Abstract
Deep brain stimulation (DBS), arguably the greatest therapeutic advancement in the treatment of Parkinson’s disease since dopamine replacement therapy, is now routinely used. While the exact mechanisms by which DBS works still remain unknown, over the past three decades since it was first described, we have gained significant insight into several of the processes involved. Though often overlooked in this regard, increasing numbers of postmortem and autopsy studies are contributing significantly to our understanding. In this manuscript, we review the literature involving the pathological findings from autopsies in patients who have undergone deep brain stimulation surgeries for Parkinson’s disease. The major results show that multiple stereotactic targeting methods can be accurate at placing leads in the desired nuclei that help with clinically effective results, that perioperative complications and inaccurate diagnosis as determined by autopsy can lead to suboptimal stimulation effect and that the normal long-term effects of chronic stimulation include fibrosis around the electrodes and a mild immune response. In addition, recent results suggest mechanisms by which DBS might be effective in Parkinson’s disease i.e., through rescuing pathological changes in microvasculature and by promoting the proliferation of neural progenitor cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deep brain stimulation (DBS) has been shown in multiple randomized clinical trials to significantly improve the motor symptoms of Parkinson’s disease when compared to medication alone (Deuschl et al. 2006; Weaver et al. 2009). Given this benefit, it is a surgery that is being performed with increased frequency and current trials are investigating its use even earlier in the disease course (Charles et al. 2014). With the increasing number of patients undergoing DBS for Parkinson’s disease, there has also been an associated increase in the number and scope of publications that have studied these patients postmortem. While initial publications were primarily case reports to verify accurate placement of the electrode in the target of interest, or to evaluate the etiology behind complications or poor effect, more recent studies have started to evaluate the effects of chronic deep brain stimulation on patients with Parkinson’s disease and have shed light on the disease pathology itself as well as what effects deep brain stimulation might have on the natural course of the disease. In this article, we review the literature involving postmortem studies on Parkinson’s disease patients with deep brain stimulators and discuss the primary questions that have been addressed with these studies.
Material and Methods
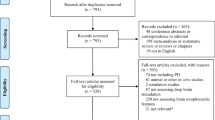
We performed a Medline search of all articles from January 1, 1999 to February 1, 2017 using combinations of the phrases, “Deep Brain Stimulation” and “Postmortem” and “Parkinson”. A similar search was performed using either “Post-mortem” or “Autopsy” in place of “Postmortem”. In all, 36 results were found. Results were filtered to include only articles written in English and those addressing human subjects (see Table 1). After filtering, 13 articles, including case series and case reports, were identified and included in the review. Further investigation into these articles revealed 10 other articles whose scope was consistent with the purposes of this review (Haberler et al. 2000; Henderson et al. 2002; Jarraya et al. 2003; Gross et al. 2004; Hariz et al. 2004; Lezcano et al. 2004; Nielsen et al. 2007; Ullman et al. 2011, 2012; Vedam-Mai et al. 2014). Of these final 23 articles, 8 primarily addressed the overall chronic effects from deep brain stimulation in Parkinson’s disease (Haberler et al. 2000; Nielsen et al. 2007; Sun et al. 2008; Vedam-Mai et al. 2011, 2014; Pienaar et al. 2015; Kronenbuerger et al. 2015; Pal et al. 2017), 4 identified the misdiagnosis of multiple systems atrophy (MSA) as the source of a poor response to deep brain stimulation (Chou et al. 2004; Lezcano et al. 2004; Ullman et al. 2012; Thavanesan et al. 2014), 4 verified either the accurate placement of the DBS electrode using different navigation modalities or the safety of MRI in confirming location (Counelis et al. 2003; Gross et al. 2004; Ullman et al. 2011; Al-Helli et al. 2015), 4 demonstrated that placement of lead close to, but not inside of, the ideal location in the subthalamic nucleus (STN) still resulted in a good clinical response (Henderson et al. 2002; Hariz et al. 2004; McClelland et al. 2007; Guehl et al. 2008) and 3 were used to identify complications from surgery (Henderson et al. 2001; Jarraya et al. 2003; Vedam-Mai et al. 2012). For conciseness and consistency in reviewing these topics, we subdivided these articles into the following sections (see Tables 2, 3, 4): “Verification”, “Complications”, “Alternative pathologies”, and “Long-term effects”.
