Abstract
Older patients with stroke have poor functional prognosis compared to younger patients. Patients with stroke who have severe white matter (WM) lesions have been reported to have swallowing problems. The aim of this study was to determine whether the location of WM lesions affects swallowing function in older patients with mild stroke. We conducted a retrospective analysis of 88 patients aged > 65 years who had a National Institutes of Health Stroke Scale score of ≤ 5 and who underwent videofluoroscopic swallowing examination after their first stroke. Participants were divided into three groups according to the involvement of corticobulbar tract (CBT) as follows: group I, no involvement of CBT; group II, involvement of CBT in one hemisphere; and group III, involvement of CBT in both hemispheres. Linear regression analysis showed that pharyngeal transit time tended to increase according to the involvement of CBT in WM lesion (p = 0.043). In addition, inadequate laryngeal elevation was related to the involvement of CBT (p = 0.016). Early spillage, inadequate laryngeal elevation, and penetration could also be predicted by Fazekas grade. Accordingly, the location of WM lesions can be regarded as a potential predictive factor for dysphagia. Moreover, in patients with WM lesions involving CBT, detailed evaluation of dysphagia is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Older patients with stroke have a poor functional prognosis compared to younger patients [1]. Initial stroke severity is directly associated with functional outcome and is considered to be a strong prognostic factor [2]. However, some elderly patients with stroke have a relatively poor prognosis even though their neurologic sequelae are mild and they do not exhibit any complications. In recent decades, patients with stroke who have severe white matter (WM) lesions have been reported to have a poor functional prognosis [3]. White matter lesions, also known as leukoaraiosis, can be detected as abnormal hypointensities on computed tomography scans and as hyperintensities on T2-weighted or fluid-attenuated inversion recovery magnetic resonance imaging (MRI). A recent LADIS (leukoaraiosis and disability) study with 3-year follow-up results showed that age-related changes in WM independently and strongly predict a rapid global functional decline [4]. A WM lesion appears as a hyperintense lesion in the cerebral WM of T2-weighted MRI. Regions of periventricular hyperintensity in the brain MRI are thought to reflect a decreased amount of nerve fibers. A previous study comparing postmortem brain MRI scans with anatomic findings reported decreased myelin, axons, and oligodendrocytes, but increased microglia in cerebral WM lesions [5]. WM lesions have also been suggested to be a form of end-organ damage [6] caused by a diffuse decrease in cerebral blood flow, suggesting poor cerebral blood flow [7]. Therefore, WM lesions might indicate increased vulnerability to ischemic challenges, such as stroke. In review of cerebral aging, WM lesion as a quantifiable nondisease-related aging of the cerebral WM observed in brain MRI may contribute to a disconnection state. Further, the prefrontal WM was most susceptible to the influence of age, and it may be associated with performance decline in cognitive domains [8].
A few studies have investigated the influence of WM lesions on swallowing dysfunction. One study reported that unidentified bright objects on MRI had a demonstrable effect on the duration of oropharyngeal swallowing in normal individuals [9]. Also, another previous study suggested that WM connections were clinically important as related to dysphagia in acute purely subcortical stroke patients [10]. In a recent study, WM lesions observed in brain magnetic resonance imaging scans can impart swallowing problems in older patients with mild stroke, regardless of initial stroke severity or other factors associated with lesion location, especially causing oral transit time delay or penetration [11].
Swallowing is a complex process of sensation and movement controlled by the brain. This process involves multiple nervous tissues including the cerebral cortex, the subcortical white matter tract, and the infratentorium [12]. The corticobulbar tract (CBT) plays some role in swallowing. The CBT is known to originate from the primary motor cortex and descend through the corona radiata and internal capsule into the cerebral peduncles. The CBT then innervates the motor cranial nerve nuclei in the brain stem to control the muscles of the face, head, and neck [13]. A previous study reported that involvement of the CBT might be a possible cause of dysphagia in normal pressure hydrocephalus [14].
Recently, there is growing evidence suggesting that clinical significance can be indicated by the anatomic location of white matter lesions and whether the functional integrity of specific fiber bundles is affected. WM lesions at the frontal horns, the so-called “capping,” are in close proximity to cholinergic axons that originate in the basal forebrain. Therefore, these lesions may result in more significant cortical deafferentation because of the more proximal axonal disruption [15, 16]. Another study reported strategic subcortical hyperintensities in cholinergic pathways and executive function decline in Alzheimer patients [17]. These findings might suggest that not only the severity of WM lesions but also the location of the WM lesions has clinical significance associated with neurologic deficit. To our knowledge, there are few studies on the involvement of CBT in WM lesions and dysphagia.
