Abstract
Nephrotic syndrome is traditionally defined using the triad of edema, hypoalbuminemia, and proteinuria, but this syndrome is very heterogeneous and difficult to clarify. Its idiopathic form (INS) is probably the most harmful and essentially comprises two entities: minimal change disease (MCD) and focal segmental glomerulosclerosis (FSGS). We will consider some hypotheses regarding the mechanisms underlying INS: (i) the presence of several glomerular permeability factors in the sera of patients that alter the morphology and function of podocytes leading to proteinuria, (ii) the putative role of immune cells. Thanks to recent data, our understanding of these disorders is evolving towards a more multifactorial origin. In this context, circulating factors may be associated according to sequential kinetic mechanisms or micro-environmental changes that need to be determined. In addition, the resulting proteinuria may trigger more proteinuria enhancing the glomerular destabilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Idiopathic nephrotic syndrome: background and description
The kidneys account for only 1% of body weight but 10% of total oxygen consumption. It is a complex organ in terms of its development, structure, physiology, and pathology. The different types of kidney disorders include nephrotic syndrome, which was initially described by Hippocrates as a generalized edema, but it was not until 1722 that Theodore Zwinger evoked this pathology for the first time and placed the seat of the disease firmly in the kidneys. However, as far as we know, Zwinger did not perform any tests on the urine. Proteinuria in conjunction with edema was first described by Domenico Cotugno (1736–1820) in Naples, in his work “De ischiade nervosa commentaries” (1770). Some decades later (in 1827), Richard Bright performed a clever experiment to detect proteinuria by heating urine in a spoon held over a candle, and observed the coagulation of urines from these patients. It was Bright who finally associated generalized edema and proteinuria with kidney disease (Pal and Kaskel 2016).
Among the different forms of nephrotic syndrome, idiopathic nephrotic syndrome (INS) is probably the most deleterious. It is defined by significant selective proteinuria (> 3 g/day) associated with hypoalbuminemia, edema, and sometimes hyperlipidemia, but without inflammatory lesions (Eddy and Symons 2003). INS is a reflection of structural/functional alterations to the cellular components within glomeruli (Barisoni et al. 2007), followed by a loss of integrity of the glomerular filtration barrier. In affected glomeruli, podocytes acquire an impaired structure because their actin network is modified and their numbers fall due to cell death. The remaining podocytes then become hypertrophic in an attempt to cover the surface of glomerular capillaries. During the evolution of this pathology, the number of renal corpuscles decreases, they become hypertrophic by adaptation, and the presence of adhesions (synechiae) between Bowman’s capsule and the glomerular tuft can be observed. This situation may activate the parietal cells of the capsule, which may either replace the lost podocytes (beneficial role) or invade the glomerulus and secrete extracellular matrix proteins (deleterious role) (Smeets et al. 2011; Puelles et al. 2016; Kaverina et al. 2019).
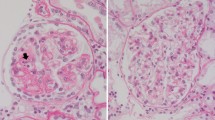
Reference is currently made to two principal forms of INS: nephrotic syndrome with minimal glomerular lesions (minimal changes disease, MCD) and focal segmental glomerulosclerosis (FSGS). MCD expresses itself as severe proteinuria without glomerular lesions or immunoglobulin deposits visible using optical microscopy or immunofluorescence. Ultrastructural lesions of MCD can be observed by electron microscopy and mainly consists in effacement of podocyte foot processes without loss of these cells (Eddy and Symons 2003). MCD is normally responsive to corticosteroid therapy which renders these podocyte lesions reversible. Glomerular damage caused in the context of FSGS results in irreversible scarring that entail a poorer prognosis and finally lead to end-stage kidney disease. The response to therapy is often linked to these different lesions, since most patients with MCD are sensitive to corticosteroids while those with FSGS are corticosteroid-resistant.
Rather than an authentic disease, FSGS is considered to result from a plethora of different glomerular impacts that are reflected by histological lesions such as sclerosis, hyalinosis, foam cell infiltration, or the vacuolization of podocytes. These lesions develop in a segmental (in part of the glomerulus) and focal manner (in some glomeruli) (D’Agati et al. 2011). The pioneering studies of Farquhar and Palade (1962) described how the visceral epithelium was mainly affected by the effacement of podocyte foot processes (Farquhar and Palade 1962). The Columbia classification (2004) distinguishes five types of lesions according to their topographic distribution within glomeruli: collapsing, tip, cellular, perihilar, and nonspecific (Han and Kim 2016). This morphological heterogeneity of FSGS may suggest the presence of different etiopathogenic agents at the source of this disorder.
A broad range of well-known causes, such as gene mutations in podocytes, viral infections, drug toxicity, and adaptive causes (nephron reduction, hyperfiltration) can be at the origin of the FSGS. By contrast, the cause for the idiopathic form remains elusive, despite considerable efforts to decipher its nature. In addition, some authors have proposed subclasses of FSGS as a function of clinical criteria such as its response to corticosteroids or immunosuppressive drugs (Rosenberg and Kopp 2017). It is also known that FSGS can relapse following kidney transplantation which is frequently followed by graft loss (Rudnicki 2016).
MCD and FSGS: two sides of the same coin?
However, it is still not totally clear whether MCD and FSGS are in fact two different phases in the same context of INS or two separate nosological entities. Although the debate is not closed, some evidence points towards the first hypothesis because (i) FSGS lesions are absent during the early phase of corticosteroid-resistant INS and (ii) FSGS lesions have been observed in serial biopsy samples reflecting progression of the disease (Fogo 2015; Fogo et al. 2015). Importantly, Canaud and colleagues reported some cases of a relapse of proteinuria after early transplantation although no glomerular lesions were visible under light microscopy (Canaud et al. 2010). However, electron microscopy revealed the extensive foot process effacement that is typical of MCD. This suggests that, at early stages in the recurrence, MCD was the main histological feature. Studying progression of the disease after the analysis of serial biopsies, the incidence of MCD decreased over the time, while that of FSGS variants increased (Canaud et al. 2010). Toxic models of proteinuria such as puromycin aminonucleoside or adriamycin induce at onset a loss of glomerular basement membrane polyanions resembling MCD, while at more advanced stages, glomerulosclerosis resembling FSGS can be seen (Bertelli et al. 2018). Nevertheless, there is no clear-cut separation between MCD and FSGS. In a pilot study, Ramezani et al. identified significant differences in plasma and urine miRNA profiles between patients with MCD and FSGS (Ramezani et al. 2015). These miRNAs could potentially serve as novel biological markers to distinguish FSGS from MCD. However, this study was limited by the small number of subjects in the control and MCD groups, as well as a significant age difference between the study groups. Urinary CD80 (B7–1) is a diagnostic tool that has been proposed to distinguish between MCD and FSGS (Garin et al. 2010). According to the authors, CD80 is released from the podocytes to urine in MCD but not in FSGS.
The INS might represent an evolutionary concept where MCD progresses to FSGS in the context of nephrotic syndrome. Agreeing with Maas and colleagues (Maas et al. 2016), there is no single cause of the initial podocyte injury because the development of podocyte lesions may result from more than one toxic factor. This idea might be very useful to improving the development of therapeutic approaches. For this reason, in this review, we are assuming this evolutionary notion that FSGS is a more advanced form of INS.
Glomerular permeability factors in the serum: the idea
For decades now, the nephrology community has been trying to decipher the identity of an enigmatic circulating factor found in the sera of idiopathic INS patients. This concept emerged after numerous observations which suggested an extra-renal origin for INS where the glomeruli are the target of some unknown circulating molecules produced in a systemic context. In an ethically questionable study, Gentili et al. (1954) administered plasma from infants affected by INS to healthy counterparts who subsequently developed transient proteinuria. The authors went on to suggest, for the first time, the presence of a serum circulating factor (SCF) as the cause for the disease (Gentili et al. 1954).
