Abstract
Over the last 60 years, accumulating evidence has suggested that acute, chronic, and maternal Toxoplasma gondii infections predispose to schizophrenia. More recent evidence suggests that chronically infected patients with schizophrenia present with more severe disease. After acute infection, parasites form walled cysts in the brain, leading to lifelong chronic infection and drug resistance to commonly used antiparasitics. Chronic infection is the most studied and closely linked with development and severity of schizophrenia. There are currently four published randomized controlled trials evaluating antiparasitic drugs, specifically azithromycin, trimethoprim, artemisinin, and artemether, in patients with schizophrenia. No trials have demonstrated a change in psychopathology with adjunctive treatment. Published trials have either selected drugs without evidence against chronic infection or used them at doses too low to reduce brain cyst burden. Furthermore, trials have failed to achieve sufficient power or account for confounders such as previous antipsychotic treatment, sex, age, or rhesus status on antiparasitic effect. There are currently no ongoing trials of anti-Toxoplasma therapy in schizophrenia despite ample evidence to justify further testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
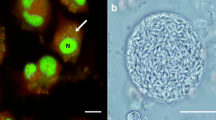
Schizophrenia exacts a significant global burden of disease: it was the 12th leading cause of years lost to disability in 2015, placing it ahead of osteoarthritis, chronic obstructive pulmonary disease, and Alzheimer’s disease (Vos et al. 2016). Yet, despite significant research, the complex interplay of genetic and environmental factors in its pathogenesis is unclear. Since at least the 1950s, there has been a hypothesized connection between schizophrenia and Toxoplasma gondii infection (Buentello 1958). T. gondii is an intracellular parasite with tropism for the muscle and brain; upon oral, intravenous, or sexual introduction into immunocompetent hosts, fast-replicating tachyzoites migrate to these organs, convert to bradyzoites, and form cysts that persist for the host’s life. Bradyzoites are resistant to almost all clinically available anti-Toxoplasma drugs, and treatment is currently only used in acute toxoplasmosis (Neville et al. 2015). Latent Toxoplasma infection is classically considered asymptomatic, affecting over 20% of the population in South America, Central and Eastern Europe, the Middle East, Southeast Asia, and Africa (Pappas et al. 2009).
Recent meta-analyses confirm that there is a greater prevalence of both IgG and IgM antibodies, as well as greater IgG titres, in patients with schizophrenia (Monroe et al. 2015; Sutterland et al. 2015). Importantly, the vast majority of studies have examined the epidemiological and pathophysiological link between latent Toxoplasma infection, marked by IgG-seropositivity, and schizophrenia in the same individual (Sutterland et al. 2015). A smaller number of studies have also supported development of schizophrenia after acute Toxoplasma infection, marked by IgM seropositivity, or maternal infection on foetal development of disease. Current evidence suggests that chronic Toxoplasma-induced neuroinflammation and cytokine imbalance alter neurotransmitter metabolism, tryptophan metabolism, host immune function, and systemic hormone levels (Elsheikha et al. 2016). In rodents, one of the most studied pathways connects chronic T. gondii infection with increased brain concentrations of dopamine via parasite-encoded tyrosine hydroxylases and host nitric oxide-mediated dopamine release (Elsheikha et al. 2016). In humans, anti-Toxoplasma IgG titres are lower in patients with more severe psychopathology, suggesting that long-term infection leads to worsening of disease over time (Holub et al. 2013).
Not only does Toxoplasma infection predispose to schizophrenia, there is mounting evidence that IgG-positive schizophrenia cases are distinct and more severe compared with seronegative cases (Flegr 2015). Three independent studies show more intense positive symptoms (e.g. hallucinations, delusions, and disorganized thought) in seropositive cases (Wang et al. 2006; Amminger et al. 2007; Holub et al. 2013). Furthermore, Çelik et al. (2015) show that seropositive cases have significantly greater risk for continuous disease, need for electroconvulsive therapy, and lack of insight into illness. Holub et al. (2013) show that seropositive cases have longer hospitalizations and are more likely to require high-dose antipsychotics. Fond et al. (2015) show that seropositive patients with schizophrenia or schizoaffective disorder have a higher lifetime number of depressive and manic episodes, suicide attempts, and psychiatric hospitalizations. One imaging study corroborates these observed clinical differences: seropositive patients with schizophrenia had significantly reduced grey matter volume bilaterally in the caudate, median cingulate, thalamus, and occipital cortex and in the left cerebellar hemispheres compared with seronegative patients with schizophrenia. No difference in the brain morphology between seronegative patients and controls was observed (Horacek et al. 2012).
