Abstract
It is largely believed that after undergoing differentiation, adipocytes can no longer divide. Yet, using ceiling culture, it was demonstrated in vitro that some adipocytes are able to regain proliferative abilities by becoming fibroblast-like cells called dedifferentiated adipocytes. Mature adipocytes are abundant, can be easily isolated, and represent a homogenous cell population. Because of these advantageous characteristics, dedifferentiated adipocytes are clinically attractive in tissue engineering as a potential treatment resource for conditions such as type 2 diabetes, cardiac and kidney diseases, as well as autoimmune diseases. The aim of this review article is to summarize current knowledge on adipocyte dedifferentiation by accurately describing dedifferentiated adipocyte characteristics such as morphological appearance, gene expression, antigen signature, pluripotency, and functionality. Current hypotheses possibly explaining the biological mechanisms and cellular reprogramming of the dedifferentiation process are summarized. Dedifferentiated adipocytes show a stem cell-like antigen profile and genome signature which add to their proliferative capacities and their ability to re-differentiate into diverse cell lineages. The dedifferentiation process likely involves liposecretion, that is, the rapid secretion of the cell’s lipid droplet. Dedifferentiated adipocytes may allow development of new uses in tissue engineering.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During embryogenesis, cells undergo many epigenetic changes that coincide with their differentiation and specialization. This process confers specific morphological characteristics and, once completed, differentiated cells acquire functionality (Ntambi and Young-Cheul 2000; Paksa 2017). Differentiation has been considered a unidirectional process until the last decades of the twentieth century, where in vivo dedifferentiation was observed in plant regeneration (Steevens and Sussex 1989). Once the milestone describing dedifferentiation was reached, other groups found incidences of dedifferentiation in vertebrae. One convincing example was observed in the zebrafish. In a well-designed study, Knopf et al. examined the dedifferentiation of osteoblasts in zebrafish fin following amputation using a transgenic reporter and genetic lineage tracing approach (Knopf et al. 2011).
Although regenerative processes have been observed in other kingdoms, they are limited or nonexistent in mammals. Evidence in the literature mostly suggests an association between dedifferentiation and tissue dysfunctions. For example, in humans, testicular dysgenesis syndrome has been associated with the presence of immature Sertoli cells (playing an important role in spermatogenesis), suggesting a process of dedifferentiation (Abrahan et al. 2009; Nistal et al. 2013). Type 2 diabetes (T2D) has also been associated to dedifferentiation in both humans and rodent models. In 2012, Talchai et al. examined the mechanisms underlying its development in mice lacking FoxO1 in β-cells. Lineage-tracing experiments demonstrated a loss of β-cell mass due to dedifferentiation (Talchai et al. 2012). Wang and colleagues obtained similar results using a insulin secretion deficiency mouse model (Wang et al. 2014). Other studies have been conducted in vitro to elucidate potential mechanisms underlying T2D. Neelankal et al. cultivated murine pancreatic β insulinoma six cell line (MIN6) under high-glucose conditions mimicking those found in diabetes in vivo (Neelankal et al. 2017). Under these conditions, MIN6 cells dedifferentiated, showing some features and neuroendocrine markers of β-cell precursors. These findings are consistent with the notion that T2D might involve β-cell dedifferentiation instead of cell death (Neelankal et al. 2017). Recently, a study conducted in humans replicated what animal studies seemed to suggest: T2D may involve β-cell dedifferentiation. When diabetic and nondiabetic pancreases were compared, the percentage of insulin-negative/synaptophysin-positive cells was greater in diabetes, indicating that dedifferentiated β-cells were more prevalent (Cinti et al. 2016). These studies suggest that, although mostly associated with pathological conditions, dedifferentiation exists in a certain number of mammalian cell types such as pancreatic β-cell and Sertoli cells.
As opposed to many others cells types, it is largely believed that once differentiated, mature adipocytes can no longer divide (Spalding et al. 2008). Yet, it is difficult to find references clearly supporting this claim (Ntambi and Young-Cheul 2000; Spalding et al. 2008). Due to their high lipid content preventing cell culture for long periods of time, the biological and cellular processes of cell division are difficult to study in adipocytes. Fortunately, in 1986, Sugihara et al., taking advantage of adipocyte buoyancy in aqueous medium, created a culture system to study the biology of mature, unilocular white adipocytes isolated from whole adipose tissue. This system was named “ceiling culture,” and it was used to demonstrate that in vitro, some adipocytes could apparently divide and proliferate (Sugihara et al. 1986). More recently, a number of research groups have found evidence suggesting that adipocyte dedifferentiation may take place in vivo. Using a triple recombinant mouse model, a study showed that increasing the expression of Notch in mature adipocytes led them to dedifferentiate and were found in newly developed dedifferentiated liposarcoma (Bi et al. 2016). However, the most striking finding was made by Wang and colleagues (Wang et al. 2018). With the particular mouse model used, called AdipoChaser, the group was able to induce a permanent label of mature adipocytes through the administration of doxycycline, which allows tracking of mature adipocytes and their distinction from adipocytes generated by adipogenesis. Their results demonstrate that secreting epithelial cells in the mammary gland do not originate from adipocyte transdifferentiation but rather that tracked adipocytes dedifferentiate into fibroblast-like cells during lactation. The opposite process was observed during weaning, where marked dedifferentiated adipocytes rapidly redifferentiate during the involution of the mammary gland (Wang et al. 2018). These studies support the notion that adipocyte dedifferentiation happens in vivo and suggest, in light of recent results, that it may be an ancestral physiological process.
Thus, a number of studies now support the presence of dedifferentiation in a variety of kingdoms, mammals included. In both humans and rodents, dedifferentiation was observed in various cell types, including adipocytes. The aim of this article is to summarize current knowledge on adipocyte dedifferentiation by accurately describing dedifferentiated fat (DFAT) cell characteristics, reviewing up-to-date hypotheses that could explain this phenomenon, address possible applications of the ceiling culture approach, and highlight questions that still need to be addressed in the field.
The isolation of dedifferentiated adipocytes: a comparison of in vitro models
A major turning point for adipocyte cell culture was made when Sugihara et al. conceived a method that allowed culture of adherent mature adipocytes. In their cell culture model, mature adipocytes are seeded in a culture flask that is completely filled with serum-enriched medium (usually between 10 and 20% serum) and cultivated upside-down. The buoyancy of mature adipocytes allows them to adhere to the top inner surface of the reversed flask. Sugihara et al. were the first to demonstrate that once adherence occurred, most of the adipocytes became multilocular and took a fibroblast-like appearance, hence the name of “dedifferentiated adipocytes.” After 7 to 10 days, the flask is reversed and the resulting cells are cultivated in standard conditions (Sugihara et al. 1986). In the last decade, several groups have used the ceiling culture system to obtain DFAT cells from rats, mice, pigs, beefs, and humans (Poloni et al. 2012; Sun et al. 2013; Wei et al. 2013; Yagi et al. 2004; Zhang et al. 2000).
Beside the standard ceiling culture system described previously, some groups developed modified approaches to study DFAT cells. Fernyhough et al. used a ceiling culture system combined with a method of differential plating to obtain a homogenous cell population of dedifferentiated adipocytes (Fernyhough et al. 2004). This protocol, by taking advantage of the increased time needed for adipocyte adherence compared to the contaminating stroma-vascular fraction (SVF), allows the generation of a pure population of DFAT cells. In our laboratory, we have developed an approach allowing the treatment of cells with various effectors during the process of dedifferentiation. To do so, a glass slide is placed on the top of a plastic bushing and cells are seeded underneath the slide, thereby substantially decreasing the number of cells needed in each experiment. Much like other methods, seeded adipocytes then attach and dedifferentiate within a week (Lessard et al. 2015a).
Another approach, which slightly differs from ceiling culture, has been developed by Jumabay and colleagues. This group obtained DFAT cells by first incubating isolated adipocytes floating in medium for 24 h. This allowed cells of the SVF to sink. Floating adipocytes were then seeded in the well of a culture plate containing a filter (70 μm) for 5 days. The dedifferentiated fat cells went through the filter and adhered to the bottom of the well, while the adipocytes that did not dedifferentiate stayed on top and were subsequently removed (Jumabay et al. 2014). DFAT isolated by this filtering method are apparently highly enriched and express stem-cell-associated genes.