Undoubtedly, the most compelling evidence to support the notion of SCF is recurrence of the disease after transplantation, as described in 1972 by Hoyer and colleagues (Hoyer et al. 1972). They studied three patients with corticosteroid-resistant idiopathic nephrotic syndrome, at its onset and then during a recurrence. Some weeks after transplantation, they observed a relapse of nephrotic syndrome with severe proteinuria and no signs of an immunological reaction and concluded that a SCF must be the source of the recurrence (Hoyer et al. 1972). This hypothesis was reinforced in 1984 by Zimmerman and collaborators who infused sera from FSGS patients in rats, which rapidly developed proteinuria (Zimmerman 1984). Other studies reported that plasmapheresis procedures, performed in recurrent FSGS patients, transiently decreased or abolished proteinuria, resulting in a partial or complete remission (Artero et al. 1994; Feld et al. 1998). In 1994, Dantal and colleagues reported a drastic reduction of proteinuria after immunoadsorption sessions onto protein A columns. These authors demonstrated that injection of the eluates from these protein A columns reproduced proteinuria in the rats (Dantal et al. 1992). Other pieces of evidence were supplied, for example, by the disappearance of nephrotic syndrome lesions after transplanting kidneys from FSGS patients into healthy recipients (Gallon et al. 2012), or the maternal-fetal transmission of proteinuria. In this case, pregnant women affected by FSGS transfer proteinuria to the fetus which disappears some days after the delivery (Lagrue et al. 1991; Kemper et al. 2001).
Does proteinuria trigger proteinuria?
Physiologic proteinuria is produced in a normal range of < 150 mg/day, which is mainly reabsorbed by the proximal tubules. Under such conditions, proteins (mainly albumin) are internalized by the epithelial cells (PTECs) through a mechanism of receptor-mediated endocytosis, which are subsequently delivered to lysosomes to be recycled without any cell damage (Christensen et al. 2009). The idea that the podocytes could also participate in the processes of albumin reuptake was taking shape little by little. Thence, in a model of hyperalbuminemia, Ashworth and James described that post-glomerular filtered albumin induced swelling and vacuolization in podocytes (Ashworth and James 1961). However, it was not until 1986 when Yoshikawa et al. reported the first evidence of an endocytic internalization of albumin in podocytes from patients affected by FSGS (Yoshikawa et al. 1986). Posterior studies performed in different models of proteinuria described that an excess of intraglomerular albumin involves deleterious effects on podocytes, including cytoskeleton alterations or even cell death (Morigi et al. 2005; Tojo et al. 2008; Okamura et al. 2013; Gonçalves et al. 2018). Recently, Jarad and colleagues compared a mouse model of Alport syndrome (Col4a3−/−) with a double-knockout mouse Alport/albumin (Col4a3−/−; Alb−/−). They concluded that filtered albumin was injurious to kidney cells at glomerular level and that the lack of albumin reduced the renal pathology (Jarad et al. 2016).
Regarding the uptake of post-filtrated albumin, it is fascinating to note the striking similarity between the PTEC cells and podocytes since, according to works of Del Prete’s group, cubilin/amnionless complex is responsible, at least in part, for the albumin uptake in podocytes (Gianesello et al. 2017). Indeed, cubilin/amnionless and megalin are the most important receptors to protein uptake by PTECs since they transport soluble proteins to lysosomes for further recycling (De et al. 2014). Other interesting in vitro researches showed that intracellular overload of albumin in podocytes provokes endoplasmic reticulum stress and apoptosis via PKC/p38/caspase12 activation (Gonçalves et al. 2018), demonstrating its cytotoxic effect.
Furthermore, a recent and a very elegant study by Müller-Deile and colleagues offered even stronger evidence using a parabiotic system in zebrafish (Müller-Deile et al. 2019). They produced a parabiosis-based zebrafish model to generate a common circulation in two zebrafish larvae. A podocyte-specific gene (nephronectin) was knocked down in one zebrafish larva which was then fused to a second un-manipulated fish. The authors observed that the proteinuria present in the knockdown fish was transmitted to the normal, parabiotically fused partner. This suggested that a SCF could be induced by proteinuria as a “second hit” even when a dysregulated gene initiated the disease. They proposed that proteinuria triggers a disease-aggravating feedback loop in the circulation and perpetuates the proteinuria phenotype.
At the light of these results, it can be conclude that, after an initial “first hit” (e.g., SCFs, gene mutations, toxic drugs), the resulting proteinuria could act as “second hit,” thereby further impairing the structure of podocytes, leading to a more severe proteinuria (Fig. 1).
Serum circulating factors: diagram of pathogenic mechanisms in idiopathic nephrotic syndrome. Different stimuli stress blood cells, which secrete circulating factors to serum. SCFs target and damage the glomerular filtration barrier in their different structures (fenestrated endothelium, GBM: glomerular basement membrane and podocytes). Plasma proteins cannot be retained and cause proteinuria, which in turn aggravates the harmful effects of SCFs by acting on podocytes and increasing the synthesis/activity of SCFs
Serum circulating factors that are better understood
Numerous laboratories have tried to unravel the identity of SCFs. Some were described during the early MCD phase, while others were seen in advanced FSGS forms or in patients whose FSGS had relapsed following renal transplantation. It is possible that some SCFs are present during the entire process of glomerular degeneration, but it is also conceivable that others might appear sequentially at different stages of the disease. However, few data are available on the coexistence of several SCFs at different times during progression of the disease.
In this review, we have looked at the SCF that have been the subject of most study, including hemopexin, soluble urokinase-type plasminogen activator receptor (suPAR), cardiotrophin-like cytokine (CLCF-1), apolipoprotein A1, autoantibodies, and CASK (Table 1).
Hemopexin
Hemopexin, a plasma β1-glycoprotein, has been found to induce proteinuria in rats with lesions similar to those of MCD. It is able to alter the function of both the glomerular endothelium and podocytes. In glomerular endothelial cell monolayers, it reduces endothelial glycocalyx and increases albumin diffusion (Bakker et al. 2005b). The injection of hemopexin in rats induced proteinuria and glomerular foot process effacement (Cheung et al. 2000). Other in vitro studies on podocytes demonstrated that hemopexin could alter cytoskeletal distribution by activating Akt and RhoA, inducing reorganization of the actin cytoskeleton, and then compromising glomerular permeability (Lennon et al. 2008). Despite the fact that hemopexin is abundant in plasma [1 mg/ml], its pathogenicity in MCD appears to be dependent on its enzymatic activity as serine protease (Bakker et al. 2005a). To date, no other studies in FSGS patients have been reported.
Cardiotrophin-like cytokine factor 1 (CLCF-1)
Savin and colleagues postulated that SCF should exhibit a lectin-like affinity to sugars in the podocyte glycocalyx, thus further affecting cell signaling pathways. By using ex vivo glomeruli models, they studied the effect of SCFs on glomerular albumin permeability (Palb) and the impact of galactose on this activity. Their results showed that while SCF increased levels of glomerular Palb, galactose abrogated this effect (Savin et al. 2008; McCarthy et al. 2010). In support of these findings, the oral administration of galactose to a patient during a recurrence following transplantation markedly decreased serum permeability activity (Savin et al. 2008). These results therefore suggested that galactose prevents an interaction between SCF and glomeruli, having a protective effect. Some clinical studies have been performed to date, but their results have been uneven (Sgambat et al. 2013; Trachtman et al. 2015).
Following their first study, Savin et al. made use of this galactose-binding feature in order to understand the true nature of SCF. Using galactose affinity chromatography and subsequent tandem LC-MS/MS, this group identified cardiotrophin-like cytokine factor 1 (CLCF-1) in the plasma of recurrent FSGS patients. Furthermore, the eluted plasma fractions were able to induce proteinuria in rats (McCarthy et al. 2010). CLCF-1 is a member of the IL-6 cytokine family and was initially cloned from T-cells. Physiologically, it is a stimulating factor of B cells that enhances the expression of immunoglobulins (Savin et al. 2015, 2017).
Levels of CLCF-1 in the circulation of patients with recurrent FSGS are up to 100 times higher than in normal individuals (Königshausen and Sellin 2016). CLCF-1 reproduced the effects of FSGS plasma on the Palb, and it was blocked by the addition of a monoclonal antibody to CLCF-1. It is worth noting that CLCF-1 decreases the expression of nephrin by in vitro cultured podocytes (Savin et al. 2015). The activity of CLCF-1 appears to be JAK/STAT-dependent because both JAK2 and STAT3 inhibition have been shown to block the ability of CLCF-1 to increase Palb, thus highlighting the need to explore the JAK–STAT pathway relative to the pathogenesis of FSGS (Sharma et al. 2015).
