Abstract
Toxoplasmosis is one of the most common parasitic infections worldwide. An effective vaccine against human and animal toxoplasmosis is still needed to control this parasitosis. The polymorphic rhoptry proteins, ROP5 and ROP18, secreted by Toxoplasma gondii during the invasion of the host cell have been recently considered as promising vaccine antigens, as they appear to be the major determinants of T. gondii virulence in mice. The goal of this study was to evaluate their immunogenic and immunoprotective activity after their administration (separately or both recombinant proteins together) with the poly I:C as an adjuvant. Immunization of BALB/c and C3H/HeOuJ mice generated both cellular and humoral specific immune responses with some predominance of IgG1 antibodies. The spleen cells derived from vaccinated animals reacted to the parasite’s native antigens. Furthermore, the immunization led to a partial protection against acute and chronic toxoplasmosis. These findings confirm the previous assumptions about ROP5 and ROP18 antigens as valuable components of a subunit vaccine against toxoplasmosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infections caused by a protozoan parasite, Toxoplasma gondii, are widely prevalent in many warm-blooded animals and humans. It has a complex life cycle, in which it can effectively bypass the sexual stage in felids to be directly transmitted among the intermediate hosts (Dubey 2009). This ubiquitous parasite has emerged as one of the major opportunistic pathogens, especially for congenitally infected or immunocompromised individuals, who are at risk of developing severe or even fatal disease (Robert-Gangneux and Dardé 2012). Toxoplasmosis is also a considerable veterinary problem, as it may lead to abortions in economically important farm animals, such as sheep and goats (Tenter et al. 2000). Currently available drugs are only effective against the tachyzoite stage of T. gondii (present during the acute phase of infection) and do not eliminate the tissue cysts that persist life-long and are the source of reactivation (Sullivan Jr WJ et al. 2009). Hence, a safe and efficient vaccine against T. gondii would be extremely valuable for controlling toxoplasmosis in both animals and humans (Innes et al. 2009; Jongert et al. 2009; Verma and Khanna 2013).
Numerous vaccination studies have focused so far on the selection of the most protective antigens to compose an effective vaccine against toxoplasmosis (Zhang et al. 2013; Hiszczyńska-Sawicka et al. 2014). The immune system of the infected host can be activated by both the surface and the secretory antigens of T. gondii (Blader and Saeij 2009). The parasite’s rhoptries, which are unique apical secretory organelles, serve as a great source of promising vaccine candidates, including the polymorphic serine–threonine ROP5 and ROP18 kinases (Dlugonska 2008). Both of these proteins are secreted into the host cell upon invasion, and then they locate in the parasitophorous vacuole, where they cooperate to inhibit the functions of the immunity-related GTPases (IRGs) and the guanylate-binding proteins (GBPs). Since the ability of mice to resist the infection depends, to a large degree on the action of IRGs and GBPs, ROP5 and ROP18 have been recognized as key determinants of T. gondii virulence (Saeij et al. 2006; Taylor et al. 2006; El Hajj et al. 2007; Qiu et al. 2009; Fentress et al. 2010; Steinfeldt et al. 2010; Behnke et al. 2011; Niedelman et al. 2012; Selleck et al. 2013). Notably, the virulence differences between various T. gondii clonal lineages are largely due to the polymorphic variations in ROP5 (Reese et al. 2011; Reese et al. 2014) and ROP18 (Khan et al. 2009; Behnke et al. 2011; Jensen et al. 2015). These findings provide a clear premise to evaluate the potential of ROP5 and ROP18 as components of a subunit vaccine against toxoplasmosis.
The objective of the present study was to determine the immunogenic activity of recombinant ROP5 and ROP18 proteins, separately and in combination, in mice with different genetic backgrounds determining their innate susceptibility to T. gondii infection. Moreover, we used two different T. gondii strains representing genotypes of type I (T. gondii RH) and II (T. gondii DX) to assess the immunoprotective effect provided by the tested vaccines.
Material and methods
Mice
Female BALB/c (relatively resistant to toxoplasmosis) and C3H/HeOuJ (moderately susceptible to toxoplasmosis) inbred mice at the age of 10–12 weeks were used (Araujo et al. 1976; Vercammen et al. 2000). Animals were bred under conventional conditions and then used in the immunization and challenge experiments conducted according to the procedures accepted by the 9th Local Ethics Commission in Łódź, Poland.
Parasites
The highly virulent RH strain of T. gondii (type I) was maintained in vitro on the L929 cell line in the Iscove’s Modified Dulbecco’s Medium (Cytogen GmbH) supplemented with penicillin (100 kU/L, Sigma-Aldrich), streptomycin (100 mg/L, Sigma-Aldrich), 2-mercaptoethanol (50 μM, Sigma-Aldrich) and foetal calf serum (10 %, Cytogen GmbH). The low virulent, highly cyst-forming DX strain of T. gondii (type II) was obtained from the brains of chronically infected C57BL/6 mice, as previously described (Gatkowska et al. 2006).
Expression and purification of recombinant ROP5 and ROP18 proteins
The heterologous expression and purification of recombinant ROP5 and ROP18 proteins was thoroughly described in our previous work (Grzybowski et al. 2015). Briefly, genomic DNA of T. gondii RH was used as a template for ROP5 (GenBank: HQ916451.1) and ROP18 (GenBank: AM075204.1) gene amplification (Table 1). The sequence-verified inserts were subcloned into the pHIS-Parallel1 expression vector (GenBank: AF097413.1, Sheffield et al. 1999) and introduced into E. coli BL21(DE3) cells. The expression of recombinant proteins was induced by adding isopropyl β-d-1-thiogalactopyranoside (IPTG). The recombinant proteins were purified by affinity chromatography using His-Bind columns (Novagen). The concentrations of purified proteins were quantified using the Bradford Reagent (Sigma-Aldrich). The purity of eluted proteins was analysed by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) combined with densitometry (FluoroChem 8800, Alpha Innotec Corp.) and it was always higher than 90 %. The results of SDS-PAGE and western blot analyses were demonstrated previously (Grzybowski et al. 2015).