Of the four in vitro models described to obtain DFAT cells, only one (Jumabay et al. 2014) does not rely on ceiling culture. The models developed by Jumabay (Jumabay et al. 2014) and Fernyhough (Fernyhough et al. 2004) are likely to increase homogeneity of DFAT cells, thereby reducing the prevalence of contaminating SVF cells. On the other hand, the ceiling culture model developed in our laboratory (Lessard et al. 2015a) allows to significantly decrease the number of cells seeded and to treat them at various time points. These modified approaches developed to isolate DFAT cells offer advantages suiting a variety of research needs and can be applied to better characterize the DFAT cell population.
An overview of DFAT cell characteristics, from cellular morphology to pluripotency
Major morphological changes during the dedifferentiation process
Important morphological changes occur when mature adipocytes are seeded in ceiling culture. Using scanning electron microscopy, Sugihara et al. characterized these changes. After 2 or 3 days, mature adipocytes adhere to the inner surface of the flask maintaining their spherical shape. At day 4, the cytoplasm of some cells begins to spread: at this time, adipocytes still contain a large lipid droplet, while smaller lipid droplets begin to appear on the periphery of these cells. Then, the cells become multilocular and their appearance is increasingly similar to fibroblastic cells (Sugihara et al. 1986). Poloni et al. observed similarities in the structure of organelles between dedifferentiated mature adipocytes and adipose-derived stem cells (ASC) cultivated in vitro. Once the adipocytes are dedifferentiated, they are characterized by a spreading cytoplasm, the presence of small mitochondria and lysosomes, a well-developed Golgi complex, small lipid droplets, and a fusiform nucleus (Poloni et al. 2012). In contrast, Zhang et al. proposed that only the cytoplasm of smaller adipocytes tends to spread while large mature adipocytes maintain a spherical shape (Zhang et al. 2000).
Thus, it appears that during the process of dedifferentiation, mature adipocytes undergo major morphological changes and become fibroblast-like cells. These cells are characterized by intracellular reorganization including, for instance, loss of their large lipid droplet. Figure 1, captured in our laboratory, illustrates these morphological rearrangements, while also referring to changes observed and reported by various authors over the years.
Process characterizing mature adipocyte dedifferentiation in ceiling culture over time. Arrow is pointing to a dedifferentiating adipocyte, whereas the star identifies the lipid droplet. Still images of mature adipocytes isolated by collagenase I digestion, treated with CellLighit® Histone-2B-GFP reagent (Molecular Probes, Life Technologies, Eugene, USA) and cultivated in ceiling culture for 6 days. Images were taken from a time-lapse experiment done using Zeiss Axio Observer Z1 microscope (Carl Zeiss, Oberkochen, Germany). The microscope photographed the slide every 30 min in different Z positions with × 10 LD-A-Plan objective (Carl Zeiss, Oberkochen, Germany) for TL phase and GFP. These conditions are the same as those used in our recent experiments (Côté et al. 2018). Images were processed using ZEISS ZEN software (Carl Zeiss, Oberkochen, Germany). Selected images were taken at T6 (3 h), T75 (37.5 h), T164 (82 h), T178 (89 h), and T218 (109 h) following the start of the experiment. 1(Sugihara et al. 1986); 2(Poloni et al. 2012); 3(Côté et al. 2018); 4(Maurizi et al. 2017)
Changes in metabolic and secretory abilities of DFAT cells
During the process of dedifferentiation, adipocytes may not only reshape their cellular structure but also their metabolic and secretory profile. A few studies have analyzed these changes as well as the functionality of DFAT cells. Zhang et al. studied the effects of hormonal treatments aimed at stimulating the processes of lipogenesis and lipolysis on adipocytes in ceiling culture. They demonstrated that during dedifferentiation, the processes of lipolysis and lipogenesis were respectively stimulated when adipocytes were treated with forskoline (10 μM) and insulin (10 and 100 nM). In that study, treatment with TNF-α increased the secretion of leptin. Using scanning confocal microscopy, cellular expression and localization of leptin in ceiling-cultured adipocytes was shown (Zhang et al. 2000). Accordingly, Sugihara et al. observed a positive effect on the process of lipogenesis following treatment with insulin and an increase of lipolysis following treatment with norepinephrine and dibutyryl-cAMP during adipocyte dedifferentiation. Immunohistochemical experiments confirmed the presence of two enzymes, triglyceride lipase and glycerophosphate deshydrogenase at the cytoplasmic level (Sugihara et al. 1986). However, stimulation of lipolysis and progressive shedding of lipids do not seem to explain the dedifferentiation process as our group failed to quantify changes in cell size and lipid content by using Oil Red O staining (Lessard et al. 2015b). The phenomenon of liposecretion, captured by time-lapse microscopy experiments as the quick release of the lipid droplet (Côté et al. 2018; Maurizi et al. 2017), could possibly explain inconsistent results and may indicate that the process is relatively independent of adipocyte size.
The ability to secrete growth factors and cytokines has also been explored. Perrini et al. demonstrated that dedifferentiated adipocytes from obese individuals were able to secrete cytokines and growth factors like IL-1β, IL-1ra, IL-6, IL-8, IL-15, IL-17, G-CSF, IFN-γ, TNF-α, eotaxin, MCP1, and VEGF. In that study, the secretion of IL-8 was significantly higher in the subcutaneous depot than in the visceral depot. In the subcutaneous compartment, secretion of IL-6 was significantly higher in dedifferentiated adipocytes than in SVF cells (Perrini et al. 2013). Poloni et al. obtained similar results using dedifferentiated adipocytes from nonobese individuals, but they observed no depot difference in the secretion profile (Poloni et al. 2012). It is noteworthy that results from the two previous studies were obtained using conditioned media. In a previous study, we observed the secretion of IL-6 and VEGF during dedifferentiation. IL-6 secretion was similar between day 7 and day 12 of the process, whereas VEGF secretion increased from day 7 to day 12 (Lessard et al. 2015b).
The above observations suggest that DFAT cells maintain some of the functional characteristics attributed to mature adipocytes including lipogenic and lipolytic abilities. Although the secretory profile of DFAT cells includes a wide range of cytokines (Perrini et al. 2013), it has been proposed that this panel may vary across the dedifferentiation process (Lessard et al. 2015b). These observations support, once again, the presence of major changes during ceiling culture.
Characterization of the surface antigen signature of DFAT cells and comparison with others stem-cell lineages
Due to the previously mentioned morphological rearrangements occurring in DFAT cells, questions may arise on possible concurrent adaptations of the cell surface antigen signature. Several groups have used flow cytometry to identify cell surface antigens in dedifferentiated adipocytes. In the study performed by Matsumoto et al., human dedifferentiated subcutaneous adipocytes were positive for surface antigens CD13, CD29, CD44, CD49d, CD90, CD105, HLA-A, HLA-B, and HLA-C, but negative for surface antigens CD11b, CD31, CD34, CD45, CD56, CD106, α-SMA, and HLA-DR (Matsumoto et al. 2008). Using subcutaneous and omental human adipocytes, Poloni et al. obtained similar results. These cells were positive for surface antigens CD29, CD44, CD73, CD90, and CD105, but negative for antigens CD14, CD34, CD45, CD117, CD133, CD271, and HLA-DR (Poloni et al. 2012). Because of their similarities, cell surface antigen signatures of dedifferentiated adipocytes are often compared to that of SVF and bone marrow stem cells (MSCBM). However, some differences have been noticed regarding antigens CD11b, CD49d, and CD106 (Kishimoto et al. 2014; Miyazaki et al. 2005; Poloni et al. 2012), and the influence on antigen signature by successive cell divisions, which seem not to affect DFAT cells (Matsumoto et al. 2008; Mitchell et al. 2006). Once again, these differences might be related to isolation techniques or to the species from which the cells originated. Table 1 shows the antigen signature of ACS, MSCBM and DFAT cells.
