Abstract
Factors that can facilitate early identification of individuals at risk of dysphagia such as stroke location are potentially of great benefit. The aim of this study was to examine the role of hemisphere and lesion location in assessing dysphagia pattern and airway invasion as identified through the use of validated, standardized interpretation measures for the videofluoroscopic swallowing study. Consecutive patients (N = 80) presenting with stroke symptoms who had a first-time acute ischemic stroke confirmed on diffusion-weighted magnetic resonance imaging (DW-MRI) scan participated. Three swallowing outcome variables were assessed using regression models: modified barium swallow impairment profile (MBSImP) oral impairment (OI) and pharyngeal impairment (PI) scores and penetration aspiration scale (PAS) score. Subjects were primarily male and demonstrated mild stroke and mild to moderate dysphagia. There was a significantly higher likelihood of abnormal PAS scores for infratentorial lesions compared to right hemisphere location (Odds ratio: 3.1, SE: 1.8, p = 0.046) and for Whites compared to African Americans (Odds ratio: 5.5, SE: 2.6, p = <0.001). However, OI scores were higher (worse) in African Americans compared to Whites (Beta = −1.2; SE: 0.56; p = 0.037). PI scores had no significant association with race or lesion location. Using DW-MRI to identify infratentorial stroke can help identify individuals at risk of airway invasion; however, imaging information concerning supratentorial infarct hemisphere and location may not be useful to predict which individuals with mild stroke are at risk for dysphagia and aspiration when admitted with acute stroke symptoms. Future studies should explore the role of race in the development of stroke-related dysphagia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysphagia is a frequent occurrence following stroke affecting approximately 50% of stroke survivors [1]. Early identification of dysphagia and aspiration risk can reduce morbidity and mortality, and reduce length of hospitalization [2,3,4]. Factors that can facilitate identification of individuals at risk of dysphagia would be of great benefit. One such factor could be stroke location. If a specific hemisphere or anatomic location was highly associated with dysphagia, individuals with acute infarction involving these specific brain regions could be targeted for expedited referral and evaluation by speech pathology. It is well established that a single supratentorial stroke can result in dysphagia with research suggesting that subcortical white matter involvement is associated with dysphagia [5,6,7,8,9]. Moreover, some studies have suggested that the hemisphere lesioned is associated with dysphagia incidence, severity, and/or characteristic of swallowing dysfunction [9,10,11,12]. That is, pharyngeal stage dysfunction, more severe dysphagia, and aspiration frequently occur following right hemispheric stroke, whereas oral stage dysfunction and less severe dysphagia are more frequent following left hemispheric stroke [11, 12]. Other research has identified no differences between dysphagia incidence, severity, or characteristics and hemisphere damaged [5, 8, 13, 14].
Past studies have frequently been based on a variety of imaging acquisition methods, magnetic resonance imaging (MRI), and/or computed tomography (CT), which may have influenced results. Using diffusion-weighted (DW) MRI can ensure that hyperacute lesions are identified. Moreover, a standard measure to define and classify dysphagia has not been used, with most studies focusing on airway invasion to determine dysphagia [8, 9]. It is well understood, however, that significant dysphagia without aspiration can occur following stroke [5, 6, 12]. Therefore, the primary aim of this study was to determine whether hemisphere and lesion location were associated with dysphagia pattern and airway invasion as identified through the use of validated, standardized interpretation measures for the videofluoroscopic swallowing study (VFSS).
Methods
Subjects
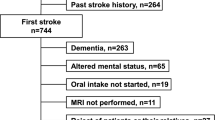
Participants included 80 individuals consecutively admitted to the Michael E. DeBakey VA Medical Center (MEDVAMC) from October 2012 to November 2014 with first-time acute ischemic stroke confirmed on the DW-MRI sequence. These individuals were part of a larger cohort of 250 patients participating in a stroke swallowing screening study for which the exclusion criteria included history of neurological disease other than stroke, history of head and neck structural damage or surgery, dysphagia unrelated to the current stroke, obtunded mental status, current presence of pneumonia or ventilator support, not competent and no legally authorized representative, and greater than five days past MEDVAMC admission [15]. The 170 additional participants from the original study were not included in this analysis as they were diagnosed with transient ischemic attack, DW-MRI was negative for acute stroke, DW-MRI was not completed, or they had a history of previous stroke. The demographic information of age, sex, and race as well as admission National Institutes of Health Stroke Scale (NIHSS) scores was obtained from the participants’ medical records.