Results
Verification
Since the borders of classic stimulation sites in stereotactic surgery, such as the STN, are difficult to discern on imaging studies, one of the most fundamental questions in the field is whether the desired target was actually reached. This question is also one of the first and most commonly addressed by postmortem case studies where neuropathological analysis is used to determine the location of the electrode tract relative to the desired targeted nucleus. While the results from these published reports are varied (see Table 2), the overarching conclusion is that, regardless of the technique used, including either with or without microelectrode recording (MER), accurate placement into the targeted nucleus can be achieved but is not necessarily guaranteed nor necessarily required for good clinical effect.
The use of MER in combination with MRI-based imaging is the gold standard for localization in the deep brain procedures and case reports in the literature have used postmortem analysis to verify accurate placement with this technique into both the STN (Counelis et al. 2003) and the ventral intermediate nucleus (VIM) of the thalamus (Gross et al. 2004). In both cases, there was no significant evidence of damage along the two to three additional tracts that were used for MER, arguing against what is one of the most common criticisms of this technique, i.e., that it increases risk and causes additional unnecessary damage. In addition, in the STN case report, the authors noted that the originally proposed tract missed the targeted nucleus entirely by a few millimeters, suggesting that the MER-based adjustments were crucial in this case for accurate targeting. It should also be noted, however, that other authors have contested this viewpoint and, by re-evaluating the neuropathological evidence provided in the original case report, have argued that the importance of MER in this case was overstated, as the postmortem analysis shows placement of the electrode lead in the medial aspect of the STN on the left, in contrast to the dorsolateral aspect which is what was targeted (Hariz et al. 2004).
On the other hand, a case report using imaging only-based localization techniques that forgo MER has also shown accurate bilateral STN electrode placement on post-partum analysis (Al-Helli et al. 2015). Post-operative verification in this approach relied on high-resolution MRI with the DBS implanted and the autopsy analysis showed no evidence that this caused appreciable damage to the brain tissue surrounding the electrode, which is important in validating the safety of MRI in patients with implanted DBS electrodes. In this way, it agreed with work carried out by Ullman et al. who demonstrated, using postmortem brains from DBS patients, that even 3.0T imaging does not lead to histopathological evidence of thermal damage from the implanted electrodes (Ullman et al. 2011).
While these case reports show that accurate placement in the targeted nucleus is possible with or without MER, it is impossible to generalize a practice recommendation either for or against MER based on these studies. Indeed, even with the stronger evidence found in the literature using radiographic and clinical results from deep brain stimulation procedures performed with or without MER (Zeiler et al. 2013; Mirzadeh et al. 2014, 2016), the results are still not definitive, with strong arguments on either side. One of the biggest questions in this debate is whether accurate placement of the DBS electrode within the STN per se is even a requisite to a good clinical response and there have been a few studies using neurohistological evidence that suggest it might not be necessary.
Indeed, over the past two decades, four case studies were published that analyzed the postmortem brains of patients who had good clinical responses to DBS of the bilateral STN at up to 6 years post-operatively and found that at least one electrode was noted to be outside the targeted nucleus in each case, with both leads outside the STN in two of the cases. The technique used in each case was independent of the accuracy, as autopsies on patients with both MER-based and imaging only-based techniques demonstrated both one (Henderson et al. 2002; McClelland et al. 2007) and two electrodes out of the target (Guehl et al. 2008; Sun et al. 2008) in equal numbers. This agrees with data from a case series of 19 postmortem brains referred from various institutions, in which approximately 12% of the electrodes were found to not be placed in the targeted regions (Vedam-Mai et al. 2011). While it is unclear to what degree the stimulation was effective in all these patients, the assumption can be made that it was effective enough to not require revision surgery.
Complications
Another area of deep brain stimulation where autopsy studies offer insight is in identifying the etiology behind suboptimal results. The postmortem literature suggests that, at least in some cases, a complication either directly or indirectly from the surgery can be the source. These include an abnormal reaction to the electrode, a migration of the electrode, or worsening secondary pathologies (see Table 3).
For example, a reported published in 2012 analyzed the brain of a 74-year-old man with Parkinson’s disease who had undergone staged bilateral DBS of the STN prior to passing away from a cardiac event 11 months later (Vedam-Mai et al. 2012). Surgery for the left STN had been performed first and the patient experienced immediate and consistent motor benefit. Approximately 2 months after the left-sided surgery, another surgery was performed on the right; however, the results from this stimulation were never as good as from the left. The postmortem brain showed abnormal fibrosis, characterized by the presence of a thick fibro-collagenous capsule, around the tip of the right electrode. Further analysis revealed hemosiderin around the lead, which the authors speculate might have been the result of a hemorrhage during lead placement that healed through fibrosis.