Gene expression of the isolated DFAT cell population
Because surface antigens signature of DFAT cells resembles that of MSCBM and ACS, it is not surprising that dedifferentiated adipocytes have a stem cell-like gene expression profile. Indeed, DFAT cells express cell cycle reprogramming genes like NANOG, SOX17, GATA4, TBX1, SOX2, OCT4, C-MYC, KLF4, RUNX2, and SOX9. Some of these genes are already expressed by mature adipocytes, while the expression of RUNX2 and SOX9 is induced during dedifferentiation (Gao et al. 2012; Matsumoto et al. 2008; Maurizi et al. 2017; Oki et al. 2008; Poloni et al. 2012). During dedifferentiation, the expression of genes related to the function of mature adipocytes like PPARγ, C/EBPβ, C/EBPα, LPL, leptin, ADIPOQ, FABP4, and GLUT4 are downregulated (Côté et al. 2017a; Lessard et al. 2015b; Matsumoto et al. 2008; Ono et al. 2011; Peng et al. 2015). Similarly, Nobosue et al. found that murine dedifferentiated subcutaneous adipocytes did not express C/EBPα, PPARγ2, and GLUT4 (Nobusue et al. 2008). Results obtained by our group suggest that PPARγ, C/EBPα, LPL, and ADIPOQ are expressed in subcutaneous and omental human mature adipocytes as expected, but that their expression is drastically diminished as the process of dedifferentiation takes place (Côté et al. 2017a). Moreover, we observed changes in the expression of genes related to the extra-cellular matrix (ECM), suggesting that adipocyte dedifferentiation involves important ECM remodeling (Lessard et al. 2015b).
However, findings on functional adipogenic-genes were not confirmed by Matsumoto et al., where human subcutaneous dedifferentiated adipocytes still expressed GLUT4, LPL, and leptin, but not PPARγ, C/EBPβ, nor C/EBPα. These differences might be explained by differences in the approach used to isolate adipocytes and in the homogeneity of the cell population as the presence of contaminating SVF cells in the mature adipocyte fraction may have influenced these results. The hypothesis that DFAT cells are actually contaminating fibroblasts has been ruled out using fluorescence-activated cell sorting to characterize floating cells (Nobusue et al. 2008). This group found a homogeneous population of floating adipocytes lacking contaminating SVF (Nobusue et al. 2008). It should be mentioned that because of demonstrated diversities among dedifferentiated cells issued from various species (Jumabay et al. 2014), results might be inconsistent.
In DFAT cells, the expression of genes related to both cell renewal and reprogramming is increased, thus resembling that often found in stem cells. At the same time, the expression of genes related to mature adipocyte functions is downregulated, suggesting at least a partial genetic reprogramming.
Lineage redifferentiation potential and pluripotent features of DFAT cells
Due to the fact that antigen and genomic signatures are often compared to the ones of MSCBM and ASC, some authors have investigated the redifferentiation abilities of DFAT cells. Because these cells are derived from the mesenchyme, it is widely believed that they can only redifferentiate in cells belonging to this lineage (adipocytes, osteoblasts, chondrocytes) and therefore may be characterized as multipotent. Supporting this hypothesis, it has been demonstrated that dedifferentiated adipocytes can be redifferentiated into adipocytes in vitro (Kou et al. 2014; Shigematsu et al. 1999), and in vivo (Nobusue et al. 2008; Yagi et al. 2004). Furthermore, it has been shown that dedifferentiated adipocytes can generate osteocytes (Justesen et al. 2004; Kishimoto et al. 2013; Matsumoto et al. 2008; Oki et al. 2008), or chondrocytes (Matsumoto et al. 2008; Okita et al. 2015), when cultivated in appropriate conditioned media. Other studies have determined that dedifferentiated adipocytes can be redifferentiated in cardiomyocytes in vivo and in vitro (Jumabay et al. 2009), in skeletal myocytes (Kazama et al. 2008), in smooth muscle cells (Obinata et al. 2011) and in endothelial cells (Planat-Benard et al. 2004). Ono et al. observed an increase in the expression of cell surface antigens associated with hematopoietic cells (CD10, CD24, CD40) and myeloid cells (CD13, CD44, CD86) during mature adipocyte dedifferentiation, suggesting that the dedifferentiated cells can be redifferentiated into hematopoietic cells (Ono et al. 2011), which has been subsequently confirmed in vitro (Poloni et al. 2012). A study also found that dedifferentiation into neuronal cells is possible (Ohta et al. 2008). This could be explained by the fact that mature adipocytes already express neuronal markers like β3-tubulin and nestin (Ohta et al. 2008).
Taken together, results suggest that dedifferentiated adipocytes are not only multipotent but rather pluripotent, meaning that they have the potential to differentiate into any of the three germ layers (endoderm, mesoderm, and/or ectoderm) (Jumabay et al. 2009). Yet, in vivo studies are necessary to evaluate the behavior of these cells in a physiological context as the aforementioned studies were limited in time and set under very specific conditions.
Summary on the major changes taking place during mature adipocyte dedifferentiation
Overall, it appears that during dedifferentiation, mature adipocytes are subjected to a number of changes. One of the most important morphological alteration is the loss of the large lipid droplet, which despite conserved lipolytic activity in DFAT cells, is secreted via liposecretion. The generated DFAT cell population display surface markers often associated to stem cells, such as ASC and MSCBM. In addition, it appears that DFAT cells undergo some form of genetic reprogramming, as the expression of genes related to stem cell renewal is amplified whereas that associated with mature adipocyte functioning is hindered. These data suggest that DFAT cells may be compared to stem cells, especially as studies support their pluripotency.
Hypothetical mechanisms underlying the dedifferentiation process
Little is known about the mechanisms underlying the process of dedifferentiation, and it is possible that the mechanisms vary according to the cell type and species from which cells are isolated. Over the years, three major hypotheses have been proposed to explain the origin of DFAT cells. The first is that the population of DFAT cells actually arises from SVF contaminating cells attached to mature cells at the time of isolation. Although the presence of contaminating cells cannot be fully excluded, it is unlikely that the whole population of DFAT cells originates from contaminating SVF cells. Indeed, evidence described in the section “An overview of DFAT cells characteristics, from cellular morphology to pluripotency” points toward a process of adipocyte reprogramming as DFAT cells have been shown to slightly differ from ASC. The second hypothesis is that asymmetric cell division rather than dedifferentiation is the process underlying the generation of DFAT cells. This implies that mature adipocytes enter the cell cycle and are able to undergo mitosis. Finally, a third hypothesis proposes that DFAT cells are in fact adipocytes that rapidly secreted their lipid droplet.
The first studies to investigate cell division in DFAT cells found that mature adipocytes may actually enter the cell cycle and thus may possibly divide asymmetrically. Sugihara and colleagues reported that after four days of dedifferentiation, approximately 2% of the unilocular adipocytes were labeled with tritiated-thymidine, while 20% and 40% of multilocular and fibroblast cells were respectively labeled. These findings supported the notion that mature adipocytes may gain the ability to replicate their DNA in ceiling culture. The authors also suggested that some of the dividing fat cells were transferring their lipid droplet to the daughter cell (Sugihara et al. 1986). Zhang et al. demonstrated that in ceiling culture, approximately 2% of the unilocular adipocytes incorporated bromodeoxyuridine (BrdU) and that dedifferentiated adipocytes had a capacity to replicate and proliferate (Zhang et al. 2000). In another study by Matsumoto et al., as many as 50% of the mature adipocytes adhering to the inner plastic surface of the flask in ceiling culture incorporated BrdU, again suggesting DNA replication. Several adipocytes that were labeled with BrdU were binucleic, indirectly suggesting that they had been through the S phase of the cell cycle and had undergone nucleus division. In the same study, real-time fluorescence microscopy experiments indirectly suggested an asymmetrical division phenomenon that generated fibroblast-like cells from unilocular mature adipocytes (Matsumoto et al. 2008). Poloni et al. suggested that the proliferative capacity of dedifferentiating adipocytes was similar to that of ASC and MSCBM (Poloni et al. 2012). In our laboratory, proliferation capacity of DFAT cells was excellent as we were able to cultivate dedifferentiated fat cells for more than 12 passages and some cells were cultivated for 23–24 passages (Lessard et al. 2015b). Although some of these studies point toward asymmetrical cell division, it should be mentioned that DNA synthesis is not a direct marker of cell division, but rather of the cell entering phase S of the cell cycle.
