSE score for patients who did not accept dentures was significantly lower than that for those who did accept and wear dentures, suggesting that the severity of dementia affects denture acceptance. In the present study, although there were no differences in age or prevalence of cerebrovascular disease and dementia, we could not consider the severity of these diseases because the sample size was small. Additionally, most patients could not follow our instructions and perform any cognitive ability tests due to their characteristics. We need to consider these limitations in the present study. There are many cases where patients with advanced dementia cannot wear dentures or remove the dentures themselves and consequently need the cooperation of caregivers for use of their dentures. It is also necessary to consider the possibility that use of dentures was discontinued at the discretion of their caregivers, including their family members.
We evaluated the swallowing function using the FEES. Compared with the survivors, the salivary pooling score, pharyngeal clearance score, and total score in the Hyodo scoring method were significantly higher in the deceased. Chiba et al. [32] reported that a total score exceeding 6 for the four parameters (range: 0–12) in the Hyodo scoring method was a predictive factor for aspiration. In the present study, the glottal closure reflex was not included in the evaluation parameters. Therefore, the total score may increase by 0–3 points depending on the patient’s function. Furthermore, although a non-thickened liquid is used as the test food in the conventional Hyodo method, a thickened liquid was used in our study. A thickened liquid was reported to have a lower risk of aspiration than a non-thickened liquid [33]. If a non-thickened liquid had been used as a test food, the scores would have been worse. Based on these findings, it is considered that the deceased with a median total score of 6 had severe swallowing disorders and a high risk of aspiration. Therefore, pneumonia may have been worsened by these factors, which may have contributed to the survival of older AP patients.
Wearing of dentures contributes to improvements in not only the oral preparatory phase (food processing) and oral propulsive phase (stage II transport and bolus aggregation), but also the pharyngeal phase of deglutition [5, 6, 34, 35]. Yamamoto et al. [5] reported that the absence of dentures in edentulous patients altered the anatomical structure and functional movements in the oral cavity and pharynx, resulting in poor bolus transport in the feeding sequence. Yoshikawa et al. [35] reported that the food bolus more frequently penetrated the larynx in individuals not wearing complete dentures than in those wearing such dentures. In this study, more patients were unable to wear dentures in the deceased. Therefore, it is possible that not wearing dentures indirectly increased the risk of aspiration of foods and saliva and thus exacerbated pneumonia. The degree of cognitive decline may also have affected the pharyngeal phase of the deglutition. Although cognitive ability tests needed to be performed to elucidate these relationships in more detail, the patients in this study could not do it due to their characteristics.
The RSST and questionnaires such as the EAT-10 are widely used in clinical fields for dysphagia rehabilitation in Japan because they are easy to carry out and useful as screening methods because of their high sensitivity and specificity for dysphagia [18, 36]. Nevertheless, only a few patients were able to perform these tests due to the fact that most patients declined their cognitive function. The results of this study suggest that the survival of older AP patients is associated with findings related to swallowing, that is, sputum suctioning and cough reflex at rest. These findings can be observed by caregivers and patients’ family members other than medical staff who specialize in dysphagia rehabilitation. Thus, it may be useful to evaluate older AP patients in not only hospitals but also nursing homes and their own homes.
Steele et al. [25] reported a strong correspondence between IDDSI-FDS and FOIS score and that FOIS scores of 4 and 5 correspond to an IDDSI-FDS range of 2 to 6. However, deceased patients in the present study showed a median IDDSI-FDS of 1, despite a median FOIS of 4, and many patients required further adjustment of posture and meal assistance. Therefore, the oral intake level did not match the actual swallowing function. Habitual intake of food that exceeds the capacity may worsen AP. Most patients in the survivors were also found to require a thickener after swallowing function evaluation. These results suggest that older adults may not have the opportunity to undergo evaluations of swallowing function and oral status unless they get AP and further suggest the importance of early assessment for such patients and instructions for appropriate food type and intake conditions at home and in nursing homes.
Hu et al. [37] reported that approximately half of the patients who died from aspiration exhibited depressed consciousness. Nishino et al. [38] reported that increasing depth of anesthesia with nitrous oxide caused progressive reduction in the number of swallows induced by superior laryngeal nerve stimulation. Teramoto et al. [39] reported that all mice anesthetized with pentobarbital exhibited nasopharyngeal contents aspiration, while unanesthetized mice did not show abnormal swallowing. These results suggest that depressed consciousness aggravates dysphagia. Therefore, the lower swallowing function in the deceased in this study may partly result from the depressed level of consciousness.
Ryu et al. [9] reported that serum total protein level, serum albumin level, and CRP level were prognostic factors for mortality in AP patients. However, there were no differences in these values between the two groups in the present study. The mean age of the patients in the former was 74.4 ± 12.4 years, while the patients in the present study had a mean age of 89.4 ± 5.0 years. This difference in patient age between the studies may have affected the results.