Preparation of Toxoplasma lysate antigen
The Toxoplasma lysate antigen (TLA) was prepared as previously described (Dziadek et al. 2009) with minor changes. Briefly, purified tachyzoites of the T. gondii RH strain were disrupted by ten subsequent cycles of freezing–thawing in liquid nitrogen. To remove the cell debris, the resulting protein extract was centrifuged for 20 min at 10,000×g at 4 °C and then filtered with a 0.2-μm sterile nitrocellulose filter (Sartorius). The total protein concentration was measured by the Bradford Reagent (Sigma). Aliquoted TLA samples were immediately lyophilized and stored at −20 °C. Prior to use, they were reconstituted to 1 mg/mL in phosphate-buffered saline (PBS).
Immunization procedure
Mice of both strains (BALB/c, C3H/HeOuJ) were randomly divided into five experimental groups, i.e. blank control, adjuvant control, ROP5, ROP18 and ROP5 + ROP18. The immunogenic activity (antibody and cellular assays) was assessed using six mice per group. The immunoprotective efficacy was determined using 12 (surveillance analysis in acute toxoplasmosis) or eight (assessment of the brain cyst load in chronic toxoplasmosis) mice per group. Animals were immunized subcutaneously with three doses of each vaccine with 2-week intervals. The final concentration of each recombinant antigen used alone or in combination was 15 μg per one dose for each mouse. The tested vaccines were adjuvanted with 25 μg of polyinosinic–polycytidylic acid (poly (I:C) HMW VacciGrade™, InvivoGen) per dose.
Specific antibody assays
Two weeks after the last immunization booster, control and vaccinated animals were killed and blood was collected. Analysis of IgG1/IgG2a isotype ratios was performed on the obtained serum samples using indirect enzyme-linked immunosorbent assay (ELISA). For this purpose, Maxisorp 96-well plates (Nunc) were coated overnight at 4 °C with 100 μL of recombinant antigens diluted in a 0.1 M carbonate buffer (pH 9.5) to optimal concentrations determined in the initial experiments (15 μg/mL for ROP5, ROP5-C and ROP18-C; 20 μg/mL for ROP18). The wells were then washed with PBS with Tween 20 (0.05 %) and blocked with skim milk (1 %) in PBS for 1 h at 37 °C. After another washing, the wells were incubated with mouse sera serially diluted from 1:50 in the blocking buffer. The third washing was followed by the addition of HRP-conjugated goat anti-mouse IgG1 or goat anti-mouse IgG2a secondary antibodies (Serotec) diluted 1:4000 in the blocking buffer (1 h, 37 °C). The immunoenzymatic reaction was developed using ABTS (Sigma) in a 0.05 M phosphate–citrate buffer (pH 4.5) containing hydrogen peroxide (0.25 μL of 30 % w/w H2O2 per 1 mL) and stopped after 20 min with SDS (1 %). The absorbance values were measured at 405 nm with the Multiscan EX automatic ELISA reader (Labsystems). All samples were run in duplicate. The optimal working dilutions of mice sera and anti-mouse secondary antibodies were determined in the preliminary titration experiments.
Lymphocyte proliferation assay
The lymphoproliferative response was assessed 2 weeks after administration of the last vaccine dose. Mice were euthanized and their spleens were isolated. The single-cell splenocyte suspensions were obtained by mechanical homogenization followed by erythrocyte lysis using ammonium chloride solution (155 mM NH4Cl, pH 7.2). After several extensive washes with Iscove’s Modified Dulbecco’s Medium supplemented with penicillin (100 kU/L), streptomycin (100 mg/L), 2-mercaptoethanol (50 μM) and foetal calf serum (5 %), the spleen cells were resuspended in the same culture medium and counted. The cell viability was determined by the trypan blue exclusion method and was always higher than 90 %. The spleen cells were seeded at 5 × 105 cells in 100 μL of the culture medium per well into a 96-well tissue culture plates (Falcon). Another 100 μL of the medium added contained recombinant ROP5 or ROP18 proteins or TLA. The final antigen concentration of each antigen was 10 μg/mL. The cells cultured without any antigen or stimulated with concanavalin A (ConA, Sigma-Aldrich) at the concentration of 2.5 μg/mL served, respectively, as negative or positive controls of proliferation. After 92 h of incubation, 20 μL of 3-(4,5-methylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT, Sigma-Aldrich) at a concentration of 5 mg/mL in PBS was added to each well. The mouse splenocytes were cultured for further 4 h in the same conditions followed by the centrifugation at 583×g for 5 min. The supernatants were removed and the formazan crystals were dissolved with 150 μL of DMSO and 25 μL glycine buffer (pH 10.5). The absorbance values were measured at 570 nm with the Multiscan EX automatic ELISA reader (Labsystems). The stimulation index (SI) was calculated as the ratio of the mean absorbance of the wells containing antigen-stimulated cells to the mean absorbance value of the wells containing cells with medium only. All experimental and control samples were run in triplicate. The optimal number of spleen cells used in proliferative assays combined with the MTT reduction assay had been determined in the preliminary experiments.
Cytokine assays
Two weeks after the last booster, control and immunized mice were euthanized and their spleens were aseptically isolated. The antigen-stimulated microcultures of spleen cells were prepared as described for the lymphocyte proliferation assay and maintained for 3 days at 37 °C and 10 % CO2. Then, the concentrations of mouse IFN-γ or IL-10 released into the post-culture supernatants were estimated using ELISA Max™ Standard Sets (BioLegend) according to the manufacturer’s protocol. The immune complexes were detected using 100 μL of TMB Substrate Solution (BioLegend), and the reaction was stopped with an equal volume of sulphuric acid solution (1 M H2SO4, Sigma-Aldrich). The absorbance values were measured with the Multiscan EX automatic ELISA reader (Labsystems); the absorbance at 570 nm was subtracted from the absorbance at 450 nm. The unknown cytokine concentrations were determined based on the standard curves, which were plotted for each assay. All experimental and control samples were run in duplicate.