Soluble urokinase receptor (suPAR)
suPAR is the soluble form of the membrane-bound urokinase plasminogen activator receptor (uPAR). uPAR is expressed on the surface of a variety of cells, including endothelial and immune cells, and participates in the regulation of cell adhesion and migration. High levels of suPAR have been described in a variety of clinical conditions, which include both systemic inflammation and malignant diseases (Smith and Marshall 2010).
At the renal level, in 2011, the group led by J. Reiser published a major study which showed that patients with recurrent FSGS in transplanted kidneys had significantly higher suPAR levels than those with MCD, healthy controls or even patients with non-recurrent FSGS (Wei et al. 2011). High suPAR levels fell after the implementation of plasmapheresis sessions. During their study, the authors established 3000 pg/mL as the cutoff value implying a high probability of diagnosing FSGS. The same authors also reported some in vivo and in vitro results which revealed that high levels of suPAR activated αvβ3 integrin in podocytes, causing the effacement of foot processes, altering podocyte adhesion to the extracellular matrix, and finally giving rise to a complete nephrotic syndrome. In addition, mice lacking uPAR (PLAUR−/−) are protected against experimental, LPS-induced proteinuria (Wei et al. 2011). More recently, it was demonstrated that the overexpression of a mouse isoform of suPAR formed a dimer in solution and required the presence of β3 integrin-Src signaling to generate proteinuria (Kopp and Heymann 2019; Wei et al. 2019).
The discovery of the involvement of suPAR in the pathogenesis of FSGS led to numerous studies which produced some conflicting results (Maas et al. 2013). Initially, the studies by Wei et al. showed that the introduction of ectopic suPAR in PLAUR−/− mice caused typical FSGS lesions and proteinuria (Wei et al. 2011), while other works did not find these effects in wild-type mice (Cathelin et al. 2014; Spinale et al. 2015; Kronbichler et al. 2016). Moreover, the overexpression of suPAR in other inflammatory diseases was not associated with proteinuria (Slot et al. 1999), suggesting that suPAR does not trigger FSGS by itself, but rather cooperates with another co-factor (the “second hit” theory) during its initial phase or the development of FSGS (Kronbichler et al. 2016; Saleem 2018).
Other contradictory studies have determined that suPAR levels were not able to distinguish FSGS patients from those with other glomerular pathologies such as MCD, membranous nephropathy (MN), IgA nephropathy, lupus nephritis, or non-chronic kidney disease (Meijers et al. 2014; Sinha et al. 2014; Kronbichler et al. 2016). This suggests that suPAR might in fact be a nonspecific marker of glomerular distress (Maas et al. 2012; Meijers et al. 2014; Sinha et al. 2014). Some studies have thus demonstrated an inverse correlation between suPAR levels and the estimated glomerular filtration rate (eGFR), probably due to impaired renal excretion rather than its function as a biomarker (Harita et al. 2014; Sinha et al. 2014; Spinale et al. 2015; Musetti et al. 2015).
On the other hand, some studies have suggested the utility of suPAR in serum to predict the recurrence of FSGS, as well as proposing its beneficial effects in post-transplant patients (Staeck et al. 2015; Schenk et al. 2017; Alachkar et al. 2018), although other studies found no correlation between serum suPAR and the post-transplant recurrence of FSGS. There have also been studies that produced conflicting results; some demonstrated a fall in suPAR levels after a remission (Morath et al. 2013; Huang et al. 2013; Alachkar et al. 2013), while others did not find any changes to serum suPAR levels (Bock et al. 2013; Sinha et al. 2014; Kitao et al. 2014). These discrepancies may have been due to the design of these epidemiological studies (most of them retrospective), the selection of controls, the collection of samples, or the statistical analyses performed. Furthermore, the overexpression of different isoforms and/or changes to their glycosylation status might have explained these divergences (Reiser 2013; Wei et al. 2019).
Apolipoprotein A-I
In African Americans, the incidence of FSGS is four to five times higher than that seen in European Americans. Friedman and colleagues found a strong correlation with variations in the gene encoding apolipoprotein A-I (APOL1) (Genovese et al. 2010; Friedman et al. 2011). The product of this gene is a secreted lipoprotein homologous to the “Bcl-2/BH3-only” family. ApoL1 circulates in the densest HDL fraction and is expressed in multiple tissue types (Page et al. 2001). Two coding variants in the APOL1 gene (named G1 and G2) are strongly associated with a risk of developing kidney disease in people of African ethnicity (Friedman et al. 2011).
Despite the fact that APOL1 has been described as a serum HDL-associated protein (Vanhollebeke and Pays 2006), its potential role as an intracellular lipid-binding protein has been suggested (Beckerman et al. 2017; Granado et al. 2017). Recently, using live-cell imaging techniques, Chun and collaborators demonstrated the different intracellular compartmentalizations of APOL1 and its variants. While wild-type APOL1 was mostly localized in lipid droplets (LDs), the G1 and G2 forms were predominantly found in the endoplasmic reticulum (ER). Importantly, these authors also showed that shifting the localization of APOL1 from the ER to LDs minimized podocyte death (Chun et al. 2019).
Another recent study reported a linkage between suPAR and variants of APOL1 (G1 and G2) (Hayek et al. 2017). The authors showed that the decrease in renal function associated with high-risk variants of APOL1 was dependent on the levels of suPAR in plasma. Moreover, suPAR, APOL1, and avβ3 integrin displayed stronger interactions on the cell surface in these APOL1 variants that were confirmed by surface plasmon resonance. This study proposed that the different APOL1 forms could act as a “second hit,” suggesting a synergistic effect of suPAR and APOL1 on the activation of integrin αvβ3 as a mechanism underlying chronic kidney disease (Hayek et al. 2017).
Autoantibodies: anti-CD40
Different models have proposed that injections of certain autoantibodies in animals could alter glomerular permeability. For example, this is the case with anti-actin, anti-adenosine triphosphate synthetase, anti-nephrin, and anti-protein tyrosine phosphatase receptor type O (Charba et al. 2009), or anti-ubiquitin carboxy-terminal hydrolase L1 (Jamin et al. 2018). In addition, Delville et al. reported in 2014 on a study that demonstrated the presence of a large number of autoantibodies in the sera of patients with recurrent FSGS. These authors succeeded in selecting ten antibodies to create a biomarker panel for the recurrence of FSGS after transplantation (Delville et al. 2014), including the anti-CD40, PTPRO, CGB5, FAS, P2RY11, SNRPB2, and APOL2 antibodies. Use of this panel had a high predictive value of recurrence, and anti-CD40 in particular was closely related to recurrent FSGS. CD40 is a member of the TNF receptor superfamily (Chatzigeorgiou et al. 2009) which plays an important role as a co-stimulator in immunity and inflammation. Like its ligand (CD40L), it is expressed in multiple tissues, particularly on the surface of antigen-presenting cells but also in the endothelium and epithelial cells (including podocytes), leading them to express chemokines, metalloproteases, uPAR, and suPAR (Wei et al. 2015). It should also be noted that the co-administration of suPAR and anti-CD40 in mice produced proteinuria that was inhibited after the blockade of integrin αvβ3. These results still need to be confirmed by other studies given their potential relevance for future clinical trials (Delville et al. 2014). The involvement of autoantibodies in the physiopathology of INS has reinforced the use of rituximab, an anti CD20 monoclonal antibody, to treat recurrent FSGS by depleting B lymphocyte levels.
Cask
Our group has detected a soluble form of CASK (calcium/calmodulin-serine protein kinase) in the sera of recurrent FSGS patients (Beaudreuil et al. 2019). CASK is a membrane-associated guanylate kinase essential for maintenance cell polarization in epithelial cells. Usually CASK is localized in the intracellular compartment, although some studies also observed the presence of CASK in the extracellular space (Yan et al. 2007).
Patients affected by FSGS that relapsed after renal transplantation were treated by immunoadsorption on protein A columns and the eluates were analyzed by mass spectroscopy. CASK was identified in eluates of patients with recurrent FSGS after transplantation but remarkably; CASK was not detectable in healthy individuals, in MCD patients, in non-FSGS-related renal-transplant patients, or in renal-transplant FSGS patients who did not exhibit recurrence after transplantation. CASK was also not found in sera from patients with significant proteinuria caused by diabetes or membranous nephropathy (Beaudreuil et al. 2019).