Studies to date
Given the close link between T. gondii infection and schizophrenia, there have been four published randomized controlled trials (RCTs) evaluating adjunctive antiparasitics in patients with schizophreniaFootnote 1 (Table 1). Each trial has significant underlying issues that prevent extrapolating evidence to all anti-Toxoplasma treatment in schizophrenia. The first published trial, conducted by Dickerson et al. (2009), randomly evaluated adjunctive azithromycin in 28 patients with IgG-positive schizophrenia or schizoaffective disorder on stable antipsychotic treatment. The treatment group (n = 13) received azithromycin 600 mg daily for 2 weeks and then weekly for an additional 14 weeks. Patients were evaluated using the Positive and Negative Syndrome Scale (PANSS) at baseline and every other week for 16 weeks. PANSS is the most widely used symptom severity scale in schizophrenia and assesses positive symptoms such as hallucinations and delusions, negative symptoms such as emotional and social withdrawal, and global psychopathology such as depression and anxiety. As per previous benchmarking studies, a total PANSS score of 58, 75, 95, and 116 correlate with mild, moderate, marked, and severe disease, respectively (Leucht et al. 2005). In the azithromycin trial, patients had a mean PANSS baseline score of 71.6, were 54% female, and had a mean duration of illness of 22.3 years.
The next trial, conducted by Shibre et al. (2010), examined 6 months of add-on trimethoprim (TMP) at 200 mg per day to usual care in a double-blind RCT. Study participants (n = 91) were all male, had schizophrenia, had an average duration of illness of 13 years, and had a baseline PANSS score of at least 60. The study was powered to detect a 7-point difference in mean PANSS score between study arms over 6 months with 80% power. PANSS was reassessed monthly.
Dickerson et al. (2011) evaluated 100 mg artemisinin twice daily in a double-blind RCT of 66 patients with schizophrenia or schizoaffective disorder. Inclusion criteria were at least moderately severe on one or more PANSS positive symptom scores and/or PANSS negative symptom scores of 4 or more or a total PANSS score of 50 or more containing at least three positive or negative items with scores of 3 or more. Treatment was given for 10 weeks and PANSS assessed at 2-week intervals. Wang et al. (2014) evaluated the related compound artemether in a double-blind RCT of 100 patients with schizophrenia or schizophreniform disorder. Inclusion criteria were IgG- or IgM-seropositive patients naïve to antipsychotics. Risperidone was started at 0.5 mg twice daily in each group and titrated up by the treating psychiatrist. At week 2, participants received 80 mg artemether or placebo daily for 1 week and then again for the fourth week. Participants were also allowed trihexyphenidyl and clonazepam. Participants were evaluated every other week for 8 weeks with PANSS.
No study found any change in PANSS total score or subscale scores with adjunctive antiparasitic treatment. In the artemisinin trial, there was no change in the Repeatable Battery for the Assessment of Neuropsychological Status (originally a tool to assess dementia) or the University of California Performance-Based Skills Assessment (an evaluation of day to day functioning). In the artemether trial, there was no change in the Clinical Global Impressions Scale (a subjective assessment by the treating physician of disease severity) or the Brief Assessment of Cognition in Schizophrenia (an assessment of memory, attention, and executive function). Furthermore, artemisinin and artemether did not significantly alter IgG-seropositivity to Toxoplasma at the end of each trial, and the other two studies did not assess this outcome.