Similar findings of suboptimal responses have been shown to be secondary to lead migration and inaccurate positioning. In a 2001 report, a 69-year-old male underwent DBS of the left ventral intermediate nucleus (VIM) of the thalamus with lead externalization for tremor dominant Parkinson’s disease (Henderson et al. 2001). He had a notable postoperative course complicated by the pulling out of his extension leads prior to placement of the pulse generator, with anterior displacement of the intracranial lead on imaging. He subsequently underwent a second surgery for placement of a new lead (keeping the first lead in place) but, after implantation of the pulse generator, was noted to have a variable and unsustained response. In addition, he had a rapid progression of symptoms on the ipsilateral (left) side. Three years after surgery, the patient died of sepsis and a postmortem analysis of his brain showed that the first lead had migrated into the anterior thalamus and there was associated damage in this area. However, it also showed that the second lead, which had been intended for the VIM, was actually placed in the centromedial/parafasicular nucleus and stimulation had resulted in drastic cell loss of over 90% in this nucleus as well, significantly more than the contralateral side. Both of these factors were felt to play a crucial role in his poor response and drastic decline after surgery.
Of course, even without abnormal physiological responses or technical complications, poor responses from DBS surgeries can also be the result of the surgery worsening an underlying secondary pathology. For example, in a 2003 report, a 67-year-old female underwent bilateral STN DBS for motor symptoms including levodopa-associated dyskinesias (Jarraya et al. 2003). Prior to surgery, however, she demonstrated mild cognitive declines. After surgery, her cognitive decline progressed and she subsequently passed away 18 months later from pulmonary embolism. Autopsy studies were consistent with the diagnosis of Parkinson’s disease and accurate placement of the electrodes in the STN; however, as the authors argued, given the cognitive impairment, the patient in this case was not an appropriate candidate for surgery and the surgery likely precipitated her cognitive decline.
Alternative pathologies
As described above, technical missteps, abnormal physiological responses or poor patient selection can all be the source of complications and poor responses to deep brain stimulation therapy. However, another etiology for a poor response is an inaccurate diagnosis. For example, in a 2004 case report, a 54-year-old male who underwent bilateral STN DBS after 9 years of levodopa, had responsive motor symptoms that was initially felt to be idiopathic Parkinson’s disease (Chou et al. 2004). While he had a reduction in his motor symptoms intraoperatively, post-operatively he had a rapid decline in both motor and cognitive function and died 12 weeks after surgery from aspiration pneumonia. Postmortem analysis revealed numerous alpha-synuclein-positive cytoplasmic inclusions throughout multiple areas of the brain, including the cerebellum and brainstem, in addition to the subcortical nuclei, which confirmed the diagnosis of multiple systems atrophy (MSA). MSA is often misdiagnosed as Parkinson’s disease by even experienced neurologists as they share many clinical features (Litvan et al. 1997). In addition, this was an unusual presentation of MSA, as roughly only 13% of patients have a response to dopamine replacement (Wenning et al. 1997) but the poor response of MSA to DBS is not unusual even in such cases. Indeed, similar cases have been published by multiple authors (Lezcano et al. 2004; Ullman et al. 2012; Thavanesan et al. 2014). In all these reports, patients with autopsy-confirmed MSA were initially diagnosed with parkinsonian symptoms responsive to dopamine replacement and underwent bilateral deep brain stimulation surgeries and, in all cases, a transient improvement in motor outcomes quickly deteriorated, accompanied by worsened cognitive and overall outcome. This agrees with the general consensus that deep brain stimulation is not typically recommended for patients in whom MSA is suspected.
In summary, postmortem studies have offered insight into the underlying etiology behind poor responses and have shown that possible causes could be complications from surgery or alternative pathologies such as MSA. However, extrapolating an estimate for how often these situations occur is difficult, as they are only reported as case reports and likely highly underrepresented. However, it is important to keep these possible sources for suboptimal responses in mind as they can be often avoided by more stringent patient selection or operative technique.
