Abstract
Familial neurohypophysial diabetes insipidus (FNDI), characterized by delayed-onset progressive polyuria and loss of arginine vasopressin (AVP) neuron, is an autosomal dominant disorder caused by AVP gene mutations. We previously generated a knock-in mouse model for FNDI, which recapitulated the phenotype of human FNDI. To address the mechanisms underlying AVP neuron loss, we subjected FNDI mice to intermittent water deprivation, which accelerated the phenotype and induced AVP neuron loss within a relative short period. Electron microscopic analyses revealed that aggregates were confined to a sub-compartment of the endoplasmic reticulum (ER), ER-associated compartment (ERAC), in AVP neurons of FNDI mice under normal conditions. In contrast, aggregates scattered throughout the dilated ER lumen, and phagophores, autophagosome precursors, emerged and surrounded the ER containing scattered aggregates in FNDI mice subjected to water deprivation for 4 weeks, suggesting that failure of ERAC formation leads to autophagy induction for degradation of aggregates. Furthermore, the cytoplasm was entirely occupied with large vacuoles in AVP neurons of FNDI mice subjected to water deprivation for 12 weeks, at which stage 30–40% of AVP neurons were lost. Our data demonstrated that although autophagy should primarily be a protective mechanism, continuous autophagy leads to gradual loss of organelles including ER, resulting in autophagy-associated cell death of AVP neurons in FNDI mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arginine vasopressin (AVP), a highly conserved nonapeptide throughout various species, is synthesized principally in the hypothalamic supraoptic (SON), paraventricular (PVN), and accessory nuclei. Magnocellular AVP neurons of the SON and PVN project their axons to the posterior pituitary and provide systemic AVP supply by release into blood stream (Swanson and Sawchenko 1983). Systemic AVP plays an essential role in the homeostasis of water balance via promoting reabsorption of free water through the AVP V2 receptor and associated aquaporin 2 in the kidney. AVP synthesis and release are regulated mainly by plasma osmolality under physiological conditions (Bisset and Chowdrey 1988; Brownstein et al. 1980; Burbach et al. 2001). Only 1–2% increases in serum sodium concentration significantly induce AVP release as well as AVP gene transcription in the SON and PVN (Arima et al. 1999). AVP deficiency causes neurohypophysial diabetes insipidus, a disorder presented with an increase in urine volume and water intake.
Familial neurohypophysial diabetes insipidus (FNDI) is an autosomal dominant disorder caused by mutations in the AVP gene. More than 80 causal mutations have been reported until now, and the majority of them are located in the coding region of neurophysin II (NPII), an AVP carrier protein (Arima et al. 2016). FNDI is characterized by delayed-onset progressive polyuria and eventual AVP neuron loss. Although the carriers manifest no symptom at birth, polyuria and polydipsia appear within several months or years after birth, despite the existence of one normal allele (Babey et al. 2011). Autopsy studies reported AVP neuron loss in the hypothalamus of patients with FNDI (Bergeron et al. 1991; Braverman et al. 1965; Nagai et al. 1984).
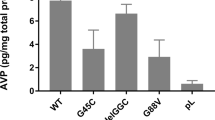
The mechanisms underlying the phenotype of FNDI have been extensively investigated in cell lines. Mutant AVP precursors reportedly accumulate and aggregate in the endoplasmic reticulum (ER) (Beuret et al. 2017; Birk et al. 2009; Ito and Jameson 1997; Nijenhuis et al. 1999), which leads to defective intracellular trafficking of wild-type AVP protein (Ito et al. 1999) and a decrease in cell viability (Castino et al. 2005a; Castino et al. 2005b; Ito and Jameson 1997). Furthermore, autophagy has been suggested to have a bifunctional role in cell survival and death in a transfected cell line expressing mutant NPII (Castino et al. 2005a; Castino et al. 2005b).