Flow cytometry
The co-expression of CD69 with CD4 or CD8 molecules on spleen cells was determined by flow cytometry. Briefly, the single-cell splenocyte suspensions, prepared as described above for lymphoproliferation assay, were washed and resuspended with PBS. The cells were then incubated for 30 min at 4 °C with a mixture of the following monoclonal antibodies: FITC-conjugated anti-mouse CD69 (0.5 μg per test), PE-cyanine5-conjugated anti-mouse CD4 (0.06 μg per test) and PE-conjugated anti-mouse CD8a (0.25 μg per test) or irrelevant isotype-matched monoclonal antibodies used as controls. All antibodies were purchased from eBioscience. After another two washes with ice-cold PBS, the cells were analysed using the FACS LSRII (BD) by collecting a minimum of 10.000 events. The data were then analysed with FlowJo software.
Challenge infection procedures
Two weeks after the last vaccine booster, immunized and control mice were intraperitoneally challenged with a lethal dose of in vivo propagated 1 × 103 T. gondii RH tachyzoites or with a nonlethal dose of five tissue cysts of the T. gondii DX strain in order to induce, respectively, an acute or chronic infection. The survival periods were recorded daily until all lethally infected mice died. Four weeks after the challenge with the cyst-forming T. gondii DX strain, all infected animals were euthanized. After isolation, the brains were placed in tubes containing PBS (final volume 2.5 mL). Following a mechanical disruption, the brain cyst load was determined by counting 25 or 50 μL of each homogenate under an inverted Olympus microscope at the ×200 magnification. All samples were counted at least in duplicate.
Statistical analysis
All statistical analyses were performed using Statistica 10.0 software (StatSoft). The Mann–Whitney U test was used for comparing two groups. For multiple comparisons, the Kruskal–Wallis ANOVA by ranks and the median test were performed. The survival periods were analysed by the Kaplan–Meier estimator and were compared using the log-rank (Mantel–Cox) test.
Results
Humoral immune response
To evaluate the intensity and the immune profile (Th1 or Th2) of humoral responses induced by immunization of experimental animals with recombinant ROP5 or ROP18 proteins, the titres of antigen-specific IgG1 and IgG2a antibodies were determined. Both recombinant antigens, administered separately or in combination, induced a significant IgG1 and IgG2a production in BALB/c and C3H/HeOuJ mice, which was estimated in ELISAs using the recombinant full-length ROP5 and ROP18 proteins (used for immunization), as well as their C-terminal fragments (Fig. 1).
In BALB/c mice, the levels of anti-ROP5, anti-ROP5-C, anti-ROP18 and anti-ROP18-C IgG1 antibodies were not significantly different when comparing the single-antigen to the combined vaccine (IgG1, 0.160 ≤ p ≤ 0.641). Similarly, there were no significant differences in IgG2a syntheses (IgG2a, 0.173 ≤ p ≤ 1.000). In the analogous analysis performed in C3H/HeOuJ mice, the levels of anti-ROP5 and anti-ROP18 IgG1 antibodies were not significantly different when comparing the single antigen with the combined vaccine (IgG1, 0.0729 ≤ p ≤ 0.118; IgG2a, p = 0.118), but the levels of IgG1 antibodies against C-terminal fragments of ROP5 or ROP18 were significantly higher in mice immunized with the combined vaccine (anti-ROP5-C, p = 0.00548; anti-ROP18-C, p = 0.00146). Similarly, the levels of anti-ROP5, anti-ROP5-C and anti-ROP18-C IgG2a antibodies were higher in mice, which have been given the “ROP5 + ROP18” vaccine (0.00317 ≤ p ≤ 0.323); only the levels of anti-ROP18 IgG2a antibodies were not significantly different (p = 0.118).
The analysis of the IgG1/IgG2a antibody ratios (Fig. 1) showed that immunization with recombinant ROP5 or ROP18 or both proteins induced a mixed type (Th1/Th2) immune response with a statistically significant predominance of IgG1 antibodies revealed for anti-ROP18 antibodies in ROP18-immunized BALB/c mice (p = 0.00624), anti-ROP5 antibodies in (ROP5 + ROP18)-immunized BALB/c mice (p = 0.0374) and anti-ROP5 and anti-ROP5-C antibodies in ROP5-immunized C3H/HeOuJ mice (p = 0.00677).
In most cases, the determined titres of antigen-specific antibodies were significantly higher in C3H/HeOuJ mice compared to those in BALB/c mice (0.00101 ≤ p ≤ 0.0101). No strain-dependent differences were observed for anti-ROP18 (p = 0.199), anti-ROP18-C (p = 1.000) IgG1 and anti-ROP18-C (p = 0.317) IgG2a antibodies in ROP18-immunized mice (Fig. 1).
Proliferative response of spleen cells
The efficacy of immunization was also determined by estimation of the specific lymphoproliferative response, which can serve as a sensitive marker of established cellular immunity in vaccinated animals.
In BALB/c mice, the statistically significant antigen-specific proliferation was noted in ROP5-stimulated splenocytes derived from ROP5- and (ROP5 + ROP18)-immunized animals as compared to PBS or poly (I:C) controls (0.00887 ≤ p ≤ 0.0288; Table 2). No statistically significant proliferation was observed in ROP5-C-stimulated spleen cells. The presence of recombinant ROP18 protein triggered a significant proliferation in the cell cultures derived from ROP18- (p = 0.0162, compared to the “PBS” group) and (ROP5 + ROP18)-immunized mice (0.00135 ≤ p ≤ 0.0261). The C-terminal fragment of ROP18 induced significant proliferation of splenocytes isolated from ROP18-immunized mice (0.00146 ≤ p ≤ 0.00378). The stimulation with TLA preparation, used as a source of native T. gondii antigens, resulted in an increased proliferation only in the ROP5 + ROP18 experimental group (p = 0.0391, compared to the “poly (I:C)” group).