The study was approved by the Institutional Review Board at Baylor College of Medicine and the Research and Development Committee at MEDVAMC in Houston, TX. All individuals provided written consent prior to participation.
Procedures
VFSS Acquisition and Analysis
Swallowing was evaluated using VFSS which were completed on average within 45.8 ± 26.7 h of admission. Lateral radiographic views of swallowing were obtained as the participants completed two non-cued trials each of self-administered Varibar thin liquid barium (5 ml, self-regulated cup sip) and 5 ml of Varibar barium pudding. Single trials of a masticated barium-coated cookie and sequential swallowing of 90 ml of Varibar thin liquid barium were also completed. The VFSS was initiated with the 5 ml thin liquid volume and progressed accordingly unless consistent significant aspiration was observed that could not be eliminated with therapeutic intervention. The VFSS was acquired using continuous fluoroscopy and recorded at 30 frames per second on the KayPentax Digital Swallow Workstation for later analysis.
The recorded VFSS were analyzed using the modified barium swallow impairment profile (MBSImP) [16] and the penetration aspiration scale (PAS) [17] by two speech-language pathologists (CBS, SKD) with over 25 years of experience in analyzing VFSS and who were certified in MBSImP analysis. The VFSS were judged using consensus scoring between the two raters who were blinded to lesion classification.
The MBSImP is a validated, standardized semi-objective measure to evaluate oral and pharyngeal swallowing physiology. Typically, 17 components are measured (6 oral, 10 pharyngeal, 1 esophageal) using a rank-ordered severity scale. As swallows were non-cued, oral component 2 (tongue control) was not evaluated. Additionally, as an anterior–posterior view was not obtained, pharyngeal component 13 (pharyngeal contraction) and esophageal component 17 (esophageal clearance) were not obtained. An overall impairment (OI) score based on the highest (worst) score for each component across all swallows was recorded. Oral OI scores and pharyngeal OI scores were then summed to obtain the oral total (range 0–19) and pharyngeal total (range 0–26) impairment scores.
The PAS is a valid, ordinal scale that evaluates depth, patient response, and clearance of airway invasion. Scores range from 1, no penetration or aspiration, to 8, silent aspiration. PAS scores were calculated across all trials for each participant. Since the PAS score distribution was unbalanced across all ordinal scale categories, we divided the PAS score outcomes into a binary variable with scores less than or equal to two categorized as normal and scores greater than two categorized as abnormal.
MRI Acquisition and Analysis
MRI brain scans were obtained on each participant upon hospital admission (44.9 ± 26.4 h). Diffusion-weighted, T2-weighted, and FLAIR sequences were reviewed by a board-certified/CAQ (certificate of added qualification in Neuroradiology) attending radiologist who was blinded to VFSS results. In acquiring the clinical MRI scans, four different vendor platforms were used with varying field strengths: Seimens Trio 3T [b1000, TE 76 ms, TR 4000 ms, SL 5/1.5 mm], Philips Achieva 3T [b1000, TE 64 ms, TR 4400 ms, SL 4 mm/1.0], Philips HFO 1T [b1000, TE 75 ms, TR 5057 ms, SL 4 mm/1.0], and GE 450 W 1.5T [b1000, TE-80-90 ms, TR 8000 ms, SL 5/0.5 mm]. Lesions were localized according to hemisphere (right, left, infratentorial, bilateral). Supratentorial lesions were further classified according to location: cortical, subcortical, and cortical–subcortical. Subcortical and cortical–subcortical lesion locations were additionally sub-classified based on involvement of gray matter, white matter, or both types of brain tissue. Infratentorial lesions were also sub-classified according to location: cerebellum, midbrain, pons, and medulla. Two individuals had infratentorial lesions with subcortical white matter extension. They were classified as infratentorial.
Statistical Analyses
Three swallowing outcome variables were assessed: OI score, PI score, and PAS score. The primary explanatory variable was lesion classification based on hemisphere (right, left, infratentorial, bilateral). In order to avoid multicollinearity, the primary hemisphere lesion classification variable and the cortical/subcortical lesion classification variable were not included simultaneously in the regression models due to very high association (χ 2 > 40.0; p < 0.001; Cramer’s V > 0.5) among these variables [18].