We hypothesized that oropharyngeal dysphagia in older stroke patients with only mild neurologic symptoms is associated with the location of preexisting WM lesions and depends heavily on CBT involvement. The aim of the present study was to test the hypothesis that the involvement of CBT in WM lesions negatively impacts swallowing function in older patients with relatively mild stroke.
Materials and Methods
Participants
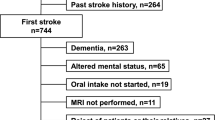
Acute and subacute patients with stroke who underwent VFSS in the Department of Physical Medicine and Rehabilitation between January 2012 and November 2017 were included in this study. VFSS was performed to screen for dysphagia. Diagnosis of stroke was limited to cases in which ischemic cerebral infarction had been verified by magnetic resonance imaging (MRI). We included patients aged ≥ 65 years and who had mild stroke and transient ischemic accident (TIA) (score ≤ 5 on the Korean version of the National Institutes of Health Stroke Scale, K-NIHSS) [18]. The exclusion criteria were as follows: (1) missing medical records or brain MRI scans, (2) difficulty identifying the lesion focus, as in subarachnoid hemorrhage, (3) previous history of stroke, dementia, or other diseases that could cause dysphagia, and (4) duration between stroke onset and VFSS evaluation exceeded 30 days. A total of 88 patients satisfied the criteria and were chosen for analysis; data from these patients were collected retrospectively. The study protocol was approved by the institutional review board of our institution, and the requirement for informed consent was waived due to the retrospective design of the study.
Methods
Review of medical records: The medical records and test results of the patients were reviewed retrospectively. Patient demographic and clinical characteristics were recorded, including age, sex, brain lesion laterality (left or right), duration between onset of stroke and VFSS evaluation (number of days), and initial severity of stroke as assessed by the K-NIHSS.
Videofluoroscopic swallowing study: Physicians of the Department of Rehabilitation Medicine conducted the VFSS by following a modified version of Logemann’s procedure [19]. Briefly, individuals were seated, and fluoroscopy was performed as the patients swallowed barium mixed with juice, yogurt, thick gruel, or rice. For juice and yogurt, two different volumes were used (2 and 5 ml). Each food type was mixed with undiluted liquid barium to ensure proper bolus observation during the fluoroscopy procedure.
Interpretation of VFSS: In the oral phase, functions such as lip sealing, bolus formation, mastication, early spillage, oral remnants, and oral transit time of the bolus were assessed. In the pharyngeal phase, laryngeal elevation and aspiration/penetration of the respiratory tract were assessed. Moreover, the pharyngeal transit time of the bolus and swallowing response time until the swallowing reflex was initiated were both recorded. Each individual finding was assessed based on the presence or absence of an abnormal finding. Oral transit time, swallowing response time, and pharyngeal transit times were recorded in seconds. Oral transit time was the interval between the first frame showing tongue tip elevation and the first frame showing arrival of the head of the bolus at the ramus of the mandible. Swallowing response time was the interval between the arrival of the bolus at the ramus of the mandible and the first frame showing upward excursion of the larynx. The pharyngeal transit time was the interval between the end of the oral transit time and the last frame showing the tail of the bolus passing through the upper esophageal sphincter. When the food entered the respiratory tract, but did not pass into the true vocal fold, it was recorded as penetration, whereas when the food passed into the true vocal fold, it was determined to be aspiration.
WM Lesions
Brain MRI scans were evaluated by a physician who was blinded to the patient’s clinical symptoms. The severity of WM lesions was determined using fluid-attenuated inversion recovery (FLAIR) magnetic resonance images. Acute infarction and WM lesions were differentiated by comparing diffusion-weighted images and FLAIR images. Severity was rated based on the Fazekas scale, which categorizes WM lesions. Periventricular hyperintensity (PVH) was graded as 0 = absence, 1=”caps” or pencil-thin lining, 2 = smooth “halo,” and 3 = irregular periventricular hyperintensity extending into the deep white matter. Separate deep white matter hyperintense signals (DWH) were rated as 0 = absence, 1 = punctate foci, 2 = beginning confluence of foci, and 3 = large confluent areas [20]. Also, the involvement of CBT was determined by two trained researchers depending on the change of signal intensity at the location of CBT, almost halfway between the most anterior and the most posterior points of the lateral ventricle, almost one third between the midline and the most lateral point of the brain, and anterior and medial compared with the corticospinal tract [21]. Participants were divided into three groups according to CBT involvement as follows: group I, no involvement of CBT; group II, involvement of CBT in one hemisphere; and group III, involvement of CBT in both hemispheres (Fig. 1).