In C3H/HeOuJ mice (Table 2), the statistically significant splenocyte proliferation was observed in ROP5-stimulated cultures derived from (ROP5 + ROP18)-immunized animals (p = 0.0172). Similarly to BALB/c mice, no significant proliferation was revealed in ROP5-C-stimulated cell cultures. The recombinant ROP18 protein induced an increased cell proliferation in the cultures derived from the (ROP5 + ROP18)-immunized mice (0.0198 ≤ p ≤ 0.0449). The ROP18-C protein stimulated the ROP18- and (ROP5 + ROP18)-derived cells to increased proliferation (0.0120 ≤ p ≤ 0.0376, compared to the PBS group). As in BALB/c mice, the TLA stimulation led to increased lymphoproliferation only in the ROP5 + ROP18 group (0.00502 ≤ p ≤ 0.0189).
No statistically significant strain-dependent differences were observed in the splenocyte proliferation assays between BALB/c and C3H/HeOuJ mice (Table 2).
Cytokine production
The supernatants derived from spleen cell cultures stimulated with recombinant and native (TLA) T. gondii antigens were used to detect the antigen-specific secretion of Th1- (IFN-γ) and Th2-type (IL-10) cytokines.
In BALB/c mice (Fig. 2, upper graph), the increased release of IFN-γ was observed only in the presence of ROP18 (“ROP18” group, 0.00267 ≤ p ≤ 0.0144; ROP5 + ROP18 group, 0.0469 ≤ p ≤ 0.157) and ROP18-C (ROP18 group, 0.00247 ≤ p ≤ 0.00625) proteins in the culture medium. The cells derived from immunized BALB/c mice did not significantly respond to the TLA stimulation; however, the highest IFN-γ production was detected in the ROP5 + ROP18 group. On the contrary, in C3H/HeOuJ mice (Fig. 2, lower graph), a significant antigen-specific IFN-γ synthesis was noted for all recombinant antigens, as well as for the native TLA preparation, when compared to the corresponding cultures in the PBS and poly (I:C) groups. The highest amounts of IFN-γ were detected in the supernatants derived from the ROP5 + ROP18 group of vaccinated animals (0.000525 ≤ p ≤ 0.00523). Moreover, the antigen-stimulated spleen cells from immunized C3H/HeOuJ mice produced significantly more IFN-γ than BALB/c mice in the “ROP5” (0.003 ≤ p ≤ 0.0383) and the ROP5 + ROP18 (0.00341 ≤ p ≤ 0.0124) groups.
As shown in Fig. 3, the overall synthesis of IL-10 in BALB/c mice was much lower than in C3H/HeOuJ mice, both in the control and the immunized animals (0.00341 ≤ p ≤ 0.0306). However, in BALB/c mice (upper graph), the statistically significant release of IL-10 was exhibited by ROP5- and ROP5-C-stimulated splenocytes derived from the ROP5 group (ROP5, 0.00397 ≤ p ≤ 0.00525; ROP5-C, 0.0173 ≤ p ≤ 0.0214), ROP18-stimulated splenocytes derived from the ROP18 and ROP5 + ROP18 groups (0.00397 ≤ p ≤ 0.0387), ROP18-C-stimulated splenocytes derived from the ROP18 group (0.00785 ≤ p ≤ 0.00847) and TLA-stimulated splenocytes derived from the ROP5 group (0.0410 ≤ p ≤ 0.0440).
In C3H/HeJ mice (Fig. 3, lower graph), the statistically significant production of IL-10 was found in the cultures of ROP5- and ROP5-C-stimulated cells derived from the ROP5 + ROP18 group (0.000677 ≤ p ≤ 0.00288 for ROP5, 0.0199 ≤ p ≤ 0.0333 for ROP5-C), ROP18- and ROP18-C-stimulated cell derived from the ROP18 (p = 0.0442 for ROP18, p = 0.0406 for ROP18-C) and ROP5 + ROP18 (0.00201 ≤ p ≤ 0.00362 for ROP18, 0.00436 ≤ p ≤ 0.00872) groups. Importantly, the TLA-stimulated cells derived from (ROP5 + ROP18)-immunized also produced significant amounts of IL-10 (0.000351 ≤ p ≤ 0.00123).
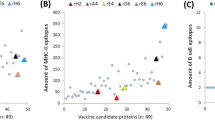
Activation of CD4+ and CD8+ T cells
Two weeks after the last vaccination booster, the activation of immune spleen cells was evaluated judging by the expression of CD69 molecule considered a very early activation marker (Borges et al. 2007). The immunization with ROP5 or ROP18 proteins did not change the overall percentage of the CD69+ cells neither in BALB/c or C3H/HeJ mice, as compared with the control groups. The only statistically significant differences were strain-dependent, i.e. the ROP5- and ROP18-immunized BALB/c mice showed a higher percentage of activated cells than the corresponding C3H/HeOuJ mice (0.00813 ≤ p ≤ 0.0268).
To distinguish the profile of the generated immune response, the co-expression of CD69 with CD4 or CD8 molecules on splenic lymphocytes was also determined (Fig. 4). The immunization with ROP5 or ROP18 T. gondii proteins did not significantly change the level of neither CD69+CD4+ or CD69+CD8+ splenic lymphocytes, as compared to the control groups receiving PBS or the poly (I:C) adjuvant alone. When analysing the CD4+/CD8+ ratios among CD69+ cells, the percentage of activated CD4+ was significantly higher than the percentage of activated CD8+ splenocytes in control groups (BALB/c, 0.00508 ≤ p ≤ 0.0304; C3H/HeJ, 0.0122 ≤ p ≤ 0.0304), as well as in all three immunized groups of C3H/HeOuJ mice (0.00195 ≤ p ≤ 0.0215) and the (ROP5 + ROP18)-immunized BALB/c mice (p = 0.00508). However, in BALB/c mice immunized with ROP5 or ROP18 protein (separately), there was no significant difference between the percentage of activated CD4+ and CD8+ immune cells (0.173 ≤ p ≤ 0.230).
Protective activity
To evaluate the immunoprotective activity of the experimental vaccines, the low-virulent T. gondii DX strain (type II) was used to induce the chronic infection with the aim of assessing the ability of the tested vaccines to prevent the tissue cyst formation (Fig. 5).
