Abstract
Many adults in residential aged care homes (RACHs) live with oropharyngeal dysphagia (OD) and its physiological, psychosocial, and economic sequalae. Timely, evidence-based assessment of OD can help healthcare teams to create OD management plans that optimize consumer health and minimize healthcare costs. Instrumental swallowing assessment (ISA), specifically flexible endoscopic evaluation of swallowing (FEES) and videofluoroscopic swallowing studies (VFSS), is generally accepted to be an important component of dysphagia assessment and management in older adults. However, its role in RACHs has not been empirically examined. This study aimed to explore the role and use of ISA in adults in RACHs from the perspective of speech–language-pathologists (SLPs) experienced in a RACH setting and/or FEES and VFSS. A three-round electronic Delphi study was conducted to guide 58 SLPs in Australia towards consensus using a combination of multiple-choice questions, statements with five-point Likert scale agreement options, and open-ended questions. Participants’ responses were analyzed using descriptive statistics and content analysis after each survey round. Feedback about group responses was provided before subsequent surveys. Consensus was defined as 70% or greater agreement. Participants reached consensus about obstacles and facilitators to the use of ISA in RACHs. Participants agreed that FEES was a valuable tool in RACHs and that a mobile service model may have advantages over standard off-site assessment. SLPs believed that appropriate governance processes, infrastructure and education were necessary to develop a safe, high-quality service. These views support equitable access to ISA across settings, aligning with person-centered care, re-ablement, and care-in-place.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many adults in residential aged care homes (RACHs) live with oropharyngeal dysphagia (OD) and its physiological, psychosocial, and economic sequalae. OD in this setting has been described as a geriatric syndrome, affecting 40–68% of adults [1,2,3,4,5]. Timely, evidence-based assessment and management of OD aims to minimize negative health outcomes (e.g., choking episodes, aspiration pneumonia, hospital admissions and readmissions,) and health expenditure by the individual, their families and society [6]. Instrumental swallowing assessment (ISA), specifically Flexible Endoscopic Evaluation of Swallowing (FEES) and videofluoroscopic swallowing studies (VFSS), is generally accepted to be an important component of dysphagia assessment and management in older adults with a variety of medical comorbidities in hospital and community settings [7]. While FEES is also part of swallowing care in adults living in RACHs, its use in this setting has only recently been systematically reviewed [8] and has not been empirically examined [8].
In Australia, adults living in RACHs must travel off-site to an outpatient clinic to access ISA. Assessment is subject to the RACHs arranging return transportation and an accompanying RACH staff member to travel with the adult (if necessary); the adult’s cognitive capacity to follow instructions in an unfamiliar environment during the allocated appointment time; and affordable funding arrangements. These prerequisites may present barriers to accessing timely off-site swallowing care, particularly for adults with dementia, who become increasingly confused in new settings, and for adults whose chronic pain may be exacerbated with travel.
Residential aged care homes are increasingly challenged to offer onsite, person-centered swallowing care to a varied population of adults [9]. These adults may experience chronic or acute OD in the context of healthy ageing, disease processes and/or end of life care. Timeliness of ISA is of particular importance for adults receiving or nearing end of life care as dysphagia teams work to optimize swallowing related quality of life and comfort at each stage of clinical deterioration. Mobile FEES (mFEES) services have been implemented internationally in RACHs in the United States and Japan [9,10,11,12,13,14,15] to address the obstacles of off-site travel and to support timely, onsite, integrated swallowing care. However, empirical information is scant on the role of and use of mFEES services in residential aged care [8, 10, 15].
Most healthcare provided to adults in Australia compares positively with international standards [16]. However, there are gaps in how services are tailored to the specific needs of each consumer [17, 18] (e.g., adults in RACHs must travel off-site for ISA). These gaps may contribute to preventable adverse events (e.g., choking is the second most common cause of preventable deaths in adults in Australian RACHs [19]), unfavorable experiences (e.g., unnecessary diet modification), and lowered quality of life (QoL) [20]. Recommendations released by The Royal Commission into Aged Care Quality and Safety in 2020, encourage innovative models of healthcare care that prioritize re-ablement, (i.e., functional independence), integrated care (i.e., multidisciplinary, coordinated care tailored to the adult’s needs) and care-in-place (i.e., catering to an individual’s increasing healthcare needs onsite in a RACH) [21].
In this context, the aim of this study was to investigate Speech–Language-Pathologists’ perspectives on the role of and use of ISA in RACHs, including the potential benefits and risks, and barriers and facilitators to providing ISA to RACH residents. In light of recent research highlighting the increased use of FEES in residential aged care settings and potential for mFEES innovation to offer integrated care over and above standard off-site assessment, this study focused on the use of FEES and mFEES in RACHs.
Specifically, this research sought to answer the following questions:
1. What is the role of and use of (i) ISA, (ii) FEES and (iii) mFEES in residential aged care?
2. What are the potential benefits, risks, barriers, and facilitators to providing (i) ISA, (ii) FEES and (iii) mFEES to RACH residents?
Materials and Methods
Study Design
A three-round electronic modified Delphi consensus study was conducted in accordance with the principles of Delphi methodology utilized in recent healthcare research [22,23,24]. The Delphi technique and its variant, the modified Delphi survey, are used to explore opinions about an issue through successive questionnaires [25, 26]. These questionnaires guide experts in the field towards a consensus [25, 26]. Distinguishing characteristics of the modified Delphi survey include: the use of questions informed by previous investigations; electronic and anonymous distribution of questions; and provision of controlled feedback electronically after every round of surveys [23].