CASK is able to induce in vitro structural alterations in podocytes: delocalization of ZO-1 in the cell junctions, actin fiber reorganization, or synaptopodin relocation. In mice, recombinant CASK induces foot processes effacement and proteinuria. On the other hand, we and others identified CD98 as the putative CASK receptor at the surface of intestinal epithelial cells (Yan et al. 2007) and in podocytes (Beaudreuil et al. 2019). We observed that the CASK/CD98 complex triggers activation of ERK. Overall, these results suggest that CASK might participate in the recurrence of FSGS after renal transplantation. However further carefully designed studies are necessary to confirm this hypothesis, because such information could help characterize the implication of a particular environment (renal transplantation) in the pathogenesis of the disease.
The genesis of serum circulating factors: cell studies
Involvement of T cells
Since it was first postulated that SCF is an etiological factor in INS, considerable efforts have been made to unravel its true nature. In 1974, Shalhoub launched the idea that the disease originated from a T cell dysfunction resulting in the secretion of a “circulating chemical mediator toxic to an immunologically innocent glomerular basement membrane” (Shalhoub 1974). “Shalhoub’s hypothesis” tried to reconcile a number of clinical observations, such as the lack of a humoral antibody response, remissions induced by measles, the therapeutic benefits of corticosteroids, or the occurrence of this syndrome in Hodgkin’s disease. Other studies have since revealed that the injection supernatants of in vitro activated T cells or peripheral blood mononuclear cells (PBMC) from INS patients increase proteinuria in animals (Lagrue et al. 1975; Tanaka et al. 1992). Likewise, Koyama and colleagues (Koyama et al. 1991) demonstrated the presence of permeability factors in the supernatants of T cell hybridomas after the fusion of T cells from INS patients but not from healthy individuals.
Another argument in favor of the T-cell modulation of INS is based on the beneficial effects of immunosuppressive agents and particularly the use of anticalcineurins (cyclosporine A, tacrolimus) which still constitute first-line therapy for corticosteroid-resistant INS patients. A part of their immunosuppressive effect, these drugs act directly on podocytes and help to preserve their structure. In some models, permeability factors may promote the influx of calcium into podocytes via TRPC-6 (transient receptor potential channel-6), provoking the activation of calcineurin and the further dephosphorylation of synaptopodin. In this form, synaptopodin is not protected from the proteolytic action of cathepsin-L and is therefore degraded. As a consequence, the association between synaptopodin and actin, which is necessary to the stability of the actin network, is no longer ensured and proteinuria appears (Faul et al. 2008).
The roles of several cytokines have been studied in PBMC from MCD patients during relapses and remissions and by comparison with other types of non-idiopathic nephrotic syndrome. For example, IL-13, a Th2 cytokine, was significantly upregulated during a relapse in MCD patients when compared to patients in remission (van den Berg and Weening 2004; Kim et al. 2016; Colucci et al. 2018). Indeed, rats which overexpressed IL-13 exhibited significant albuminuria as well as foot process effacement in podocytes (Lai et al. 2007). Moreover, at a glomerular level, IL-13 enhanced the expression of CD80, IL-4R, and IL-13R and downregulated nephrin, podocin, and dystroglycan (Lai et al. 2007). Due to the pathogenic role of IL-13 in allergic processes, it has been suggested that there is a correlation between allergy and INS, perhaps mediated by IL-13 following the expression of CD80 in podocytes (Reiser et al. 2004).
Dantal’s group studied the Buffalo/Mna rat model which develops proteinuria at 8 weeks of age. The group observed damage at a glomerular level that was similar to that caused by FSGS. These lesions appeared to be due to abnormal T cells with a Th2 phenotype, as well as the considerable activation of macrophages (Le Berre et al. 2005). In addition, kidneys transplanted in these animals developed glomerular injury. These researchers postulated the presence of a circulating factor as being responsible for proteinuria, but it has not yet been identified (Le Berre et al. 2011).
The role of hematopoietic stem cells in the pathogenesis of INS was examined using an interesting approach. In 2007, Sellier-Leclerc and colleagues proposed an experimental INS model by injecting CD34+ stem cells from INS patients into immune-deficient mice. Following the injection, they observed that the stem cells triggered albuminuria and effacement of the foot process in podocytes. They concluded that the cells responsible for INS must likely be of immature origin rather than mature peripheral T cells (Sellier-Leclerc et al. 2007). The evolution towards FSGS in this model has not yet been studied. However, another study suggested that the impact of hematopoietic stem cells on proteinuria might be due to a general disturbance of hematopoietic cell trafficking rather than a thymus homeostasis disorder (Lapillonne et al. 2008).
Role of B cells
Traditionally, cellular studies of the etiologic mechanisms underlying nephrotic syndrome have focused on the dysregulation of T cells. Nevertheless, there is increasing evidence of an important role for B cells in this context. As described above, the beneficial use of immunoadsorption to reduce proteinuria permits the theory regarding a potential role for B cells and secreted antibodies in the pathogenesis of INS. This idea has been highlighted by the efficient use of rituximab, mainly in pediatric INS patients. Rituximab is a chimeric monoclonal anti-CD20 that depletes B cells, thus disrupting important B-cell-T-cell interactions and then inhibiting the production of autoantibodies and permeability factors. Treatment with rituximab in corticosteroid-sensitive pediatric INS patients has produced an excellent response (Cortazar et al. 2019), but its efficacy in refractory corticosteroid-resistant patients remains poorer and uncertain (Kemper et al. 2014; Sinha et al. 2015; Boumediene et al. 2018). Interestingly, Colucci et al. demonstrated that levels of memory B cells, more than other B-cell subsets, were increased in sera from corticosteroid-sensitive pediatric INS patients and seem to be pathogenically significant (Colucci et al. 2019).
Rituximab interacts with sphingomyelin phosphodiesterase acid-like 3b protein (SMPDL-3b), which regulates acid sphingomyelinase activity and then cellular activation via the generation of ceramides (Perosa et al. 2006). In addition to B cells, Fornoni and colleagues demonstrated that SMPDL-3b is also expressed in podocytes (Fornoni et al. 2011). Importantly, the binding of rituximab to SMPDL-3b in podocyte membrane rafts permits its co-localization with synaptopodin and stabilizes the actin cytoskeleton in podocytes (Fornoni et al. 2011).
Podocytes
After decades of morphological and genetic studies, a large group of gene mutations in podocyte genes (i.e., NPHS1, NPHS2, or WT1) have been associated with nephrotic syndrome (Bierzynska et al. 2015; Boyer et al. 2017; Harita 2018). These mutations determine malfunctioning of the glomerular filtration barrier, mainly through the structural disruption of podocytes. In this context, it is also conceivable that SCFs may further deteriorate the filtration barrier in glomerular diseases that already originated from different gene mutations. SCFs may therefore act not only as initial factors which damage the glomerular filtration barrier but also exacerbate an earlier pathological phenotype to generate a positive feedback loop, as described in a genetic model of FSGS (Müller-Deile et al. 2019), although this conjunction between environmental and genetic factors could only affect a fraction of patients.
On the other hand, several podocyte proteins have been suggested as contributing to or inducing INS. For example, podocyte-secreted angiopoietin-like 4 (Angtpl4) has been proposed to play a role in the development of proteinuria in MCD (Clement et al. 2011, 2014). The research group demonstrated that the in vivo podocyte expression of Angptl4 in transgenic rats induced 500 times higher levels of albuminuria, a loss of glomerular filtration membrane charge, and effacement of the foot process, whereas the transgenic expression of Angptl4 in adipose tissue increased circulating levels of Angptl4 but not proteinuria (Clement et al. 2011). These authors explained that hyposialation might be a mechanism by which Angptl4 could induce proteinuria. However, other studies have questioned the utility of Angptl4 as a biomarker for MCD. Garin’s group quantified urinary Angptl4 from patients with MCD, FSGS, and MN (membranous nephropathy) who were either in relapse or remission. They observed high levels of Angptl4 in the urine which were probably associated with different types of nephrotic proteinuria but not with a specific disease (Cara-Fuentes et al. 2017).