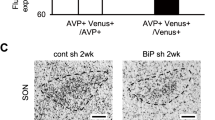
Three animal models, including one from our group, have been reported to decipher the pathophysiology of FNDI in vivo (Hayashi et al. 2009; Russell et al. 2003; Si-Hoe et al. 2000). All these animal models harbor a Cys98stop mutation (previously called Cys67stop) in the Avp gene, which causes FNDI in humans (Nagasaki et al. 1995). Si-Hoe and colleagues first reported an animal model for FNDI using a conventional transgenic approach (Si-Hoe et al. 2000) and showed no differences in urine volume compared with a wild-type line under normal conditions due to a possible low transgene expression, whereas urine volume in transgenic rats significantly increased under chronic intermittent dehydration, which ensured sustained transgene expression (Si-Hoe et al. 2000). Pathological examination revealed that mutant NPII accumulated in the ER of AVP neurons (Si-Hoe et al. 2000), and upregulated lysosomal markers were colocalized with mutant NPII under chronic intermittent dehydration (Davies and Murphy 2002), suggesting that accumulated mutant NPII in the ER could be a target for lysosomal degradation by autophagy. However, AVP neuron loss in the transgenic rat model was not reported. Russell and colleagues generated an alternative knock-in mouse line harboring the Cys98stop mutation (Russell et al. 2003). The heterozygous mice presented delayed-onset and progressive polyuria accompanied by low levels of plasma AVP and urine osmolality, as was found in patients with FNDI (Russell et al. 2003). Furthermore, the heterozygous mice also exhibited a selective and progressive AVP neuron loss in the SON and PVN (Russell et al. 2003). Although the induction of immunoglobulin heavy chain binding protein (BiP), an ER chaperone, was observed in the AVP neurons of the heterozygous mice (Russell et al. 2003), suggesting that ER stress could be related to the pathogenesis of FNDI, the precise mechanisms underlying AVP neuron loss in FNDI still remained to be elucidated in this report.
In analogy to Russell et al. (2003), we also generated a knock-in mice model for FNDI harboring the Cys98stop mutation (Hayashi et al. 2009). The heterozygous mice also manifested delayed-onset progressive polyuria due to AVP deficiency and eventual AVP neuron loss, which fully recapitulated the phenotype of FNDI in humans (Hayashi et al. 2009). Decreased AVP axonal staining and pituitary AVP contents suggested that axonal AVP transport was impaired (Hayashi et al. 2009). Moreover, mutant NPII accumulation in the ER of AVP neurons was parallel to phenotype progression of FNDI mice (Hayashi et al. 2009; Hiroi et al. 2010). Further investigation revealed that sustained autophagy induced by ER stress led to AVP neuron loss in FNDI mice (Hagiwara et al. 2014). In the present review, we demonstrate the mechanisms of cell death of AVP neurons in FNDI based on our findings in FNDI mice.
Phenotype acceleration
Capturing the feature of cell death is difficult under conditions in which cell death progresses gradually over time, as is the case for FNDI. Therefore, simultaneous changes of AVP neurons towards cell death are essential to decipher the mechanisms of AVP neuron loss. To do so, we subjected FNDI mice to intermittent water deprivation (WD), which promoted mutant NPII accumulation in the ER of AVP neurons. As expected, urine volume started to increase at 4 weeks after WD initiation (Hagiwara et al. 2014). Furthermore, whereas the number of AVP neurons in the SON of 3-month-old FNDI mice subjected to WD for 4 weeks did not differ from control, 2 months later, that of FNDI mice subjected to WD for 12 weeks decreased by 30–40% (Hagiwara et al. 2014). Thus, we succeeded in the establishment of an experimental system of FNDI mice for analysis of AVP neuron loss, in which AVP neurons were dying within a relatively short period.