Sample
Purposive quota sampling [25, 26] was used to recruit an expert panel of participants who were Australian speech–language-pathologists (SLPs) with a minimum of 2 years professional experience working with adults in the evaluation and management of swallowing difficulties and either (i) experience providing services to adults in RACHs and/or (ii) training and experience in all aspects of VFSS and FEES. These inclusion criteria captured SLPs with an understanding of the unique environment and issues associated with residential aged care settings, as well as the advantages, challenges, and limitations of ISA.
An electronic advertisement for the study with links to the plain language statement, consent form and the first survey was distributed nationally. The advertisement was posted on social media platforms; published in an electronic Speech Pathology Australia (SPA) newsletter; and emailed to coordinators of speech–language-pathology swallowing interest groups. It was also emailed to speech–language-pathology department heads in public and private healthcare networks, universities and RACHs around Australia.
There are no universally accepted criteria for the number of participants recruited into a Delphi study [22]. Fifty patients were recruited into the study to provide adequate coverage of the small proportion of Australian SLPs working with older adults in residential aged care settings [27] and the even smaller proportion of Australian SLPs who are trained in all aspects of FEES.
Survey Design
This study included three iterative survey rounds. Demographic information was collected during survey one and additional information about the specific area of professional expertise of each participant was collected during survey two. Each survey was organized into three sections exploring swallowing care in adults in RACHs: (1) ISA, (2) FEES and (3) mFEES. All surveys contained relational logic, enabling clarifying questions to appear contingent on participant responses. Questions were a combination of statements with five-point Likert scale response options (ranging from 1 “strongly disagree” to 5 “strongly agree”) for participants to indicate their level of agreement (e.g., ‘Adults living in residential care facilities should have access to timely instrumental swallowing assessment’); closed-ended questions with multiple-choice response options (e.g., ‘Which instrumental swallowing assessment(s) have you seen evidence of being used by SLP in the evaluation and management of swallowing in adults living in RACHs?’); and open-ended questions (e.g., ‘Please state the reason why your concern(s) about mFEES being provided to adults in RACHs cannot be addressed through appropriate funding, infrastructure, processes and/ or education’).
The development of the first survey was informed by our recent scoping review focusing on ISA in adults in RACHs [8, 10] (see Appendix A for survey one). It contained between 24 and 36 items, with relational logic opening up additional questions contingent on participants’ responses. Prior to administration, the survey was piloted and refined based on feedback from five experienced SLPs with expertise in survey development, dysphagia and ISA. These SLPs did not participate in the survey.
The second (between 24 and 29 items) and third (between 34 and 37 items) surveys were formulated to explore areas where consensus was not reached in surveys one and two, respectively (see Appendix B for survey two and Appendix C for survey three). The total number of questions and the number of questions relating to ISA, FEES and mFEES varied between survey rounds because statements from previous surveys were repeated or revised based on participant responses within each survey round. Repeated and revised questions helped to clarify group opinions, giving participants the opportunity to reconsider their viewpoints. Open-ended questions enabled participants to provide a rationale for their opinions and to raise any new issues. Feedback summarizing group responses was emailed to all participants between surveys, emphasizing questions for which agreement was not reached. The aim of this process was for all participants to consider the range of responses and if possible, to reach agreement in their opinions.
Procedures
Ethical approval was granted by The University of Melbourne Human Research and Ethics Committee (#1853221, 13/03/2019–31/12/2019). Consent was provided electronically by study participants after reading an online plain language statement. Data were collected and managed using REDCap electronic data capture tools hosted at The University of Melbourne [28, 29]. The first survey was available between 05/06/2019 and 16/07/2019. Links to the remaining two surveys were active during 14/08/2019–11/09/2019 and 17/11/2019–15/12/2019, respectively. They were emailed directly to study participants who completed every question of the first survey and provided a valid email address for future correspondence (Table 1).
Data Analysis
Quantitative data were analyzed in Minitab® 18 (2017). Demographic characteristics were summarized using descriptive statistics.
To analyse consensus, responses to Likert Scale questions were aggregated into three groups: (1) undecided (2) agree (cumulative score of strongly agree and agree) and (3) disagree (cumulative score of strongly disagree and disagree). Agreement was defined as 70% or above consensus about an issue in response to Likert Scale and multiple-choice questions. The criterion of 70% or above was chosen because it has been utilized in multiple Delphi studies within the field of healthcare research and it was considered to provide a clinically meaningful and reproduceable indication of consensus among healthcare professionals [22, 30,31,32,33]. Data were not divided into demographic groups (i.e., geographical practice classification, years of experience and area of professional expertise) for analysis because the purpose of the Delphi study was to identify areas of consensus rather than discrepancy in consensus between groups of participants. Percent agreement and counts are reported for these data.
Qualitative data from the open-ended questions were analyzed using the principles of thematic analysis described by Braun and Clarke [34]. Two authors (i.e., OB and MB) individually reviewed each response, extracted response patterns (codes) and grouped these into themes. Collaboratively, both authors reviewed all themes to reach agreement about theme definitions and response classification.
Results
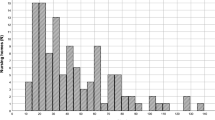
A total of 143 SLPs opened the first survey link. Of these 143 SLPs, 64 (44.8%) completed questions relating to eligibility and fulfilled the eligibility criteria. 58 SLPs (90.6%, n = 58, N = 64) provided informed consent to participate in the study (Fig. 1). Demographic information about six SLPs who did not consent to participate in the study could not be collected. Forty-five participants completed survey two (77.6%, n = 45, N = 58) and 44 completed survey three (75.9%, n = 44, N = 58).
