Abstract
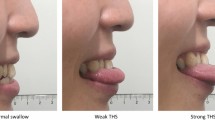
The aim of this prospective observational study was to determine the associations among age, maximum lingual isometric pressures, and maximum swallow pressures in specific regions of the tongue. Individuals 21 years and older who reported normal swallowing were enrolled. Seventy-one healthy adults were stratified by age into young (21–40 years), middle (41–60), and old (61–82) groups. Maximum pressures were measured for each individual during isometric tongue press tasks as well as saliva, 5, and 10 mL thin liquid bolus swallows at 5 sensors located on the hard palate: front, middle, left, right, and back. Lower maximum lingual pressures for all tasks were associated with increased age (p < 0.04). Saliva pressures exhibited a different pressure pattern than bolus swallows with pressures higher than bolus swallows on middle (p < 0.03) and back (p < 0.05) tongue sensors but not in the front. Diminished swallow pressure reserve (maximum isometric pressure–maximum swallow pressure) also was found with increased age (p < 0.03). Isometric pressures were greater than swallow pressures in young and middle age groups at both the front (p < 0.04) and back (p < 0.03) sensors, but only significantly greater at the front sensor for the oldest group (p < 0.04). Older healthy adults have lower lingual isometric pressures and lower swallow pressures than younger healthy adults. Elders have a decreased swallow pressure reserve to draw upon during occasions of physiological stress. While the exact mechanisms for age-related decline in lingual pressures remain unclear, they are likely due, at least in part, to sarcopenia. Saliva, 5, and 10 mL thin boluses also exhibit different age-related declines in pressure at specific sensors, indicating they may elicit different muscle activation patterns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of dysphagia is known to increase with age [1] with one in nine older healthy adults self-reporting signs of dysphagia [2] and up to 52 % of older nursing home residents suffering from this devastating condition [3]. In order to improve the understanding of swallowing biomechanics that contribute to dysphagia and subsequently target the underlying pathophysiology for treatment, it is necessary to examine normal swallowing across the age continuum.
The tongue is the major propulsive force in normal oropharyngeal swallowing. Lingual musculature is unique and consists of four intrinsic muscles (superior longitudinal, inferior longitudinal, transversus, and verticalis), which have origin and insertion in the muscles of the tongue, and four extrinsic muscles (palatoglossus, genioglossus, hyoglossus, and styloglossus), which have origin in structures outside the tongue and insertion in the tongue [4]. The anterior tongue consists of mostly fast twitch, type II muscle fibers and is used mainly for volitional movements, such as chewing and manipulation of a bolus [5]. The posterior tongue, in contrast, consists of mostly slow twitch type I muscle fibers and is involved in more involuntary movements mainly for bolus propulsion through the oropharynx.
Changes in oral motor function occur with age and are related to the decrease in size and strength of striated musculature that affect the whole body including lingual musculature, known as sarcopenia [6–8]. Previous research has revealed that healthy older adults generate lower maximum isometric pressure (MIP) than younger individuals, which is likely due in part to sarcopenia [8–16]. While MIP has been shown to decrease with age, no significant age differences have been found for maximum swallow pressure (MSP) [8–11, 13–16]. Swallowing is a submaximal pressure-generating task, meaning MSP is lower than MIP within the same individual. While MSP does not decrease with age, the aged swallow is nonetheless affected by the decrease in MIP due to a decrease in pressure reserve and pattern of pressure generation [15]. Swallow pressure reserve is the difference between the MIP and the MSP, and a decreased swallow pressure reserve increases the risk of dysphagia by limiting the amount that MIP can decrease (due to physiological stress) without affecting the MSP.
The purpose of this exploratory study was to compare MIP during single-sensor maximal lingual sensorimotor isometric presses to MSP during saliva, 5 mL thin liquid, and 10 mL thin liquid bolus swallows. Comparison of MIP to MSP values during various swallow tasks will elucidate the degree to which swallowing, a submaximal pressure generation task, may change with age, sensor location, and type of swallow.
This study also includes normative MIP and MSP data from the participating healthy cohort across age groups to allow comparisons and promote accurate, specifically-targeted development of dysphagia management and intervention programs. Findings will increase understanding of underlying swallowing biomechanics and how they are affected by age, which may help in identifying individuals most at risk for dysphagia and the potential impact of therapeutic interventions.
Methods
Subjects
The study participants comprised 71 healthy adults, 35 females and 36 males, stratified by age into three groups. The young group consisted of 12 males and 11 females between the ages of 21 and 40 years (mean = 25 years). The middle group consisted of 12 males and 12 females between the ages of 41 and 60 years (mean = 50 years). The old group consisted of 12 males and 12 females between the ages of 61 and 82 years (mean = 68 years). Groups were identified based on early work by Robbins and colleagues who found that swallowing begins to slow with age as early as the fourth decade of life and then more significantly after the sixth decade [17]. This study was approved by the Institutional Review Board of the University of Wisconsin-Madison, and all participants signed the informed consent statements.
