Abstract
Although children are more radio-sensitive than adults, few studies have evaluated radiation dosage during videofluoroscopic swallowing study (VFSS) in children. The aim of the study was to investigate the radiation dosage using dose-area product (DAP) for VFSS in pediatric cases and to identify factors affecting the radiation dose. Patients aged 0–17 years who had undergone VFSS were included. The following data were collected retrospectively: DAP; fluoroscopic time; number of tried diets; and clinical characteristics including sex, age, etiology of dysphagia, and recommended feeding type. In the videofluoroscopic field, use of collimation and appearance of metal object, such as a lead apron or a wheel chair, was checked. A total of 290 VFSSs were included. The mean DAP was 5.78 ± 4.34 Gy cm2 with a mean screening time of 2.69 ± 1.30 min. The factors associated with the DAP included screening time, appearance of metal objects in the field, and use of collimation. In 98 cases with no metal object in the field and with collimation, the mean DAP was decreased to 2.96 ± 2.53 Gy cm2. This study evaluated the radiation dosage during VFSS in children according to age groups and the influencing factors such as screening time, appearance of metal objects in the field, and use of collimation in VFSS. To reduce radiation risk, it is important to identify and control modifiable factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Videofluoroscopic swallowing study (VFSS) is useful in assessing the type of swallowing problems and can assist in setting treatment goals targeting the underlying pathophysiological mechanism [1]. However, radiation exposure is a disadvantage of VFSS. Several studies have evaluated radiation dose during VFSS in adults and confirmed a safety benefit in radiation exposure risk [2,3,4,5]. According to the mean effective radiation exposure dose reported in a study, performing more than 40 VFSSs per year could be within the annual radiation exposure dose limit [3]. As it is difficult to exceed the annual dose limit, VFSS can be considered relatively safe in terms of its associated radiation exposure risk.
However, few studies have evaluated the radiation dose for VFSS in children [2, 3, 6,7,8]. It is especially important that the dose-area product (DAP) used in imaging studies for children is kept as low as practicable while providing the clinician with diagnostic information [9], because children are 10 times more sensitive than adults to radiation-induced cancer [10].
The interest in use of radiation dose for pediatric cases undergoing VFSS is increasing [11]. The National Radiological Protection Board (NRPB) published the diagnostic reference levels (DRLs) in the UK, including pediatric barium swallow, for the first time in 2002 [9], and they updated it in 2009 [6]. However, very little work has been published on the radiation dose in pediatric cases undergoing VFSS; currently, there is no reference level in many countries.
Moreover, many factors are associated with radiation dose in VFSS [7]. To our best knowledge, there is only 1 study reporting factors which are associated with radiation dose of VFSS in pediatric cases [7]. To reduce radiation dose, it is important to identify its associated factors. It is also important to analyze the radiation dose according to age, since the type and number of diets vary according to age. Therefore, the objectives of this study were to determine the mean DAP and the fluoroscopic time for VFSS in pediatric cases, subsequently, to analyze them based on the patients’ ages, and identify factors affecting radiation dose.
Materials and Method
Participants
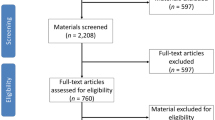
Pediatric patients aged 0–17 years old who had undergone VFSS at Seoul National University Hospital from September 2014 to September 2017 were included. During this period, a total of 508 VFSSs were performed in children. Out of these, 208 examinations were excluded because DAP could not be obtained for them. There were three reasons for loss of the DAP, loss of recorded video files (n = 46), early discontinuation of recording videos (n = 38), and recording by another machine that cannot calculate the DAP (n = 124). Finally, 300 VFSSs from 217 patients were included in the study.