There were participants from all states/territories and geographical remoteness classifications (i.e., city, regional and remote) [35]. 74% of participants had greater than 10 years professional experience in the field of dysphagia. Forty-five and forty-four participants completed surveys two and three, respectively. Approximately half of the participants who progressed to surveys two and three had experience working in RACHs, half were experienced across all aspects of VFSS and FEES, and 22.2% were experienced in both fields (Table 2).
SLPs Value ISA for Adults in Residential Aged Care Homes
Desired Service
Participants agreed that ISA (89.7%, n = 52, N = 58) should play a role in swallowing evaluation and management in adults living in RACHs. Participants also agreed that integrating ISA findings with Supplementary Data (such as progress notes and consumer reports) supports informed clinical care. Respondents identified potential medical, fiscal, and psychosocial benefits of ISA. Timeliness (84.5%, n = 49, N = 58) and the ability to elicit as closely as possible usual swallowing function (88%, n = 51, N = 58) were considered to be important characteristics of the desired ISA service. Timely ISA was described to occur between 4 and 14 days from referral (84.5%, n = 37, N = 44). Participants did not reach agreement on a more refined time frame. Participants who advocated for a 3-day referral response rate (15.6%, n = 7, N = 44) emphasized the need to offer equitable care to adults irrespective of their care setting; and the role of ISA in minimizing harm, improving patient outcomes and assisting differential dysphagia diagnosis. Participants (84.5%, n = 37, N = 44) who believed that longer waiting periods were acceptable (4–14 days) discussed obstacles to timely ISA, proposing that adults in RACHs with acute or severe dysphagia be transferred to an acute care setting for evaluation and management.
Current Service
Participants agreed that ISA is currently underutilized in the residential aged care setting (74.2%, n = 43, N = 58). FEES (95.3%, n = 41, N = 43) and VFSS (97.7%, n = 42, N = 43) were identified as the most underutilized tools, despite VFSS being reported as the most commonly used ISA (86.2%, n = 50, N = 58) (Table 3). Only 32.8% (n = 19, N = 58) of participants reported seeing evidence of FEES being used in adults living in RACHs.
Participants reported that a number of barriers prevented adults in RACHs from accessing timely (94.8%, n = 55, N = 58) and representative ISA (89.6%, n = 52, N = 58). Common barriers related to the absence of onsite ISA services. Specifically, transportation costs (74.5%, n = 41, N = 55), the burden of traveling and/or availability of adequately trained support staff to travel with consumers to ISA (94.5%, n = 52, N = 55) (Table 3). Participants also discussed the impact of staff and consumer knowledge about ISA (86.7%, n = 39, N = 45); fiscal management (75.6%, n = 34, N = 45); and the availability of ISA services (71.1%, n = 32, N = 45) in limiting timely ISA. The adults’ health status also influenced their ability to access ISA. Adults receiving end-stage palliative care or presenting with severe cognitive challenges (e.g., agitation) that increased risks of FEES associated complications, were not offered ISA (73.3%, n = 33, N = 45). Participants agreed that governance (77.3%, n = 34, N = 44) was another potential barrier to timely ISA. Clinical governance is a framework of systems to ensure that consumers are provided with person-centered, reliable, safe and high-quality healthcare [18]. Within the survey, questions relating to governance were organized under the following themes: leadership and culture within the RACHs, consumer partnerships with the RACHs, organizational systems within RACHs that support SLPs in providing and improving swallowing care, quality and safety monitoring of dysphagia services by speech–language-pathology care providers, workforce effectiveness (i.e., including RACH staff and visiting speech–language-pathology service providers), communication and relationships within RACHs and between RACH staff and visiting SLPs. Participants could not agree on which of these areas of governance were barriers to ISA (see Appendix D for survey items where agreement was not reached by study participants). Notably, 10.5% (n = 4, N = 38) of participants agreed that RACHs monitor the quality of dysphagia care services received by their consumers. Through qualitative feedback, participants elaborated on the influence of governance and culture. Participants described three influences that compromised swallowing care: (1) inconsistent points of contact at the RACHs for speech–language-pathology service providers to discuss patient care; (2) ineffective processes utilized by RACHs, ISA service providers and visiting SLPs (e.g., RACH staff making slow referrals, FEES providers failing to prioritize adults from residential aged care settings in allocating appointments); and (3) culture within RACHs (e.g., “concerned with meeting minimal standards rather than quality of care”, “SLPs feel time pressured because they are external contractors”). Participants reported that support for timely ISA varied within and between RACHs.
Participants suggested that as a consequence of delayed ISA, adults were at risk of overly conservative dysphagia management (91.1%, n = 41, N = 45). While participants did not agree that delayed ISA could increase dysphagia management risks, they acknowledged that ISA could reduce preventable emergency department presentations (79.3%, n = 46, N = 58) and minimize dysphagia associated complications (79.4%, n = 46, N = 58).