Statistical Analysis
Differences between the three groups were evaluated using the Kruskal–Wallis test. Partial correlation analyses with adjustments for age, NIHSS, and Fazekas grade were performed to examine the correlations between involvement of CBT and swallowing parameters in VFSS. To assess whether clinical characteristics of lesion location, laterality, sex, age, severity of stroke, WM lesion severity, and CBT involvement were independent variables in predicting swallowing problems, while controlling for other possible confounding variables, the corresponding rates of findings were calculated. We set each VFSS finding as an independent variable and determined the corresponding rate of each finding. The 95% confidence intervals and equivalent p values were calculated using multivariate linear logistic regression analysis.
The statistical package SPSS (IBM SPSS Statistics for Windows, Version 21.0; IBM, Armonk, NY, USA) was used for all statistical analyses. Statistical significance was defined as p < 0.05.
Results
General Characteristics of the Participants
The demographic and clinical characteristics of the 88 patients are shown in Table 1. Groups according to the location of the WM lesion were as follows: group I (no involvement of CBT) was 45 patients, while group II (involvement of CBT in one hemisphere) and group III (involvement of CBT in both hemispheres) contained 25 and 18 patients, respectively.
Differences Among the Groups According to the Involvement of CBT in WM Lesion
Significant differences were observed in the Fazekas grade (PVH), Fazekas grade (DWH), sum score of Fazekas grade, and the laryngeal elevation abnormality among three groups according to the CBT involvement (Fig. 2).
The relationships between WM lesion’s involvement of CBT and VFSS findings are shown in Table 2. The partial correlation coefficients adjusted for age, initial severity (K-NIHSS), and Fazekas sum score were calculated. Statistically significant correlations were observed between the involvement of CBT and delayed pharyngeal transit time and inadequate laryngeal elevation. In the correlation analysis with combined group II + III, it showed similar results: there were significant correlations between the involvement of CBT and delayed pharyngeal transit time, delayed swallowing response time, and inadequate laryngeal elevation. (detailed data were not described.)
Predictors of Dysphagia
To control for other confounding factors of age, sex, lesion laterality, lesion location, and initial stroke severity, Fazekas grade, multiple logistic regression analyses were conducted to examine the role of WM lesions location in swallowing problems in older patients with mild stroke. Based on the VFSS results, the factors relevant to dysphagia are described in Table 3. Several swallowing parameters were related to the degree of WM lesion severity and involvement of CBT. Early spillage, inadequate laryngeal elevation, and penetration were seen more frequently as Fazekas grade increased (p = 0.043, 0.040, and 0.020, respectively). In the pharyngeal phase of swallowing, multivariate regression analysis revealed that a WM lesion involving CBT was a significant factor associated with inadequate laryngeal elevation and delayed pharyngeal transit time. Therefore, involvement of CBT by a WM lesion was an independent prognostic factor of pharyngeal swallowing problem, regardless of Fazekas grade.
Discussion
The present study demonstrates that some swallowing parameters after stroke in elderly patients with mild neurologic symptoms are influenced by the severity and location of WM lesions. Moreover, these effects are independent of age, sex, initial stroke severity, lesion location, and lesion laterality. The results, using a linear regression model, indicate that the degree of WM lesions is correlated with the early spillage, laryngeal elevation, and penetration. Also, the location of WM lesion (involvement of CBT) has some influence on the laryngeal elevation and pharyngeal transit time.
A number of previous studies reported prognostic factors of dysphagia in stroke patients, and the initial severity of the stroke was a strong predictor [22]. However, among patients with mild stroke, NIHSS score was not associated with any of the swallowing parameters according to linear regression analysis. This finding suggests that the K-NIHSS scoring system might not be useful for predicting swallowing problems in older patients with mild stroke.
Considering all previous reports, WM lesions can lead to functional decline in elderly patients, and it may have some important role for presbyphagia often manifested in old age. In a previous study, severe WM lesion was associated with pseudobulbar signs, [23] and WM lesions observed in brain magnetic resonance imaging scans can indicate swallowing problems in older patients with mild stroke, regardless of initial stroke severity or other factors associated with lesion location, especially causing oral transit time delay or penetration [11]. Also, a severe WM lesion might predict stroke-associated pneumonia in patients with acute ischemic stroke [24]. However, in these studies, the location of WM lesions was not considered.