There are some limitations of the present study. First, the sample size was small. A study with a larger sample size to further verify the results will increase the reliability of the conclusions. Second, only number of teeth and occlusal support were analyzed for evaluation of the oral status. A future study is required to investigate the relationships between survival and other oral statuses such as oral hygiene, tongue/orofacial movement, and masticatory function. Third, the glottal closure reflex, an indicator for pharyngeal and laryngeal sensory function, was not evaluated in the FEES to prevent complications such as vasovagal syncope and laryngospasm [23]. A further study employing the cough test with citric acid, as a less invasive method for predicting sensory function [40], is recommended to explore the relationship between survival and risk of silent aspiration.
Conclusion
We investigated the relationships between survival and oral status, swallowing function, and oral intake level in older patients hospitalized for AP. These factors were related to the survival outcomes in these patients.
References
Ministry of Health, Labor and Welfare. Demographic statistics. https://www.mhlw.go.jp/toukei/list/81-1a.html
Teramoto S, Fukuchi Y, Sasaki H, Sato K, Sekizawa K, Matsuse T. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 2008;56:577–9.
Taylor JK, Fleming GB, Singanayagam A, Hill AT, Chalmers JD. Risk factors for aspiration in community-acquired pneumonia: analysis of a hospitalized UK cohort. Am J Med. 2013;126:995–1001.
Takemura K, Yoshimuta Y, Ono T, Kokubo Y, Kida M, Kosaka T, Yasui S, Nokubi T, Maeda Y. The relationship between masticatory ability and food feeding behaviors: the Suita Study. J Jpn Soc Mastication Sci Health Promot. 2013;23:81–9.
Yamamoto H, Furuya J, Tamada Y, Kondo H. Impacts of wearing complete dentures on bolus transport during feeding in elderly edentulous. J Oral Rehabil. 2013;40:923–31.
Yoshida M, Masuda S, Amano J, Akagawa Y. Immediate effect of denture wearing on swallowing in rehabilitation hospital inpatients. J Am Geriatr Soc. 2013;61:655–7.
Ramos A, Asensio A, Caballos D, Mariño MJ. Prognostic factors associated with community-acquired aspiration pneumonia. Med Clin. 2002;119:81–4.
Kim H, Jo S, Lee JB, Jin Y, Jeong T, Yoon J, Lee JM, Park B. Diagnostic performance of initial serum albumin level for predicting in-hospital mortality among aspiration pneumonia patients. Am J Emerg Med. 2018;36:5–11.
Ryu S, Oh SK, Cho SU, You Y, Park JS, Min JH, Jeong W, Cho YC, Ahn HJ, Kang C. Utility of the blood urea nitrogen to serum albumin ratio as a prognostic factor of mortality in aspiration pneumonia patients. Am J Emerg Med 2020.
Nakashima T, Maeda K, Tahira K, Taniguchi K, Mori K, Kiyomiya H, Akagi J. Silent aspiration predicts mortality in older adults with aspiration pneumonia admitted to acute hospitals. Geriatr Gerontol Int. 2018;18:828–32.
Naruishi K, Nishikawa Y. Swallowing impairment is a significant factor for predicting life prognosis of elderly at the end of life. Aging Clin Exp Res. 2018;30:77–80.
Suzuki R, Kikutani T, Yoshida M, Yamashita Y, Hirayama Y. Prognosis-related factors concerning oral and general conditions for homebound older adults in Japan. Geriatr Gerontol Int. 2015;15:1001–6.
Papadopoulos D, Bader I, Gkioxari E, Petta V, Tsaras T, Galanopoulou N, Archontouli MA, Diamantea F, Kastanakis E, Karagianidis N, Filaditaki V. Microbiology and prognosis assessment of hospitalized patients with aspiration pneumonia: a single-center prospective cohort study. Infez Med. 2018;26:103–14.
Kohno S, Imamura Y, Shindo Y, Seki M, Ishida T, Teramoto S, Kadota J, Tomono K, Watanabe A. Clinical practice guidelines for nursing- and healthcare-associated pneumonia (NHCAP) [complete translation]. Respir Investig. 2013;51:103–26.
Eichner K. Renewed examination of the group classification of partially edentulous arches by Eichner and application advices for studies on morbidity statistics. Stomatologie der DDR. 1990;40:321–5.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, Leonard RJ. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919–24.
Oguchi K, Saitoh E, Mizuno M, Baba M, Okui M, Suzuki M. The repetitive saliva swallowing test (RSST) as a screening test of functional dysphagia (1) normal values of RSST. Jpn J Rehabil Med. 2000;37:375–82.
Oguchi K, Saitoh E, Baba M, Kusudo S, Tanaka T, Onogi K. The repetitive saliva swallowing test (RSST) as a screening test of functional dysphagia (2) validity of RSST. Jpn J Rehabil Med. 2000;37:383–8.