Drug selection and dosing
All published studies suffered from selection of drugs without established activity against Toxoplasma bradyzoites in comparable animal models. Azithromycin has previously been tested in at least two mouse models of chronic Toxoplasma infection (Dumas et al. 1994; Mahmoud 2006). In the Dumas et al. experiment, mice were treated for the same duration (14–19 weeks) as the human trial (16 weeks) but received treatment daily for the full duration instead of weekly for weeks 3 to 16. Each treatment dose was roughly equivalent between studies after correcting for inter-species differences (488 mg daily human equivalent vs. 600 mg daily) (Nair and Jacob 2016). Despite in vitro evidence for azithromycin against bradyzoites (Huskinson-Mark et al. 1991), no in vivo reduction in brain cysts was seen in this experiment. One explanation is that drug concentrations in mouse brain were too low to exert antiparasitic activity: In the second experiment (Mahmoud 2006), a human equivalent dose of 1220 mg daily azithromycin was used for 13 weeks, and this dose led to a decrease in the number of cysts in the brains of chronically infected mice. While Mahmoud used a more virulent, albeit still chronic, cystogenic strain of T. gondii, additional evidence comes from inhibiting efflux of other macrolides, such as spiramycin, from the brain. Achieving sufficient drug concentration in the brain is challenging because macrolides are effluxed via multidrug-resistant protein 2 and P-glycoprotein (Sugie et al. 2004; Munić et al. 2010), resulting in drug concentrations 10- to 100-fold lower than in other organs of Toxoplasma-infected mice (Araujo et al. 1991). Adjunctive metronidazole, an efflux inhibitor, increased maximum spiramycin concentration in chronically infected mouse brain by 72% and reduced cyst burden by 10-fold compared with spiramycin alone (Chew et al. 2012). Given the weekly dosing of azithromycin in the human schizophrenia trial and the lack of evidence at equivalent daily doses in mice, it is unlikely that human patients saw any reduction in cyst burden, precluding changes in PANSS.
The choice of TMP as the active agent in the Shibre et al. trial is perplexing and likely led to negative study results. A literature search could identify no studies evaluating TMP alone against chronic Toxoplasma. Studies examining TMP with sulphamethoxazole (SMX) in chronic infection found the combination, which is synergistic, could not eradicate cysts from mouse brain (Nguyen and Stadtsbaeder 1983) but could increase survival (Dumas et al. 1999) compared with placebo. In a mouse model of acute toxoplasmosis, mice treated with TMP alone did not have increased survival, whereas addition of SMX protected all animals from death (Dumas et al. 1999). Shibre et al. rationalize their choice of active drug by stating that TMP is used for toxoplasmosis prophylaxis in immunocompromised hosts. This argument is invalid as TMP is almost always prescribed with SMX; for example, current HIV guidelines do not recommend TMP alone (Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents 2017).
Finally, there is no direct evidence that artemisinin or artemether, related compounds used to treat malaria, has activity against bradyzoites (Sharif et al. 2016; Loo et al. 2017). Artemether, which is twice as potent as artemisinin against tachyzoites in vitro (Hencken et al. 2010), failed to reduce cyst burden in chronically infected mice (Schultz et al. 2014). Artemether was given daily for 16 days at a human equivalent of 49 mg, longer but at 5/8th the dose of the human schizophrenia trial. One derivative of artemisinin did reduce cyst burden in this study, but given lack of activity of artemether and three other artemisinin derivatives in vivo (Dunay et al. 2009; Schultz et al. 2014), this effect cannot be extrapolated to the class.
Study power and inclusion criteria
Aside from the selection of potentially inappropriate antimicrobial therapy, most published studies have design flaws that further precluded meaningful results. Three (Dickerson et al. 2009; Shibre et al. 2010; Dickerson et al. 2011) out of four studies omitted sample size calculation from their manuscript and were likely inappropriately powered to detect significant difference. Only two studies (Dickerson et al. 2009; Wang et al. 2014) excluded Toxoplasma-seronegative patients, further decreasing power, with the TMP evaluation including 11% IgG-negative patients.
Including patients already on a stable course of antipsychotics could have confounded analysis of the remaining IgG-positive patients. It has been reported that select antipsychotics possess activity against Toxoplasma tachyzoites in vitro (Jones-Brando et al. 2003; Goodwin et al. 2011; Fond et al. 2014). In a subacute toxoplasmosis rat model, treatment with haloperidol reduced behavioural disturbance more than a pyrimethamine/dapsone combination, which was superior to valproic acid (Webster et al. 2006). Interestingly, these reductions occurred in proportion to the number of animals with Toxoplasma-staining neurons and glia in each treatment arm, and each treatment had the opposite effect in uninfected rats (i.e. they increased behavioural disturbance). The authors speculate that the anti-Toxoplasma activity of each drug led to behavioural improvement; however, the relevance of these findings to chronic infection in schizophrenia is unclear. Treatment in this rat model started on day 14 when most T. gondii cells were in tachyzoite stage, although brain cysts have been reported to form as early as day 8 post-infection (Lainson 1958). As well, pyrimethamine and dapsone both have activity against tachyzoites and bradyzoites as monotherapy (Chang et al. 1994). In humans, one retrospective cohort study failed to find a difference in treatment response between IgG-positive patients treated with antipsychotics active against tachyzoites (Fond et al. 2015). Future RCTs evaluating adjunctive antiparasitic treatment should avoid confounding by only including patients on antipsychotics with no known antiparasitic activity.