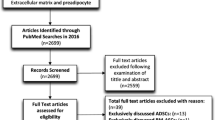
Recent studies suggest that DFAT cells are generated through a process during which mature adipocytes shed their large lipid droplet either gradually or rapidly. Maurizi et al. suggested for the first time that the dedifferentiation process was not due to a progressive loss of lipids, as would occur through lipolysis, but to a phenomenon that has been named “liposecretion” (Maurizi et al. 2017). Time-lapse and electron microscopy experiments suggested that when seeded in ceiling culture, some adipocytes quickly secrete their lipid droplet and become fibroblast-like cells that no longer contain lipids. It was also suggested that this phenomenon may be visualized in explants of subcutaneous adipose tissue that are maintained in matrigel (Maurizi et al. 2017). Our recent results (Côté et al. 2018) replicated these findings using time-lapse microscopy with fluorescence labeling of the cell nucleus and pointed to a possible process of arrested mitosis followed by liposecretion leading to the fibroblast-like cell. Considering data on the molecular mechanisms possibly implicated in liposecretion, Maurizi et al. suggested that the phenomenon is likely controlled by autocrine and external signaling molecules (Maurizi et al. 2018b). Figure 2 schematically illustrates the liposecretion process as well as the theoretical model characterizing temporal aspects of cell cycle progression in ceiling culture.
The process of dedifferentiation and the proposed progression of the cell cycle in mature adipocytes undergoing ceiling culture. The image illustrates the key morphological changes in ceiling cultured adipocytes (fading arrow) along with the hypothesized progression of the cell cycle (dotted line). Data on cell cycle progression have been inferred by the observation of phosphorylated histone 3 and cyclin B1 histochemical labeling in mature human adipocytes undergoing ceiling culture (Côté et al. 2018). Morphological adaptations described by a number of authors are represented. Following adherence, mature adipocytes elongate (Côté et al. 2018; Lessard et al., .2015b; Maurizi et al. 2017; Poloni et al. 2012), show a fusiform nucleus (Poloni et al. 2012) and small lipid droplets appear (Lessard et al. 2015b). Secretion of the lipid droplet has been termed liposecretion. We proposed that the rapid secretion of the lipid droplet happens concurrently to a reversible arrest in G2/M phase of the cell cycle (Côté et al. 2018). Cell cycle progression would resume only after liposecretion. The secreted lipid droplet is represented enclosed by a membrane according to electron microscopy data suggesting that the adipocyte lipid droplet is surrounded by a trilaminar membrane (Maurizi et al. 2017). This has yet to be confirmed using other approaches
Extracellular signals possibly driving adipocyte dedifferentiation
Regarding the causes of dedifferentiation, it should be kept in mind that reliable data explaining the causes of mature adipocyte dedifferentiation are still lacking. The numerous hypotheses put forth in the literature may not necessarily be exclusive to adipose tissue and can be applied to dedifferentiation in general. One of them suggests that stress, whether physical, chemical, or metabolic, could be a triggering factor for dedifferentiation. By dedifferentiating, the cells would be protected from harm or injury. This was suggested to explain the dedifferentiation of myelinating Schwann cells in the context of nerve injury (Chen et al. 2007; Jessen and Mirsky 2008). This theory may also apply to adipocytes. To study the effects of physical stress on adipocytes, Liao et al. created a model using a tissue expander placed under the inguinal fat pads of rats. Water injection gradually expanded the fat pad. There were fewer unilocular adipocytes in the expanded fat pad compared to the untreated fat pad and an increase in the number of proliferative cells was observed only under the expanded fat condition. In addition, unilocular adipocytes became multilocular adipocytes and then fibroblast-like cells. Finally, the expression of PPARγ, C/EBPα, and ADIPOQ was significantly downregulated in the treated fat pads (Liao et al. 2015). In another context, it was suggested that metabolic stress induced by chronic overload of nutrients could trigger pancreatinc β-cell dedifferentiation in T2D. By losing their differentiated characteristics, β-cells would be protected from metabolic stress such as hyperglycemia (White et al. 2016). Dedifferentiation of retinal glial cells in response to oxidative stress is another example of how various kinds of stress may favor loss of the differentiated phenotype (Abrahan et al. 2009).
Another possible mechanism is hypoxia-induced dedifferentiation. Studies in chondrocytes and smooth muscle cells suggested that lack of oxygen could induce or exacerbate dedifferentiation (Aitken et al. 2010; Lafont 2010). These mechanisms may also be applicable to adipocytes, as they are known to be sensitive to oxygen flow (Flynn and Woodhouse 2008).
The triggering factors and the mechanisms underlying adipocyte dedifferentiation could be different in vitro and in vivo. Weinberg et al. suggested that in vitro, dedifferentiation of β-cells could be triggered by the absence of pancreatic tissue (dissociation to single-cell culture). Indeed, when they are cultivated in vitro, pancreatic islets lose their tridimensional conformation, a process that could be induced by β-cell isolation from their environment (Weinberg et al. 2007). This could also explain why mature adipocytes undergo dedifferentiation in vitro as they need to be isolated from whole tissue by enzymatic digestion to be cultivated. Our group postulated that mature adipocyte dedifferentiation could be involved in adipose tissue remodeling (Lessard et al. 2015b). This adaptive mechanism could help modulate adipose tissue lipid storage capacity by favoring increases in adipocyte cell number. This is consistent with the finding that expression of gene encoding proteins associated with the ECM is modulated after weight loss (Henegar et al. 2008). Aging and multiparity could also trigger the process of dedifferentiation, at least in mice (Talchai et al. 2012).
Although it has never been clearly demonstrated, adherence of adipocytes to the plastic surface of the flasks could favor the process of dedifferentiation. Medium composition could also contribute to the process as ceiling culture is generally performed in relatively high serum conditions.
Suggested intracellular pathways involved in dedifferentiation
The causes of mature adipocyte dedifferentiation are at the moment only hypothetical, and the same goes for the intracellular pathways triggering liposecretion in mature adipocytes. Overall, three major pathways have been suggested to be implicated in adipocyte dedifferentiation: the TGF-β, Wnt, and Notch pathways. Because serum contains growth factors such as TGF-β, it has been suggested that this factor could play a role in the process (Côté et al. 2017b; Huber and Kluger 2015; Sugihara et al. 1989) much like it was reported in β-cells (Toren-Haritan and Efrat 2015). Similarly, it appears that the Notch signaling pathway may be involved, at least at some level, in adipocyte dedifferentiation. By selectively stimulating the expression of Notch intracellular domain in murine mature adipocytes, Bi and colleagues showed that these cells dedifferentiate and are detected in samples of dedifferentiated liposarcoma (Bi et al. 2016).
More recently, the microenvironment of the cells was suggested to influence their behavior and trigger the process of dedifferentiation. Relocation of mature cells into a niche of stem cells could lead to reprogramming events. The environmental cues given by the stem cells could induce epigenetic modulations and/or specific gene activation and overexpression (Shoshani and Zipori 2011). The microenvironment generated by cancer cells could also lead to dedifferentiation. Zoico et al. observed a decrease in gene expression of mature adipocyte markers and an increase in the expression of fibroblast-specific genes when 3T3-L1 cells were co-cultured with a cell line from undifferentiated human pancreatic carcinoma. These effects were partly mediated by an increased activation of the Wnt pathway (Zoico et al. 2016; Zoico et al. 2018). Similar results were obtained when adipocytes were co-cultured with breast cancer-associated fibroblasts. The proximity between adipocytes and cancer cells enhanced the secretion of fibronectin and the migratory abilities of adipocyte-derived fibroblasts. These effects were mediated by increased activation of the Wnt pathway in response to the secretion of Wnt3A by cancer cells (Bochet et al. 2013). These studies suggest that tumor cells could contribute to mature adipocyte dedifferentiation, which in turn, would facilitate the proliferation of tumor cells by secreting pro-inflammatory cytokines and metabolites essential to cancer cell survival.
These mechanisms are hypothetical and literature is quite inconsistent. However, pathways involved in cell-cell communication and those related to cell proliferation and/or cell fate are likely to play a role during the process of adipocyte dedifferentiation.