Evaluation
VFSS was performed using a fluoroscopy machine (SONIALVISION G4R®, Shimadzu Corporation, Kyoto, Japan) with DAP meter (VACUDAP®, Shimadzu Corporation, Kyoto, Japan) and recorded using a digital computer frame grabber board (Pegasus HD/SD Board, Grass Valley Inc., Honorine, France) and image processing software (EDIUS 4.5, Grass Valley Inc., Honorine, France). The DAP is one of the most accurate measures of effective dose and is the most practical quantity for monitoring radiation delivered to patients [12]. The DAP and fluoroscopic time for VFSS exam were automatically calculated by the fluoroscopy machine and displayed on the monitor at the end of the study. The image acquisition rate was 30 frames/s.
After turning the fluoroscopy machine 90°, the test was conducted while the subjects sat alone, if possible, on one side of the table. Infants who were unable to cooperate due to their disability or anxiety were tested while being seated on their primary caregivers’ laps and arms. The primary caregivers wore lead aprons. The study was completed in the lateral view in most of the cases.
A test diet was chosen appropriately taking into account the age of the infant and severity of the disease. Children under 1 year of age were tested with bottled milk or weaning food. Under the instruction of a physiatrist, barium mixed fluid (2 ml, 5 ml), yogurt, and boiled rice were fed to children of the ≥ 1-year-old age group in tolerable range. The video was taken individually for each number of diets attempted, and the number of tried diets was confirmed. Two times of bolus presentation and swallowing were tried in each diet. The interpretation of VFSS and diet recommendation required consensus of two physiatrists who had at least 2 years of experience in dysphagia management.
To reduce radiation exposure, a radiologic technician used collimation for some cases of VFSS (Fig. 1). Metal objects such as lead aprons worn by the caregiver of children or wheel chair were shown in the videofluoroscopic (VF) field in some cases. We defined these as ‘contrast amplifiers’, because maximum (100%) contrast is produced when no radiation penetrates objects such as metal. Clinical characteristics including sex, age, etiology of dysphagia, and recommended feeding type were collected retrospectively by a physician.
Images show videofluoroscopic field (VF) with variable cases. a 9-year-old, with unknown origin of dysphagia. b 1 years old, unknown origin of dysphagia with collimation. c 2-year-old, unknown origin of dysphagia with a lead apron. d 2-year-old, epilepsy with a wheel chair and collimation. When metal objects are shown in VF (c, d), fluoroscopy machine generate more X-rays (increasing mA) and/or produce more penetrating X-rays (increasing kVp) to automatically adjust brightness control
Analysis
The patients were divided into 4 age groups: 0–1 year, 2–5 years, 6–9 years, and 10–17 years. The outliers, less than the first quartile or greater than the third quartile by more than 1.5 times the interquartile range, were removed for each age group on the basis of screening time. A total of 10 VFSSs were eliminated (3 in 0–1 year, 5 in 2–5 years, 1 in 6–9 years and 1 in 10–17 years). As a result, 290 VFSSs from 207 patients were included in the study.
Group differences in the screening time, the DAP, and the number of tried diet were analyzed using ANOVA with Bonferroni’s post hoc test. Correlations between the DAP and age, number of tried diet, and screening time were evaluated using Pearson correlation analysis. The stepwise multiple linear regression was performed in order to explore the factors associated with the DAP as a dependent variable. The independent variables were age, screening time, number of tried diet, collimation, contrast amplifier, etiology of dysphagia, and recommended feeding type. In the analyses, collimation and contrast amplifier were used as dichotomized variables (yes and no). In stepwise selection, entry condition of P value < 0.05 and removal condition of P value > 0.10 were applied. The cases which used collimation but not the contrast amplifier in the VF field were selected, and ANOVA was performed to identify group differences in the screening time and the DAP by the age group.
Statistical analysis was performed using SPSS, version 19.0 (IBM Co., Armonk, NY, USA) and SAS statistical software (SAS system for Windows, version 9.3, SAS institute, Cary, NC).
Results
The mean age of the participants was 4.02 ± 4.60 years old with a range of 1 month to 17 years. Of the 290 cases, 161 cases in 138 patients were boys. The collimation was done in 73.9% of the cases. The contrast amplifier was shown in 169 cases (58.3%). The most common etiology of dysphagia was central nervous system disorder (Table 1).