Participants were recruited through community advertisements and flyers and underwent a phone screening. Inclusion criteria required that subjects should be at least 21 years of age with self-reported normal swallowing, consuming a general diet, and able to provide informed consent. Subjects were excluded from the study if they had a history of neurologic disease, head and neck cancer or surgery, history of swallowing problems, or food allergies. Subjects were asked whether they were right- or left-handed, but as the right-handed group was much larger than the left-handed group, the effect of handedness was not analyzed.
Instrumentation
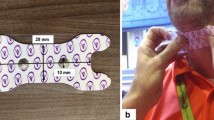
The Madison Oral Strengthening Therapeutic (MOST®) device (Swallow Solutions, LLC) was used in this study to measure pressures [18, 19]. The MOST® device was a portable unit which consisted of a netbook connected to a mouthpiece that was fitted to the subject’s hard palate. The pressure sensitive mouthpiece had five air-filled sensors; on the midsagittal plane, the front sensor was located at the alveolar ridge, the back sensor located at the posterior hard palate, and the middle sensor approximately halfway between (see Fig. 1). The left and right sensors were located lateral to the middle sensor. The sensors indirectly measured strength as the amount of pressure exerted between the tongue and the hard palate in units of hectopascals (hPa). This current study used the waveform function of the device, which measured pressure with a sampling frequency of 100 Hz. The waveforms were analyzed using functions in Excel and Matlab to determine the maximum pressures at each sensor for each task.
Tasks
Tasks performed were sorted into two categories: isometric pressure generation tasks and swallow tasks. Category order was randomized as well as task order within each category. The isometric category consisted of single-sensor isometric press tasks at each sensor, and the swallow category included saliva, 5 mL thin liquid bolus, and 10 mL thin liquid bolus swallow tasks. Subjects were provided with rest periods, and were provided verbal encouragement (Table 1).
Tasks in the isometric category included three sets of three maximum isometric presses at each individual target sensor. Each press was held for 2 s with a 2- to 3-s break between presses, and a 1-min break between sets. A 15-min break was provided between the isometric and swallow categories. Tasks in the swallow category included three repetitions each of saliva, 5 mL thin liquid, and 10 mL thin liquid swallows. Thin liquid boluses were room temperature water with a viscosity of ~1cP. Subjects were provided with 2- to 3-s break between task repetitions, and a 1-min break between swallow tasks.
Statistical Analysis
For statistical analysis, a three-way ANOVA was performed using SPSS with maximum pressure generated dependent on independent variables of age group, sensor location, and type of task [20]. Fisher’s least significant difference (LSD) post hoc tests were performed. A nominal p value of 0.05 was regarded as being statistically significant.
Results
Age Groups by Task
For the single-sensor isometric pressure tasks (Fig. 2a), MIPs significantly decreased between the young group (21–40 years) and the old group (61–82 years) (p < 0.04) as well as between the middle group (41–60) and the old group (p < 0.003) at both the front and back sensors.
Saliva MSPs (Fig. 2b) decreased significantly between the young and middle groups (p < 0.04), and between the young and old groups (p < 0.05) at the front sensor. 5-mL thin liquid MSPs (Fig. 2c) significantly decreased at both the front and back sensors between the young and middle groups (p < 0.05) and between the young and old groups (p < 0.04). The 10-mL thin liquid MSPs (Fig. 2d) significantly decreased at the back sensor between the young and old groups (p < 0.05).
Swallow Category by Age Group and Sensor Location
In the young group (21–40 years) (Fig. 3a), saliva MSPs were significantly greater than the 5-mL thin liquid MSPs at the left sensor (p < 0.03) and significantly greater than 10-mL thin liquid MSPs at the left, middle, and right sensors (p < 0.03). The 5-mL thin liquid MSPs also were significantly greater than the 10-mL thin liquid MSPs at the left sensor (p < 0.03). For the middle group (41–60 years) (Fig. 3b), saliva MSPs were significantly greater than the 5-mL thin liquid and 10-mL thin liquid MSPs at the back sensor only (p < 0.05). In the old group (61–82 years) (Fig. 3c), saliva MSPs were greater than the 5- and 10-mL thin liquid MSPs at the middle, left, and right sensors (p < 0.03). The difference did not reach significance at the back sensor.