Evidence of epigenetic regulation and posttranscriptional modulation of gene expression
As mentioned, little is known about the exact cellular mechanisms allowing somatic cells to dedifferentiate. Sugihara and colleagues suggested that the dedifferentiation process may represent a development phase in which mature adipocytes specialized in lipid storage become non-differentiated fibroblast-like precursor cells (Sugihara et al. 1986). Nevertheless, to reverse the process of differentiation acquired by a mature cell, some sort of cellular reprogramming, if not nuclear reprogramming, is required. Some transcription factors have been identified as important players in dedifferentiation. Studies published in the last decade supported the role of four transcription factors, namely Sox2, Oct3/4, Klf4, and c-Myc, which are able to convert differentiated somatic cells into pluripotent stem cells (Takahashi and Yamanaka 2016). Data on DFAT cells are consistent with a similar hypothesis, as stem cell markers like Oct4, Sox2, c-Myc, and Nanog and stem cell-associated antigens are found in dedifferentiated adipocytes (Gao et al. 2012; Matsumoto et al. 2008; Poloni et al. 2012).
Studies have also suggested that miRNA may participate in the maintenance and regulation of dedifferentiated cell phenotypes. MiRNAs are noncoding, single-stranded RNAs incorporated into RNA-induced silencing complex (RISC) found in the cytoplasm, and their role is to suppress gene expression through mRNA degradation (Gu and Kay 2010). Although miRNAs have been suggested to act mostly as reprogramming efficiency boosters, studies are showing that miRNA particles (miR 106a-363, miR 302–367 clusters, miR 200 family, and miR 93/106b) activated by transcription factors Oct4, Sox2, Klf4, and c-Myc may favor mesenchymal-to-epithelial progression in induced pluripotent stem (iPS) cells. In addition, a recent review (Maurizi et al. 2018a) listed a number of miRNAs that are hypothetically involved in the regulation of liposecretion. Although data are based on the role of miRNAs in adipocyte differentiation, rather than dedifferentiation, it may be interesting to study these molecules in the contexts of dedifferentiation. In addition, some miRNAs may be involved in the regulation of cell cycle factors such as p21 and p53 (Li et al. 2017), which could in turn explain the drive of the cell cycle observed in ceiling culture.
However, it appears that these two mechanisms may not be sufficient to explain the entire cellular process of dedifferentiation in somatic cells. A third mechanism involving epigenetic changes is very likely to be present. Indeed, when undifferentiated somatic cells differentiate, the transcribed portion of their genome is heavily reduced. This is achieved through epigenetic changes such as DNA methylation, histone, or chromatin modifications that induce the formation of heterochromatin. Dedifferentiated cells should, therefore, have a loose chromatin structure to enable global gene expression and remodeling (Eguizabal et al. 2013; Shoshani and Zipori 2011). This hypothesis is supported by Poloni et al., who found that DFAT cells show DNA methylation patterns similar to MSCBM. In-depth analyses showed that the epigenetic signature was significantly different between mature and dedifferentiated adipocytes, but no difference could be found between dedifferentiated adipocytes and MSCBM (Poloni et al. 2012). These results suggest that epigenetic reprogramming takes place during dedifferentiation and may be a crucial step supporting pluripotency.
By inducing a more “permissive” status (Shoshani and Zipori 2011) in which somatic cells could express a larger portion of the whole genome, the cells enter the cell cycle. Differentiated cells are considered to be in the G0 phase of the cell cycle. It is now thought that this process can be reversed and that quiescent cells can re-enter the cell cycle (G1 phase) under specific conditions (Eguizabal et al. 2013). Because the cell cycle is partially controlled by cyclically activated protein kinases (Shugart et al. 1995), a potential involvement of protein regulation via degradation or phosphorylation has been proposed (Shoshani and Zipori 2011). A drive of the cell cycle has been reported in DFAT cells since 2008, when Matsumoto et al. discovered that these cells actually enter the cell cycle (Matsumoto et al. 2008). Ullah et al. further support this drive by illustrating the association of adipocyte gene expression with cell cycle arrest and dedifferentiated cell gene expression with cell cycle drive (Ullah et al. 2013). A possible implication of the cell cycle was also recently suggested in our study (Côté et al. 2018), where the process of dedifferentiation was explored in adipocytes using immunofluorescence labeling of phosphorylated serine 10 on histone 3 and cyclin B1. Results showed that, during ceiling culture, both proteins were found in the nucleus, suggesting mitosis. Yet, time-lapse microscopy excluded this hypothesis by illustrating that during the phenomenon of liposecretion, cell division did not occur. In addition, the use of anti-mitotic agents caused a consistent reduction in fibroblast confluence during ceiling culture but did not prevent liposecretion. Taken together, this may indicate that following liposecretion, the DFAT cells multiply eventually leading to confluence of dedifferentiated adipocytes (Côté et al. 2018).
Changes in gene expression and cell cycle status could coincide with changes in telomere length, although this has yet to be confirmed in human cells. Indeed, cell proliferation is associated with a decrease in the length of telomeric DNA (Harley et al. 1990) and telomeres are elongated in iPS compared to differentiated cells from which they were derived (Marion et al. 2009). When under stress, the cells could dedifferentiate and lengthen their telomeres to favor the proliferation of new cells.
Possible applications of DFAT cells in tissue engineering and regenerative medicine
Because of their unique characteristics, dedifferentiated cells are attractive candidate for the treatment of several clinical conditions such as T2D, cardiovascular diseases, liver diseases, kidney diseases, as well as autoimmune diseases. Several groups have examined the potential of DFAT cells for the treatment of these pathological conditions. Jumabay et al. showed that DFAT cells isolated from GFP-transgenic rats were able to differentiate into cardiomyocytes when co-cultured with neonatal cardiomyocytes. In that study, when GFP dedifferentiated adipocytes were transplanted in a rat acute myocardial infarction model, GFP cells accumulated in great amounts in the infarcted myocardia 8 weeks after transplantation. Most of these cells expressed cardiac markers, suggesting redifferentiation into cardiomyocytes. The capillary density in the infarcted area was increased and no GFP-positive vessels were detected. Moreover, no adipocytes and osteocytes were found in the infarcted cardiac tissue. The authors suggested that once they are transplanted, dedifferentiated cells promote neovascularization by secreting proangiogenic factors (Jumabay et al. 2009). This hypothesis is consistent with the results obtained by Nakagami et al. in a study that examined the angiogenic potential of adipose-derived stem cells for the treatment of ischemic diseases (Nakagami et al. 2005).
Few treatments are currently available for neurodegenerative diseases. In rats, transplantation of DFAT cells into the spinal cord improved induced spinal cord injuries. Allografting of DFAT cells also led to an improvement of motor dysfunction. This improvement was thought to occur through expression of neural markers by dedifferentiated cells before and after their engraftment in the injured spinal cord area (Ohta et al. 2008).
In kidney, transplantation of DFAT cells was shown to improve kidney diseases through anti-inflammatory and immunosuppressive effects (Maruyama et al. 2015; Nur et al. 2008). Obinata et al. showed that injection of dedifferentiated adipocytes into the paraurethral connective tissue in Sprague–Dawley rats improved muscle regeneration of the sphincter and its function (Obinata et al. 2011). Transplantation of DFAT cells in a model of vesico-urethral reflux decreased the number of apoptotic cells and the formation of connective tissue while improving the condition (Ikado et al. 2016).
Soejima et al. studied the potential of DFAT cells in combination with a basic fibroblast growth factor (FGF) treatment for dermal regeneration after artificial dermis graft in rats. They showed that dedifferentiated cells under FGF treatment differentiated into endothelial cells and contributed to the process of angiogenesis. Vascularization of the skin graft was improved in rats treated with dedifferentiated cells compared to the control group only receiving the skin graft (Soejima et al. 2015).
Regeneration of bone tissues is essential for bone injuries arising from traumatic/neoplastic processes or congenital anomalies. Most of the techniques used for bone regeneration include a combination of stem cells and biomaterial scaffold (Tang et al. 2008; Yoon et al. 2007). In a study by Kishimoto et al., DFAT cells isolated from subcutaneous rabbit fat pads were able to proliferate and redifferentiate into osteoblasts when cultivated in osteogenic medium on a titanium fiber mesh scaffold (Kishimoto et al. 2013). A subsequent study performed in humans also demonstrated that DFAT cells isolated from buccal fat pads had a higher osteogenic potential than ASC, even though they shared similar characteristics (Kishimoto et al. 2014). However, it should be brought to attention that this study was performed using the fat pad of a single individual. Similarly, DFAT cells could support healing in articular cartilage injuries. This has been shown in rats with ostochondral femur defects, where transplanted dedifferentiated adipocytes promoted cartilage repair within one month of transplantation (Shimizu et al. 2018).