Participants commented on the differential impact of instrumentation and contrived swallowing conditions when considering the need to elicit usual swallowing patterns. Hurdles to ISA that elicited the resident’s usual swallowing function, were predominantly related to the environment in which ISA was conducted (92.3%, n = 48, N = 52) and to the absence of regular mealtime assistants (73.9%, n = 28, N = 38). Approximately half of participants agreed that food and fluids trialed during the ISA failed to represent the type, quantity, and manner of usual meals at the RACH. Participants also commented that positioning for ISA and difficulty capturing the impact of fatigue during a limited assessment could undermine usual swallowing function.
FEES for Adults in Residential Aged Care Homes
A gap was evident between participant views on the benefits of providing FEES to adults in RACHs and current practice patterns. Participants agreed that FEES could play a valuable role in educating consumers, families and RACH staff who are involved in providing swallowing care (81.1%, n = 47, N = 58). However, respondents felt that challenges in accessing FEES in this setting, resulted in SLPs being reluctant to refer adults for assessment (72.4%, n = 42, N = 58).
Throughout surveys one and two consensus was not reached in considering if SLPs managing adults with dysphagia in residential aged care settings possessed an appropriate level of understanding of FEES referral criteria and limitations. In survey three, participants were asked to consider strategies to improve the quality of dysphagia care. Participants suggested that SLPs involved in managing adults with dysphagia in RACHs should: (1) have stronger partnerships with FEES service providers (89.5%, n = 34, N = 38); and (2) receive further education and training in FEES referral criteria (94.7%, n = 36, N = 38), FEES benefits and limitations (100%, n = 38, N = 38). Participants commented on the need for increased understanding, training, and support in FEES broadly within the speech–language-pathology profession. Further, participants suggested that FEES accessibility is symbiotic with FEES knowledge and training.
While the impact of geographical location was not explored as part of this study, participants made qualitative comments about the remoteness of RACHs. Participants stated that RACHs in regional and remote areas may be particularly disadvantaged in offering ISA, including FEES, through a lack of resources, effective processes and a culture that is resistant to change.
Mobile FEES for Adults in Residential Aged Care Homes
Responding to questions about mFEES specifically, participants reported that mFEES could be provided safely in RACHs if appropriate governance processes and infrastructure, including the physical environment, equipment, information technology, systems and processes [36] were established (77.6%, n = 45, N = 48). Participants reported that there were advantages to offering FEES to adults in RACHs using a mobile, onsite service model (86.3%, n = 50, N = 58). These advantages related to improving the adult’s assessment experience by eliminating the need for travel (100%, n = 50, N = 50), and providing increasingly timely assessment (82%, n = 41, N = 50) in a familiar environment (94%, n = 47, N = 50). Participants reached consensus that mFEES may lead to more effective and efficient dysphagia therapy programs (77.6%, n = 45, N = 58). Participants also agreed that mFEES could play a role in advanced care planning, helping teams to reach more informed quality of life and medical care decisions about swallowing management (81.1%, n = 47, N = 58%). In considering the broad impact of mFEES, participants agreed that it may increase FEES education opportunities for consumers and staff (92%, n = 46, N = 50). Participants also commented that mFEES service delivery could improve the quality of swallowing care in RACHs. Participants highlighted the importance of integrating mFEES into a multidisciplinary care model that capitalizes on the medical expertise of ENT surgeons, neurologists, and general practitioners in delivering quality dysphagia care.
While the vast majority of participants encouraged research into mFEES in RACHs (93.1%, n = 54, N = 58), some participants raised concerns about mFEES in this setting (57.9%, n = 22, N = 38). Of participants with concerns, only four believed that their concerns could not be addressed through appropriate funding, infrastructure, processes and/or education. In a separate question, participants were asked to respond to specific areas of concerns about mFEES. Of those who responded, 71.1% (n = 27, N = 38) worried about the resources (i.e., equipment and cost) and 76.3% (n = 29, N = 38) about the quality of care, including consumers’ access to integrated multidisciplinary team support. Additional areas of concern for which there was no agreement included regard for consumers’ wishes, participation of adults with dementia; the impact of mFEES on consumers’ swallowing related outcomes and QoL; mFEES providers’ skills; models and processes of mFEES service provision, including emergency management protocols. These concerns were about consumer directed care and beneficence; ensuring safety of consumers and staff; developing supportive infrastructure and governance. Broadly reflecting on mFEES in residential aged care settings, some participants suggested complementary areas of future research, including exploration of mobile VFSS.
Discussion
In this modified Delphi study, we uniquely explored agreement among SLPs about the role and use of ISA in adults in RACHs. To the authors’ knowledge, this is the first study to examine and obtain expert consensus on offering onsite ISA, specifically mFEES, in a residential aged care setting (Fig. 2). The findings have implications for the development and implementation of innovative, person-centered approaches to swallowing care. They should be considered in developing services that prioritize re-ablement, care-in-place and equitable healthcare access for older people living in RACHs.
Participants agreed that ISA (including VFSS and FEES) in RACHs was valuable. Participants agreed that in Australia there is currently a discrepancy between the swallowing care needs of adults in RACHs and ISA services provided. The expert panel identified barriers to quality care and strategies for improvement. Participants agreed that mFEES was a viable and potentially valuable service model, requiring further research and stronger evidence-base (Table 4).