The reduction of the brain cyst burden in immunized mice was only partial, since both control and vaccinated animals developed a chronic T. gondii infection (Fig. 5). The statistically significant reduction in the brain cyst load was demonstrated only in the ROP18-immunized BALB/c mice, where the protection rate reached 57 % (325 cysts per brain), as compared with the poly (I:C) control group (763 cysts per brain; p = 0.0232). In C3H/HeOuJ mice, the statistically significant protection against chronic toxoplasmosis was observed only in (ROP5 + ROP18)-immunized animals, where the protection rate reached 46 % (1833 cyst per brain), as compared with the poly (I:C) control group (3400 cysts per brain; p = 0.0408). Moreover, very clear strain-dependent differences could be seen in the susceptibility to chronic T. gondii invasion between BALB/c and C3H/HeOuJ mice. In all five experimental groups, the estimated brain cyst load was significantly higher in C3H/HeOuJ than in BALB/c mice (0.00146 ≤ p ≤ 0.0107).
In order to examine whether the immunization resulted in an effective protection against acute toxoplasmosis, the highly virulent T. gondii RH strain (type I) was used (Fig. 6). In both BALB/c and C3H/HeOuJ mice, all three experimental vaccines provided a statistically significant partial protection against acute T. gondii infection, which was manifested by a prolonged time of survival after a lethal challenge, as compared with the control groups (0.00153 ≤ p ≤ 0.0144). Noteworthy, 25 % of the ROP18-immunized BALB/c mice survived the infection. There were no significant differences between PBS and poly (I:C) groups neither in BALB/c or C3H/HeOuJ mice. The only strain-dependent difference was revealed between the poly (I:C) groups, as the C3H/OuHeJ mice succumbed to the infection later than the BALB/c mice (p = 0.0289).
Discussion
The global distribution and the ability to infect virtually all warm-blooded animals make the protozoan T. gondii an extraordinary and successful parasite with up to one third of the human population being infected (Montoya and Liesenfeld 2004). The lack of effective drugs with low toxicity together with the overall socio-economic impact of toxoplasmosis makes the development of T. gondii vaccine an important global challenge. The currently available veterinary vaccine (Toxovax®) is based on live tachyzoites of the attenuated S48 T. gondii strain. Although it limits the incidence of abortion in sheep, it is unknown if the vaccine aids in the reduction of meat contamination with tissue cysts (Roberts et al. 2014). A rational strategic approach to a novel veterinary vaccine seems to be the immunization of domestic cats in order to disrupt the zoonotic cycle of T. gondii and thereby to reduce the frequency of infection in both livestock and humans. Besides, there is an urgent need to develop a vaccine suitable for humans to prevent the infection or at least the incidence of clinical disease in congenitally infected or immunocompromised individuals (Jongert et al. 2009; Verma and Khanna 2013).
The recent progress in studies on identifying key determinants of T. gondii virulence prompted us to investigate the immunoprophylactic potential of recombinant ROP5 and ROP18 proteins, members of the ROP2 superfamily (El Hajj et al. 2006). These highly polymorphic rhoptry kinases are essential virulence factors of T. gondii. The pseudokinase ROP5 is the major determinant of acute virulence in mice (Behnke et al. 2011; Reese and Boyle 2012). It complexes with the active kinase ROP18, which evolved to target the immunity-related GTPases (IRGs). Thus, the combined activity of ROP5 and ROP18 thwarts the innate immune mechanisms thereby protecting the parasites from intracellular killing (Fentress and Sibley 2011; Etheridge et al. 2014).
A rational approach towards specific immunoprophylaxis involves the construction of vaccines which are highly protective, but also safe and immunologically strictly defined. Recombinant subunit vaccines are attractive tools in the development of protective immunity against T. gondii. The major advantage of subunit vaccines is their high safety, so they virtually may be administered regardless of the patient’s health status. In this study, we evaluated the immunogenic and protective activity of recombinant full-length ROP5 and ROP18 proteins adjuvanted with poly (I:C)—a synthetic analogue of double-stranded RNA (dsRNA) recognized by TLR3 receptors (Salem et al. 2005). To our knowledge, this is the first report on using these proteins as a bivalent subunit vaccine.
The cellular immune response is the key protective mechanism during the T. gondii invasion (Pifer and Yarovinsky 2011). The appropriate vaccine design should consider the direction of the Th response generated after immunization and thus the vaccine against toxoplasmosis needs to stimulate effectively the synthesis of IFN-γ, the major effector cytokine affecting the fate of T. gondii (Sturge and Yarovinsky 2014). Since it principally restricts the parasite proliferation in the acute phase of infection and thwarts the reactivation of dormant parasites enclosed in tissue cysts, it is considered to be the main determinant of the protective vaccine-induced immunity against T. gondii (Suzuki et al. 1988). We found that the immunization with ROP5 or ROP18 proteins resulted in a significant IFN-γ production by murine splenocytes stimulated in vitro by antigens used for vaccination. Importantly, the TLA preparation, used as a source of native T. gondii antigens, also stimulated the cells to the significant production of IFN-γ. On the other hand, we measured the levels of IL-10 which is a Th2-type cytokine. IL-10 restores the immune homeostasis by regulating the inflammatory response during the acute T. gondii infection (Wilson et al. 2005; Dupont et al. 2012) but may also contribute to the inhibition of the T and B lymphocyte proliferation and thus suppress the killing of T. gondii by macrophages (Abdollahi et al. 2013). Significant amounts of this regulatory cytokine were produced by cells derived from both mouse strains; however, evident differences between C3H/HeOuJ and BALB/c were shown. The increased level of this cytokine could contribute to the weakening of the lymphoproliferative response, which was only moderately enhanced in both BALB/c and C3H/HeOuJ strains. The stimulation index (SI) for ROP5-pulsed splenocytes from ROP5-immunized mice was comparable with the SI observed by Zheng et al. (2013). Interestingly, they observed about twofold increase of proliferation after the addition of recombinant SAG1 antigen to the vaccine. The flow cytometry analysis of splenocytes derived from ROP5- or ROP18-vaccinated mice did not show any significant changes in the percentage of activated (CD69+) immune cells after vaccination (without in vitro restimulation). In general, the levels of CD69+CD4+ cells were higher than those observed for CD69+CD8+ cells; however, in BALB/c mice immunized with either ROP5 or ROP18, the differences were less polarized and the CD4+/CD8+ ratios were the lowest which may indicate a weak stimulation of the cytotoxic immune mechanisms. The crucial parameter for inducing a robust cytotoxic T cell response, particularly significant for vaccines against intracellular pathogens, is the antigen delivery system. Subunit vaccines stimulate mostly the exogenous antigen presentation pathway (MHC class II restricted) which may lead to a limited activation of CD8+ T cells. Hence, a stronger activation of CD4+ and CD8+ T cells was reported upon the use of ROP5- (Chen et al. 2015) or ROP18-based (Yuan et al. 2011) DNA vaccines.