Only one RCT (Shibre et al. 2010) accounted for an interaction between Toxoplasma infection and sex by study design (excluding females from their trial), and no trials used statistical analysis to account for sex. It has been reported that Toxoplasma infection presents differently in each sex: In a cohort of 251 patients, schizophrenia presented 1 year earlier and 2.5 years later in males and females, respectively (Holub et al. 2013). In the same cohort, males, but not females, scored significantly higher in negative PANSS scores, reality distortion, disorganization, and cognitive composite scores than uninfected counterparts. These changes are consistent with sex differences of latent infection on human behaviour (Lindová et al. 2006; Lindová et al. 2013) and modifications to T. gondii susceptibility and immune response with experimental manipulation of sex hormones (Roberts et al. 2001). Given that sex hormones change in a non-linear fashion throughout life, the effect of age on sex and Toxoplasma infection must also be taken into account.
Further complicating the interaction of sex, age, and T. gondii infection is the rhesus factor. At least five studies report that the RhD blood group positivity protects from effects of latent T. gondii infection, including prolongation of reaction time, increased risk of traffic accidents, and excessive pregnancy weight gain (Flegr 2013). In 185 patients with schizophrenia, RhD status significantly interacted with sex, protecting RhD-positive females from greater PANSS positive and distortion of reality scores (Holub et al. 2011). Given the complex interplay between genetic and environmental factors in schizophrenia, careful analysis will be necessary to understand treatment effect and target therapy to appropriate subgroups.
Future research
The time is ripe to evaluate antiparasitic drugs in Toxoplasma-infected patients with schizophrenia. At the time of writing (February 2017), there are no ongoing trials registered with the Stanley Medical Research Institute evaluating antiparasitic drugs in schizophrenia, with the exception of minocycline. There is an additional study (NCT02118610) registered with ClinicalTrials.gov evaluating L-tetrahydropalmatine, an anti-inflammatory agent with anti-protozoal properties; however, this agent is not market-approved in North America or Europe. A recent review (Neville et al. 2015) highlighted currently approved and investigational drugs with activity against different stages of Toxoplasma. Future research should examine agents with demonstrable activity against the chronic, bradyzoite stage of T. gondii in patients with schizophrenia. Notably, recent studies have demonstrated activity of spiramycin combined with metronidazole (Chew et al. 2012), didanosine (Sarciron et al. 1997), miltefosine (Eissa et al. 2015), sulfadiazine (Araujo and Remington 1974; Eissa et al. 2015), and atovaquone combined with clindamycin (Djurković-Djaković et al. 2002) against chronic Toxoplasma infection in vivo.
Minocycline, a broad-spectrum tetracycline antibiotic, also has activity against T. gondii cysts in an in vivo model (Chang et al. 1991). Interestingly, there is a growing body of evidence that minocycline augmentation therapy in schizophrenia results in lower PANSS total scores, and negative and general subscale scores (Oya et al. 2014). It is currently unknown how minocycline affects the schizophrenic brain; however, there is evidence that it also has antipsychotic properties in an uninfected rat model of schizophrenia (Fujita et al. 2008). Another potential, yet untested, mechanism for therapeutic effect in human schizophrenia is through reduction of Toxoplasma cyst burden. Future research should look to delineate the antiparasitic effect of minocycline from its neuromodulatory effect in humans with schizophrenia by IgG stratification.
There is robust evidence that Toxoplasma infection increases risk for schizophrenia, and seropositive cases appear to present with worse psychopathology. There have been four trials to date evaluating antiparasitics in Toxoplasma-positive patients with schizophrenia; however, there are significant challenges to these trials preventing extrapolation to other anti-Toxoplasma agents. Given the significant global burden of schizophrenia, there is a pressing need to evaluate novel therapy approaches.
Notes
Search strategy included querying Medline, Cochrane Controlled Trials Register, PsychInfo, and Embase with query “Toxoplasm* AND schizophreni*”. Resulting abstracts were screened for relevant randomized controlled trials in humans. Reference lists of included trials were screened for additional trials.