In 2010, Sahali’s group identified abnormal expression of the c-mip gene (c-maf inducing protein) in podocytes from patients with INS, including MCD, some subsets of FSGS and MN (Zhang et al. 2010; Sendeyo et al. 2013).These authors also reported an overexpression of c-mip in T cells and podocytes in relapsing INS patients but not in healthy individuals. In addition, the overexpression of c-mip in transgenic mice induced massive proteinuria. C-mip switches off podocyte signaling by precluding the interaction of nephrin with Fyn and thereby inhibiting nephrin phosphorylation. In addition, c-mip hinders interactions between Nck and nephrin and between Fyn and N-WASP, leading to cytoskeletal disorganization and podocyte foot process effacement (Zhang et al. 2010).
On the other hand, the overexpression of c-mip has been observed in some malignancies such as Hodgkin’s lymphoma. In that context, c-mip was upregulated in Reed-Sternberg cells and associated with the MCD which appeared in some patients (Audard et al. 2010). More recently, there has been a report of a case of paraneoplastic nephrotic syndrome during the course of small cell lung carcinoma. Carboplatin-etoposide therapy procured tumor remission and resolved the associated nephrotic syndrome. It should be noted that the serum samples collected prior to treatment induced podocyte disorganization, whereas those collected after the remission did not. The authors concluded that the expression of c-mip might be related to the presence of a serum circulating factor (Bouatou et al. 2017).
Discussion and future directions
During the past five or so decades, scientists working in the field of nephrology have been making intense efforts to identify the mechanisms underlying glomerular permeability. The identification of a serum circulating permeability factor as the causal agent of INS is a challenge that has often been referred to as the “Holy Grail” of nephrologists. Thanks to the major advances achieved in recent years, and particularly the discovery of new permeability factors (suPAR, anti-CD40, CASK), initial ideas concerning the existence of a single molecule as being etiologically responsible have become obsolete. The Columbia classification, in itself, denotes considerable histological heterogeneity that already evoked the presence of distinct processes at the origin of the disorder. Because of our increasing knowledge of SCFs, it is now logical to admit that INS should rather be seen as a cluster of numerous and poorly characterized nephrotic syndromes. In other words, INS is at present conceived as a “hodgepodge” that contains countless nosological entities that we cannot yet understand.
Recent discoveries have suggested that coexistence of different SCFs (i.e., suPAR-APOL1 and other stressors) is required to explain their pathogenicity. This may explain why some patients do not develop the disease in the presence of a single and innocuous SCF, but after it encounters another SCF (or stress situation), it becomes pathologically active. This may be the case of CASK, a potential glomerular permeability factor that has been recently found in a particular environment (renal transplantation). Following a similar philosophy, it is tempting to speculate that some genetic dysfunctions in podocytes that were not self-deleting themselves may be very damaging in the presence of other additional SCFs.
Another interesting concept is that proteinuria acts as a “hit” on its own: “proteinuria triggers proteinuria”, thus adding greater pathogenic complexity. It is possible to conceive that, after a given stress, the resulting proteinuria may generate the appearance of SCFs and then more proteinuria, triggering a vicious positive feedback circle. All these different stimuli (or “hits”) may occur over time either simultaneously or consecutively, resulting in a kind of “molecular ballet” where the start corresponds to MCD, followed or not by FSGS, and the curtain drops at end-stage renal disease. Overall, the presence or absence of different stimuli, related to different circulating factors (deleterious or protective), must be considered as a reality that is necessary to find a broader vision and determine better therapeutic strategies for INS.
Abbreviations
- SCF:
-
Serum circulating factor
- INS:
-
Idiopathic nephrotic syndrome
- FSGS:
-
Focal segmental glomerulosclerosis
- rFSGS:
-
Recurrent focal segmental glomerulosclerosis
- MCD:
-
Minimal change disease
- CLC-1:
-
Cardiotrophin-like cytokine-1
- suPAR:
-
Soluble urokinase plasminogen activator receptor
- APOL1:
-
Apolipoprotein A-I
References
Alachkar N, Wei C, Arend LJ et al (2013) Podocyte effacement closely links to suPAR levels at time of posttransplantation focal segmental glomerulosclerosis occurrence and improves with therapy. Transplantation 96:649–656. https://doi.org/10.1097/TP.0b013e31829eda4f
Alachkar N, Li J, Matar D et al (2018) Monitoring suPAR levels in post-kidney transplant focal segmental glomerulosclerosis treated with therapeutic plasma exchange and rituximab. BMC Nephrol:19. https://doi.org/10.1186/s12882-018-1177-x
Artero ML, Sharma R, Savin VJ, Vincenti F (1994) Plasmapheresis reduces proteinuria and serum capacity to injure glomeruli in patients with recurrent focal glomerulosclerosis. Am J Kidney Dis Off J Natl Kidney Found 23:574–581
Ashworth CT, James JA (1961) Glomerular excretion of macromolecular substances. Electron microscopic study of rat kidney after administration of human serum albumin. Am J Pathol 39:307–316
Audard V, Zhang S, Copie-Bergman C et al (2010) Occurrence of minimal change nephrotic syndrome in classical Hodgkin lymphoma is closely related to the induction of c-mip in Hodgkin-reed Sternberg cells and podocytes. Blood 115:3756–3762. https://doi.org/10.1182/blood-2009-11-251132
Bakker WW, Borghuis T, Harmsen MC et al (2005a) Protease activity of plasma hemopexin. Kidney Int 68:603–610. https://doi.org/10.1111/j.1523-1755.2005.00438.x
Bakker WW, van Dael CML, Pierik LJWM et al (2005b) Altered activity of plasma hemopexin in patients with minimal change disease in relapse. Pediatr Nephrol Berl Ger 20:1410–1415. https://doi.org/10.1007/s00467-005-1936-3
Barisoni L, Schnaper HW, Kopp JB (2007) A proposed taxonomy for the podocytopathies: a reassessment of the primary nephrotic diseases. Clin J Am Soc Nephrol CJASN 2:529–542. https://doi.org/10.2215/CJN.04121206
Beaudreuil S, Zhang X, Herr F et al (2019) Circulating CASK is associated with recurrent focal segmental glomerulosclerosis after transplantation. PLoS One 14:e0219353. https://doi.org/10.1371/journal.pone.0219353
Beckerman P, Bi-Karchin J, Park ASD et al (2017) Transgenic expression of human APOL1 risk variants in podocytes induces kidney disease in mice. Nat Med 23:429–438. https://doi.org/10.1038/nm.4287
Bertelli R, Bonanni A, Caridi G et al (2018) Molecular and cellular mechanisms for proteinuria in minimal change disease. Front Med 5:170. https://doi.org/10.3389/fmed.2018.00170
Bierzynska A, Soderquest K, Koziell A (2015) Genes and Podocytes-new insights into mechanisms of Podocytopathy. Front Endocrinol 5. https://doi.org/10.3389/fendo.2014.00226
Bock ME, Price HE, Gallon L, Langman CB (2013) Serum soluble Urokinase-type plasminogen activator receptor levels and idiopathic FSGS in children: a single-center report. Clin J Am Soc Nephrol 8:1304–1311. https://doi.org/10.2215/CJN.07680712