Long-term effects
One the most straightforward things to note from the postmortem analysis of patients’ brains who died from DBS is the neuropathological effects from chronic stimulation (see Table 4). One of the earliest reports in this regard was a case series published in 2000 that analyzed the brains of 8 patients with Parkinson’s disease who underwent DBS brain stimulation of either the VIM (6 patients) or the STN (2 patients) for periods of time ranging from 2 days to 70 months (Haberler et al. 2000). The results showed very similar responses irrespective of the duration of stimulation, excluding the one patient who died 2 days after stimulation. In all patients, there was a characteristic three-layer response around the electrode lead. First, there was a thin, less than 25 µm, layer of fibrous tissue. Surrounding this was a thicker rim of fibrillary gliosis that was less than 500 µm. Finally, surrounding this was an even thicker (approximately 1 mm) layer of loosely scattered glial fibrillary acidic-protein reactive astrocytes. There was also evidence of scarce mononuclear leukocytes and multinucleated giant cells in the tract and surrounding tissue. In 2007, a case report largely confirmed these findings in the postmortem analysis of a single patient with Parkinson’s disease who died 29 months after high-frequency stimulation to the subthalamic nucleus (Nielsen et al. 2007) and they referred to the approximately 150-µm layer of connective fibrous tissue and surrounding gliosis as a “capsule”. Another case report in 2008 showed similar findings in the postmortem analysis of an 81-year-old man with Parkinson’s disease who had undergone successful bilateral STN DBS for 71 months prior to dying from pneumonia. In this patient, however, they noted the presence of Rosenthal fibers in the gliotic tissue surrounding the lead. Interestingly, they were also able to find evidence of one of the test tracts that had initially been used during the surgery on the left side. This tract also showed evidence of gliosis, although it lacked the thick capsule formation or Rosenthal fibers. A larger case series published in 2011 on over 19 postmortem brains also largely confirmed these findings with all but one of their brains showing the previously described layers of fibrous and gliosis (Vedam-Mai et al. 2011). The abnormal brain had an unusually large fibrous capsule as described above (Vedam-Mai et al. 2012).
In 2015, a more detailed case series extended these results by evaluating the axonal changes with immunohistochemistry and analyzing differences in the histopathological findings based on the etiology of death in 10 patients with either Parkinson’s disease or essential tremor (Kronenbuerger et al. 2015). In addition to previously reported findings of gliosis around the electrode leads, they also reported on the presence of T-lymphocytes in over 90% of patients and multinucleated giant cells in approximately 70% of patients. In addition, they found an increase in axonal swellings that were immune-reactive to amyloid precursor protein at electrically active parts of the electrode. Finally, they showed that the cause of death was also a differentiating factor in the histopathological findings, with patients dying of septicemia showing more of a gliotic reaction around the electrodes than those dying from cardiac events.
More recent studies have increased our understanding of how the DBS might demonstrate its effects by comparing the postmortem brains of Parkinson’s patients with DBS to those who did not receive DBS (see Table 4). For example, an investigative report in 2015 compared the brains of 5 patients with STN DBS for Parkinson’s disease to an approximately equal number of Parkinson patients without DBS and non-Parkinson controls (Pienaar et al. 2015). In this interesting analysis, they found that, when compared to normal control, Parkinson patients had a decreased number of capillaries in the STN and decreased endothelial cell thickness. However, in the brains of patients who had DBS, there was an increase in the number of capillaries and the endothelial cell thickness when compared to controls. There was also an increase in the length of the capillaries when compared to both controls and non-stimulated Parkinson patients. This finding suggested that an etiology behind some of the symptoms of Parkinson’s disease might be a disruption of the microvascular integrity and that a possible method for the effect of DBS is through improving this integrity. They further investigated this hypothesis with immunohistochemistry, which showed that the STN of Parkinson patients had a decrease in proteins associated with tight junctions and the integrity of the blood–brain barrier. However, in the brains of patients with DBS, these protein levels were rescued even higher than control levels. Further analysis showed an overexpression of VEGF in DBS patients, lending further credence to the hypothesis that DBS may improve damaged microvascular integrity in Parkinson’s disease (Lee and Pienaar 2014; Pienaar et al. 2015).