Age and race were used to control for any inequality in outcomes that may arise due to genetic or biological differences among participants [19]. Sex was excluded as a covariate in the analyses due to a very small proportion of female participants (n = 3). The NIHSS was excluded during the analysis due to very low correlation between NIHSS scores and the outcome variables (r < 0.5). The NIHSS score for 89% of the participants was between 0 and 5, indicating that most of our study population had a mild stroke; the highest NIHSS score in the cohort was 12.
All explanatory variables were summarized using percentages and frequencies for categorical variables and means and SDs for continuous variables. Differences in outcome variables were examined using Student’s t tests or analyzed using analysis of variance (ANOVA). Since multiple PAS scores were obtained across trials for each participant, random-effects logistic regression using a binomial distribution, logit link, and cluster-adjusted robust standard errors was utilized to estimate the association between PAS scores and the explanatory variables. Analyses were conducted using STATA, version 13.0 (Stata Corp., College Station, Texas). Ordinary least-squares (OLS) regression was employed to estimate the association between the impairment score outcome variables and the explanatory variables since these outcome variables followed a normal distribution.
Results
The initial sample had 80 participants with a mean age of 64 years. Slightly more than one-half of these (54%) were African American, and a majority were male (96%) (Table 1). All of the White participants were non-Hispanic except for three individuals. The population demographics were reflective of the veteran population receiving services at our study site. Most infratentorial infarcts involved the pons (54.5%), while most supratentorial infarcts were isolated subcortical strokes (47%). The overall averages for PAS score, oral OI score, and pharyngeal OI score in our sample were 1.5 (range: 1–8), 7.4 (range: 3–14), and 5.0 (range: 0–16), respectively (Tables 2 and 3), suggesting relatively mild to moderate dysphagia in the majority of our cohort. After binary categorization of PAS scores, we had 83.4% normal (PAS ≤ 2) and 16.6% abnormal (PAS ≥ 3). The two patients with bilateral lesion location were excluded during regression analyses due to the extremely small cell size. Thus, our final sample size had oral and pharyngeal OI scores for 78 observations, but we had 1024 observations (from 78 patients) for PAS scores.
The random-effects logistic regression model results using PAS score categories (Table 4) showed that there was a significantly higher likelihood of abnormal PAS scores for infratentorial lesions compared to RHD lesions (odds ratio: 3.1, SE: 1.8, p = 0.046) and for Whites (more impairment) compared to African Americans (Odds ratio: 5.5, SE: 2.6, p < 0.001). There was no significant association between PAS scores and participant age.
In the OLS regression models (Table 5), there were no significant associations between oral OI scores and hemisphere or participant age. Oral OI, however, was significantly associated with race (p = 0.04), with Whites having OI scores 1.2 points lower (less impairment) than African Americans. There was no significant association between pharyngeal OI scores and hemisphere, age, or race.
For other types of lesion classification, the ANOVA for supratentorial location had no significance for oral OI scores (F = 0.19, p = 0.830) or pharyngeal OI scores (F = 0.25, p = 0.741). Moreover, ANOVA measures of association between subcortical gray and white matter involvement and oral OI scores (F = 1.79, p = 0.180), or pharyngeal OI scores (F = 0.01, p = 0.987) were not statistically significant. Similarly, the analysis of variance for infratentorial location had no significance for oral OI scores (F = 0.47, p = 0.706) or pharyngeal OI scores (F = 2.2, p = 0.124).
Separate bivariate random-effects logistic regression for measuring the association of PAS scores with supratentorial location (Wald Chi Square: 1.76, p = 0.415), subcortical gray and white matter involvement (Wald Chi Square: 0.94, p = 0.625), or infratentorial location (Wald Chi Square: 2.24, p = 0.135) had no significant association between PAS scores and these lesion classification variables.
Sensitivity Analysis
The regression models were reevaluated after excluding extreme outlier values as shown in Fig. 1. No meaningful differences in regression results were identified. Similarly, we did not find any meaningful differences in regression results after excluding the females from our data; therefore, all data points were included in the analyses.