Isometric Versus Swallow Categories by Age Group and Sensor Location
MIPs were greater than all MSPs in the young and middle groups (p < 0.04) at the front sensor, and greater than MSPs for saliva and 5-mL thin liquid swallows in the old group (p < 0.04). The diminishment of swallow pressure reserve, or the difference between MIP and MSP, was greatest between the middle and old groups. At the back sensor, MIPs were significantly greater than MSPs for the young and middle groups (p < 0.03) but there was no significant difference for the old group. The swallow pressure reserve decreased greatly between the middle and old group, to the point where MIP was no longer significantly greater than MSP in the old group (Fig. 4).
Discussion
Results of this exploratory study confirmed previous findings that MIPs decrease with age [8–16]. However, contrary to previous results that showed no change in MSPs [8–10, 12–16], MSPs in this study were found to decrease with age. The difference in results between studies may be due to variations in instrumentation and methodology used.
MSPs appear to decrease earlier in the life span and slower than MIPs. Significant decreases in MSP were found between the young and middle as well as the young and old groups, whereas significant decreases in MIP were found between the young and old as well as the middle and old groups. Sensor locations of MSP decline also varied in quantity and significance. While pressures at both the front and back sensors decreased significantly during the 5-ml thin bolus swallow, only pressures at the front sensor for the saliva swallow and back sensor for the 10-ml thin swallow decreased significantly. This suggests that pressures produced during a specific task vary relative to bolus parameters and swallow functional requirements, likely due to changes in the physiological handling of the bolus with variations in coordination and related muscle activation or to the way a bolus transfers the pressures. For instance, older individuals have been found to hold a bolus more posteriorly in the oral cavity [18]. Also, this finding may reflect the predominance of fast twitch Type II fibers in the anterior tongue and mostly slow twitch Type I fibers used more for involuntary, propulsive bolus movements at the posterior tongue.
The decrease in MSP shown to occur with aging is important for improved understanding of risk factors for dysphagia and definition of treatment parameters. Understanding this change, especially as it may relate to sarcopenic changes at the periphery, is crucial to future efforts to improve dysphagia prevention and treatment in older adults. While it is uncertain at this point that the same factors which cause a decrease in MIP generation also lead to a decrease in MSP generation, it is clear that the two decrease in parallel, while at different rates. These findings suggest that the study of strengthening therapies in the older population may be a logical and necessary step in dysphagia prevention and intervention. Since MIP and MSP decrease in parallel, strengthening the musculature that increases MIP at the desired location has the potential to increase the corresponding MSP. If MSP increases, which may be more related to central nervous system innervation, do not occur with increases in MIP, the pressure reserve increase would still be likely to decrease risk of dysphagia.
Additionally, data in this study show that saliva swallows produce a different pressure pattern than non-saliva swallows; saliva swallows result in lower pressures in the front and higher in the middle and back than 5- and 10-ml thin bolus swallows. As previously mentioned, it is likely that the bolus distributes the pressures generated by the tongue musculature over the palate in a pattern determined by the size, shape, and consistency of the bolus, leading to varying pressure patterns. Also, it is likely that the musculature is activated differently in response to change in parameters.
There were several limitations to this study. First, it did not include videofluoroscopic evaluation, which may have provided information regarding holding patterns for bolus containment. Also, there were a majority of right-handed subjects, which may affect the pressures applied to the lateral sensors. Additionally, potential confounders (e.g., gender, medical history/diagnoses, smoking history) were not accounted for in the statistical analyses.
The present work offers early steps toward improved understanding of bolus effects on not only maximum pressure generation, but also which muscles are recruited to produce more pressure and in what pattern the pressures occur as the bolus travels. Understanding pressures generated for specific bolus types and oral activities will improve the ability to treat dysphagia with dietary alterations and targeted strengthening therapy.
Finally, these data support that while both MIP and MSP decrease with age, the greatest decrease found is the difference between them, the pressure reserve [21]. Findings from previous studies examining decreases in pressure reserve with age are conflicting [22, 23], which is likely due to variations in methods used to collect pressures and calculate reserve. In this study, both the front and back sensors recorded a decrease in pressure reserve with age between the middle and old groups. The findings may reflect peripheral as well as central nervous system changes over the lifespan that may not occur in parallel, identical quantities. It has been found that increased white matter hyperintensities occur with age as does brain atrophy [24–26]. Little is known about further variability in these mechanisms relative to aging. Since reserve is necessary during times of physiological stress, the decrease found in this study may put the older population at greater risk for dysphagia. Increasing pressure reserve through strengthening therapy may play a role in decreasing the risk.
References
Morris H. Dysphagia in the elderly- a management challenge for nurses. Br J Nurs. 2006;15(10):558–62.
Anderson M, Anzalone J, Holland L, Tracey E. Treatment of language, motor speech impairments, and Dysphagia, Continuum (Minneap Minn). Neurorehabilitation. 2011;17(3):471–93.
Park Y-H, Han H-R, Oh B-M, Lee J, Park J, Yu SJ, Chang H. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs. 2013;34(3):212–7.