The mean DAP for the entire group was 5.78 ± 4.34 Gy cm2, and the mean screening time was 2.69 ± 1.28 min. The DAP was correlated with the screening time (r = 0.707, P < 0.001), age (r = 0.241, P < 0.001), and number of tried diet (r = 0.313, P < 0.001). There were significant differences in the DAP, screening time, and number of tried diet among the 4 age groups (Table 2). Patients in the 10-17 years-old group had a higher DAP (8.17 ± 5.15 Gy cm2), a longer screening time (3.47 ± 1.45 min), and a larger number of tried diets (4.86 ± 2.43) compared with the age group of 0-1 year-old (5.15 ± 4.36 Gy cm2, P = 0.001; 2.53 ± 1.19 min, P < 0.001;2.21 ± 0.99, P < 0.001), and the age group of 2–5 years-old (5.37 ± 3.89 Gy cm2, P = 0.001;2.50 ± 1.14 min, P < 0.001; 3.32 ± 1.53, P < 0.001), respectively. In addition, the patients of 6–9 years group had a larger number of tried diets (5.00 ± 2.16) compared with that of the age group of 0–1 year-old (2.21 ± 0.99, P < 0.001), and age group of 2–5 years (3.32 ± 1.53, P < 0.001).
In the multiple linear regression analysis, the factors associated with the DAP included screening time (β = 0.035, P < 0.001), contrast amplifier (β = 1.286, P < 0.001), and collimation (β = − 4.128, P < 0.001) (Table 3).
In 98 cases with no contrast amplifier in the VF field and with use of collimation, the mean DAP decreased to 2.96 ± 2.53 Gy cm2. Among these, the DAP values were 1.59 ± 1.23 Gy cm2 (1.85 ± 0.83 min), 2.52 ± 2.07 Gy cm2 (2.13 ± 1.14 min), 3.98 ± 3.03 Gy cm2 (2.36 ± 1.52 min), and 5.22 ± 2.96 Gy cm2(3.39 ± 1.29 min) in the age groups of 0–1 year-old (n = 21), 2–5 years-old (n = 49), 6–9 years-old (n = 10), and the 10–17 years-old (n = 18), respectively. In addition, there were significant intergroup differences in DAP values between the two groups under 5 years old, and the two groups above 5 years old (P < 0.001, except compared age group of 0–1 years to age group of 6–9 years (P = 0.039)). The DAP value of age under 5 was 2.22 ± 1.93 Gy cm2 (2.01 ± 1.03 min).
Discussion
This study presents the mean DAP and the fluoroscopic time during VFSS in pediatric cases and factors associated with the DAP in children. The mean DAP was 5.78 ± 4.34 Gy cm2 with screening time of 2.69 ± 1.28 min, with significant differences between age groups. The age, screening time, contrast amplifier, and collimation were correlated with the DAP. The mean DAP was 2.96 ± 2.53 Gy cm2 in the cases with no contrast amplifier in the VF field and with use of collimation. The DAP values were significantly decreased in the age group of under 5 years as compared to those in the other age groups.
Weir et al. [7] has reported a mean DAP of 0.2879 ± 0.4172 Gy cm2 in children with the mean age of 1.57 years old and the mean screening time of 2.48 ± 0.81 min. Even considering the low age of the study subjects, the DAP was much lower than that reported in other studies. The use of frame rate of 15 frames per second may have been a contributing factor in low mean DAP in the study. Bibbo et al. [13] have also reported a low mean DAP value, 0.451 Gy cm2 in children under 1 year and 1.238 Gy cm2 in children over 10 years, during barium swallow and meal studies with very low frame rate of 0.5 to 8 frames per second. Chau et al. [2] and Kim et al. [3] have reported mean DAP of 2.1 ± 2.3 Gy cm2 with screening time of 4.49 ± 3.14 min, and the mean DAP of 3.71 ± 2.06 Gy cm2 with the screening time of 2.42 ± 1.00 min, respectively, in VFSS in pediatric cases; however, their data were a small part of the DAP investigation in adults, no mean age of children was presented, and the number of pediatric data was 15 and 24, respectively. Based on data from national surveys, the DRLs of the NRPB were 1.2–3.5 Gy cm2 for children of ages between 1 and 15 years old in barium swallow [6]. Since VFSS, also known as modified barium swallow, uses a variety of test diets, the reference level is considered to be much higher than that of barium swallow. Nevertheless, in our study, the mean DAP was relatively high, as compared to that of other studies previously reported in the literature. We might consider two reasons for this. First, the existence of contrast amplifiers and/or omission of collimation in some data. Second, we surveyed a wide age range from 0 to 17 years old.