Box-plot of oral OI scores and pharyngeal OI scores. The box-plot (aka box-and-whiskers plot) visually displays a five-number summary of each continuous variable. The first and third quartiles are the horizontal ends of each box and represent the interquartile range (IQR). The dashed line in the interior of the box is the median, and the maximum and minimum are the ends of the whiskers. The diamond and square points denote outlier observations that are at least 1.5 times the IQR of their respective distributions
Discussion
The aim of this study was to determine if hemisphere and supratentorial and infratentorial locations predicted swallowing characteristics and risk of airway invasion. There were three major findings from the study. First, hemisphere was an independent predictor of risk of airway invasion. Infratentorial strokes were associated with higher PAS scores compared to supratentorial stroke. Second, neither hemisphere nor supratentorial location was a predictor of oral stage or pharyngeal stage impairment. Third, race independently predicted both PAS scores and OI scores. Notably, African Americans showed higher oral OI scores but lower PAS scores than Whites. Findings expand on previous research by using DW-MRI scans to localize all lesions in a large cohort of consecutively admitted patients with acute first-time stroke. Further, a valid and reliable standard measure to determine overall oral and pharyngeal stage impairment was utilized.
Infratentorial brain regions, particularly the pons and medulla, have long been identified as important in swallowing [for review, [20] ]. The medulla contains the swallowing central pattern generator [21] which provides rhythmic patterns of pharyngeal swallowing activity, and the pons is a sensory relay system providing information from the peripheral oral, pharyngeal, and laryngeal receptors to higher nervous systems [22]. Systematic review of studies using MRI to confirm lesion location identified a high incidence of dysphagia involving the pons and medulla with limited to no incidence involving the midbrain and cerebellum [23]. It is important to note that most of the studies that we reviewed identified dysphagia based on clinical, not instrumental, evaluation. Without objective instrumental measures, the occurrence of dysphagia and airway invasion cannot be confirmed which limits the strength of results from these studies. Findings from our study, using VFSS analyzed with objective swallowing measures, identified higher PAS scores to be associated with infratentorial stroke compared to supratentorial stroke which helps support findings from these clinical studies. However, infratentorial stroke did not predict overall OI or PI. It may be that PAS is a more sensitive swallowing measure, at least in mild stroke and mild dysphagia. Specific infratentorial brain regions (cerebellum, midbrain, pons, medulla) could not be reliably assessed for any swallowing outcome due to small cell sizes for most infratentorial brain region locations in our sample. Thus, we cannot draw any conclusion on how lesioning these specific infratentorial brain regions affects swallowing.
Laterality of swallowing characteristics was not identified in this study. That is, there was no significant difference in airway invasion as measured by the PAS between right and left hemispheric stroke. Moreover, oral and pharyngeal stage dysfunction, as measured by the MBSImP, did not differ based on hemisphere. Findings support previous research which suggests equal incidence of oral and pharyngeal dysphagia and risk of aspiration regardless of hemisphere lesioned [5, 8, 13, 14]. While current thought based on functional brain imaging and transcranial magnetic stimulation supports a dominant swallowing hemisphere, independent of handedness, the hemisphere of dominance is variable with no distinction between oral and pharyngeal dysfunction [for review, [24] ]. Moreover, we did not identify higher oral and pharyngeal OI scores and higher PAS scores to be associated with cortical, subcortical, or cortical–subcortical location consistent with previous research [5, 14]. Further analysis concerning the effects of subcortical white matter versus gray matter lesions revealed no relationship between white matter involvement and dysphagia, which has been identified in numerous studies [5,6,7,8,9]. Our power, however, may have been limited due to small sample sizes.
Surprisingly, we identified race to be an independent predictor in our swallowing measures with African Americans having significantly higher OI scores as compared to Whites and Whites having significantly higher PAS scores compared to African Americans. These findings were independent of lesion localization and age and cannot be explained by differences in NIHSS score as the majority of participants had a mild stroke. There is limited understanding concerning the effects of race on swallowing. Two previous studies conducted using various U.S. medical databases demonstrated increased incidence of stroke-related dysphagia in minority groups, particularly Asians, as compared to Whites [25, 26]. Characteristics of dysphagia were not identified as data were captured retrospectively using ICD-9 codes. Our work partially supports and expands the findings of Gonzalez-Fernandez et al. [25, 26] in that we found higher oral OI scores in African Americans than Whites. Our work, however, disagrees with these database studies that suggest minorities may be at higher risk of dysphagia as we identified significantly higher PAS scores in Whites which has also been previously reported [6]. Given the small number of Hispanic participants, ethnicity was not analyzed. To our knowledge, this is the first study to analyze the combined effect of race and lesion location on swallowing. We do not have information on comorbid history which may help explain the results. Due to the limited literature available on race, ethnicity, and dysphagia, the reason for such a dichotomy between oral impairment and PAS outcomes is not clear. The scoring methodology was different between the two measures. Further research is required to determine if these findings are stable, and whether our findings reflect true risk effects related to race or differences in measurement methods.