Knowledge, education, and collaboration emerged as inter-related barriers to current use of ISA in adults in RACHs, but also as opportunities for improving the quality of future swallowing care. These barriers/opportunities were discussed by participants in relation to SLPs, medical professionals, RACH staff and adults with dysphagia. Among the panel there was strong support to increase FEES education for SLPs working in RACHs and to increase collaboration between SLPs making FEES referrals and ISA service providers. Participants believed that an mFEES service delivery model may increase dysphagia learning opportunities for all RACH staff and consumers. In support of this perspective, there is mounting evidence on the positive impact of collaborative learning and multidisciplinary teams on delivering high-quality healthcare [4], including improving patient outcomes, reducing preventable errors, minimizing healthcare costs, and strengthening team relationships [37,38,39,40]. Conversely, teamwork failures (e.g., poor communication) are notable contributors to preventable medical errors [41]. In a residential aged care setting, where multidisciplinary teams may include numerous stakeholders (e.g., general practitioners, nursing staff, consumers, SLPs working at the RACH and an off-site SLP ISA provider, dieticians, dentists, carers, geriatricians, neurologists, ENT surgeons, gastroenterologists, physiotherapists, occupational therapists and family members who assist with meals), achieving integrated dysphagia care may be further challenged by the geographical dispersion of team members. Professionals offering RACH residents care off-site may be disconnected from the culture and practices of a specific RACH. Recommendations for Prevention of Injury-Related Deaths in Residential Aged Care Services [38] encourage RACH providers to develop multidisciplinary dysphagia teams specific to each facility and to investigate collaborative links with their local health services. Bringing ISA services onsite, through mFEES, may also facilitate stakeholder collaboration and context specific care planning cognizant of what is realistically possible at the specific RACH (Table 5).
Multidisciplinary collaboration in healthcare may also assist in the management of clinical risks [41] by reducing risk-averse thinking [42] and helping to prevent iatrogenic complications in older adults [43]. Participants believed that in the absence of timely ISA, adults in RACHs were at risk of overly conservative dysphagia management,. Qualitative comments clarified that speech–language-pathology professionals were “risk-averse”. These findings are supported by literature reports that due to liability concerns, healthcare providers may prioritize recommendations that reduce the likelihood of aspiration of oral intake [44]. This is a concerning bias, prone to unwitting harm [44], in the context of holistic patient care. In a residential aged care setting, over-management with thickened fluids, food texture modification or swallowing strategies may contribute to dehydration, malnutrition, reduced QoL and subtherapeutic drug dosages [45,46,47]. Vulnerable adults may be susceptible to electrolyte imbalances with associated confusion, acute renal impairment, muscle wasting, falls, sepsis and complications of untreated comorbidities, including depression [44]. Over-management risks may be reduced if information from timely ISA is available and professionals from different disciplines collaborate to evaluate the risks and benefits of a clinical decision (e.g., introduction of thickened fluids) from their unique areas of expertise (e.g., respiratory vs nutritional vs psychosocial functioning). In this way dysphagia teams can reach increasingly informed, collaborative decisions that prioritize consumers’ needs.
Participants discussed the ubiquitous impact of governance on many aspects of ISA for adults in RACHs, including how governance affects quality of care and resources. However, there was a wide range of views about the impact of other areas of governance, with many participants feeling undecided. This response pattern suggests a possible lack of knowledge about governance processes underpinning swallowing care in RACHs among SLPs and the need for further research in this field.
Under an established governance framework, the timeliness of ISA for adults living in RACHs should be defined. Timeliness was a contentious topic in this study, with two similarly sized groups of participants supporting a 4–7 days (46.7%) and an 8–14 days (37.8%) referral response rate. There were suggestions that while a shorter response rate is desired by SLPs, current models of care lack the flexibility to offer prompt ISA to adults in RACHs. Many participants who supported a longer waiting period believed that acute and severe cases of dysphagia would be transferred to hospital for evaluation and management. This assumption appears to contradict care-in-place a guiding principle of healthcare in residential aged care [21] that encourages healthcare onsite, in the primary environment rather than in a specialist setting [48]. For example, in Australia an adult who develops a lower respiratory tract infection and is diagnosed with acute, severe dysphagia, may be managed medically through initiatives such as hospital in the home, to avoid a hospital admission, and associated complications [48]. In this context, prompt ISA, including mFEES, may support onsite integrated care.
While participants in this study supported the use of mFEES in adults in RACHs, in survey three 57.9% of participants (n = 22, N = 38) expressed concerns about this model of care. Of participants who expressed concerns, 59.1% (n = 13, N = 22) believed that these concerns could be addressed through appropriate funding, processes, and infrastructure. Mobile FEES is currently not offered in RACHs in Australia. There is a paucity of published literature describing its use internationally and no studies specifically examining the obstacles and governance systems supporting this care model [10]. Thus, it is likely that participants’ judgements were based on experience offering general dysphagia care in RACHs and/or FEES outside of the residential aged care setting. Research in the analogous field of mobile radiography for adults in RACHs suggests that mobile assessment achieved a similar quality of care, reduced hospital transfers, improved psychosocial wellbeing of consumers, improved timely diagnosis and treatment access compared to hospital based instrumental assessment [49]. Authors report that mobile radiography can increase the use of imaging by adults in RACHs to levels that approximate those of adults accessing imaging in acute or outpatient care [49, 50]. In expressing support for mobile imaging services in RACHs, the Australian Medical Association (AMA) identified issues that need to be addressed to ensure that high-quality services are provided to consumers [51]. These considerations paralleled concerns expressed by speech pathologists who participated in this study and related to equipment quality, expertise of staff providing onsite instrumental services, the identification of appropriate cases for assessment, and availability of skilled nursing staff to support mobile instrumental assessment in RACHs [51]. Furthermore, the AMA called for government support to ensure that mobile instrumental assessment is an economically viable service for healthcare providers and consumers [51]. Similarly, another group identified financial, managerial (i.e., governance) and procedural barriers relating to communication between RACHs and hospitals that were overcome to establish successful mobile radiography services [52]. Direct research into the use of mFEES in RACHs is needed to evaluate the outcomes of this model, including obstacles, governance structures and risks associated with mobile assessment.