References
Amminger GP, McGorry PD, Berger GE et al (2007) Antibodies to infectious agents in individuals at ultrahigh risk for psychosis. Biol Psychiatry 61:1215–1217. doi:10.1016/j.biopsych.2006.09.034
Araujo FG, Remington JS (1974) Effect of clindamycin on acute and chronic toxoplasmosis in mice. Antimicrob Agents Chemother 5:647–651. doi:10.1128/AAC.5.6.647
Araujo FG, Shepard RM, Remington JS (1991) In vivo activity of the macrolide antibiotics azithromycin, roxithromycin and spiramycin against Toxoplasma gondii. Eur J Clin Microbiol Infect Dis 10:519–524. doi:10.1007/BF01963942
Buentello E (1958) Preliminary observations on the relationship between toxoplasmosis, lysergic acid and schizophrenia. Gac Med Mex 88:693–710
Çelik T, Kartalci Ş, Aytaş Ö et al (2015) Association between latent toxoplasmosis and clinical course of schizophrenia—continuous course of the disease is characteristic for Toxoplasma gondii-infected patients. Folia Parasitol 62:15. doi:10.14411/fp.2015.015
Chang HR, Arsenijevic D, Comte R et al (1994) Activity of epiroprim (Ro 11-8958), a dihydrofolate reductase inhibitor, alone and in combination with dapsone against Toxoplasma gondii. Antimicrob Agents Chemother 38:1803–1807. doi:10.1128/AAC.38.8.1803
Chang HR, Comte R, Piguet PF, Pechère JC (1991) Activity of minocycline against Toxoplasma gondii infection in mice. J Antimicrob Chemother 27:639–645. doi:10.1093/jac/27.5.639
Chew WK, Segarra I, Ambu S, Mak JW (2012) Significant reduction of brain cysts caused by Toxoplasma gondii after treatment with spiramycin coadministered with metronidazole in a mouse model of chronic toxoplasmosis. Antimicrob Agents Chemother 56:1762–1768. doi:10.1128/AAC.05183-11
Dickerson FB, Stallings CR, Boronow JJ et al (2009) A double-blind trial of adjunctive azithromycin in individuals with schizophrenia who are seropositive for Toxoplasma gondii. Schizophr Res 112:198–199. doi:10.1016/j.schres.2009.05.005
Dickerson F, Stallings CR, Vaughan C et al (2011) Artemisinin reduces the level of antibodies to gliadin in schizophrenia. Schizophr Res 129:196–200. doi:10.1016/j.schres.2011.04.010
Djurković-Djaković O, Milenković V, Nikolić A et al (2002) Efficacy of atovaquone combined with clindamycin against murine infection with a cystogenic (Me49) strain of Toxoplasma gondii. J Antimicrob Chemother 50:981–987. doi:10.1093/jac/dkf251
Dumas JL, Chang R, Mermillod B et al (1994) Evaluation of the efficacy of prolonged administration of azithromycin in a murine model of chronic toxoplasmosis. J Antimicrob Chemother 34:111–118. doi:10.1093/jac/34.1.111
Dumas JL, Pizzolato G, Pechère JC (1999) Evaluation of trimethoprim and sulphamethoxazole as monotherapy or in combination in the management of toxoplasmosis in murine models. Int J Antimicrob Agents 13:35–39. doi:10.1016/S0924-8579(99)00073-4
Dunay IR, Chan WC, Haynes RK, Sibley LD (2009) Artemisone and artemiside control acute and reactivated toxoplasmosis in a murine model. Antimicrob Agents Chemother 53:4450–4456. doi:10.1128/AAC.00502-09
Eissa MM, Barakat AMA, Amer EI, Younis LK (2015) Could miltefosine be used as a therapy for toxoplasmosis? Exp Parasitol 157:12–22. doi:10.1016/j.exppara.2015.06.005
Elsheikha HM, Büsselberg D, Zhu XQ (2016) The known and missing links between Toxoplasma gondii and schizophrenia. Metab Brain Dis 31:749–759. doi:10.1007/s11011-016-9822-1
Flegr J (2013) Influence of latent Toxoplasma infection on human personality, physiology and morphology: pros and cons of the Toxoplasma–human model in studying the manipulation hypothesis. J Exp Biol 216:127–133. doi:10.1242/jeb.073635
Flegr J (2015) Schizophrenia and Toxoplasma gondii: an undervalued association? Expert Rev Anti-Infect Ther 13:817–820. doi:10.1586/14787210.2015.1051033