The natural T. gondii infection leads to the activation of B cells and the subsequent production of specific antibodies (Filisetti and Candolfi 2004). The efficient humoral response is also required for the vaccine-induced resistance to virulent tachyzoites, as the antibodies may act protectively by limiting the infection of host cells by blocking their receptors (Sayles et al. 2000). Our study demonstrated that subcutaneous immunization with ROP5 or ROP18 proteins adjuvanted with poly (I:C) triggered a significant antibody response, which was more robust in C3H/HeOuJ than in BALB/c mice. Moreover, in C3H/HeJ mice, the levels of ROP5- and ROP18-specific antibodies were higher in the group of animals immunized with the bivalent vaccine. Since different antigens often lead to the preferential development of Th1 or Th2 responses resulting in a distinctive production of, respectively, IgG2a or IgG1 antibodies (Mosmann and Coffman 1989), we analysed the ratios of IgG1/IgG2a in the sera of immunized mice. We found that a mixed type (Th1/Th2) of immune response was elicited with some predominance of the IgG1 antibodies, which are specific for Th2 profile. These findings are consistent with our previous observations (Dziadek et al. 2009, 2011, 2012) showing that BALB/c and C3H/HeOuJ mice immunized with other recombinant rhoptry proteins (ROP2, ROP4) developed a mixed type of the immune response with a predominant IgG1 synthesis. Similar outcomes were revealed by Qu et al. (2013a), who analysed the protection in mice immunized with recombinant ROP18 co-administered with gingenoside Re as an adjuvant. However, these observations are contrary to the results obtained by Zheng et al. (2013), who immunized BALB/c mice with recombinant ROP5 and demonstrated a predominance of specific IgG2a antibodies, which is generally observed for DNA vaccines (Yuan et al. 2011; Qu et al. 2013b; Chen et al. 2015; Li et al. 2015) and occurs naturally during T. gondii infection (Denkers and Gazzinelli 1998).
The primary goal of vaccination is to provide an effective protection against the pathogen. In the case of T. gondii, the ideal vaccine construct should be aimed at preventing both the acute and the chronic toxoplasmosis. Hence, in our study, we performed a parallel challenge using two strains of different T. gondii lineages, i.e. a highly virulent RH (type I) and low-virulent cyst-forming DX (type II) strain. The studied vaccines provided a partial protection against chronic infection, as estimated by enumeration of the brain cysts. The most effective were the ROP18 vaccine in BALB/c mice and the ROP5 + ROP18 bivalent vaccine in C3H/HeOuJ mice. In the model of acute infection, all three tested vaccines significantly increased the time of survival after a lethal challenge, and noteworthy, a part of the ROP18-immunized BALB/c mice were even able to overcome the disease. We found no significant synergistic effect after bivalent immunization with ROP5 + ROP18. The above findings support the previous observation of Zheng et al. (2013) and Qu et al. (2013a), who also demonstrated a prolonged mice survival after vaccination with, respectively, recombinant ROP5 and ROP18 proteins. Furthermore, few other studies on ROP5- or ROP18-based DNA vaccines showed similar results (Yuan et al. 2011; Qu et al. 2013b; Chen et al. 2015; Li et al. 2015).
In conclusion, our results demonstrated that immunization with ROP5 and ROP18 proteins leads to the activation of both humoral and cellular immune mechanisms, resulting in the partial protection against highly virulent and cyst-forming strains of T. gondii. Although the outcomes of the experiments might not be fully satisfactory, these results provide additional evidence that ROP5 and ROP18 proteins may be valuable components of a multi-antigenic vaccine against T. gondii.