Chen P-H, Golub JS, Hapner ER, Johns MM. Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia. 2009;24(1):1–6.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46.
Pikus L, Levine MS, Yang Y-X, Rubesin SE, Katzka DA, Laufer I, Gefter WB. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. AJR Am J Roentgenol. 2003;180(6):1613–6.
Sokoloff AJ. Activity of tongue muscles during respiration: it takes a village? J Appl Physiol. 2004;96(2):438–9.
Stål P, Marklund S, Thornell L-E, De Paul R, Eriksson P-O. Fibre composition of human intrinsic tongue muscles. Cells Tissues Organs. 2003;173(3):147–61.
von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle. 2010;1(2):129–33.
Evans WJ. What is sarcopenia? J Gerontol A Biol Sci Med Sci. 1995;50:5–8.
Buehring B, Hind J, Fidler E, Krueger D, Binkley N, Robbins J. Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc. 2013;61(3):418–22.
Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50(5):M257–62.
Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The Effects of Lingual Exercise on Swallowing in Older Adults. J Am Geriatr Soc. 2005;53(9):1483–9.
Youmans SR, Youmans GL, Stierwalt JAG. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24(1):57–65.
Crow HC, Ship JA. Tongue strength and endurance in different aged individuals. J Gerontol A Biol Sci Med Sci. 1996;51(5):M247–50.
Steele CM, Bailey GL, Molfenter SM. Tongue pressure modulation during swallowing: water versus nectar-thick liquids. J Speech Lang Hear Res. 2010;53(2):273–83.
Robbins J, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103(3):823–9.
Robbins JA, Bomsztyk ED, Heppner AL, Koranda CL, Kroner AR, Kuchenreuther JM, Meister DM, Staerkel BS. Apparatus for measuring tongue/hard palate contact pressure. US6702765 B2. 2004.
Robbins JA, Hind JA, Hewitt AL. Oral-lever resistance exercise device. US7238145 B2. 2007.
IBM Corp. IBM SPSS statistics for windows. Armonk: IBM Corp.; 2013.
Lazarus CL, Logemann JA, Rademaker AW, Kahrilas PJ, Pajak T, Lazar R, Halper A. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Arch Phys Med Rehabil. 1993;74(10):1066–70.
Nicosia MA, Hind JA, Roecker EB, Carnes M, Doyle J, Dengel GA, Robbins J. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A Biol Sci Med Sci. 2000;55(11):M634–40.
Steele CM. Optimal approaches for measuring tongue-pressure functional reserve. J Aging Res. 2013;2013:542909.
Levine R, Robbins JA, Maser A. Periventricular white matter changes and oropharyngeal swallowing in normal individuals. Dysphagia. 1992;7(3):142–7.
Okada R, Okada T, Okada A, Muramoto H, Katsuno M, Sobue G, Hamajima N. Severe brain atrophy in the elderly as a risk factor for lower respiratory tract infection. Clin Interv Aging. 2012;7:481–7.
Birdsill AC, Koscik RL, Jonaitis EM, Johnson SC, Okonkwo OC, Hermann BP, Larue A, Sager MA, Bendlin BB. Regional white matter hyperintensities: aging, Alzheimer’s disease risk, and cognitive function. Neurobiol Aging. 2014;35(4):769–76.
Acknowledgments
The authors would like to thank Ronald Gangnon, PhD, for his guidance regarding statistical analysis for this manuscript. This article is the result of work supported by resources at the University of Wisconsin School of Medicine and Public Health (UW SMPH), the University of Wisconsin Department of Biomedical Engineering, and the William S. Middleton Memorial VA Hospital Geriatric Research Education and Clinical Center (GRECC), Madison, Wisconsin. The manuscript was prepared at the William S. Middleton Veteran Affairs Hospital in Madison, WI; GRECC manuscript #2015-016. The views and content expressed in this article are solely the responsibility of the authors and do not necessarily reflect the position, policy, or official views of the Department of Veteran Affairs or the U.S. government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
There are no relevant conflicts of interest to report for Nicole Rogus-Pulia, Naomi Humpal, or Kelsey Banaszynski. Jacqueline Hind is an employee of Swallow Solutions, LLC. JoAnne Robbins is inventor on patents administered through the Wisconsin Alumni Research Foundation, two of which have been licensed, one to Bracco Diagnostic Imaging and another to Swallow Solutions, LLC of which she is the founder.
Rights and permissions
About this article
Cite this article
Robbins, J., Humpal, N.S., Banaszynski, K. et al. Age-Related Differences in Pressures Generated During Isometric Presses and Swallows by Healthy Adults. Dysphagia 31, 90–96 (2016). https://doi.org/10.1007/s00455-015-9662-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9662-x