ERAC formation
We investigated morphological changes of AVP neurons in FNDI mice before and after the initiation of AVP neuron loss. Electron microscopic analyses demonstrated massive and electron-dense aggregates in the AVP neurons of 3-month-old FNDI mice under normal conditions (Fig. 1a). It is of note that the lumen of the ER adjacent to massive aggregates was preserved intact (Fig. 1b). We also found that irregular-shaped aggregates confined to some compartments of the ER (Fig. 1c), which communicated with intact ER lumen (Fig. 1d, arrowheads). These observations indicate that aggregates are confined to a certain compartment of the ER. Several mutant secretory and transmembrane proteins are reportedly segregated into specialized sub-compartments of the ER in vitro (Granell et al. 2008; Huyer et al. 2004; Ito et al. 2012; Valetti et al. 1991). These structures were named in each report as Russell body (Valetti et al. 1991), ER-derived protective organelle (Ito et al. 2012), or ER-associated compartment (Huyer et al. 2004) (hereinafter, referred to as ERAC). Some studies reported that ERAC formation itself does not perturb normal protein processing through the ER nor induce unfolded protein response (Granell et al. 2008; Huyer et al. 2004). Consistent with these previous studies in vitro, BiP expression levels in the SON were comparable between FNDI and wild-type mice under normal conditions despite the existence of massive aggregates accumulated in the ER of AVP neurons in FNDI mice. This indicates that ERAC formation alleviates ER stress caused by mutant NPII accumulation in the ER (Hagiwara et al. 2014). In contract to the observations under normal conditions, aggregates scattered throughout the dilated ER lumen in AVP neurons of 3-month-old FNDI mice subjected to WD for 4 weeks (Fig. 1e, f). The failure of ERAC formation resulted in increase in ER stress as demonstrated by elevated BiP expression in the SON of FNDI mice compared with WT mice subjected to WD (Hagiwara et al. 2014). ERAC formation was also observed in AVP neurons of 5-month-old (Fig. 2a) and 12-month-old FNDI mice (Hayashi et al. 2009) under normal conditions. However, at these stages, the lumen of the ER adjacent to ERACs was dilated (Fig. 2b). Furthermore, ERAC disruption, as seen in 3-month-old FNDI mice subjected to WD for 4 weeks, was also found in 5-month-old (Fig. 2c, d) and 12-month-old FNDI mice (Hayashi et al. 2009) under normal conditions. These findings suggest that the failure of ERAC formation occurs over time even under normal conditions.
Electron microscopic analysis of AVP neurons in 3-month-old FNDI mice. AVP neurons of the SON in 3-month-old FNDI mice under normal conditions (a–d) and in those subjected to water deprivation for 4 weeks (e–h). Higher magnification images of boxed areas in a, c, e, g are shown in b, d, f, h, respectively. The arrowheads in d indicate irregular-shaped aggregates confined to a compartment of the ER, which communicates with intact ER lumen, and those in h indicate phagophores engulfing the ER which contains scattered aggregates. Scale bars, 2 μm (a, e, g), 1 μm (c). Referred to Hagiwara et al. (2014)
Electron microscopic analysis of AVP neurons in 5-month-old FNDI mice. AVP neurons of the SON in 5-month-old FNDI mice under normal conditions (a–d) and in those subjected to water deprivation for 12 weeks (e–h). Higher magnification images of boxed areas in a, c, e are shown in b, d, f, respectively. Scale bars, 2 μm (a, e, g, h), 1 μm (c). Referred to Hagiwara et al. (2014)
Autophagy induction
Further electron microscopic observations revealed that phagophores, double-membrane structures of autophagosome precursors, emerged in AVP neurons of 3-month-old FNDI mice subjected to WD for 4 weeks (Fig. 1g). It is also noteworthy that the phagophores surrounded the ER with scattered aggregates (Fig. 1h). To further confirm autophagy induction in the AVP neurons, we utilized GFP-LC3 transgenic mice, reporting autophagosome formation, crossed with FNDI mice. Although no GFP signals were detected in AVP neurons in 3-month-old FNDI;GFP-LC3 mice under normal conditions, GFP signals were elicited in the mice subjected to WD for 4 weeks, indicating that autophagosome formation is induced in FNDI mice after WD (Hagiwara et al. 2014). Moreover, p62, a receptor for ubiquitinated cargos to deliver to autophagosomes in selective autophagy, was upregulated and colocalized with mutant NPII in AVP neurons of FNDI mice subjected to WD, suggesting that selective autophagy is induced to degrade mutant NPII (Hagiwara et al. 2014). These findings are consistent with previous studies both in vitro (Castino et al. 2005a; Castino et al. 2005b; Castino et al. 2008) and in vivo (Davies and Murphy 2002; Si-Hoe et al. 2000) reporting a possible involvement of autophagy in the pathogenesis of FNDI. Our data suggest that autophagy is induced after ERAC disruption resulting in increased ER stress and, that the targets of autophagy is not only aggregates alone but also the ER (ER-phagy). ER stress per se is previously shown to trigger autophagy in vitro (Ogata et al. 2006; Yorimitsu et al. 2006). We also confirmed that an ER stressor induced autophagy in hypothalamic organotypic cultures of GFP-LC3 transgenic mice (Hagiwara et al. 2014). Although ER-phagy has been demonstrated to be induced in yeast by ER stressors (Bernales et al. 2006) and in cell line-transfected mutant α1-antitrypsin (Kamimoto et al. 2006; Teckman and Perlmutter 2000), our finding in FNDI mice is the first evidence of ER-phagy in neurons in vivo.