Limitations
Our stroke cohort was large for a group of consecutively admitted first-time stroke patients who underwent DW-MRI and VFSS compared to previous studies which analyzed both CT and MRI [5, 9, 10, 14], evaluated referrals for dysphagia evaluation [9, 14], and/or determined dysphagia based on clinical assessment [7, 8, 10]. Nevertheless, the majority of our participants had mild stroke based on the NIHSS score. While mild stroke can produce dysphagia and aspiration [6, 15], this may have contributed to some of the reported differences between our findings and past research. Moreover, the majority of the cohort demonstrated relatively mild to moderate dysphagia based on PAS, oral OI, and pharyngeal OI scores. Thus, the generalizability of our results cannot be extended to populations with more severe stroke or more severe dysphagia. Although the MBSImP takes into consideration some normative data such as not considering residual trace coating of structures in the OI and PI, the use of the MBSImP has not been systematically studied in healthy young and older adults, and thus specific oral and pharyngeal OI scores have not been identified that distinguish between normal and disordered swallowing. Furthermore, the number of swallows scored by the PAS was variable across subjects due to either dysphagia severity which restricted the number of trials or observed differences in the number of swallows required to sequentially swallow a 90 ml thin liquid volume. This variability in the number of swallows may have influenced results. Last, while imaging with DWI is standard, slice thickness/imaging parameters on three different vendor platforms (Siemens, GE, Philips) with varying field strengths (1.0–3.0 T) resulted in inherent imaging variation. In addition, protocols did not include volumetric 3D sequences precluding volume measurements. Lesion size and region of interest may provide further information concerning the effects of ischemic stroke on swallowing as well as how these factors paired with race may impact the occurrence of dysphagia.
Conclusions
For individuals with mild stroke and mild to moderate dysphagia, supratentorial hemisphere and lesion location do not appear to predict dysphagia and aspiration risk. While infratentorial stroke is associated with higher PAS score, it is unclear whether specific regions are associated with increased airway invasion. It is notable that the majority of patients in our study had mild stroke and mild dysphagia which limits the generalizability of our results to individuals with more severe stroke or more severe dysphagia. As such, based on these data, DW-MRI data cannot be used to predict which individuals are at risk for dysphagia and aspiration when admitted with stroke symptoms. Therefore, we would recommend that all individuals presenting with suspected stroke should have swallowing screening. Race appears to be an independent factor related to swallowing safety and stage of impairment, albeit in different ways for African Americans and Whites. Further research is required to fully understand the effects of race on the development of stroke-related dysphagia.
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63. doi:10.1161/01STR.0000190056.76543.eb.
Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005;36:1972–6. doi:10.1161/01.STR.0000177529.86868.8d.
Odderson IR, McKenna BS. A model for management of patients with stroke during the acute phase. Outcomes and economic implications. Stroke. 1993;24:1823–7. doi:10.1161/01.STR.24.12.1823.
Martino R, Pron G, Diamont N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidance. Dysphagia. 2000;15:19–30. doi:10.1007/s004559910006.
Daniels SK, Foundas AL. Lesion localization in acute stroke. J Neuroimaging. 1999;9:91–8. doi:10.1111/jon19999291.
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41:482–6. doi:10.1161/STROKEAHA.109.566133.
Gonzalez-Fernandez M, Kleinman JT, Ky PKS, Palmer JB, Hillis AE. Supratentorial regions of acute ischemia associated with clinically important swallowing disorders. Stroke. 2008;39:3022–8. doi:10.1161/STROKE.AHA.108.518969.
Galovic M, Leisi N, Muller M, Weber J, Abela E, Kagi G, Weder B. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013;44:2760–7. doi:10.1161/STROKE.AHA.113.001690.