Interestingly, this same group also found that, compared to controls, Parkinson patients had an increase in the number of microglia within the STN. However, in stimulated patients, there was a reduction in this upregulation of microglia. This correlates with recent animal studies that have shown that, in lesioned animal models, the upregulation of activated microglia by the lesioning process is mitigated by stimulation (Vedam-Mai et al. 2016). This reduction in the number of activated microglia is in turn associated with an increase in the number of neural progenitor cells in the animal model and builds on prior studies that were able to isolate neural progenitor cells from the postmortem brain of Parkinson’s patients as well as from discarded deep brain stimulating electrodes (Wang et al. 2012). It also agrees with previous work involving a postmortem analysis of 12 Parkinson patients with prior DBS, in which the investigators were able to use immunohistochemistry to compare the number of neural progenitor cells to matched non-stimulated Parkinson controls and non-Parkinson controls (Vedam-Mai et al. 2014). They found that stimulation was associated with an increase in the number of cells expressing neural progenitor markers in several regions of the brain, including the subventricular zones of the lateral ventricles and third ventricle as well as the tissue surrounding the DBS electrodes. The extent of this increase was up to 6-fold in some regions. Taken together, these results build on what is turning out to be a complex relationship between microglia and neural progenitor cells. With prior studies showing that the upregulation of microglia in response to inflammation is associated with decreased neurogenesis (Monje et al. 2003; Mosher et al. 2012), the overarching picture is one in which DBS may be able to decrease the detrimental influence of activated microglia and perhaps promote the proliferation of neural progenitor cells in Parkinson’s disease. This might not only explain the improvement in motor symptoms seen with stimulation but also suggest the interesting possibility that stimulation might be neuroprotective or neurorestorative.
In 2017, however, another study compared the postmortem brains of stimulated versus non-stimulated Parkinson patients who donated their brains to the Arizona Study of Aging and Neurodegenerative Disorders and Brain and Body Program (Pal et al. 2017). In that analysis of 167 patients, 11 of whom had bilateral DBS STN, while the rest did not have any stimulation, they found no significant differences in the level of pigmented neuron loss in the substantia nigra. Interestingly, they also found a statistically significant increase in the amount of alpha synuclein, a key marker for Parkinson’s disease, in the substantia nigra of the DBS patients. This increase was also found in several other regions of the brain, although, outside the substantia nigra, only the locus ceruleus and olfactory bulb were statistically significant. The increased alpha synuclein would suggest that DBS may have a possible toxic effect; however, as the authors stress, this conclusion cannot be obtained from this study alone given the limited sample size and cross-sectional nature of the study.
Discussion
The recent increase in the number of DBS patients has led to an increase in the number and quality of publications analyzing the brains of these patients postmortem, thereby adding to an existing body of literature that attempts to give us a better understanding of the methods by which DBS is working (Dostrovsky and Lozano 2002; Johnson et al. 2008; Hess et al. 2013).
Thus far, the postmortem literature, which has been largely dominated by studies with low levels of evidence such as case reports, has focused on questions that can be at least partially addressed with small sample sizes, such as validating accurate placement of the electrodes using particular techniques and/or demonstrating that good clinical effect can be achieved with electrodes located near but not necessarily in the targeted region. Indeed, while the published postmortem literature to date has shown neurohistologically that both MER- and imaging only-based targeting methods can be accurate in reaching the desired nucleus, it also demonstrates that neither method guarantees accuracy or that accuracy is even required for a beneficial clinical response. In this regard, it does not resolve the current debate in the literature regarding the efficacy of MER. Larger studies would be needed to further address this question.
Similarly, the small sample size studies in the postmortem literature has also proven useful in identifying etiologies that have led to poor clinical results, which include perioperative complications such as migrated electrodes, abnormal histological responses to the electrodes including excessive fibrosis and the presence of alternative pathologies, such as multiple system atrophy. However, once again, the limited size of the studies limits the degree to which we can estimate how often these complications and alternative pathologies are present in DBS patients. More recent studies are utilizing larger sample sizes to pursue an understanding of the global effects of DBS by evaluating the brains of DBS patients and comparing them to non-stimulated controls. So far, these studies have helped to describe what is likely a normal response to chronic stimulation, which includes the development of a thin fibrous layer, surrounded by two progressively larger gliotic layers. They have also begun to identify methods by which DBS could be effective, including through rescuing pathological changes in microvasculature and promoting neuroprogentior proliferation. This goal is further advanced by the establishment of tissue banks where large numbers of postmortem brains can be analyzed to assess for overall trends (Vedam-Mai et al. 2011; Beach et al. 2015). The future of these much-needed endeavors will undoubtedly shed more light on the mechanism behind one of the most powerful tools in the treatment of Parkinson’s disease.