Autophagy-associated cell death
Electron microscopic analyses in AVP neurons of 5-month-old FNDI mice subjected to WD for 12 weeks, at which stage 30–40% of AVP neurons were lost, revealed that vacuoles were found throughout the cytoplasm of AVP neurons whereas the nuclear structure was relatively preserved (Fig. 2e, f). Furthermore, very large vacuoles containing aggregates inside were also observed in some AVP neurons (Fig. 2g, h). The canonical classifications of cell death based on the morphology are apoptosis, necrosis, and autophagic cell death (Hotchkiss et al. 2009; Kroemer et al. 2009). Among them, autophagic cell death is morphologically defined as the absence of chromatin condensation with massive autophagic vacuolization of the cytoplasm (Kroemer and Levine 2008), which is consistent with our electron microscopic observations in AVP neurons of FNDI mice. Since our data demonstrated that autophagy was induced in AVP neurons of FNDI mice from 4 weeks after WD initiation, the cell death of AVP neurons is suggested to be associated with autophagy.
Autophagy and even ER-phagy shown in FNDI mice should primarily be a protective and adaptive mechanism by which misfolded proteins are degraded in AVP neurons. Indeed, an autophagy inducer rapamycin reduces aggregates; on the contrary, chloroquine, which inhibits autophagic degradation via suppression of lysosomal function, increases aggregates in AVP neurons of FNDI mice (unpublished data). On the other hand, if excessively induced autophagy continues over time in order to cope with protein aggregates, substantial amount of ER could be lost, resulting in the disruption of ER homeostasis. Under these conditions, organelles other than ER would also be damaged and degraded via autophagy. Electron microscopic analyses revealed that the cytoplasm was entirely occupied with large vacuoles in remaining AVP neurons of 5-month-old FNDI mice subjected to WD for 12 weeks, while 30–40% of AVP neurons died. We interpret these data as an evidence for AVP neuron loss through “autophagy-associated cell death” (Kroemer and Levine 2008), a term that is more appropriate than “autophagic cell death” from the aspect of the initially beneficial role of autophagy (Pierzynowska et al. 2018) in AVP neurons of FNDI mice.
Possible dysfunction of oxytocin system in FNDI
Oxytocin (OT) is a nonapeptide synthesized in the SON, PVN, and accessory nuclei in the hypothalamus in analogy with AVP (Swanson and Sawchenko 1983). OT as well as AVP is transported through their axons to the posterior pituitary from which OT is released into blood stream, and systemic OT plays canonical roles in milk ejection and uterine contraction. OT neurons also project their axons to diverse forebrain regions where social behaviors are involved and OT receptors are identified (Grinevich et al. 2016; Knobloch et al. 2012). The axonal OT release in various brain regions far from the hypothalamus provides a basis for OT effects on wide-ranging types of social behaviors (Chini et al. 2017).
Impairment of OT secretion has been reported in various animal models for acquired neurohypophysial diabetes insipidus (Bernal et al. 2016) and patients with this disease (Daughters et al. 2017). Conversely, OT system has been assumed to be preserved in FNDI so far. However, OT neurons might be affected negatively by adjacent dying AVP neurons and/or their surrounding environment in FNDI. Indeed, a postmortem morphological examination of a patient with FNDI reportedly demonstrated that neurons were lost by over 95% in the SON (Green et al. 1967). Furthermore, patients with FNDI were reported to present some social deficits (Bruins et al. 2006), implying the possibility of impaired OT neuron system in FNDI. In addition to possible OT neuron loss, axonal OT transport and release might also be impaired in FNDI, as with the impaired AVP axonal transport in FNDI mice. Although further studies are required, this could address the mechanism of social deficits in FNDI.