Strengths and Weaknesses of This Study
High levels of consent and engagement were offered by participants with expertise in residential aged care settings and in ISA. We assume sample representativeness, yet there is no information on the 10% of eligible SLPs (n = 58, N = 64) who did not consent to participate in this study. Furthermore, eligible SLPs who chose to participate in this survey may have been a subset of SLPs with concerns about or an interest in ISA in residential aged care settings. These opinions may have influenced participants’ responses to the survey resulting in over-or under-representation of particular viewpoints. While retention decreased with progressive survey rounds, the lowest response rate was a reasonable 75.9% for survey three. Efforts were made to maximize the external validity of the study by recruiting experts working in public and private networks, across the continuum of healthcare (acute, inpatient rehabilitation and community settings), in all Australian states/territories and geographical classifications (metropolitan, regional, rural, and remote). While this aim was achieved, there were relatively small and unequal numbers of participants within each group, reflecting lower numbers of SLPs practicing in rural and remote settings, and less SLPs with FEES expertise in more remote geographical locations [53]. Hence perspectives unique to each group may not have been adequately represented. Demographic information about the area of professional expertise of each study participant was not collected until survey two. Therefore, full demographic information is not available for survey one participants who did not complete survey two.
Some questions presented to participants during the three survey rounds subsumed more than one concept about ISA. While participants could make qualitative comments to explain their opinions, additional survey rounds may have helped to tease out participant views about individual concepts.
Survey responses may have also been influenced by participants’ response biases, rather than by the content of questions. For example, different self-report styles, including acquiescence, disacquiescence and extreme responding, may have prompted some participants to preference particular response categories.
While it is possible that some survey items could be interpreted as leading questions, most questions were positively worded irrespective of whether they supported or raised concerns about ISA in RACHs (e.g., I have a/some concern(s) about mFEES being provided to adults in RCFs vs. Adults living in RCFs should have access to timely instrumental swallowing assessment).
Future Directions
Further research is required to explore the use of ISA in adults in RACHs internationally, specifically considering service equity and accessibility in different geographical settings, socioeconomic and cultural groups. Consideration should also be given to adults who exercise consumer choice to refuse ISA and adults who are assessed to be inappropriate for or are unable to tolerate specific ISA procedures, including FEES. Ultimately, consumers will benefit if the range of possible ISA techniques available to adults outside of the residential aged care setting, including VFSS, are systematically explored for use in a residential aged care setting.
To deliver evidence-based care, clinical expertise of SLPs explored in the current study, must be integrated with patient values and perspectives of other stakeholders (e.g., geriatricians, GPs, ENT surgeons, RACH clinical care and management staff). To develop a more comprehensive understanding of current practice patterns and issues in delivering ISA in RACHs, direct sampling of medical records in RACHs is necessary. These data may guide the development and assessment of mobile ISA models in residential aged care settings.
Conclusion
This study uniquely examined the role and use of ISA in adults in RACHs in Australia from the perspective of SLPs. Over three survey rounds, experts reached consensus about the value of timely ISA in this setting and disparity between current practice patterns and characteristics of the desired ISA service. There was agreement on some of the obstacles and facilitators to the use of ISA in RACHs. Participants agreed that FEES was a valuable tool in the residential aged care setting and that a mobile service delivery model may have advantages over and above standard off-site assessment. Participants believed that appropriate governance processes (including interdisciplinary collaboration), infrastructure and education were necessary to develop a safe, high-quality service. These views align with geriatric principles of person-centered care, re-ablement, integrated care and care-in-place. They are supported by international studies exploring quality issues in healthcare across settings, studies examining quality improvement in RACHs, and the analogous field of mobile radiography in RACHs. Future research into ISA in RACHs is important to develop a more integrated understanding of current practice patterns and issues from the perspective of other stakeholders, including the consumers.
References
Steele CM, Greenwood C, Ens I, Robertson C, Seidman Carlson R. Mealtime difficulties in a home for the aged: not just dysphagia. Dysphagia. 1997;12(1):43–50.
Li-Chan L, Shiao-Chi W, Shen CH, Tyng-Guy W, Miao-Yen C. Prevalence of impaired swallowing in institutionalized older people in Taiwan. J Am Geriatr Soc. 2002;50:1118–23.
Park YH, Han HR, Oh BM, Lee J, Park JA, Yu SJ, Chang H. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs. 2013;34:212–7.
Nogueira D, Reis E. Swallowing disorders in nursing home residents: how can the problem be explained? Clin Interv Aging. 2013;8:221–7.
Kayser-Jones J, Pengilly K. Dysphagia among nursing home residents. Geriatr Nurs. 1999;20:77–84.
Attrill S, White S, Murray J, Hammond S, Doeltgen S. Impact of oropharyngeal dysphagia on healthcare cost and length of stay in hospital: a systematic review. BMC Health Serv Res. 2018;18:594.
Langmore SE. History of fiberoptic endoscopic evaluation of swallowing for evaluation and management of pharyngeal dysphagia changes over the years. Dysphagia. 2017;32:27–38.