References
Al-Helli O, Thomas DL, Massey L, Foltynie T, Limousin P, Holton JL, Yousry TA, Zrinzo L (2015) Deep brain stimulation of the subthalamic nucleus: histological verification and 9.4-T MRI correlation. Acta Neurochir (Wien) 157:2143–2147. doi:10.1007/s00701-015-2599-x
Beach TG, Adler CH, Sue LI, Serrano G, Shill HA, Walker DG, Lue L, Roher AE, Dugger BN, Maarouf C, Birdsill AC, Intorcia A, Saxon-Labelle M, Pullen J, Scroggins A, Filon J, Scott S, Hoffman B, Garcia A, Caviness JN, Hentz JG, Driver-Dunckley E, Jacobson SA, Davis KJ, Belden CM, Long KE, Malek-Ahmadi M, Powell JJ, Gale LD, Nicholson LR, Caselli RJ, Woodruff BK, Rapscak SZ, Ahern GL, Shi J, Burke AD, Reiman EM, Sabbagh MN (2015) Arizona Study of Aging and Neurodegenerative Disorders and Brain and Body Donation Program. Neuropathology 35:354–389. doi:10.1111/neup.12189
Charles D, Konrad PE, Neimat JS, Molinari AL, Tramontana MG, Finder SG, Gill CE, Bliton MJ, Kao C, Phibbs FT, Hedera P, Salomon RM, Cannard KR, Wang L, Song Y, Davis TL (2014) Subthalamic nucleus deep brain stimulation in early stage Parkinson’s disease. Parkinsonism Relat Disord 20:731–737. doi:10.1016/j.parkreldis.2014.03.019
Chou KL, Forman MS, Trojanowski JQ, Hurtig HI, Baltuch GH (2004) Subthalamic nucleus deep brain stimulation in a patient with levodopa-responsive multiple system atrophy. Case report. J Neurosurg 100:553–556. doi:10.3171/jns.2004.100.3.0553
Counelis GJ, Simuni T, Forman MS, Jaggi JL, Trojanowski JQ, Baltuch GH (2003) Bilateral subthalamic nucleus deep brain stimulation for advanced PD: correlation of intraoperative MER and postoperative MRI with neuropathological findings. Mov Disord 18:1062–1065. doi:10.1002/mds.10489
Deuschl G, Schade-Brittinger C, Krack P, Volkmann J, Schäfer H, Bötzel K, Daniels C, Deutschländer A, Dillmann U, Eisner W, Gruber D, Hamel W, Herzog J, Hilker R, Klebe S, Kloss M, Koy J, Krause M, Kupsch A, Lorenz D, Lorenzl S, Mehdorn HM, Moringlane JR, Oertel W, Pinsker MO, Reichmann H, Reuss A, Schneider G-H, Schnitzler A, Steude U, Sturm V, Timmermann L, Tronnier V, Trottenberg T, Wojtecki L, Wolf E, Poewe W, Voges J, German Parkinson Study Group, Section N (2006) A randomized trial of deep-brain stimulation for Parkinson’s disease. N Engl J Med 355:896–908. doi:10.1056/NEJMoa060281
Dostrovsky JO, Lozano AM (2002) Mechanisms of deep brain stimulation. Mov Disord 17(Suppl 3):S63–S68
Gross RE, Jones EG, Dostrovsky JO, Bergeron C, Lang AE, Lozano AM (2004) Histological analysis of the location of effective thalamic stimulation for tremor. Case report. J Neurosurg 100:547–552. doi:10.3171/jns.2004.100.3.0547
Guehl D, Vital A, Cuny E, Spampinato U, Rougier A, Bioulac B, Burbaud P (2008) Postmortem proof of effectiveness of zona incerta stimulation in Parkinson disease. Neurology 70:1489–1490. doi:10.1212/01.wnl.0000310426.18409.11
Haberler C, Alesch F, Mazal PR, Pilz P, Jellinger K, Pinter MM, Hainfellner JA, Budka H (2000) No tissue damage by chronic deep brain stimulation in Parkinson’s disease. Ann Neurol 48:372–376
Hariz M, Blomstedt P, Limousin P (2004) The myth of microelectrode recording in ensuring a precise location of the DBS electrode within the sensorimotor part of the subthalamic nucleus. Mov Disord 19:863–864. doi:10.1002/mds.20135
Henderson JM, O’Sullivan DJ, Pell M, Fung VS, Hely MA, Morris JG, Halliday GM (2001) Lesion of thalamic centromedian--parafascicular complex after chronic deep brain stimulation. Neurology 56:1576–1579