Conclusions and perspectives
As depicted in Fig. 3, showing putative process and mechanisms of cell death of AVP neurons in FNDI, accumulated and aggregated mutant NPII are confined to a sub-compartment of the ER (i.e., ERAC) in AVP neurons, which is assumed to be a protective cellular mechanism for maintenance of ER homeostasis. Subsequently, failure of the aggregate compartmentation induces autophagy to degrade aggregates, whereas the continuous autophagy leads to gradual loss of organelles including ER, resulting in autophagy-associated cell death of AVP neurons. Further investigations of molecular mechanisms underlying the formation and disruption of ERAC and the induction of autophagy and autophagy-associated cell death of AVP neurons remain interesting future works.
Putative schema of the process and mechanisms of cell death of AVP neurons in FNDI. Accumulated and aggregated mutant NPII are confined to a sub-compartment of the ER, so called ER-associated compartment (ERAC), in AVP neurons. Subsequently, ERAC disruption induces autophagy. Furthermore, the continuous autophagy leads to gradual loss of organelles including ER, resulting in autophagy-associated cell death of AVP neurons
Regarding possible impairment of OT system in FNDI, further studies remain to be conducted to elucidate whether or not OT neurons are also affected in both patients afflicted with FNDI and animal models for this disease. Precise anatomical analyses of OT neurons and their projections to extrahypothalamic socially relevant brain regions and subsequent behavioral studies in FNDI mice should provide an insight into this issue.
References
Arima H, Kondo K, Kakiya S, Nagasaki H, Yokoi H, Yambe Y, Murase T, Iwasaki Y, Oiso Y (1999) Rapid and sensitive vasopressin heteronuclear RNA responses to changes in plasma osmolality. J Neuroendocrinol 11:337–341
Arima H, Azuma Y, Morishita Y, Hagiwara D (2016) Central diabetes insipidus. Nagoya J Med Sci 78:349–358
Babey M, Kopp P, Robertson GL (2011) Familial forms of diabetes insipidus: clinical and molecular characteristics. Nat Rev Endocrinol 7:701–714
Bergeron C, Kovacs K, Ezrin C, Mizzen C (1991) Hereditary diabetes insipidus: an immunohistochemical study of the hypothalamus and pituitary gland. Acta Neuropathol 81:345–348
Bernal A, Mahía J, Puerto A (2016) Animal models of central diabetes insipidus: human relevance of acquired beyond hereditary syndromes and the role of oxytocin. Neurosci Biobehav Rev 66:1–14
Bernales S, McDonald KL, Walter P (2006) Autophagy counterbalances endoplasmic reticulum expansion during the unfolded protein response. PLoS Biol 4:e423
Beuret N, Hasler F, Prescianotto-Baschong C, Birk J, Rutishauser J, Spiess M (2017) Amyloid-like aggregation of provasopressin in diabetes insipidus and secretory granule sorting. BMC Biol 15:5
Birk J, Friberg MA, Prescianotto-Baschong C, Spiess M, Rutishauser J (2009) Dominant pro-vasopressin mutants that cause diabetes insipidus form disulfide-linked fibrillar aggregates in the endoplasmic reticulum. J Cell Sci 122:3994–4002
Bisset GW, Chowdrey HS (1988) Control of release of vasopressin by neuroendocrine reflexes. Q J Exp Physiol 73:811–872
Braverman LE, Mancini JP, McGoldrick DM (1965) Hereditary idiopathic diabetes insipidus. A case report with autopsy findings. Ann Intern Med 63:503–508
Brownstein MJ, Russell JT, Gainer H (1980) Synthesis, transport, and release of posterior pituitary hormones. Science 207:373–378
Bruins J, Kovács GL, Abbes AP, Burbach JP, van den Akker EL, Engel H, Franken AA, de Wied D (2006) Minor disturbances in central nervous system function in familial neurohypophysial diabetes insipidus. Psychoneuroendocrinology 31:80–91