Currently, most of the studies were performed using animal models and the long-term consequences of using DFAT cells for the treatment of clinical conditions or diseases are unknown. Stem cell research regulation obviously needs careful consideration, especially for uses intended for humans.
Future directions
Although research on DFAT cells has significantly expanded over the years, many important questions still need to be answered in this field.
The large majority of the examples presented in the previous section do not address differences between ASC or DFAT cells in tissue engineering. ASC show a differentiation potential similar to that of DFAT cells and thus are also suitable candidates for tissue engineering (Lindroos et al. 2011; Saler et al. 2017; Zuk et al. 2002). However, available literature suggests some differences between SVF and DFAT cells regarding secreted factors (Côté et al. 2017b; Lessard et al. 2015b) and gene expression (Côté et al. 2017a; Poloni et al. 2012). Current knowledge does not yet allow an accurate comparison between these two cell types, at least regarding their potential in tissue engineering. For this reason, more research is needed addressing the functionality of the tissues generated using either ASC or DFAT cells.
Regarding the phenomenon of liposecretion, many questions remain unanswered. The pathways regulating this process are not known. In a recent review, Maurizi and colleagues suggested that at least three gene clusters may be involved in this phenomenon. Indeed, due to remarkable differences between mature adipocytes and MSCBM gene expression, these investigators highlighted that clusters involving cell morphogenesis, cell proliferation, and membrane lipid transport are likely to be implicated (Maurizi et al. 2018b). Other groups suggested a role of the Wnt (Zoico et al. 2018), Notch (Bi et al. 2016), or even TGF-β (Côté et al. 2017b) pathways in adipocyte dedifferentiation. Although interesting, data emerging in the literature are not consistent and the role of these pathways has yet to be confirmed.
The development of a trilaminar plasma membrane surrounding the adipocyte lipid droplet during liposecretion needs also to be confirmed. To date, no study investigated membrane dynamics or composition during liposecretion.
Finally, although examples of in vivo adipocyte dedifferentiation have already been reported (Bi et al. 2016; Maurizi et al. 2017; Wang et al. 2018), it may be interesting to have a larger body of evidence. This, combined with data on the role of dedifferentiation in adipose tissue homeostasis, may add a novel angle to our understanding of this organ.
Conclusion
DFAT cells show a stem cell-like antigen profile and genome signature, which add to their proliferative capacities and their ability to re-differentiate into diverse cell lineages (Matsumoto et al. 2008). This may allow the development of new uses in tissue engineering. Human stem cells, particularly those isolated from bone marrow and adipose tissue have received wider attention in the last decades in the field of regenerative medicine because they can be easily isolated and cultured in vitro. However, both methodologies have disadvantages: mesenchymal stem cells collected from the bone marrow require a painful procedure and allow the isolation of a minor quantity of stem cells; similarly, a relatively large sample of adipose tissue is required to isolate a considerable number of ASC. Compared to other types of stem cells, mature adipocytes are abundant, they can be easily isolated and they represent a rather homogenous population. For these reasons, the discovery of mature adipocyte dedifferentiation may underline a new role for DFAT cells in the field of regenerative medicine.
References
Abrahan CE, Insua MF, Politi LE, German OL, Rotstein NP (2009) Oxidative stress promotes proliferation and dedifferentiation of retina glial cells in vitro. J Neurosci Res 87:964–977
Aitken KJ, Tolg C, Panchal T, Leslie B, Yu J, Elkelini M, Sabha N, Tse DJ, Lorenzo AJ, Hassouna M et al (2010) Mammalian target of rapamycin (mTOR) induces proliferation and de-differentiation responses to three coordinate pathophysiologic stimuli (mechanical strain, hypoxia, and extracellular matrix remodeling) in rat bladder smooth muscle. Am J Pathol 176:304–319
Bi P, Yue F, Karki A, Castro B, Wirbisky SE, Wang C, Durkes A, Elzey BD, Andrisani OM, Bidwell CA et al (2016) Notch activation drives adipocyte dedifferentiation and tumorigenic transformation in mice. J Exp Med 213:2019–2037
Bochet L, Lehuede C, Dauvillier S, Wang YY, Dirat B, Laurent V, Dray C, Guiet R, Maridonneau-Parini I, Le Gonidec S et al (2013) Adipocyte-derived fibroblasts promote tumor progression and contribute to the desmoplastic reaction in breast cancer. Cancer Res 73:5657–5668
Chen ZL, Yu WM, Strickland S (2007) Peripheral regeneration. Annu Rev Neurosci 30:209–233
Cinti F, Bouchi R, Kim-Muller JY, Ohmura Y, Sandoval PR, Masini M, Marselli L, Suleiman M, Ratner LE, Marchetti P et al (2016) Evidence of beta-cell dedifferentiation in human type 2 diabetes. J Clin Endocrinol Metab 101:1044–1054
Côté JA, Guenard F, Lessard J, Lapointe M, Biron S, Vohl MC, Tchernof A (2017a) Temporal changes in gene expression profile during mature adipocyte dedifferentiation. Int J Genomics 2017:5149362
Côté JA, Lessard J, Pelletier M, Marceau S, Lescelleur O, Fradette J, Tchernof A (2017b) Role of the TGF-beta pathway in dedifferentiation of human mature adipocytes. FEBS Open Bio 7:1092–1101
Côté JA, Gauthier MF, Ostinelli G, Brochu D, Bellmann K, Marette A, Julien F, Lebel S, Tchernof A (2019) Characterization and visualization of the liposecretion process taking place during ceiling culture of human mature adipocytes. J Cell Physiol 234(7):10270–10280
Eguizabal C, Montserrat N, Veiga A, Izpisua Belmonte JC (2013) Dedifferentiation, transdifferentiation, and reprogramming: future directions in regenerative medicine. Semin Reprod Med 31:82–94
Fernyhough ME, Vierck JL, Hausman GJ, Mir PS, Okine EK, Dodson MV (2004) Primary adipocyte culture: adipocyte purification methods may lead to a new understanding of adipose tissue growth and development. Cytotechnology 46:163–172
Flynn L, Woodhouse KA (2008) Adipose tissue engineering with cells in engineered matrices. Organogenesis 4:228–235
Gao Q, Zhao L, Song Z, Yang G (2012) Expression pattern of embryonic stem cell markers in DFAT cells and ADSCs. Mol Biol Rep 39:5791–5804
Gronthos S, Franklin DM, Leddy HA, Robey PG, Storms RW, Gimble JM (2001) Surface protein characterization of human adipose tissue-derived stromal cells. J Cell Physiol 189:54–63
Gu S, Kay MA (2010) How do miRNAs mediate translational repression? Silence 1:11
Harley CB, Futcher AB, Greider CW (1990) Telomeres shorten during ageing of human fibroblasts. Nature 345:458–460
Henegar C, Tordjman J, Achard V, Lacasa D, Cremer I, Guerre-Millo M, Poitou C, Basdevant A, Stich V, Viguerie N et al (2008) Adipose tissue transcriptomic signature highlights the pathological relevance of extracellular matrix in human obesity. Genome Biol 9:R14
Huber B, Kluger PJ (2015) Decelerating mature adipocyte dedifferentiation by media composition. Tissue Eng Part C, Methods 21:1237–1245
Ikado Y, Obinata D, Matsumoto T, Murata Y, Kano K, Fukuda N, Yamaguchi K, Takahashi S (2016) Transplantation of mature adipocyte-derived dedifferentiated fat cells for the treatment of vesicoureteral reflux in a rat model. Int Urol Nephrol 48:1951–1960