Recently, growing evidences about the location of WM and neurologic deficit were reported. WM lesions at the frontal horns were reported to result in more significant cortical deafferentation and cognitive dysfunction [15, 16]. Another study reported the strategic subcortical hyperintensities in cholinergic pathways and executive function decline in Alzheimer patients [17]. In this study, CBT involvement of WM lesions did affect some parameters of VFSS. Of course, the more severe a WM lesion is, the greater the involvement of CBT. In group comparisons according to CBT involvement, the Fazekas grade showed significant difference among groups. However, multivariate regression analysis showed that the location of CBT had significant influence on the inadequate laryngeal elevation and prolonged pharyngeal transit time regardless of the Fazekas sum score.
Therefore, abnormal swallowing parameters or prolonged pharyngeal transit times might result from the combined effects of acute focal damage and preexisting destruction of CBT pathways. Increased periventricular WM lesions might contribute to this inefficient use of neural networks. This observation might be due to disruptions in the corticobulbar tract [25].
In swallowing function after stroke, CBT might have an important role. It plays a functional role in motor function of the non-oculomotor cranial nerve, therefore it affects the bulbar function. The CBT is associated with the muscles of the face, head, and neck. For this reason, injury of CBT often results in bulbar symptoms, such as dysphagia, dysarthria, and facial palsy [26]. A recent study reported that early swallowing recovery after stroke was influenced by lesions disrupting CBT fibers. Disrupting these fibers would lead to disconnection of the swallowing centers in the cortex and brain stem [27].
Based on these previous studies mentioned above, WM lesion location involving CBT might affect the integrity of the tract that results in dysphasia after stroke. The involved tract holds primary influence on the pharyngeal phase on swallowing, inadequate laryngeal elevation, and delayed pharyngeal transit time. In a previous study, more severe WM lesions showed longer oral transit times [11]. However, in this study, the location of CBT affected the pharyngeal phase predominantly.
The main limitations of our study are its retrospective design and the relatively small sample size. However, although imaging was assessed retrospectively, videofluoroscopic swallowing evaluations were performed according to a standard method. Moreover, clinical data such as vascular risk factors are routinely collected in patient admission records. Another limitation relates to the imaging analysis method. In our study, we assessed the involvement of CBT in WM lesions by only the presence of high signal intensity in structural MRI. The integrity of CBT was not demonstrated by a more objective method, such as diffusion tensor tractography.
Further research with a prospective design and advanced neuroimaging analysis such as diffusion tensor imaging is needed to confirm the associations of swallowing problems with WM lesion location and to complement the limitations of this study. Also, we could not analyze all the region of interests related with swallowing function except CBT. In future study, another ROI associated with swallowing function should be considered to complement our study.
Conclusions
In summary, our results suggest that WM lesion’s location involving the CBT might affect the integrity of the tract that results in dysphagia in older patients with mild stroke, regardless of the initial stroke severity. CBT predominantly influenced the pharyngeal phase of swallowing, with inadequate laryngeal elevation and delayed pharyngeal transit time. Accordingly, the location of WM lesions can be regarded as a potential predictive factor for dysphagia. Moreover, in patients with WM lesions involving CBT, a detailed evaluation for dysphagia is needed.
References
Denti L, Scoditti U, Tonelli C, Saccavini M, Caminiti C, Valcavi R, et al. The poor outcome of ischemic stroke in very old people: a cohort study of its determinants. J Am Geriatr Soc. 2010;58(1):12–7.
Forti P, Maioli F, Procaccianti G, Nativio V, Lega MV, Coveri M, et al. Independent predictors of ischemic stroke in the elderly: prospective data from a stroke unit. Neurology. 2013;80(1):29–38.
Liou LM, Chen CF, Guo YC, Cheng HL, Lee HL, Hsu JS, et al. Cerebral white matter hyperintensities predict functional stroke outcome. Cerebrovasc Dis. 2010;29(1):22–7.
Inzitari D, Pracucci G, Poggesi A, Carlucci G, Barkhof F, Chabriat H, et al. Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS (leukoaraiosis and disability) study cohort. BMJ. 2009;339:b2477.
Murray ME, Vemuri P, Preboske GM, Murphy MC, Schweitzer KJ, Parisi JE, et al. A quantitative postmortem MRI design sensitive to white matter hyperintensity differences and their relationship with underlying pathology. J Neuropathol Exp Neurol. 2012;71(12):1113–22.
Mitchell GF. Effects of central arterial aging on the structure and function of the peripheral vasculature: implications for end-organ damage. J Appl Physiol (1985). 2008;105(5):1652–60.