Bouatou Y, Koessler T, Oniszczuk J et al (2017) Nephrotic syndrome in small cell lung Cancer and induction of C-Mip in Podocytes. Am J Kidney Dis Off J Natl Kidney Found 69:477–480. https://doi.org/10.1053/j.ajkd.2016.09.026
Boumediene A, Vachin P, Sendeyo K et al (2018) NEPHRUTIX: a randomized, double-blind, placebo vs rituximab-controlled trial assessing T-cell subset changes in minimal change Nephrotic syndrome. J Autoimmun 88:91–102. https://doi.org/10.1016/j.jaut.2017.10.006
Boyer O, Dorval G, Servais A (2017) Hereditary podocytopathies in adults: the next generation. Kidney Dis 3:50–56. https://doi.org/10.1159/000477243
Canaud G, Dion D, Zuber J et al (2010) Recurrence of nephrotic syndrome after transplantation in a mixed population of children and adults: course of glomerular lesions and value of the Columbia classification of histological variants of focal and segmental glomerulosclerosis (FSGS). Nephrol Dial Transplant 25:1321–1328. https://doi.org/10.1093/ndt/gfp500
Cara-Fuentes G, Segarra A, Silva-Sanchez C et al (2017) Angiopoietin-like-4 and minimal change disease. PLoS One 12:e0176198. https://doi.org/10.1371/journal.pone.0176198
Cathelin D, Placier S, Ploug M et al (2014) Administration of recombinant soluble urokinase receptor per se is not sufficient to induce podocyte alterations and proteinuria in mice. J Am Soc Nephrol JASN 25:1662–1668. https://doi.org/10.1681/ASN.2013040425
Charba DS, Wiggins RC, Goyal M et al (2009) Antibodies to protein tyrosine phosphatase receptor type O (PTPro) increase glomerular albumin permeability (P(alb)). Am J Physiol Ren Physiol 297:F138–F144. https://doi.org/10.1152/ajprenal.00122.2008
Chatzigeorgiou A, Lyberi M, Chatzilymperis G et al (2009) CD40/CD40L signaling and its implication in health and disease. BioFactors Oxf Engl 35:474–483. https://doi.org/10.1002/biof.62
Cheung PK, Klok PA, Baller JF, Bakker WW (2000) Induction of experimental proteinuria in vivo following infusion of human plasma hemopexin. Kidney Int 57:1512–1520. https://doi.org/10.1046/j.1523-1755.2000.00996.x
Christensen EI, Verroust PJ, Nielsen R (2009) Receptor-mediated endocytosis in renal proximal tubule. Pflugers Arch 458:1039–1048. https://doi.org/10.1007/s00424-009-0685-8
Chun J, Zhang J-Y, Wilkins MS et al (2019) Recruitment of APOL1 kidney disease risk variants to lipid droplets attenuates cell toxicity. Proc Natl Acad Sci 116:3712–3721. https://doi.org/10.1073/pnas.1820414116
Clement LC, Avila-Casado C, Macé C et al (2011) Podocyte-secreted angiopoietin-like-4 mediates proteinuria in glucocorticoid-sensitive nephrotic syndrome. Nat Med 17:117–122. https://doi.org/10.1038/nm.2261
Clement LC, Macé C, Avila-Casado C et al (2014) Circulating angiopoietin-like 4 links proteinuria with hypertriglyceridemia in nephrotic syndrome. Nat Med 20:37–46. https://doi.org/10.1038/nm.3396
Colucci M, Corpetti G, Emma F, Vivarelli M (2018) Immunology of idiopathic nephrotic syndrome. Pediatr Nephrol Berl Ger 33:573–584. https://doi.org/10.1007/s00467-017-3677-5
Colucci M, Carsetti R, Cascioli S et al (2019) B cell phenotype in pediatric idiopathic nephrotic syndrome. Pediatr Nephrol Berl Ger 34:177–181. https://doi.org/10.1007/s00467-018-4095-z
Cortazar FB, Rosenthal J, Laliberte K, Niles JL (2019) Continuous B-cell depletion in frequently relapsing, steroid-dependent and steroid-resistant nephrotic syndrome. Clin Kidney J 12:224–231. https://doi.org/10.1093/ckj/sfy067
D’Agati VD, Kaskel FJ, Falk RJ (2011) Focal segmental glomerulosclerosis. N Engl J Med 365:2398–2411. https://doi.org/10.1056/NEJMra1106556
Dantal J, Testa A, Bigot E, Soulillou JP (1992) Effects of plasma-protein a immunoadsorption on idiopathic nephrotic syndrome recurring after renal transplantation. Ann Med Interne (Paris) 143(Suppl 1):48–51
De S, Kuwahara S, Saito A (2014) The endocytic receptor megalin and its associated proteins in proximal tubule epithelial cells. Membranes 4:333–355. https://doi.org/10.3390/membranes4030333
Delville M, Sigdel TK, Wei C et al (2014) A circulating antibody panel for pretransplant prediction of FSGS recurrence after kidney transplantation. Sci Transl Med 6:256ra136. https://doi.org/10.1126/scitranslmed.3008538
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet Lond Engl 362:629–639. https://doi.org/10.1016/S0140-6736(03)14184-0
Farquhar MG, Palade GE (1962) Functional evidence for the existence of a third cell type in the renal glomerulus: phagocytosis of filtration residues by a distinctive “third” cell. J Cell Biol 13:55–87. https://doi.org/10.1083/jcb.13.1.55
Faul C, Donnelly M, Merscher-Gomez S et al (2008) The actin cytoskeleton of kidney podocytes is a direct target of the antiproteinuric effect of cyclosporine a. Nat Med 14:931–938. https://doi.org/10.1038/nm.1857
Feld SM, Figueroa P, Savin V et al (1998) Plasmapheresis in the treatment of steroid-resistant focal segmental glomerulosclerosis in native kidneys. Am J Kidney Dis Off J Natl Kidney Found 32:230–237
Fogo AB (2015) Causes and pathogenesis of focal segmental glomerulosclerosis. Nat Rev Nephrol 11:76–87. https://doi.org/10.1038/nrneph.2014.216
Fogo AB, Lusco MA, Najafian B, Alpers CE (2015) AJKD atlas of renal pathology: minimal change disease. Am J Kidney Dis Off J Natl Kidney Found 66:376–377. https://doi.org/10.1053/j.ajkd.2015.04.006
Fornoni A, Sageshima J, Wei C et al (2011) Rituximab targets podocytes in recurrent focal segmental glomerulosclerosis. Sci Transl Med 3:85ra46. https://doi.org/10.1126/scitranslmed.3002231
Friedman DJ, Kozlitina J, Genovese G et al (2011) Population-based risk assessment of APOL1 on renal disease. J Am Soc Nephrol JASN 22:2098–2105. https://doi.org/10.1681/ASN.2011050519
Gallon L, Leventhal J, Skaro A et al (2012) Resolution of recurrent focal segmental glomerulosclerosis after retransplantation. N Engl J Med 366:1648–1649. https://doi.org/10.1056/NEJMc1202500
Garin EH, Mu W, Arthur JM et al (2010) Urinary CD80 is elevated in minimal change disease but not in focal segmental glomerulosclerosis. Kidney Int 78:296–302. https://doi.org/10.1038/ki.2010.143
Genovese G, Friedman DJ, Ross MD et al (2010) Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 329:841–845. https://doi.org/10.1126/science.1193032
Gentili A, Tangheroni W, Gelli G (1954) Proteinuria caused by transfusion of blood from nephrotic to non-nephrotic individuals. Minerva Med 45:603–608
Gianesello L, Priante G, Ceol M et al (2017) Albumin uptake in human podocytes: a possible role for the cubilin-amnionless (CUBAM) complex. Sci Rep 7. https://doi.org/10.1038/s41598-017-13789-z
Gonçalves GL, Costa-Pessoa JM, Thieme K et al (2018) Intracellular albumin overload elicits endoplasmic reticulum stress and PKC-delta/p38 MAPK pathway activation to induce podocyte apoptosis. Sci Rep 8:18012. https://doi.org/10.1038/s41598-018-36933-9
Granado D, Müller D, Krausel V et al (2017) Intracellular APOL1 risk variants cause cytotoxicity accompanied by energy depletion. J Am Soc Nephrol JASN 28:3227–3238. https://doi.org/10.1681/ASN.2016111220
Han M-H, Kim Y-J (2016) Practical application of Columbia classification for focal segmental Glomerulosclerosis. Biomed Res Int 2016:9375753. https://doi.org/10.1155/2016/9375753
Harita Y (2018) Application of next-generation sequencing technology to diagnosis and treatment of focal segmental glomerulosclerosis. Clin Exp Nephrol 22:491–500. https://doi.org/10.1007/s10157-017-1449-y