Jessen KR, Mirsky R (2008) Negative regulation of myelination: relevance for development, injury, and demyelinating disease. Glia 56:1552–1565
Jumabay M, Matsumoto T, Yokoyama S, Kano K, Kusumi Y, Masuko T, Mitsumata M, Saito S, Hirayama A, Mugishima H et al (2009) Dedifferentiated fat cells convert to cardiomyocyte phenotype and repair infarcted cardiac tissue in rats. J Mol Cell Cardiol 47:565–575
Jumabay M, Abdmaulen R, Ly A, Cubberly MR, Shahmirian LJ, Heydarkhan-Hagvall S, Dumesic DA, Yao Y, Bostrom KI (2014) Pluripotent stem cells derived from mouse and human white mature adipocytes. Stem Cells Transl Med 3:161–171
Justesen J, Pedersen SB, Stenderup K, Kassem M (2004) Subcutaneous adipocytes can differentiate into bone-forming cells in vitro and in vivo. Tissue Eng 10:381–391
Katz AJ, Tholpady A, Tholpady SS, Shang H, Ogle RC (2005) Cell surface and transcriptional characterization of human adipose-derived adherent stromal (hADAS) cells. Stem Cells (Dayton, Ohio) 23:412–423
Kazama T, Fujie M, Endo T, Kano K (2008) Mature adipocyte-derived dedifferentiated fat cells can transdifferentiate into skeletal myocytes in vitro. Biochem Biophys Res Commun 377:780–785
Kishimoto N, Momota Y, Hashimoto Y, Ando K, Omasa T, Kotani J (2013) Dedifferentiated fat cells differentiate into osteoblasts in titanium fiber mesh. Cytotechnology 65:15–22
Kishimoto N, Momota Y, Hashimoto Y, Tatsumi S, Ando K, Omasa T, Kotani J (2014) The osteoblastic differentiation ability of human dedifferentiated fat cells is higher than that of adipose stem cells from the buccal fat pad. Clin Oral Investig 18:1893–1901
Knopf F, Hammond C, Chekuru A, Kurth T, Hans S, Weber CW, Mahatma G, Fisher S, Brand M, Schulte-Merker S et al (2011) Bone regenerates via dedifferentiation of osteoblasts in the zebrafish fin. Dev Cell 20:713–724
Kou L, Lu XW, Wu MK, Wang H, Zhang YJ, Sato S, Shen JF (2014) The phenotype and tissue-specific nature of multipotent cells derived from human mature adipocytes. Biochem Biophys Res Commun 444:543–548
Lafont JE (2010) Lack of oxygen in articular cartilage: consequences for chondrocyte biology. Int J Exp Pathol 91:99–106
Lessard J, Côté JA, Lapointe M, Pelletier M, Nadeau M, Marceau S, Biertho L, Tchernof A (2015a) Generation of human adipose stem cells through dedifferentiation of mature adipocytes in ceiling cultures. J Vis Exp 97:e52485
Lessard J, Pelletier M, Biertho L, Biron S, Marceau S, Hould FS, Lebel S, Moustarah F, Lescelleur O, Marceau P et al (2015b) Characterization of dedifferentiating human mature adipocytes from the visceral and subcutaneous fat compartments: fibroblast-activation protein alpha and dipeptidyl peptidase 4 as major components of matrix remodeling. PLoS One 10:e0122065
Li N, Long B, Han W, Yuan S, Wang K (2017) microRNAs: important regulators of stem cells. Stem Cell Res Ther 8:110
Liao Y, Zeng Z, Lu F, Dong Z, Chang Q, Gao J (2015) In vivo dedifferentiation of adult adipose cells. PLoS One 10:e0125254
Lindroos B, Suuronen R, Miettinen S (2011) The potential of adipose stem cells in regenerative medicine. Stem Cell Rev 7:269–291
Marion RM, Strati K, Li H, Tejera A, Schoeftner S, Ortega S, Serrano M, Blasco MA (2009) Telomeres acquire embryonic stem cell characteristics in induced pluripotent stem cells. Cell Stem Cell 4:141–154
Maruyama T, Fukuda N, Matsumoto T, Kano K, Endo M, Kazama M, Kazama T, Ikeda J, Matsuda H, Ueno T et al (2015) Systematic implantation of dedifferentiated fat cells ameliorated monoclonal antibody 1-22-3-induced glomerulonephritis by immunosuppression with increases in TNF-stimulated gene 6. Stem Cell Res Ther 6:80
Matsumoto T, Kano K, Kondo D, Fukuda N, Iribe Y, Tanaka N, Matsubara Y, Sakuma T, Satomi A, Otaki M et al (2008) Mature adipocyte-derived dedifferentiated fat cells exhibit multilineage potential. J Cell Physiol 215:210–222
Maurizi G, Poloni A, Mattiucci D, Santi S, Maurizi A, Izzi V, Giuliani A, Mancini S, Zingaretti MC, Perugini J et al (2017) Human white adipocytes convert into “rainbow” adipocytes in vitro. J Cell Physiol 232:2887–2899
Maurizi G, Babini L, Della Guardia L (2018a) Potential role of microRNAs in the regulation of adipocytes liposecretion and adipose tissue physiology. J Cell Physiol 233:9077–9086
Maurizi G, Petaisto T, Maurizi A, Della Guardia L (2018b) Key-genes regulating the liposecretion process of mature adipocytes. J Cell Physiol 233:3784–3793
Mitchell JB, McIntosh K, Zvonic S, Garrett S, Floyd ZE, Kloster A, Di Halvorsen Y, Storms RW, Goh B, Kilroy G et al (2006) Immunophenotype of human adipose-derived cells: temporal changes in stromal-associated and stem cell-associated markers. Stem Cells (Dayton, Ohio) 24:376–385
Miyazaki T, Kitagawa Y, Toriyama K, Kobori M, Torii S (2005) Isolation of two human fibroblastic cell populations with multiple but distinct potential of mesenchymal differentiation by ceiling culture of mature fat cells from subcutaneous adipose tissue. Differentiation 73:69–78
Nakagami H, Maeda K, Morishita R, Iguchi S, Nishikawa T, Takami Y, Kikuchi Y, Saito Y, Tamai K, Ogihara T et al (2005) Novel autologous cell therapy in ischemic limb disease through growth factor secretion by cultured adipose tissue-derived stromal cells. Arterioscler Thromb Vasc Biol 25:2542–2547
Neelankal JA, Morahan G, Jiang FX (2017) Incomplete re-expression of neuroendocrine progenitor/stem cell markers is a key feature of beta-cell dedifferentiation. J Neuroendocrinol 29(1):1–12
Nistal M, Gonzalez-Peramato P, De Miguel MP (2013) Sertoli cell dedifferentiation in human cryptorchidism and gender reassignment shows similarities between fetal environmental and adult medical treatment estrogen and antiandrogen exposure. Reprod Toxicol (Elmsford, N.Y.) 42:172–179
Nobusue H, Endo T, Kano K (2008) Establishment of a preadipocyte cell line derived from mature adipocytes of GFP transgenic mice and formation of adipose tissue. Cell Tissue Res 332:435–446
Ntambi JM, Young-Cheul K (2000) Adipocyte differentiation and gene expression. J Nutr 130:3122s–3126s
Nur R, Fukuda N, Matsumoto T, Medet J, Kano K, Yamamoto C, Maruyama T, Endo M, Matsumoto K (2008) Implantation of dedifferentiated fat cells ameliorates habu snake venom-induced chronic renal dysfunction in tenascin-C-deficient mice. Nephron Exp Nephrol 110:e91–e98
Obinata D, Matsumoto T, Ikado Y, Sakuma T, Kano K, Fukuda N, Yamaguchi K, Mugishima H, Takahashi S (2011) Transplantation of mature adipocyte-derived dedifferentiated fat (DFAT) cells improves urethral sphincter contractility in a rat model. Int J Urol 18:827–834
Ohta Y, Takenaga M, Tokura Y, Hamaguchi A, Matsumoto T, Kano K, Mugishima H, Okano H, Igarashi R (2008) Mature adipocyte-derived cells, dedifferentiated fat cells (DFAT), promoted functional recovery from spinal cord injury-induced motor dysfunction in rats. Cell Transplant 17:877–886
Oki Y, Watanabe S, Endo T, Kano K (2008) Mature adipocyte-derived dedifferentiated fat cells can trans-differentiate into osteoblasts in vitro and in vivo only by all-trans retinoic acid. Cell Struct Funct 33:211–222
Okita N, Honda Y, Kishimoto N, Liao W, Azumi E, Hashimoto Y, Matsumoto N (2015) Supplementation of strontium to a chondrogenic medium promotes chondrogenic differentiation of human dedifferentiated fat cells. Tissue Eng. Part A 21:1695–1704
Ono H, Oki Y, Bono H, Kano K (2011) Gene expression profiling in multipotent DFAT cells derived from mature adipocytes. Biochem Biophys Res Commun 407:562–567
Paksa A a RJ (2017) The epigenetic basis of cellular plasticity. Curr Opin Cell Biol 49:116–122