Suntrup S, Kemmling A, Warnecke T, Hamacher C, Oelenber S, Niederstadt T, Heindel W, Wiendl H, Dziewas R. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 1: dysphagia incidence, severity, and aspiration. Eur J Neurol. 2015;22:832–8. doi:10.1111/ene.12670.
Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, Pedace C, Lenzi L. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009;18:329–35. doi:10.1016/j.jstrokecerebrovasdis.2009.01.009.
Daniels SK, Foundas AL, Iglesia GC, Sullivan MA. Lesion site in unilateral stroke patients with dysphagia. J Stroke Cerebrovasc Dis. 1996;6:30–4. doi:10.1016/S1052-3057(96)80023-1.
Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993;74:1295–300. doi:10.1016/0003-9993(93)90082-L.
Alberts MJ, Horner J, Gray L, Brazer SR. Aspiration after stroke: lesion analysis by brain MRI. Dysphagia. 1992;7:170–3. doi:10.1007/BF02493452.
Jeon WH, Park GW, Lee JH, Jeong HJ, Sim YJ. Association between location of brain lesion and clinical factors and findings of videofluoroscopic swallowing study in subacute stroke patients. Brain Neurorehabil. 2014;7:54–60. doi:10.12786/bn.2014.7.1.54.
Daniels SK, Pathak S, Rosenbek JC, Morgan RO, Anderson JA. Rapid aspiration screening for suspected stroke: part 1: development and validation. Arch Phys Med Rehabil. 2016;97:1440–8. doi:10.1016/j.apmr.2016.03.025.
Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS Measurement tool for swallow impairment-MBSImP: establishing a standard. Dysphagia. 2008;23:392–405. doi:10.1007/s00455-008-9185-9.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8. doi:10.1007/BF00417897.
Vatcheva KP, Lee MJ, Mccormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiological studies. Epidemiology (Sunnyvale). 2016;6(2):227. doi:10.4172/2161-1165.1000227.
Vander Weele TJ, Robinson WR. On causal interpretation of race in regressions adjusting for confounding and mediating variables. Epidemiology (Cambridge). 2014;25:473–84. doi:10.1097/EDE.0000000000000105.
Miller AJ. The neuroscientific principles of swallowing and dysphagia. San Diego: Singular; 1999.
Kessler JP, Jean A. Identification of the medullary swallowing regions in rats. Exp Brain Res. 1985;57:256–63. doi:10.1007/BF00236530.
Jean A. Brain control of swallowing: neuronal network and cellular mechanisms. Physiol Rev. 2001;81:929–69.
Flowers HL, Skoretz SA, Streiner DL, Silver FL, Martino R. MRI-based neuroanatomical predictors of dysphagia after acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2011;32:1–10. doi:10.1159/000324940.
Vansant DH, Hamdy S. Cerebral cortical control of deglutition. In: Shaker R, Belafsky PC, Postma GN, Easterling C, editors. Principles of deglutition. New York: Springer; 2013.
Gonzalez-Fernandez M, Kuhlemeier KV, Palmer JB. Racial disparities in the development of dysphagia after stroke: analysis of the California (MIRCal) and New York (SPARCS) inpatient databases. Arch Phys Med Rehabil. 2008;89:1358–65. doi:10.1016/j.apmr.2008.02.016.
Bussell SA, Gonzalez-Fernandez M. Racial disparities in the development of dysphagia after stroke: further evidence from the medicare database. Arch Phys Med Rehabil. 2011;92:737–42. doi:10.1016/j.apmr.2010.12.005.
Acknowledgements
The project described was based on work supported by a Merit Award (1I01RX000121) from the Rehabilitation Research & Development Service of the VA Office of Research and Development. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the University of Texas School of Public Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Stephanie K. Daniels, Shweta Pathak, and Robert Morgan received salary support for a grant from the Department of Veterans Affairs. Shalini V. Mukhi, Carol B. Stach, and Jane A. Anderson report no conflict of interest.
Rights and permissions
About this article
Cite this article
Daniels, S.K., Pathak, S., Mukhi, S.V. et al. The Relationship Between Lesion Localization and Dysphagia in Acute Stroke. Dysphagia 32, 777–784 (2017). https://doi.org/10.1007/s00455-017-9824-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9824-0