Burbach JP, Luckman SM, Murphy D, Gainer H (2001) Gene regulation in the magnocellular hypothalamo-neurohypophysial system. Physiol Rev 81:1197–1267
Castino R, Davies J, Beaucourt S, Isidoro C, Murphy D (2005a) Autophagy is a prosurvival mechanism in cells expressing an autosomal dominant familial neurohypophyseal diabetes insipidus mutant vasopressin transgene. FASEB J 19:1021–1023
Castino R, Isidoro C, Murphy D (2005b) Autophagy-dependent cell survival and cell death in an autosomal dominant familial neurohypophyseal diabetes insipidus in vitro model. FASEB J 19:1024–1026
Castino R, Thepparit C, Bellio N, Murphy D, Isidoro C (2008) Akt induces apoptosis in neuroblastoma cells expressing a C98X vasopressin mutant following autophagy suppression. J Neuroendocrinol 20:1165–1175
Chini B, Verhage M, Grinevich V (2017) The action radius of oxytocin release in the mammalian CNS: from single vesicles to behavior. Trends Pharmacol Sci 38:982–991
Daughters K, Manstead ASR, Rees DA (2017) Hypopituitarism is associated with lower oxytocin concentrations and reduced empathic ability. Endocrine 57:166–174
Davies J, Murphy D (2002) Autophagy in hypothalamic neurones of rats expressing a familial neurohypophysial diabetes insipidus transgene. J Neuroendocrinol 14:629–637
Granell S, Baldini G, Mohammad S, Nicolin V, Narducci P, Storrie B (2008) Sequestration of mutated alpha1-antitrypsin into inclusion bodies is a cell-protective mechanism to maintain endoplasmic reticulum function. Mol Biol Cell 19:572–586
Green JR, Buchan GC, Alvord EC, Swanson AG (1967) Hereditary and idiopathic types of diabetes insipidus. Brain 90:707–714
Grinevich V, Knobloch-Bollmann HS, Eliava M, Busnelli M, Chini B (2016) Assembling the puzzle: pathways of oxytocin signaling in the brain. Biol Psychiatry 79:155–164
Hagiwara D, Arima H, Morishita Y, Wenjun L, Azuma Y, Ito Y, Suga H, Goto M, Banno R, Sugimura Y, Shiota A, Asai N, Takahashi M, Oiso Y (2014) Arginine vasopressin neuronal loss results from autophagy-associated cell death in a mouse model for familial neurohypophysial diabetes insipidus. Cell Death Dis 5:e1148
Hayashi M, Arima H, Ozaki N, Morishita Y, Hiroi M, Nagasaki H, Kinoshita N, Ueda M, Shiota A, Oiso Y (2009) Progressive polyuria without vasopressin neuron loss in a mouse model for familial neurohypophysial diabetes insipidus. Am J Physiol Regul Integr Comp Physiol 296:R1641–R1649
Hiroi M, Morishita Y, Hayashi M, Ozaki N, Sugimura Y, Nagasaki H, Shiota A, Oiso Y, Arima H (2010) Activation of vasopressin neurons leads to phenotype progression in a mouse model for familial neurohypophysial diabetes insipidus. Am J Physiol Regul Integr Comp Physiol 298:R486–R493
Hotchkiss RS, Strasser A, McDunn JE, Swanson PE (2009) Cell death. N Engl J Med 361:1570–1583
Huyer G, Longsworth GL, Mason DL, Mallampalli MP, McCaffery JM, Wright RL, Michaelis S (2004) A striking quality control subcompartment in Saccharomyces cerevisiae: the endoplasmic reticulum-associated compartment. Mol Biol Cell 15:908–921
Ito M, Jameson JL (1997) Molecular basis of autosomal dominant neurohypophyseal diabetes insipidus. Cellular toxicity caused by the accumulation of mutant vasopressin precursors within the endoplasmic reticulum. J Clin Invest 99:1897–1905
Ito M, Yu RN, Jameson JL (1999) Mutant vasopressin precursors that cause autosomal dominant neurohypophyseal diabetes insipidus retain dimerization and impair the secretion of wild-type proteins. J Biol Chem 274:9029–9037
Ito D, Yagi T, Ikawa M, Suzuki N (2012) Characterization of inclusion bodies with cytoprotective properties formed by seipinopathy-linked mutant seipin. Hum Mol Genet 21:635–646