Fond G, Boyer L, Gaman A et al (2015) Treatment with anti-toxoplasmic activity (TATA) for Toxoplasma positive patients with bipolar disorders or schizophrenia: a cross-sectional study. J Psychiatr Res 63:58–64. doi:10.1016/j.jpsychires.2015.02.011
Fond G, Macgregor A, Tamouza R et al (2014) Comparative analysis of anti-toxoplasmic activity of antipsychotic drugs and valproate. Eur Arch Psychiatry Clin Neurosci 264:179–183. doi:10.1007/s00406-013-0413-4
Fujita Y, Ishima T, Kunitachi S et al (2008) Phencyclidine-induced cognitive deficits in mice are improved by subsequent subchronic administration of the antibiotic drug minocycline. Prog Neuro-Psychopharmacol Biol Psychiatry 32:336–339. doi:10.1016/j.pnpbp.2007.08.031
Goodwin DG, Strobl JS, Lindsay DS (2011) Evaluation of five antischizophrenic agents against Toxoplasma gondii in human cell cultures. J Parasitol 97:148–151. doi:10.1645/GE-2536.1
Hencken CP, Jones-Brando L, Bordón C et al (2010) Thiazole, oxadiazole, and carboxamide derivatives of artemisinin are highly selective and potent inhibitors of Toxoplasma gondii. J Med Chem 53:3594. doi:10.1021/jm901857d
Holub D, Flegr J, Dragomirecká E et al (2013) Differences in onset of disease and severity of psychopathology between toxoplasmosis-related and toxoplasmosis-unrelated schizophrenia. Acta Psychiatr Scand 127:227–238. doi:10.1111/acps.12031
Holub D, Motlová L, Dragomirecká E et al (2011) Possible protective function of Rh factor in schizophrenia. Psychiatrie 15:37–42
Horacek J, Flegr J, Tintera J et al (2012) Latent toxoplasmosis reduces gray matter density in schizophrenia but not in controls: voxel-based-morphometry (VBM) study. World J Biol Psychiatry 13:501–509. doi:10.3109/15622975.2011.573809
Huskinson-Mark J, Araujo FG, Remington JS (1991) Evaluation of the effect of drugs on the cyst form of Toxoplasma gondii. J Infect Dis 164:170–171. doi:10.1093/infdis/164.1.170
Jones-Brando L, Torrey EF, Yolken R (2003) Drugs used in the treatment of schizophrenia and bipolar disorder inhibit the replication of Toxoplasma gondii. Schizophr Res 62:237–244. doi:10.1016/S0920-9964(02)00357-2
Lainson R (1958) Observations on the development and nature of pseudocysts and cysts of Toxoplasma gondii. Trans R Soc Trop Med Hyg 52:396–407. doi:10.1016/0035-9203(58)90123-8
Leucht S, Kane JM, Kissling W et al (2005) What does the PANSS mean? Schizophr Res 79:231–238. doi:10.1016/j.schres.2005.04.008
Lindová J, Kuběna AA, Šturcová H et al (2013) Pattern of money allocation in experimental games supports the stress hypothesis of gender differences in Toxoplasma gondii-induced behavioural changes. Folia Parasitol 57:136–142. doi:10.14411/fp.2010.017
Lindová J, Novotná M, Havlícek J et al (2006) Gender differences in behavioural changes induced by latent toxoplasmosis. Int J Parasitol 36:1485–1492. doi:10.1016/j.ijpara.2006.07.008
Loo CSN, Lam NSK, Yu D et al (2017) Artemisinin and its derivatives in treating protozoan infections beyond malaria. Pharmacol Res 117:192–217. doi:10.1016/j.phrs.2016.11.012
Mahmoud SS (2006) Azithromycin macrolids with a potent activity on chronic experimental toxopiasmosis. Iraqi J Pharm 6:1–5
Monroe JM, Buckley PF, Miller BJ (2015) Meta-analysis of anti-Toxoplasma gondii IgM antibodies in acute psychosis. Schizophr Bull 41:989–998. doi:10.1093/schbul/sbu159
Munić V, Kelnerić Ž, Mikac L, Eraković Haber V (2010) Differences in assessment of macrolide interaction with human MDR1 (ABCB1, P-gp) using rhodamine-123 efflux, ATPase activity and cellular accumulation assays. Eur J Pharm Sci 41:86–95. doi:10.1016/j.ejps.2010.05.016
Nair AB, Jacob S (2016) A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm 7:27–31. doi:10.4103/0976-0105.177703