The use of collimation and some metal objects in the VF field had influence on the radiation dose. With respect to controlling of other factors that affect the DAP, the use of collimation reduced the DAP by 4.128 Gy cm2 compared to the instances without the use of collimation. In addition, contrast amplifiers in the VF field increased the DAP because high-density objects need high-energy (kVP) beam to produce an image with appropriate level of brightness, thereby resulting in an increase in the required radiation dose. For infants who were unable to sit alone, a tumble-form chair made of plastic was used in some hospitals, instead of testing with primary caregivers who wore lead aprons [11]. In addition, there is controversy about the image acquisition rates in VFSS in pediatric cases. Many studies recommend a frame rate of 30 frames/s to identify brief penetration-aspiration events and to increase sensitivity of the examination [14,15,16]; this frame rate was used in our study. However, in some cases with pediatric patients, a frame rate of 15 frames/s is preferred, considering the radiation risk [7, 11]. In addition to appropriate use of collimation and removal of contrast amplifiers in the VF field, lowering of frame rate may also be considered as a measure to reduce radiation dose in pediatric VFSS, if the sensitivity of the study can be maintained at a reasonable level.
The DAP is reportedly strongly correlated with the screening time [7, 17]. Additionally, the number of tried diet was correlated with DAP, age, and screening time in our study, since increased range of tolerable diet with growth resulted in an increased number of tried diet and increase in the DAP. Minimizing the number of tried diet is likely to reduce radiation doses.
Although the effective dose is the most useful descriptor of radiation dose, the DAP was used in this study because it was practical for routine use during VFSS [12]. The DAP is a product of the irradiated surface area multiplied by the radiation dose at the surface; the effective dose is obtained by multiplying the radiation dose delivered to each organ by its weighting factor and then by summation of those values [12]. It can be used to assess the risk of radiation-induced cancers and serious hereditary effects for future generations, regardless of the procedure being performed [12]. It is likely that the DAP is more closely related to effective dose, since it takes into account the X-ray beam area that affects the number of organs irradiated [12]. However, the actual doses achieved will vary greatly depending on the age, sex, body mass, body thickness, and cooperation of the child [9].
Our study has some limitations. First, the present study did not evaluate the effective dose and average X-ray tube voltage (kV). Although the DAP is practical and widely used, it is important to estimate the exact radiation risk. Second, because clinical information was reviewed retrospectively, missing data could not be obtained. For example, we considered height and weight as factors associated with radiation dose, but these were not included in the analysis. Third, efforts to reduce radiation, such as the use of collimation and eliminating radiopaque obstacles, varied according to the VFSS examiners. Based on the results of multiple regression analysis, the mean DAP could have been reduced by the effort of the examiners.
Conclusion
This study evaluated the radiation dosage in VFSS in children according to their age groups. Radiation dose was associated with screening time, metal objects in the field, and use of collimation in VFSS in children. To reduce radiation risk, it is important to identify modifiable factors and control them. In addition, the frame rate of fluoroscopy and the number of tried diet are worth considering as measures to reduce the radiation dose. It would be recommendable to adopt the radiation dose obtained under conditions of adequately controlled modifiable factors as the reference dose in VFSS in pediatric cases, i.e., about 2.96 Gy cm2 in all children, and in particular, about 2.22 Gy cm2 in pediatric patients aged under 5 years, if frame rate of 30 frames per second is used.