Kamimoto T, Shoji S, Hidvegi T, Mizushima N, Umebayashi K, Perlmutter DH, Yoshimori T (2006) Intracellular inclusions containing mutant alpha1-antitrypsin Z are propagated in the absence of autophagic activity. J Biol Chem 281:4467–4476
Knobloch HS, Charlet A, Hoffmann LC, Eliava M, Khrulev S, Cetin AH, Osten P, Schwarz MK, Seeburg PH, Stoop R, Grinevich V (2012) Evoked axonal oxytocin release in the central amygdala attenuates fear response. Neuron 73:553–566
Kroemer G, Levine B (2008) Autophagic cell death: the story of a misnomer. Nat Rev Mol Cell Biol 9:1004–1010
Kroemer G, Galluzzi L, Vandenabeele P, Abrams J, Alnemri ES, Baehrecke EH, Blagosklonny MV, El-Deiry WS, Golstein P, Green DR, Hengartner M, Knight RA, Kumar S, Lipton SA, Malorni W, Nuñez G, Peter ME, Tschopp J, Yuan J, Piacentini M, Zhivotovsky B, Melino G, NCoCD (2009) Classification of cell death: recommendations of the nomenclature committee on cell death 2009. Cell Death Differ 16:3–11
Nagai I, Li CH, Hsieh SM, Kizaki T, Urano Y (1984) Two cases of hereditary diabetes insipidus, with an autopsy finding in one. Acta Endocrinol 105:318–323
Nagasaki H, Ito M, Yuasa H, Saito H, Fukase M, Hamada K, Ishikawa E, Katakami H, Oiso Y (1995) Two novel mutations in the coding region for neurophysin-II associated with familial central diabetes insipidus. J Clin Endocrinol Metab 80:1352–1356
Nijenhuis M, Zalm R, Burbach JP (1999) Mutations in the vasopressin prohormone involved in diabetes insipidus impair endoplasmic reticulum export but not sorting. J Biol Chem 274:21200–21208
Ogata M, Hino S, Saito A, Morikawa K, Kondo S, Kanemoto S, Murakami T, Taniguchi M, Tanii I, Yoshinaga K, Shiosaka S, Hammarback JA, Urano F, Imaizumi K (2006) Autophagy is activated for cell survival after endoplasmic reticulum stress. Mol Cell Biol 26:9220–9231
Pierzynowska K, Gaffke L, Cyske Z, Puchalski M, Rintz E, Bartkowski M, Osiadły M, Pierzynowski M, Mantej J, Piotrowska E, Węgrzyn G (2018) Autophagy stimulation as a promising approach in treatment of neurodegenerative diseases. Metab Brain Dis. https://doi.org/10.1007/s11011-018-0214-6
Russell TA, Ito M, Yu RN, Martinson FA, Weiss J, Jameson JL (2003) A murine model of autosomal dominant neurohypophyseal diabetes insipidus reveals progressive loss of vasopressin-producing neurons. J Clin Invest 112:1697–1706
Si-Hoe SL, De Bree FM, Nijenhuis M, Davies JE, Howell LM, Tinley H, Waller SJ, Zeng Q, Zalm R, Sonnemans M, Van Leeuwen FW, Burbach JP, Murphy D (2000) Endoplasmic reticulum derangement in hypothalamic neurons of rats expressing a familial neurohypophyseal diabetes insipidus mutant vasopressin transgene. FASEB J 14:1680–1684
Swanson LW, Sawchenko PE (1983) Hypothalamic integration: organization of the paraventricular and supraoptic nuclei. Annu Rev Neurosci 6:269–324
Teckman JH, Perlmutter DH (2000) Retention of mutant alpha(1)-antitrypsin Z in endoplasmic reticulum is associated with an autophagic response. Am J Physiol Gastrointest Liver Physiol 279:G961–G974
Valetti C, Grossi CE, Milstein C, Sitia R (1991) Russell bodies: a general response of secretory cells to synthesis of a mutant immunoglobulin which can neither exit from, nor be degraded in, the endoplasmic reticulum. J Cell Biol 115:983–994
Yorimitsu T, Nair U, Yang Z, Klionsky DJ (2006) Endoplasmic reticulum stress triggers autophagy. J Biol Chem 281:30299–30304
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hagiwara, D., Grinevich, V. & Arima, H. A novel mechanism of autophagy-associated cell death of vasopressin neurons in familial neurohypophysial diabetes insipidus. Cell Tissue Res 375, 259–266 (2019). https://doi.org/10.1007/s00441-018-2872-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-018-2872-4