Peng X, Song T, Hu X, Zhou Y, Wei H, Peng J, Jiang S (2015) Phenotypic and functional properties of porcine dedifferentiated fat cells during the long-term culture in vitro. Biomed Res Int 2015:673651
Perrini S, Ficarella R, Picardi E, Cignarelli A, Barbaro M, Nigro P, Peschechera A, Palumbo O, Carella M, De Fazio M et al (2013) Differences in gene expression and cytokine release profiles highlight the heterogeneity of distinct subsets of adipose tissue-derived stem cells in the subcutaneous and visceral adipose tissue in humans. PLoS One 8:e57892
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR (1999) Multilineage potential of adult human mesenchymal stem cells. Science (New York, N.Y.) 284:143–147
Planat-Benard V, Silvestre JS, Cousin B, Andre M, Nibbelink M, Tamarat R, Clergue M, Manneville C, Saillan-Barreau C, Duriez M et al (2004) Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation 109:656–663
Poloni A, Maurizi G, Leoni P, Serrani F, Mancini S, Frontini A, Zingaretti MC, Siquini W, Sarzani R, Cinti S (2012) Human dedifferentiated adipocytes show similar properties to bone marrow-derived mesenchymal stem cells. Stem Cells (Dayton, Ohio) 30:965–974
Saler M, Caliogna L, Botta L, Benazzo F, Riva F, Gastaldi G (2017) hASC and DFAT, multipotent stem cells for regenerative medicine: a comparison of their potential differentiation in vitro. Int J Mol Sci 18(12):2699
Shah M, George RL, Evancho-Chapman MM, Zhang G (2016) Current challenges in dedifferentiated fat cells research. Organogenesis 12:119–127
Shen JF, Sugawara A, Yamashita J, Ogura H, Sato S (2011) Dedifferentiated fat cells: an alternative source of adult multipotent cells from the adipose tissues. Int J Oral Sci 3:117–124
Shigematsu M, Watanabe H, Sugihara H (1999) Proliferation and differentiation of unilocular fat cells in the bone marrow. Cell Struct Funct 24:89–100
Shimizu M, Matsumoto T, Kikuta S, Ohtaki M, Kano K, Taniguchi H, Saito S, Nagaoka M, Tokuhashi Y (2018) Transplantation of dedifferentiated fat cell-derived micromass pellets contributed to cartilage repair in the rat osteochondral defect model. J Orthop Sci 23:688–696
Shoshani O, Zipori D (2011) Mammalian cell dedifferentiation as a possible outcome of stress. Stem Cell Rev 7:488–493
Shugart EC, Levenson AS, Constance CM, Umek RM (1995) Differential expression of gas and gadd genes at distinct growth arrest points during adipocyte development. Cell Growth Differ 6:1541–1547
Soejima K, Kashimura T, Asami T, Kazama T, Matsumoto T, Nakazawa H (2015) Effects of mature adipocyte-derived dedifferentiated fat (DFAT) cells on generation and vascularisation of dermis-like tissue after artificial dermis grafting. J Plast Surg Hand Surg 49:25–31
Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O, Blomqvist L, Hoffstedt J, Naslund E, Britton T et al (2008) Dynamics of fat cell turnover in humans. Nature 453:783–787
Steevens TA, Sussex IM (1989) Patterns in plant development. Cambridge university press, New York, United States of America
Sugihara H, Yonemitsu N, Miyabara S, Yun K (1986) Primary cultures of unilocular fat cells: characteristics of growth in vitro and changes in differentiation properties. Differentiation 31:42–49
Sugihara H, Funatsumaru S, Yonemitsu N, Miyabara S, Toda S, Hikichi Y (1989) A simple culture method of fat cells from mature fat tissue fragments. J Lipid Res 30:1987–1995
Sun W, Wang H, Li Y, Zhou X, Teng Y, Chen J (2013) Acquisition of pig intramuscular preadipocytes through dedifferentiation of mature adipocytes and establishment of optimal induction conditions. Genet Mol Res: GMR 12:5926–5936
Takahashi K, Yamanaka S (2016) A decade of transcription factor-mediated reprogramming to pluripotency. Nat Rev Mol Cell Biol 17:183–193
Talchai C, Xuan S, Lin HV, Sussel L, Accili D (2012) Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell 150:1223–1234
Tang Y, Tang W, Lin Y, Long J, Wang H, Liu L, Tian W (2008) Combination of bone tissue engineering and BMP-2 gene transfection promotes bone healing in osteoporotic rats. Cell Biol Int 32:1150–1157
Toren-Haritan G, Efrat S (2015) TGFbeta pathway inhibition redifferentiates human pancreatic islet beta cells expanded in vitro. PLoS One 10:e0139168
Ullah M, Stich S, Notter M, Eucker J, Sittinger M, Ringe J (2013) Transdifferentiation of mesenchymal stem cells-derived adipogenic-differentiated cells into osteogenic- or chondrogenic-differentiated cells proceeds via dedifferentiation and have a correlation with cell cycle arresting and driving genes. Differentiation 85:78–90
Wang Z, York NW, Nichols CG, Remedi MS (2014) Pancreatic beta cell dedifferentiation in diabetes and redifferentiation following insulin therapy. Cell Metab 19:872–882
Wang QA, Song A, Chen W, Schwalie PC, Zhang F, Vishvanath L, Jiang L, Ye R, Shao M, Tao C et al (2018) Reversible de-differentiation of mature white adipocytes into preadipocyte-like precursors during lactation. Cell Metab 28:282-288.e283
Wei S, Du M, Jiang Z, Duarte MS, Fernyhough-Culver M, Albrecht E, Will K, Zan L, Hausman GJ, Elabd EM et al (2013) Bovine dedifferentiated adipose tissue (DFAT) cells: DFAT cell isolation. Adipocyte 2:148–159
Weinberg N, Ouziel-Yahalom L, Knoller S, Efrat S, Dor Y (2007) Lineage tracing evidence for in vitro dedifferentiation but rare proliferation of mouse pancreatic beta-cells. Diabetes 56:1299–1304
White MG, Shaw JA, Taylor R (2016) Type 2 diabetes: the pathologic basis of reversible beta-cell dysfunction. Diabetes Care 39:2080–2088
Yagi K, Kondo D, Okazaki Y, Kano K (2004) A novel preadipocyte cell line established from mouse adult mature adipocytes. Biochem Biophys Res Commun 321:967–974
Yoon E, Dhar S, Chun DE, Gharibjanian NA, Evans GR (2007) In vivo osteogenic potential of human adipose-derived stem cells/poly lactide-co-glycolic acid constructs for bone regeneration in a rat critical-sized calvarial defect model. Tissue Eng 13:619–627
Zhang HH, Kumar S, Barnett AH, Eggo MC (2000) Ceiling culture of mature human adipocytes: use in studies of adipocyte functions. J Endocrinol 164:119–128
Zoico E, Darra E, Rizzatti V, Budui S, Franceschetti G, Mazzali G, Rossi AP, Fantin F, Menegazzi M, Cinti S et al (2016) Adipocytes WNT5a mediated dedifferentiation: a possible target in pancreatic cancer microenvironment. Oncotarget 7:20223–20235
Zoico E, Darra E, Rizzatti V, Tebon M, Franceschetti G, Mazzali G, Rossi AP, Fantin F, Zamboni M (2018) Role of adipose tissue in melanoma cancer microenvironment and progression. Int J Obes (2005) 42:344–352
Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, Alfonso ZC, Fraser JK, Benhaim P, Hedrick MH (2002) Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell 13:4279–4295
Acknowledgments
Work performed on DFAT cells has been supported by discovery grants from the Natural Sciences and Engineering Research Council of Canada (2011-371697, 2016-05249, 2017-05825) to AT. JAC was funded by a doctoral fellowship from Natural Sciences and Engineering Council of Canada. AL was funded by an undergraduate Natural Sciences and Engineering Council of Canada scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
AT receives funding from Johnson & Johnson Medical Companies and Medtronic for studies unrelated to this manuscript. The other authors declare no conflict of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Côté, J.A., Ostinelli, G., Gauthier, MF. et al. Focus on dedifferentiated adipocytes: characteristics, mechanisms, and possible applications. Cell Tissue Res 378, 385–398 (2019). https://doi.org/10.1007/s00441-019-03061-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-019-03061-3