Bisschops RH, van der Graaf Y, Mali WP, van der Grond J, group Ss. High total cerebral blood flow is associated with a decrease of white matter lesions. J Neurol. 2004;251(12):1481–5.
Madden DJ, Bennett IJ, Song AW. Cerebral white matter integrity and cognitive aging: contributions from diffusion tensor imaging. Neuropsychol Rev. 2009;19(4):415–35.
Levine R, Robbins JA, Maser A. Periventricular white matter changes and oropharyngeal swallowing in normal individuals. Dysphagia. 1992;7(3):142–7.
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41(3):482–6.
Moon HI, Nam JS, Leem MJ, Kim KH. Periventricular white matter lesions as a prognostic factor of swallowing function in older patients with mild stroke. Dysphagia. 2017;32(4):480–6.
Lavin JM, Tieu D, Maddalozzo J. Complementary and integrative treatments: swallowing disorders. Otolaryngol Clin N Am. 2013;46(3):447–60.
Jenabi M, Peck KK, Young RJ, Brennan N, Holodny AI. Identification of the corticobulbar tracts of the tongue and face using deterministic and probabilistic DTI fiber tracking in patients with brain tumor. AJNR Am J Neuroradiol. 2015;36(11):2036–41.
Jo KW, Kim Y, Park GY, Park IS, Jang Y, Gyun SD, et al. Oropharyngeal dysphagia in secondary normal pressure hydrocephalus due to corticobulbar tract compression: cases series and review of literature. Acta Neurochir (Wien). 2017;159(6):1005–11.
Bohnen NI, Bogan CW, Muller ML. Frontal and periventricular brain white matter lesions and cortical deafferentation of cholinergic and other neuromodulatory axonal projections. Eur Neurol J. 2009;1(1):33–50.
Blahak C, Baezner H, Pantoni L, Poggesi A, Chabriat H, Erkinjuntti T, et al. Deep frontal and periventricular age related white matter changes but not basal ganglia and infratentorial hyperintensities are associated with falls: cross sectional results from the LADIS study. J Neurol Neurosurg Psychiatry. 2009;80(6):608–13.
Behl P, Bocti C, Swartz RH, Gao F, Sahlas DJ, Lanctot KL, et al. Strategic subcortical hyperintensities in cholinergic pathways and executive function decline in treated Alzheimer patients. Arch Neurol. 2007;64(2):266–72.
Lee KM, Jang Y, Kim YH, Moon SK, Park JH, Park SW, Yu HJ, Lee SG, Chun MH, Han TR. Reliability and validity of Korean Version of National Institutes of Health Stroke Scale. J Korean Acad Rehab Med. 2004;28:422–35.
Logemann JA, Rademaker AW, Pauloski BR, Ohmae Y, Kahrilas PJ. Normal swallowing physiology as viewed by videofluoroscopy and videoendoscopy. Folia Phoniatr Logop. 1998;50(6):311–9.
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149(2):351–6.
Jang SH, Seo JP. The anatomical location of the corticobulbar tract at the corona radiata in the human brain: diffusion tensor tractography study. Neurosci Lett. 2015;590:80–3.
Kumar S, Doughty C, Doros G, Selim M, Lahoti S, Gokhale S, et al. Recovery of swallowing after dysphagic stroke: an analysis of prognostic factors. J Stroke Cerebrovasc Dis. 2014;23(1):56–62.
Poggesi A, Gouw A, van der Flier W, Pracucci G, Chabriat H, Erkinjuntti T, et al. Cerebral white matter changes are associated with abnormalities on neurological examination in non-disabled elderly: the LADIS study. J Neurol. 2013;260(4):1014–21.
Nam KW, Kwon HM, Lim JS, Lee YS. Leukoaraiosis is associated with pneumonia after acute ischemic stroke. BMC Neurol. 2017;17(1):51.
Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009;40(5):1903–6.
Clark DL, Boutros NN, Mendez MF. The brain and behavior: an introduction to behavioral neuroanatomy. 2nd ed. Cambridge: Cambridge University Press; 2005.
Galovic M, Leisi N, Pastore-Wapp M, Zbinden M, Vos SB, Mueller M, et al. Diverging lesion and connectivity patterns influence early and late swallowing recovery after hemispheric stroke. Hum Brain Mapp. 2017;38(4):2165–76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to declare with respect to the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Moon, H.I., Kim, G.S. & Lee, E. Is the Location of White Matter Lesions Important in the Swallowing Function of Older Patients with Mild Stroke?. Dysphagia 34, 407–414 (2019). https://doi.org/10.1007/s00455-018-9955-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-018-9955-y