Birchall O, Bennett M, Lawson N, Cotton S, Vogel AP. Fiberoptic endoscopic evaluation of swallowing and videofluoroscopy swallowing assessment of adults in residential care facilities: a scoping review protocol. JBI Evid Synth. 2020;18(3):599–609. https://doi.org/10.11124/JBISRIR-D-19-00015.
Barczi SR, Sullivan PA, Robbins JA. How should dysphagia care of older adults differ? Establishing optimal practice patterns. Semin Speech Lang. 2020;21:0347–64.
Birchall O, Bennett M, Lawson N, Cotton SM, Vogel AP. Instrumental swallowing assessment in adults in residential aged care homes: a scoping review. J Am Med Dir Assoc. 2021;22(2):372-379.e376.
DeFabrizio ME, Rajappa A. Contemporary approaches to dysphagia management. J Nurse Pract. 2010;6:622–30.
Takahashi N, Kikutani T, Tamura F, Groher M, Kuboki T. Videoendoscopic assessment of swallowing function to predict the future incidence of pneumonia of the elderly. J Oral Rehabil. 2012;39:429–37.
Casper ML. Ethically navigating the maze of billing, documentation, and reimbursement for dysphagia services in long-term care. Perspect Swallowing Swallowing Disord (Dysphagia). 2014;23:58–64.
Tejima C, Kikutani T, Takahashi N, Tamura F, Yoshida M. Application of simple swallowing provocation test with fiberoptic endoscopic evaluation of swallowing in a cross-sectional study. BMC Geriatr. 2015;15:48.
Hase T, Miura Y, Nakagami G, Okamoto S, Sanada H, Sugama J. Food bolus-forming ability predicts incidence of aspiration pneumonia in nursing home older adults: a prospective observational study. J Oral Rehabil. 2020;47(1):53–60.
OECD. Health at a Glance 2013: OECD indicators. OECD Publishing; 2013. https://doi.org/10.1787/health_glance-2013-en. Accessed 1 April 2020.
Australian Commission on Safety and Quality in Health Care (ACSQHC) (2015) Vital signs 2015: the state of safety and quality in Australian health care. ACSQHC; 2015.
Australian Commission on Safety and Quality in Healthcare. National Model Clinical Governance Framework. Australian Commission on Safety and Quality in Healthcare; 2019. https://www.safetyandquality.gov.au/topic/national-model-clinical-governance-framework. Accessed 29 May 2020.
Ibrahim J. Nature and extent of external-cause deaths of nursing home residents in Victoria, Australia. J Am Geriatr Soc. 2015;63:954–62.
State of Victoria Department of Health and Human Services. Services SoVDoHaH: supporting the delivery of quality healthcare for aged care residents: residential aged care services, general practitioners and health services. State of Victoria Department of Health and Human Services; 2016. https://www2.health.vic.gov.au/about/publications/policiesandguidelines/supporting-the-delivery-of-quality-healthcare-for-aged-care-residents. Accessed 1 April 2020.
Dyer SM, van den Berg M, Barnett K, Brown A, Johnstone G, Laver K, Lowthian J, Maeder AJ, Meyer C, Moores C, Ogrin R, Parrella A, Ross T, Shulver W, Winsall M, Crotty M. Review of innovative models of aged care for the The Royal Commission into Aged Care Quality and Safety. 2019. https://agedcare.royalcommission.gov.au/publications/Documents/research-paper-3-review-innovative-models-of-aged-care.pdf. Accessed 1 April 2020.
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53:205–12.
Stewart D, Gibson-Smith K, MacLure K, Mair A, Alonso A, Codina C, Cittadini A, Fernandez-Llimos F, Fleming G, Gennimata D, Gillespie U, Harrison C, Junius-Walker U, Kardas P, Kempen T, Kinnear M, Lewek P, Malva J, McIntosh J, Scullin C, Wiese B. A modified Delphi study to determine the level of consensus across the European Union on the structures, processes and desired outcomes of the management of polypharmacy in older people. PLoS ONE. 2017;12(11):e0188348. https://doi.org/10.1371/journal.pone.0188348.
Hollaar V, van der Maarel-Wierink C, van der Putten G-J, van der Sanden W, de Swart B, de Baat C. Defining characteristics and risk indicators for diagnosing nursing home-acquired pneumonia and aspiration pneumonia in nursing home residents, using the electronically-modified Delphi Method. BMC Geriatr. 2016;16:60.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(1008–1015):26.
Williams PL, Web G. The Delphi technique: an adaptive research tool. Br J Occup Ther. 1994;61(4):153–6.
Parliament of Australia (2014) Prevalence of different types of speech, language and communication disorders and speech pathology services in Australia. Chapter 5: The availability and adequacy of speech pathology services in Australia https://www.aph.gov.au/-/media/Committees/Senate/committee/clac_ctte/speech_pathology/report/c05.pdf?la=en&hash=55F948C66C179D97722D839F34D8332B8BA9A6E4. Accessed 1 April 2020.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Gephart SM, Effken JA, McGrath JM, Reed PG. Expert consensus building using e-Delphi for necrotizing enterocolitis risk assessment. J Obstet Gynecol Neonatal Nurs. 2013;42(3):332–47.
Vogel C, Zwolinsky S, Griffiths C, Hobbs M, Henderson E, Wilkins E. A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes. 2019;43(12):2573–86.
Slade SC, Dionne CE, Underwood M, Buchbinder R. Standardised method for reporting exercise programmes: protocol for a modified Delphi study. BMJ Open. 2014;4(12):e006682.