Neville AJ, Zach SJ, Wang X et al (2015) Clinically available medicines demonstrating anti-Toxoplasma activity. Antimicrob Agents Chemother 59:7161–7169. doi:10.1128/AAC.02009-15
Nguyen B, Stadtsbaeder S (1983) Comparative effects of cotrimoxazole (trimethoprim-sulphamethoxazole), pyrimethamine-sulphadiazine and spiramycin during avirulent infection with Toxoplasma gondii (Beverley strain) in mice. Br J Pharmacol 79:923–928. doi:10.1111/j.1476-5381.1983.tb10537.x
Oya K, Kishi T, Iwata N (2014) Efficacy and tolerability of minocycline augmentation therapy in schizophrenia: a systematic review and meta-analysis of randomized controlled trials. Hum Psychopharmacol 29:483–491. doi:10.1002/hup.2426
Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents (2017) Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. https://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed 18 Feb 2017
Pappas G, Roussos N, Falagas ME (2009) Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol 39:1385–1394. doi:10.1016/j.ijpara.2009.04.003
Roberts CW, Walker W, Alexander J (2001) Sex-associated hormones and immunity to protozoan parasites. Clin Microbiol Rev 14:476–488. doi:10.1128/CMR.14.3.476-488.2001
Sarciron ME, Lawton P, Saccharin C et al (1997) Effects of 2′,3′-dideoxyinosine on Toxoplasma gondii cysts in mice. Antimicrob Agents Chemother 41:1531–1536
Schultz TL, Hencken CP, Woodard LE et al (2014) A thiazole derivative of artemisinin moderately reduces Toxoplasma gondii cyst burden in infected mice. J Parasitol 100:516–521. doi:10.1645/13-451.1
Sharif M, Sarvi S, Pagheh AS et al (2016) The efficacy of herbal medicines against Toxoplasma gondii during the last 3 decades: a systematic review. Can J Physiol Pharmacol 94:1237–1248. doi:10.1139/cjpp-2016-0039
Shibre T, Alem A, Abdulahi A et al (2010) Trimethoprim as adjuvant treatment in schizophrenia: a double-blind, randomized, placebo-controlled clinical trial. Schizophr Bull 36:846–851. doi:10.1093/schbul/sbn191
Sugie M, Asakura E, Zhao YL et al (2004) Possible involvement of the drug transporters P glycoprotein and multidrug resistance-associated protein Mrp2 in disposition of azithromycin. Antimicrob Agents Chemother 48:809–814. doi:10.1128/AAC.48.3.809-814.2004
Sutterland AL, Fond G, Kuin A et al (2015) Beyond the association. Toxoplasma gondii in schizophrenia, bipolar disorder, and addiction: systematic review and meta-analysis. Acta Psychiatr Scand 132:161–179. doi:10.1111/acps.12423
Vos T, Allen C, Arora M et al (2016) Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388:1545–1602. doi:10.1016/S0140-6736(16)31678-6
Wang HL, Wang GH, Li QW et al (2006) Prevalence of Toxoplasma infection in first-episode schizophrenia and comparison between Toxoplasma-seropositive and Toxoplasma-seronegative schizophrenia. Acta Psychiatr Scand 114:40–48. doi:10.1111/j.1600-0447.2006.00780.x
Wang HL, Xiang YT, Li QY et al (2014) The effect of artemether on psychotic symptoms and cognitive impairment in first-episode, antipsychotic drug-naive persons with schizophrenia seropositive to Toxoplasma gondii. J Psychiatr Res 53:119–124. doi:10.1016/j.jpsychires.2014.02.016
Webster JP, Lamberton PHL, Donnelly CA, Torrey EF (2006) Parasites as causative agents of human affective disorders? The impact of anti-psychotic, mood-stabilizer and anti-parasite medication on Toxoplasma gondii’s ability to alter host behaviour. Proc R Soc Lond B Biol Sci 273:1023–1030. doi:10.1098/rspb.2005.3413
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Rights and permissions
About this article
Cite this article
Chorlton, S.D. Toxoplasma gondii and schizophrenia: a review of published RCTs. Parasitol Res 116, 1793–1799 (2017). https://doi.org/10.1007/s00436-017-5478-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-017-5478-y