References
Fung C-W, Khong P-L, To R, Goh W, Wong V. Video-fluoroscopic study of swallowing in children with neurodevelopmental disorders. Pediatr Int. 2004;46:26–30.
Chau KHT, Kung CMA. Patient dose during videofluoroscopy swallowing studies in a Hong Kong public hospital. Dysphagia. 2009;24:387–90.
Kim HM, Choi KH, Kim TW. Patients’ radiation dose during videofluoroscopic swallowing studies according to underlying characteristics. Dysphagia. 2013;28:153–8.
Bonilha HS, Humphries K, Blair J, Hill EG, McGrattan K, Carnes B, et al. Radiation exposure time during MBSS: influence of swallowing impairment severity, medical diagnosis, clinician experience, and standardized protocol use. Dysphagia. 2013;28:77–85.
Zammit-Maempel I, Chapple C-L, Leslie P. Radiation dose in videofluoroscopic 198 swallow studies. Dysphagia. 2007;22:13–5.
Hart D, Hillier MC, Wall BF. National reference doses for common radiographic, fluoroscopic and dental X ray examinations in the UK. Br J Radiol. 2009;82:1–12.
Weir KA, McMahon SM, Long G, Bunch JA, Pandeya N, Coakley KS, et al. Radiation doses to children during modified barium swallow studies. Pediatr Radiol. 2007;37:283–90.
Wall BF, Kendall GM, Edwards AA, Bouffler S, Muirhead CR, Meara JR. What are the risks from medical X rays and other low dose radiation? Br J Radiol. 2006;79:285–94.
Hiorns MP, Saini A, Marsden PJ. A review of current local dose–area product levels for paediatric fluoroscopy in a tertiary referral centre compared with national standards. Why are they so different? Br J Radiol. 2014;79:940.
Hall EJ. Lessons we have learned from our children: cancer risks from diagnostic radiology. Pediatr Radiol. 2002;32:700–6.
Hiorns MP, Ryan MM. Current practice in paediatric videofluoroscopy. Pediatr Radiol. 2006;36:911–9.
Le Heron JC. Estimation of effective dose to the patient during medical x-ray examinations from measurements of the dose-area product. Phys Med Biol. 1992;37:2117.
Bibbo G, Balman D, Linke R. Diagnostic reference levels for common paediatric fluoroscopic examinations performed at a dedicated paediatric Australian hospital. J Med Imaging Radiat Oncol. 2016;60:469–74.
Peladeau-Pigeon M, Steele CM. Technical aspects of a videofluoroscopic swallowing study. Can J Speech Lang Pathol Audiol. 2013;37:216–26.
Mercado-Deane M-G, Burton EM, Harlow SA, Glover AS, Deane DA, Guill MF, et al. Swallowing dysfunction in infants less than 1 year of age. Pediatr Radiol. 2001;31:423–8.
Cohen MD. Can we use pulsed fluoroscopy to decrease the radiation dose during video fluoroscopic feeding studies in children? Clin Radiol. 2009;64:70–3.
Wright RE, Boyd CS, Workman A. Radiation doses to patients during pharyngeal videofluoroscopy. Dysphagia. 1998;13:113–5.
Acknowledgement
We thank the Medical Research Collaborating Center (MRCC) of Seoul National University Hospital for their assistance with statistical analysis.
Funding
This study was not supported by any Grant or funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are solely responsible for the content and writing of the paper.
Ethical Approval
This study was conducted in conformance with the ethical standards of the Declaration of Helsinki (1964) and was approved by the Institutional Review Board of our institution before study initiation (IRB No. 1605-030-760). The requirement for informed consent was waived because of the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Im, H.W., Kim, S.Y., Oh, BM. et al. Radiation Dose During Videofluoroscopic Swallowing Studies and Associated Factors in Pediatric Patients. Dysphagia 35, 84–89 (2020). https://doi.org/10.1007/s00455-019-10006-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-019-10006-z