Harita Y, Ishizuka K, Tanego A et al (2014) Decreased glomerular filtration as the primary factor of elevated circulating suPAR levels in focal segmental glomerulosclerosis. Pediatr Nephrol Berl Ger 29:1553–1560. https://doi.org/10.1007/s00467-014-2808-5
Hayek SS, Koh KH, Grams ME et al (2017) A tripartite complex of suPAR, APOL1 risk variants and αvβ3 integrin on podocytes mediates chronic kidney disease. Nat Med 23:945–953. https://doi.org/10.1038/nm.4362
Hoyer JR, Vernier RL, Najarian JS et al (1972) Recurrence of idiopathic nephrotic syndrome after renal transplantation. Lancet Lond Engl 2:343–348. https://doi.org/10.1016/s0140-6736(72)91734-5
Huang J, Liu G, Zhang Y-M et al (2013) Plasma soluble urokinase receptor levels are increased but do not distinguish primary from secondary focal segmental glomerulosclerosis. Kidney Int 84:366–372. https://doi.org/10.1038/ki.2013.55
Jamin A, Berthelot L, Couderc A et al (2018) Autoantibodies against podocytic UCHL1 are associated with idiopathic nephrotic syndrome relapses and induce proteinuria in mice. J Autoimmun 89:149–161. https://doi.org/10.1016/j.jaut.2017.12.014
Jarad G, Knutsen RH, Mecham RP, Miner JH (2016) Albumin contributes to kidney disease progression in Alport syndrome. Am J Physiol Ren Physiol 311:F120–F130. https://doi.org/10.1152/ajprenal.00456.2015
Kaverina NV, Eng DG, Freedman BS et al (2019) Dual lineage tracing shows that glomerular parietal epithelial cells can transdifferentiate toward the adult podocyte fate. Kidney Int 96:597–611. https://doi.org/10.1016/j.kint.2019.03.014
Kemper MJ, Wolf G, Müller-Wiefel DE (2001) Transmission of glomerular permeability factor from a mother to her child. N Engl J Med 344:386–387. https://doi.org/10.1056/NEJM200102013440517
Kemper MJ, Lehnhardt A, Zawischa A, Oh J (2014) Is rituximab effective in childhood nephrotic syndrome? Yes and no. Pediatr Nephrol Berl Ger 29:1305–1311. https://doi.org/10.1007/s00467-013-2529-1
Kim SH, Park SJ, Han KH et al (2016) Pathogenesis of minimal change nephrotic syndrome: an immunological concept. Korean J Pediatr 59:205–211. https://doi.org/10.3345/kjp.2016.59.5.205
Kitao T, Kimata T, Kanda E et al (2014) Soluble urokinase receptor in a toddler with focal segmental glomerulosclerosis. Kidney Int 86:208. https://doi.org/10.1038/ki.2014.135
Königshausen E, Sellin L (2016) Circulating permeability factors in primary focal segmental Glomerulosclerosis: a review of proposed candidates. Biomed Res Int 2016:3765608. https://doi.org/10.1155/2016/3765608
Kopp JB, Heymann J (2019) C-Src is in the effector pathway linking uPAR and podocyte injury. J Clin Invest 129:1827–1829. https://doi.org/10.1172/JCI127927
Koyama A, Fujisaki M, Kobayashi M et al (1991) A glomerular permeability factor produced by human T cell hybridomas. Kidney Int 40:453–460
Kronbichler A, Saleem MA, Meijers B, Shin JI (2016) Soluble Urokinase receptors in focal segmental Glomerulosclerosis: a review on the scientific point of view. J Immunol Res 2016:1–14. https://doi.org/10.1155/2016/2068691
Lagrue G, Xheneumont S, Branellec A et al (1975) A vascular permeability factor elaborated from lymphocytes. I. Demonstration in patients with nephrotic syndrome. Biomed Publiee Pour AAICIG 23:37–40
Lagrue G, Branellec A, Niaudet P et al (1991) Transmission of nephrotic syndrome to two neonates. Spontaneous regression. Presse Medicale Paris Fr 1983 20:255–257
Lai K-W, Wei C-L, Tan L-K et al (2007) Overexpression of interleukin-13 induces minimal-change-like nephropathy in rats. J Am Soc Nephrol JASN 18:1476–1485. https://doi.org/10.1681/ASN.2006070710
Lapillonne H, Leclerc A, Ulinski T et al (2008) Stem cell mobilization in idiopathic steroid-sensitive nephrotic syndrome. Pediatr Nephrol Berl Ger 23:1251–1256. https://doi.org/10.1007/s00467-008-0793-2
Le Berre L, Hervé C, Buzelin F et al (2005) Renal macrophage activation and Th2 polarization precedes the development of nephrotic syndrome in Buffalo/Mna rats. Kidney Int 68:2079–2090. https://doi.org/10.1111/j.1523-1755.2005.00664.x
Le Berre L, Bruneau S, Renaudin K et al (2011) Development of initial idiopathic nephrotic syndrome and post-transplantation recurrence: evidence of the same biological entity. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc 26:1523–1532. https://doi.org/10.1093/ndt/gfq597
Lennon R, Singh A, Welsh GI et al (2008) Hemopexin induces nephrin-dependent reorganization of the actin cytoskeleton in podocytes. J Am Soc Nephrol JASN 19:2140–2149. https://doi.org/10.1681/ASN.2007080940
Maas RJH, Wetzels JFM, Deegens JKJ (2012) Serum-soluble urokinase receptor concentration in primary FSGS. Kidney Int 81:1043–1044. https://doi.org/10.1038/ki.2012.32
Maas RJH, Deegens JKJ, Wetzels JFM (2013) Serum suPAR in patients with FSGS: trash or treasure? Pediatr Nephrol Berl Ger 28:1041–1048. https://doi.org/10.1007/s00467-013-2452-5
Maas RJ, Deegens JK, Smeets B et al (2016) Minimal change disease and idiopathic FSGS: manifestations of the same disease. Nat Rev Nephrol 12:768–776. https://doi.org/10.1038/nrneph.2016.147
McCarthy ET, Sharma M, Savin VJ (2010) Circulating permeability factors in idiopathic nephrotic syndrome and focal segmental glomerulosclerosis. Clin J Am Soc Nephrol CJASN 5:2115–2121. https://doi.org/10.2215/CJN.03800609
Meijers B, Maas RJH, Sprangers B et al (2014) The soluble urokinase receptor is not a clinical marker for focal segmental glomerulosclerosis. Kidney Int 85:636–640. https://doi.org/10.1038/ki.2013.505
Morath C, Wei C, Macher-Goeppinger S et al (2013) Management of severe recurrent focal segmental glomerulosclerosis through circulating soluble urokinase receptor modification. Am J Ther 20:226–229. https://doi.org/10.1097/MJT.0b013e3182811aca
Morigi M, Buelli S, Angioletti S et al (2005) In response to protein load podocytes reorganize cytoskeleton and modulate endothelin-1 gene: implication for permselective dysfunction of chronic nephropathies. Am J Pathol 166:1309–1320. https://doi.org/10.1016/S0002-9440(10)62350-4
Müller-Deile J, Schenk H, Schroder P et al (2019) Circulating factors cause proteinuria in parabiotic zebrafish. Kidney Int. https://doi.org/10.1016/j.kint.2019.02.013
Musetti C, Quaglia M, Cena T et al (2015) Circulating suPAR levels are affected by glomerular filtration rate and proteinuria in primary and secondary glomerulonephritis. J Nephrol 28:299–305. https://doi.org/10.1007/s40620-014-0137-1
Okamura K, Dummer P, Kopp J et al (2013) Endocytosis of albumin by Podocytes elicits an inflammatory response and induces apoptotic cell death. PLoS One 8:e54817. https://doi.org/10.1371/journal.pone.0054817
Page NM, Butlin DJ, Lomthaisong K, Lowry PJ (2001) The human apolipoprotein L gene cluster: identification, classification, and sites of distribution. Genomics 74:71–78. https://doi.org/10.1006/geno.2001.6534
Pal A, Kaskel F (2016) History of Nephrotic syndrome and evolution of its treatment. Front Pediatr 4. https://doi.org/10.3389/fped.2016.00056
Perosa F, Favoino E, Caragnano MA, Dammacco F (2006) Generation of biologically active linear and cyclic peptides has revealed a unique fine specificity of rituximab and its possible cross-reactivity with acid sphingomyelinase-like phosphodiesterase 3b precursor. Blood 107:1070–1077. https://doi.org/10.1182/blood-2005-04-1769