Veugelers R, Gaakeer MI, Patka P, Huijsman R. Improving design choices in Delphi studies in medicine: the case of an exemplary physician multi-round panel study with 100% response. BMC Med Res Methodol. 2020;20(1):156.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Australian Bureau of Statistics. Remoteness structure: the Australian Statistical Geography Standard remoteness structure. Australian Bureau of Statistics; 2017. https://www.abs.gov.au/websitedbs/D3310114.nsf/home/remoteness+structure. Accessed 1 April 2020.
Luxon L. Infrastructure—the key to healthcare improvement. Future Hosp J. 2015;2:4–7.
Ouslander JG, Lamb G, Tappen R, Herndon L, Diaz S, Roos BA, Grabowski DC, Bonner A. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II Collaborative Quality Improvement Project. J Am Geriatr Soc. 2011;59:745–53.
Ibrahim J. Recommendations for prevention of injury-related deaths in residential aged care services. Southbank: Monash University; 2017. https://www.aph.gov.au/DocumentStore.ashx?id=525f03d1-245d-4da2-9482-df2948748824. Accessed 1 March 2020.
Yeon-Hwan P, Hwal Lan B, Hae-Ra H, Hee-Kyung C. Dysphagia screening measures for use in nursing homes: a systematic review. J Korean Acad Nurs. 2015;45:1–13.
Giammarino C. Safety concerns and multidisciplinary management of the dysphagic patient. Phys Med Rehabil Clin N Am. 2012;23:335.
Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, Weaver SJ. Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am Psychol. 2018;73:433–50.
Victoria State Government (2017) An interdisciplinary approach to caring. Victoria State Government; 2017. https://www2.health.vic.gov.au/hospitals-and-health-services/patient-care/older-people/resources/improving-access/ia-interdisciplinary. Accessed 2 Dec 2020.
Permpongkosol S. Iatrogenic disease in the elderly: risk factors, consequences, and prevention. Clin Interv Aging. 2011;6:77–82.
McGinnis CM, Homan K, Solomon M, Taylor J, Staebell K, Erger D, Raut N. Dysphagia: interprofessional management, impact, and patient-centered care. Nutr Clin Pract. 2019;34:80–95.
Cichero JA, Cichero JAY. Thickening agents used for dysphagia management: effect on bioavailability of water, medication and feelings of satiety. Nutr J. 2013;12:54.
Murray J, Miller M, Doeltgen S, Scholten I. Intake of thickened liquids by hospitalized adults with dysphagia after stroke. Int J Speech Lang Pathol. 2014;16:486–94.
Crary MA, Humphrey JL, Carnaby-Mann G, Sambandam R, Miller L, Silliman S. Dysphagia, nutrition, and hydration in ischemic stroke patients at admission and discharge from acute care. Dysphagia. 2013;28:69–76.
Leong LJP, Crawford GB. Residential aged care residents and components of end of life care in an Australian hospital. BMC Palliat Care. 2018;17:84. https://doi.org/10.1186/s12904-018-0337-x.
Kjelle E, Lysdahl KB. Mobile radiography services in nursing homes: a systematic review of residents’ and societal outcomes. BMC Health Serv Res. 2017;17:1–8.
Kjelle E, Lysdahl KB, Olerud HM. Impact of mobile radiography services in nursing homes on the utilisation of diagnostic imaging procedures. BMC Health Serv Res. 2019;19(1):428.
Australian Medical Association. AMA submission to the Medical Services Advisory Committee—new mobile imaging services for residential aged care facilities. Australian Medical Association; 2018. https://ama.com.au/sites/default/files/documents/AMA_submission_to_MSAC_new_mobile_imaging_services_for_residential_aged_care_facilities.pdf. Accessed 2 Dec 2020.
Kjelle E, Lysdahl KB, Olerud HM, Myklebust AM. Managers’ experience of success criteria and barriers to implementing mobile radiography services in nursing homes in Norway: a qualitative study. BMC Health Serv Res. 2018;18(1):301.
The Speech Pathology Association of Australia. Submission to the senate community affairs references committee future of Australia’s aged care sector workforce. The Speech Pathology Association of Australia; 2016. https://www.speechpathologyaustralia.org.au/SPAweb/Resources_for_the_Public/Advocacy/Submissions_prior_2018.aspx. Accessed 31 May 2020.
Funding
This study was conducted as part of a PhD research program. This work was supported by the following sources of funding: OB is receiving the Australian Government Research Training Scholarship funding through the University of Melbourne to participate in this research program; AV holds a Fellowship from the National Health and Medical Research Council, Australia (#1135683); and SC is supported by a National Health and Medical Council Senior Research Fellowship (SRF, # APP1136344).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, survey distribution and data collection were performed by OB, MB and NL. Data analysis was performed by OB and MB. The first draft of the manuscript was written by OB. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article. The authors declare that they have no conflict of interest.
Ethical Approval
Ethical approval was granted by The University of Melbourne Human Research and Ethics Committee (#1853221, 13/03/2019–31/12/2019).
Informed Consent
Consent was provided electronically by study participants after reading an online plain language statement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Birchall, O., Bennett, M., Lawson, N. et al. The Role of Instrumental Swallowing Assessment in Adults in Residential Aged Care Homes: A National Modified Delphi Survey Examining Beliefs and Practices. Dysphagia 37, 510–522 (2022). https://doi.org/10.1007/s00455-021-10296-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-021-10296-2