Henderson JM, Pell M, O’Sullivan DJ, McCusker EA, Fung VSC, Hedges P, Halliday GM (2002) Postmortem analysis of bilateral subthalamic electrode implants in Parkinson’s disease. Mov Disord 17:133–137
Hess CW, Vaillancourt DE, Okun MS (2013) The temporal pattern of stimulation may be important to the mechanism of deep brain stimulation. Exp Neurol 247:296–302. doi:10.1016/j.expneurol.2013.02.001
Jarraya B, Bonnet A-M, Duyckaerts C, Houeto J-L, Cornu P, Hauw J-J, Agid Y (2003) Parkinson’s disease, subthalamic stimulation, and selection of candidates: a pathological study. Mov Disord 18:1517–1520. doi:10.1002/mds.10607
Johnson MD, Miocinovic S, McIntyre CC, Vitek JL (2008) Mechanisms and targets of deep brain stimulation in movement disorders. Neurother J Am Soc Exp Neurother 5:294–308. doi:10.1016/j.nurt.2008.01.010
Kronenbuerger M, Nolte KW, Coenen VA, Burgunder J-M, Krauss JK, Weis J (2015) Brain alterations with deep brain stimulation: New insight from a neuropathological case series. Mov Disord 30:1125–1130. doi:10.1002/mds.26247
Lee H, Pienaar IS (2014) Disruption of the blood-brain barrier in Parkinson’s disease: curse or route to a cure? Front Biosci Landmark Ed 19:272–280
Lezcano E, Gómez-Esteban JC, Zarranz JJ, Alcaraz R, Atarés B, Bilbao G, Garibi J, Lambarri I (2004) Parkinson’s disease-like presentation of multiple system atrophy with poor response to STN stimulation: a clinicopathological case report. Mov Disord 19:973–977. doi:10.1002/mds.20108
Litvan I, Goetz CG, Jankovic J, Wenning GK, Booth V, Bartko JJ, McKee A, Jellinger K, Lai EC, Brandel JP, Verny M, Chaudhuri KR, Pearce RK, Agid Y (1997) What is the accuracy of the clinical diagnosis of multiple system atrophy? A clinicopathologic study. Arch Neurol 54:937–944
McClelland S, Vonsattel JP, Garcia RE, Amaya MD, Winfield LM, Pullman SL, Yu Q, Fahn S, Ford B, Goodman RR (2007) Relationship of clinical efficacy to postmortem-determined anatomic subthalamic stimulation in Parkinson syndrome. Clin Neuropathol 26:267–275
Mirzadeh Z, Chapple K, Lambert M, Dhall R, Ponce FA (2014) Validation of CT-MRI fusion for intraoperative assessment of stereotactic accuracy in DBS surgery. Mov Disord 29:1788–1795. doi:10.1002/mds.26056
Mirzadeh Z, Chapple K, Lambert M, Evidente VG, Mahant P, Ospina MC, Samanta J, Moguel-Cobos G, Salins N, Lieberman A, Tröster AI, Dhall R, Ponce FA (2016) Parkinson’s disease outcomes after intraoperative CT-guided “asleep” deep brain stimulation in the globus pallidus internus. J Neurosurg 124:902–907. doi:10.3171/2015.4.JNS1550
Monje ML, Toda H, Palmer TD (2003) Inflammatory blockade restores adult hippocampal neurogenesis. Science 302:1760–1765. doi:10.1126/science.1088417
Mosher KI, Andres RH, Fukuhara T, Bieri G, Hasegawa-Moriyama M, He Y, Guzman R, Wyss-Coray T (2012) Neural progenitor cells regulate microglia functions and activity. Nat Neurosci 15:1485–1487. doi:10.1038/nn.3233
Nielsen MS, Bjarkam CR, Sørensen JC, Bojsen-Møller M, Sunde NA, Østergaard K (2007) Chronic subthalamic high-frequency deep brain stimulation in Parkinson’s disease--a histopathological study. Eur J Neurol 14:132–138. doi:10.1111/j.1468-1331.2006.01569.x
Pal GD, Ouyang B, Serrano G, Shill HA, Goetz C, Stebbins G, Metman LV, Driver-Dunckley E, Mehta SH, Caviness JN, Sabbagh MN, Adler CH, Beach TG, Arizona Study of Aging Neurodegenerative Disorders (2017) Comparison of neuropathology in Parkinson’s disease subjects with and without deep brain stimulation. Mov Disord 32:274–277. doi:10.1002/mds.26882