References
Abdollahi SH, Ayoobi F, Khorramdelazad H, Hassanshahi G, Ahmadabadi BN, Rezayati M, Ravary A, Shamsizadeh A, Arababadi MK (2013) Interleukin-10 serum levels after vaccination with in vivo prepared Toxoplasma gondii excreted/secreted antigens. Oman Med J 28:112–5
Araujo FG, Williams DM, Grumet FC, Remington JS (1976) Strain-dependent differences in murine susceptibility to toxoplasma. Infect Immun 13:1528–1530
Behnke MS, Khan A, Wootton JC, Dubey JP, Tang K, Sibley LD (2011) Virulence differences in Toxoplasma mediated by amplification of a family of polymorphic pseudokinases. Proc Natl Acad Sci U S A 108:9631–9636
Blader IJ, Saeij JP (2009) Communication between Toxoplasma gondii and its host: impact on parasite growth, development, immune evasion, and virulence. APMIS 117:458–476
Borges O, Borchard G, de Sousa A, Junginger HE, Cordeiro-da-Silva A (2007) Induction of lymphocytes activated marker CD69 following exposure to chitosan and alginate biopolymers. Int J Pharm 337:254–264
Chen J, Li ZY, Petersen E, Huang SY, Zhou DH, Zhu XQ (2015) DNA vaccination with genes encoding Toxoplasma gondii antigens ROP5 and GRA15 induces protective immunity against toxoplasmosis in Kunming mice. Expert Rev Vaccines 14:617–624
Denkers EY, Gazzinelli RT (1998) Regulation and function of T-cell-mediated immunity during Toxoplasma gondii infection. Clin Microbiol Rev 11:569–588
Dlugonska H (2008) Toxoplasma rhoptries: unique secretory organelles and source of promising vaccine proteins for immunoprevention of toxoplasmosis. J Biomed Biotechnol 2008:632424
Dubey JP (2009) History of the discovery of the life cycle of Toxoplasma gondii. Int J Parasitol 39:877–882
Dupont CD, Christian DA, Hunter CA (2012) Immune response and immunopathology during toxoplasmosis. Semin Immunopathol 34:793–813
Dziadek B, Gatkowska J, Brzostek A, Dziadek J, Dzitko K, Długonska H (2009) Toxoplasma gondii: the immunogenic and protective efficacy of recombinant ROP2 and ROP4 rhoptry proteins in murine experimental toxoplasmosis. Exp Parasitol 123:81–89
Dziadek B, Gatkowska J, Brzostek A, Dziadek J, Dzitko K, Grzybowski M, Dlugonska H (2011) Evaluation of three recombinant multi-antigenic vaccines composed of surface and secretory antigens of Toxoplasma gondii in murine models of experimental toxoplasmosis. Vaccine 29:821–830
Dziadek B, Gatkowska J, Grzybowski M, Dziadek J, Dzitko K, Dlugonska H (2012) Toxoplasma gondii: the vaccine potential of three trivalent antigen-cocktails composed of recombinant ROP2, ROP4, GRA4 and SAG1 proteins against chronic toxoplasmosis in BALB/c mice. Exp Parasitol 131:133–138
El Hajj H, Demey E, Poncet J, Lebrun M, Wu B, Galéotti N, Fourmaux MN, Mercereau-Puijalon O, Vial H, Labesse G, Dubremetz JF (2006) The ROP2 family of Toxoplasma gondii rhoptry proteins: proteomic and genomic characterization and molecular modeling. Proteomics 6:5773–5784
El Hajj H, Lebrun M, Arold ST, Vial H, Labesse G, Dubremetz JF (2007) ROP18 is a rhoptry kinase controlling the intracellular proliferation of Toxoplasma gondii. PLoS Pathog 3, e14
Etheridge RD, Alaganan A, Tang K, Lou HJ, Turk BE, Sibley LD (2014) The Toxoplasma pseudokinase ROP5 forms complexes with ROP18 and ROP17 kinases that synergize to control acute virulence in mice. Cell Host Microbe 15:537–50
Fentress SJ, Sibley LD (2011) The secreted kinase ROP18 defends Toxoplasma’s border. Bioessays 33:693–700
Fentress SJ, Behnke MS, Dunay IR, Mashayekhi M, Rommereim LM, Fox BA, Bzik DJ, Taylor GA, Turk BE, Lichti CF, Townsend RR, Qiu W, Hui R, Beatty WL, Sibley LD (2010) Phosphorylation of immunity-related GTPases by a Toxoplasma gondii-secreted kinase promotes macrophage survival and virulence. Cell Host Microbe 8:484–495
Filisetti D, Candolfi E (2004) Immune response to Toxoplasma gondii. Ann Ist Super Sanita 40:71–80
Gatkowska J, Hiszczynska-Sawicka E, Kur J, Holec L, Długonska H (2006) Toxoplasma gondii: an evaluation of diagnostic value of recombinant antigens in a murine model. Exp Parasitol 114:220–227
Grzybowski MM, Dziadek B, Dziadek J, Gatkowska J, Dzitko K, Długońska H (2015) Toxoplasma gondii: cloning. expression and immunoreactivity of recombinant ROP5 and ROP18 antigens. Exp Parasitol 150:1–6
Hiszczyńska-Sawicka E, Gatkowska JM, Grzybowski MM, Długońska H (2014) Veterinary vaccines against toxoplasmosis. Parasitology 141:1365–1378
Innes EA, Bartley PM, Maley S, Katzer F, Buxton D (2009) Veterinary vaccines against Toxoplasma gondii. Mem Inst Oswaldo Cruz 104:246–51
Jensen KD, Camejo A, Melo MB, Cordeiro C, Julien L, Grotenbreg GM, Frickel EM, Ploegh HL, Young L, Saeij JP (2015) Toxoplasma gondii superinfection and virulence during secondary infection correlate with the exact ROP5/ROP18 allelic combination. MBio 6, e02280
Jongert E, Roberts CW, Gargano N, Förster-Waldl E, Petersen E (2009) Vaccines against Toxoplasma gondii: challenges and opportunities. Mem Inst Oswaldo Cruz 104:252–66
Khan A, Taylor S, Ajioka JW, Rosenthal BM, Sibley LD (2009) Selection at a single locus leads to widespread expansion of Toxoplasma gondii lineages that are virulent in mice. PLoS Genet 5, e1000404
Li XZ, Wang XH, Xia LJ, Weng YB, Hernandez JA, Tu LQ, Li LT, Li SJ, Yuan ZG (2015) Protective efficacy of recombinant canine adenovirus type-2 expressing TgROP18 (CAV-2-ROP18) against acute and chronic Toxoplasma gondii infection in mice. BMC Infect Dis 15:114
Montoya JG, Liesenfeld O (2004) Toxoplasmosis. Lancet 363:1965–1976
Mosmann TR, Coffman RL (1989) TH1 and TH2 cells: different patterns of lymphokine secretion lead to different functional properties. Annu Rev Immunol 7:145–173