Wakabayashi H, Kayashita J. Translation, reliability, and validity of the Japanese version of the 10-item Eating Assessment Tool (EAT-10) for the screening of dysphagia. J Jpn Soc Parenter Enter Nutr. 2014;29:871–6.
Hyodo M, Nishikubo K, Hirose K. New scoring proposed for endoscopic swallowing evaluation and clinical significance. Nihon Jibiinkoka Gakkai kaiho. 2010;113:670–8.
2013 TddcotJSoDR: The Japanese Dysphagia Diet 2013. Jpn J Dysphagia Rehabil 17: 255–267, 2013.
Takata N, Yamagata Y, Kayashita J. A comparison of viscosity classifications between the Japanese Dysphagia diet 2013 criteria and the international dysphagia diet standardisation initiative. 2017.
Langmore S, Pelletier C, Nelson R. Results of FEES survey on safety of endoscopy for swallowing assessment. Presented at Fourth Annual Meeting of the Dysphagia Research Society, McLean, VA, October 28, 1995.
Crary MA, Mann GDC, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Steele CM, Namasivayam-MacDonald AM, Guida BT, Cichero JA, Duivestein J, Hanson B, Lam P, Riquelme LF. Creation and initial validation of the international dysphagia diet standardisation initiative functional diet scale. Arch Phys Med Rehabil. 2018;99:934–44.
Ohta T, Waga S, Handa W, Saito I, Takeuchi K. New grading of level of disordered consiousness (author’s transl). No shinkei geka Neurol Surg. 1974;2:623–7.
Mortensen EM, Coley CM, Singer DE, Marrie TJ, Obrosky DS, Kapoor WN, Fine MJ. Causes of death for patients with community-acquired pneumonia: Results from the pneumonia patient outcomes research team cohort study. Arch Int Med. 2002;162:1059–64.
Maeda K, Akagi J. Muscle Mass Loss Is a Potential Predictor of 90-Day Mortality in Older Adults with Aspiration Pneumonia. J Am Geriatr Soc. 2017;65:e18–22.
Avivi-Arber L, Sessle BJ. Jaw sensorimotor control in healthy adults and effects of ageing. J Oral Rehabil. 2018;45:50–80.
Cera ML, Ortiz KZ, Bertolucci PH, Minett TS. Speech and orofacial apraxias in Alzheimer’s disease. Int Psychogeriatr. 2013;25:1679–85.
Taji T, Yoshida M, Hiasa K, Abe Y, Tsuga K, Akagawa Y. Influence of mental status on removable prosthesis compliance in institutionalized elderly persons. Int J Prosthodont. 2005;18:146–9.
Chiba Y, Sano D, Ikui Y, Nishimura G, Yabuki K, Arai Y, Tanabe T, Ikemiyagi H, Hyakusoku H, Oridate N. Predictive value of the Hyodo score in endoscopic evaluation of aspiration during swallowing. Auris Nasus Larynx. 2018;45:1214–20.
Clavé P, de Kraa M, Arreola V, Girvent M, Farré R, Palomera E, Serra-Prat M. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24:1385–94.
Onodera S, Furuya J, Yamamoto H, Tamada Y, Kondo H. Effects of wearing and removing dentures on oropharyngeal motility during swallowing. J Oral Rehabil. 2016;43:847–54.
Yoshikawa M, Yoshida M, Nagasaki T, Tanimoto K, Tsuga K, Akagawa Y. Influence of aging and denture use on liquid swallowing in healthy dentulous and edentulous older people. J Am Geriatr Soc. 2006;54:444–9.
Rofes L, Arreola V, Mukherjee R, Clavé P. Sensitivity and specificity of the eating assessment tool and the volume-viscosity swallow test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil. 2014;26:1256–65.
Hu X, Yi ES, Ryu JH. Aspiration-related deaths in 57 consecutive patients: autopsy study. PLoS ONE. 2014;9:e103795.
Nishino T, Honda Y, Kohchi T, Shirahata M, Yonezawa T. Effects of increasing depth of anaesthesia on phrenic nerve and hypoglossal nerve activity during the swallowing reflex in cats. Br J Anaesth. 1985;57:208–13.
Teramoto S, Matsuse T, Oka T, Ito H, Fukuchi Y, Ouchi Y. Investigation of effects of anesthesia and age on aspiration in mice through LacZ gene transfer by recombinant E1-deleted adenovirus vectors. Am J Respir Crit Care Med. 1998;158:1914–9.
Sato M, Tohara H, Iida T, Wada S, Inoue M, Ueda K. Simplified cough test for screening silent aspiration. Arch Phys Med Rehabil. 2012;93:1982–6.
Acknowledgements
The authors thank Alison Sherwin, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, T., Tsujimura, T., Magara, J. et al. Relationships Between Survival and Oral Status, Swallowing Function, and Oral Intake Level in Older Patients with Aspiration Pneumonia. Dysphagia 37, 558–566 (2022). https://doi.org/10.1007/s00455-021-10306-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10306-3