Pienaar IS, Lee CH, Elson JL, McGuinness L, Gentleman SM, Kalaria RN, Dexter DT (2015) Deep-brain stimulation associates with improved microvascular integrity in the subthalamic nucleus in Parkinson’s disease. Neurobiol Dis 74:392–405. doi:10.1016/j.nbd.2014.12.006
Sun DA, Yu H, Spooner J, Tatsas AD, Davis T, Abel TW, Kao C, Konrad PE (2008) Postmortem analysis following 71 months of deep brain stimulation of the subthalamic nucleus for Parkinson disease. J Neurosurg 109:325–329. doi:10.3171/JNS/2008/109/8/0325
Thavanesan N, Gillies M, Farrell M, Green AL, Aziz T (2014) Deep brain stimulation in multiple system atrophy mimicking idiopathic Parkinson’s disease. Case Rep Neurol 6:232–237. doi:10.1159/000368571
Ullman M, Vedam-Mai V, Krock N, Sudhyadhom A, Foote KD, Yachnis AT, Merritt S, Resnick AS, Zeilman P, Okun MS (2011) A pilot study of human brain tissue post-magnetic resonance imaging: information from the National Deep Brain Stimulation Brain Tissue Network (DBS-BTN). NeuroImage 54(Suppl 1):S233–S237. doi:10.1016/j.neuroimage.2010.09.014
Ullman M, Vedam-Mai V, Resnick AS, Yachnis AT, McFarland NR, Merritt S, Zeilman P, Foote KD, Okun MS (2012) Deep brain stimulation response in pathologically confirmed cases of multiple system atrophy. Parkinsonism Relat Disord 18:86–88. doi:10.1016/j.parkreldis.2011.09.008
Vedam-Mai V, Krock N, Ullman M, Foote KD, Shain W, Smith K, Yachnis AT, Steindler D, Reynolds B, Merritt S, Pagan F, Marjama-Lyons J, Hogarth P, Resnick AS, Zeilman P, Okun MS (2011) The national DBS brain tissue network pilot study: need for more tissue and more standardization. Cell Tissue Bank 12:219–231. doi:10.1007/s10561-010-9189-1
Vedam-Mai V, Yachnis A, Ullman M, Javedan SP, Okun MS (2012) Postmortem observation of collagenous lead tip region fibrosis as a rare complication of DBS. Mov Disord 27:565–569. doi:10.1002/mds.24916
Vedam-Mai V, Gardner B, Okun MS, Siebzehnrubl FA, Kam M, Aponso P, Steindler DA, Yachnis AT, Neal D, Oliver BU, Rath SJ, Faull RLM, Reynolds BA, Curtis MA (2014) Increased precursor cell proliferation after deep brain stimulation for Parkinson’s disease: a human study. PloS ONE 9:e88770. doi:10.1371/journal.pone.0088770
Vedam-Mai V, Baradaran-Shoraka M, Reynolds BA, Okun MS (2016) Tissue Response to Deep Brain Stimulation and Microlesion: A Comparative Study. Neuromodulation 19:451–458. doi:10.1111/ner.12406
Wang S, Okun MS, Suslov O, Zheng T, McFarland NR, Vedam-Mai V, Foote KD, Roper SN, Yachnis AT, Siebzehnrubl FA, Steindler DA (2012) Neurogenic potential of progenitor cells isolated from postmortem human Parkinsonian brains. Brain Res 1464:61–72. doi:10.1016/j.brainres.2012.04.039
Weaver FM, Follett K, Stern M, Hur K, Harris C, Marks WJ, Rothlind J, Sagher O, Reda D, Moy CS, Pahwa R, Burchiel K, Hogarth P, Lai EC, Duda JE, Holloway K, Samii A, Horn S, Bronstein J, Stoner G, Heemskerk J, Huang GD, CSP 468 Study Group (2009) Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA 301:63–73. doi:10.1001/jama.2008.929
Wenning GK, Tison F, Ben Shlomo Y, Daniel SE, Quinn NP (1997) Multiple system atrophy: a review of 203 pathologically proven cases. Mov Disord 12:133–147. doi:10.1002/mds.870120203
Zeiler FA, Wilkinson M, Krcek JP (2013) Subthalamic nucleus deep brain stimulation: an invaluable role for MER. Can J Neurol Sci 40:572–575
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reddy, G.D., Lozano, A.M. Postmortem studies of deep brain stimulation for Parkinson’s disease: a systematic review of the literature. Cell Tissue Res 373, 287–295 (2018). https://doi.org/10.1007/s00441-017-2672-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-017-2672-2