Puelles VG, Cullen-McEwen LA, Taylor GE et al (2016) Human podocyte depletion in association with older age and hypertension. Am J Physiol Ren Physiol 310:F656–F668. https://doi.org/10.1152/ajprenal.00497.2015
Ramezani A, Devaney JM, Cohen S et al (2015) Circulating and urinary microRNA profile in focal segmental glomerulosclerosis: a pilot study. Eur J Clin Investig 45:394–404. https://doi.org/10.1111/eci.12420
Reiser J (2013) Circulating permeability factor suPAR: from concept to discovery to clinic. Trans Am Clin Climatol Assoc 124:133–138
Reiser J, von Gersdorff G, Loos M et al (2004) Induction of B7-1 in podocytes is associated with nephrotic syndrome. J Clin Invest 113:1390–1397. https://doi.org/10.1172/JCI20402
Rosenberg AZ, Kopp JB (2017) Focal Segmental Glomerulosclerosis. Clin J Am Soc Nephrol CJASN 12:502–517. https://doi.org/10.2215/CJN.05960616
Rudnicki M (2016) FSGS recurrence in adults after renal transplantation. Biomed Res Int 2016:1–7. https://doi.org/10.1155/2016/3295618
Saleem MA (2018) What is the role of soluble Urokinase-type plasminogen activator in renal disease? Nephron 139:334–341. https://doi.org/10.1159/000490118
Savin VJ, McCarthy ET, Sharma R et al (2008) Galactose binds to focal segmental glomerulosclerosis permeability factor and inhibits its activity. Transl Res J Lab Clin Med 151:288–292. https://doi.org/10.1016/j.trsl.2008.04.001
Savin VJ, Sharma M, Zhou J et al (2015) Renal and hematological effects of CLCF-1, a B-cell-stimulating cytokine of the IL-6 family. J Immunol Res 2015:714964. https://doi.org/10.1155/2015/714964
Savin VJ, Sharma M, Zhou J et al (2017) Multiple targets for novel therapy of FSGS associated with circulating permeability factor. Biomed Res Int 2017:6232616. https://doi.org/10.1155/2017/6232616
Schenk H, Müller-Deile J, Schmitt R et al (2017) Removal of focal segmental glomerulosclerosis (FSGS) factor suPAR using CytoSorb. J Clin Apher 32:444–452. https://doi.org/10.1002/jca.21538
Sellier-Leclerc A-L, Duval A, Riveron S et al (2007) A humanized mouse model of idiopathic nephrotic syndrome suggests a pathogenic role for immature cells. J Am Soc Nephrol JASN 18:2732–2739. https://doi.org/10.1681/ASN.2006121346
Sendeyo K, Audard V, Zhang S et al (2013) Upregulation of c-mip is closely related to podocyte dysfunction in membranous nephropathy. Kidney Int 83:414–425. https://doi.org/10.1038/ki.2012.426
Sgambat K, Banks M, Moudgil A (2013) Effect of galactose on glomerular permeability and proteinuria in steroid-resistant nephrotic syndrome. Pediatr Nephrol Berl Ger 28:2131–2135. https://doi.org/10.1007/s00467-013-2539-z
Shalhoub RJ (1974) Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet Lond Engl 2:556–560. https://doi.org/10.1016/s0140-6736(74)91880-7
Sharma M, Zhou J, Gauchat J-F et al (2015) Janus kinase 2/signal transducer and activator of transcription 3 inhibitors attenuate the effect of cardiotrophin-like cytokine factor 1 and human focal segmental glomerulosclerosis serum on glomerular filtration barrier. Transl Res J Lab Clin Med 166:384–398. https://doi.org/10.1016/j.trsl.2015.03.002
Sinha A, Bajpai J, Saini S et al (2014) Serum-soluble urokinase receptor levels do not distinguish focal segmental glomerulosclerosis from other causes of nephrotic syndrome in children. Kidney Int 85:649–658. https://doi.org/10.1038/ki.2013.546
Sinha A, Bhatia D, Gulati A et al (2015) Efficacy and safety of rituximab in children with difficult-to-treat nephrotic syndrome. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc 30:96–106. https://doi.org/10.1093/ndt/gfu267
Slot O, Brünner N, Locht H et al (1999) Soluble urokinase plasminogen activator receptor in plasma of patients with inflammatory rheumatic disorders: increased concentrations in rheumatoid arthritis. Ann Rheum Dis 58:488–492. https://doi.org/10.1136/ard.58.8.488
Smeets B, Kuppe C, Sicking E-M et al (2011) Parietal epithelial cells participate in the formation of sclerotic lesions in focal segmental glomerulosclerosis. J Am Soc Nephrol JASN 22:1262–1274. https://doi.org/10.1681/ASN.2010090970
Smith HW, Marshall CJ (2010) Regulation of cell signalling by uPAR. Nat Rev Mol Cell Biol 11:23–36. https://doi.org/10.1038/nrm2821
Spinale JM, Mariani LH, Kapoor S et al (2015) A reassessment of soluble urokinase-type plasminogen activator receptor in glomerular disease. Kidney Int 87:564–574. https://doi.org/10.1038/ki.2014.346
Staeck O, Slowinski T, Lieker I et al (2015) Recurrent primary focal segmental Glomerulosclerosis managed with intensified plasma exchange and concomitant monitoring of soluble Urokinase-type plasminogen activator receptor-mediated Podocyte β3-integrin activation. Transplantation 99:2593–2597. https://doi.org/10.1097/TP.0000000000000914
Tanaka R, Yoshikawa N, Nakamura H, Ito H (1992) Infusion of peripheral blood mononuclear cell products from nephrotic children increases albuminuria in rats. Nephron 60:35–41. https://doi.org/10.1159/000186702
Tojo A, Onozato ML, Kitiyakara C et al (2008) Glomerular albumin filtration through podocyte cell body in puromycin aminonucleoside nephrotic rat. Med Mol Morphol 41:92–98. https://doi.org/10.1007/s00795-008-0397-8
Trachtman H, Vento S, Herreshoff E et al (2015) Efficacy of galactose and adalimumab in patients with resistant focal segmental glomerulosclerosis: report of the font clinical trial group. BMC Nephrol 16:111. https://doi.org/10.1186/s12882-015-0094-5
van den Berg JG, Weening JJ (2004) Role of the immune system in the pathogenesis of idiopathic nephrotic syndrome. Clin Sci Lond Engl 1979 107:125–136. https://doi.org/10.1042/CS20040095
Vanhollebeke B, Pays E (2006) The function of apolipoproteins L. Cell Mol Life Sci CMLS 63:1937–1944. https://doi.org/10.1007/s00018-006-6091-x
Wei C, El Hindi S, Li J et al (2011) Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nat Med 17:952–960. https://doi.org/10.1038/nm.2411
Wei C, Sigdel TK, Sarwal MM, Reiser J (2015) Circulating CD40 autoantibody and suPAR synergy drives glomerular injury. Ann Transl Med 3:300. https://doi.org/10.3978/j.issn.2305-5839.2015.11.08
Wei C, Li J, Adair BD et al (2019) uPAR isoform 2 forms a dimer and induces severe kidney disease in mice. J Clin Invest 129:1946–1959. https://doi.org/10.1172/JCI124793
Yan Y, Vasudevan S, Nguyen H et al (2007) Extracellular interaction between hCD98 and the PDZ class II domain of hCASK in intestinal epithelia. J Membr Biol 215:15–26. https://doi.org/10.1007/s00232-007-9001-8
Yoshikawa N, Ito H, Akamatsu R et al (1986) Glomerular podocyte vacuolation in focal segmental glomerulosclerosis. Arch Pathol Lab Med 110:394–398
Zhang SY, Kamal M, Dahan K et al (2010) C-mip impairs Podocyte proximal signaling and induces heavy proteinuria. Sci Signal 3:ra39–ra39. https://doi.org/10.1126/scisignal.2000678
Zimmerman SW (1984) Increased urinary protein excretion in the rat produced by serum from a patient with recurrent focal glomerular sclerosis after renal transplantation. Clin Nephrol 22:32–38
Funding
Hans K. Lorenzo was supported by the “ Fondation du Rein”/“Fondation pour la Recherche Médicale”, grant number R16099LL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Candelier, JJ., Lorenzo, HK. Idiopathic nephrotic syndrome and serum permeability factors: a molecular jigsaw puzzle. Cell Tissue Res 379, 231–243 (2020). https://doi.org/10.1007/s00441-019-03147-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-019-03147-y