Niedelman W, Gold DA, Rosowski EE, Sprokholt JK, Lim D, Farid Arenas A, Melo MB, Spooner E, Yaffe MB, Saeij JP (2012) The rhoptry proteins ROP18 and ROP5 mediate Toxoplasma gondii evasion of the murine, but not the human, interferon-gamma response. PLoS Pathog 8, e1002784
Pifer R, Yarovinsky F (2011) Innate responses to Toxoplasma gondii in mice and humans. Trends Parasitol 27:388–93
Qiu W, Wernimont A, Tang K, Taylor S, Lunin V, Schapira M, Fentress S, Hui R, Sibley LD (2009) Novel structural and regulatory features of rhoptry secretory kinases in Toxoplasma gondii. EMBO J 28:969–79
Qu D, Han J, Du A (2013a) Enhancement of protective immune response to recombinant Toxoplasma gondii ROP18 antigen by ginsenoside Re. Exp Parasitol 135:234–239
Qu D, Han J, Du A (2013b) Evaluation of protective effect of multiantigenic DNA vaccine encoding MIC3 and ROP18 antigen segments of Toxoplasma gondii in mice. Parasitol Res 112:2593–2599
Reese ML, Boyle JP (2012) Virulence without catalysis: how can a pseudokinase affect host cell signaling? Trends Parasitol 28:53–57
Reese ML, Zeiner GM, Saeij JP, Boothroyd JC, Boyle JP (2011) Polymorphic family of injected pseudokinases is paramount in Toxoplasma virulence. Proc Natl Acad Sci U S A 108:9625–9630
Reese ML, Shah N, Boothroyd JC (2014) The Toxoplasma pseudokinase ROP5 is an allosteric inhibitor of the immunity-related GTPases. J Biol Chem 289:27849–27858
Robert-Gangneux F, Dardé ML (2012) Epidemiology of and diagnostic strategies for toxoplasmosis. Clin Microbiol Rev 25:264–296
Roberts CW, McLeody R, Henriquez FL, Alexander J (2014) Vaccination against toxoplasmosis: current status and future prospects. In: Weiss LM, Kim K (ed) Toxoplasma gondii. The model apicomplexan – perspectives and methods, 2nd edn. Elsevier, pp 995–1045
Saeij JP, Boyle JP, Coller S, Taylor S, Sibley LD, Brooke-Powell ET, Ajioka JW, Boothroyd JC (2006) Polymorphic secreted kinases are key virulence factors in toxoplasmosis. Science 314:1780–1783
Salem ML, Kadima AN, Cole DJ, Gillanders WE (2005) Defining the antigen-specific T-cell response to vaccination and poly (I: C)/TLR3 signaling: evidence of enhanced primary and memory CD8 T-cell responses and antitumor immunity. J Immunother 28:220–228
Sayles PC, Gibson GW, Johnson LL (2000) B cells are essential for vaccination-induced resistance to virulent Toxoplasma gondii. Infect Immun 68:1026–1033
Selleck EM, Fentress SJ, Beatty WL, Degrandi D, Pfeffer K, Virgin HW 4th, Macmicking JD, Sibley LD (2013) Guanylate-binding protein 1 (Gbp1) contributes to cell-autonomous immunity against Toxoplasma gondii. PLoS Pathog 9, e1003320
Sheffield P, Garrard S, Derewenda Z (1999) Overcoming expression and purification problems of RhoGDI using a family of “parallel” expression vectors. Protein Expr Purif 15:34–39
Steinfeldt T, Könen-Waisman S, Tong L, Pawlowski N, Lamkemeyer T, Sibley LD, Hunn JP, Howard JC (2010) Phosphorylation of mouse immunity-related GTPase (IRG) resistance proteins is an evasion strategy for virulent Toxoplasma gondii. PLoS Biol 8, e1000576
Sturge CR, Yarovinsky F (2014) Complex immune cell interplay in the gamma interferon response during Toxoplasma gondii infection. Infect Immun 82:3090–3097
Sullivan WJ Jr, Smith AT, Joyce BR (2009) Understanding mechanisms and the role of differentiation in pathogenesis of Toxoplasma gondii: a review. Mem Inst Oswaldo Cruz 104:155–61
Suzuki Y, Orellana MA, Schreiber RD, Remington JS (1988) Interferon-gamma: the major mediator of resistance against Toxoplasma gondii. Science 240:516–518
Taylor S, Barragan A, Su C, Fux B, Fentress SJ, Tang K, Beatty WL, Hajj HE, Jerome M, Behnke MS, White M, Wootton JC, Sibley LD (2006) A secreted serine-threonine kinase determines virulence in the eukaryotic pathogen Toxoplasma gondii. Science 314:1776–1780
Tenter AM, Heckeroth AR, Weiss LM (2000) Toxoplasma gondii: from animals to humans. Int J Parasitol 30:1217–58
Vercammen M, Scorza T, Huygen K, De Braekeleer J, Diet R, Jacobs D, Saman E, Verschueren H (2000) DNA vaccination with genes encoding Toxoplasma gondii antigens GRA1, GRA7, and ROP2 induces partially protective immunity against lethal challenge in mice. Infect Immun 68:38–45
Verma R, Khanna P (2013) Development of Toxoplasma gondii vaccine: a global challenge. Hum Vaccin Immunother 9:291–293
Wilson EH, Wille-Reece U, Dzierszinski F, Hunter CA (2005) A critical role for IL-10 in limiting inflammation during toxoplasmic encephalitis. J Neuroimmunol 165:63–74
Yuan ZG, Zhang XX, Lin RQ, Petersen E, He S, Yu M, He XH, Zhou DH, He Y, Li HX, Liao M, Zhu XQ (2011) Protective effect against toxoplasmosis in mice induced by DNA immunization with gene encoding Toxoplasma gondii ROP18. Vaccine 29:6614–6619
Zhang NZ, Chen J, Wang M, Petersen E, Zhu XQ (2013) Vaccines against Toxoplasma gondii: new developments and perspectives. Expert Rev Vaccines 12:1287–1299
Zheng B, Lu S, Tong Q, Kong Q, Lou D (2013) The virulence-related rhoptry protein 5 (ROP5) of Toxoplasma gondii is a novel vaccine candidate against toxoplasmosis in mice. Vaccine 31:4578–84
Acknowledgments
This project was funded by the National Science Centre (Poland) on the basis of the decision DEC-2011/03/N/NZ6/04655.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grzybowski, M.M., Dziadek, B., Gatkowska, J.M. et al. Towards vaccine against toxoplasmosis: evaluation of the immunogenic and protective activity of recombinant ROP5 and ROP18 Toxoplasma gondii proteins. Parasitol Res 114, 4553–4563 (2015). https://doi.org/10.1007/s00436-015-4701-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-015-4701-y