Abstract
Purpose
The use of complementary and alternative medicine (CAM) is common among breast cancer patients, but less is known about whether CAM influences breast cancer survival. The primary aim of this study was to determine the impact of self-use of herbs on the overall survival.
Methods
This was a prospective study including 110 patients with breast cancer. All patients were questioned about the concept of taking herbs. We analyzed the demographic data and the overall survival.
Results
The average age was 51 years (30–80 years old). 37 had metastatic disease (33.6%). 48 patients had taken plants (43.6%). 19 patients consumed Graviola (39.6%) and 29 Alenda (60.4%). Overall survival at 3 years and at 5 years were, respectively, 96.2% and 82.4% in the absence of plant consumption versus 78.5% and 78.5% in case of plant consumption (p = 0.015).
Conclusion
This study concluded that self-medication with Graviola or Alenda may be associated with an increase of death risk in patients with breast cancer. Further studies are needed to confirm these results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer in Tunisian women. In 2020, 3092 new cases were diagnosed, which represents 34.5% of registered cancers in women according to the data of Globocan 2020. It is the most fatal cancer in women with a mortality of 8.3%. Its treatment is based on surgery, chemotherapy, radiotherapy, hormone therapy, and targeted therapies.
The use of complementary and alternative medicine (CAM) has been increasing worldwide (DiGianni et al. 2002) over the past two decades. Several reports have described patterns of CAM use among breast cancer patients (Matthews et al. 2007; Pedersen et al. 2009).
Complementary health approaches can be divided into several main categories as, for example, natural products (such as herbs), mind and body practices (including yoga, meditation, massage, acupuncture, etc.) and so-called holistic approaches (e.g., Traditional Chinese medicine, homeopathy, Ayurvedic medicine, etc.) (NCCIH 2016).
According to Firkins et al., there was a risk of interactions between a biological CAM method and conventional drugs in 54.9% of the patients using CAM (Firkins et al. 2018). Few data exist on the impact of CAM on the breast cancer survival. This is an important gap in the literature given the high prevalence of use and the strong belief by many patients that CAM improves their health. A longitudinal study attempting to measure the pattern of CAM use and its impact on survival in a heterogeneous cancer patient cohort from northern Norway was reported in 1998 (Risberg et al. 1998). There was no difference in overall survival between the 2 groups. In 2003, Risberg et al. concluded that the use of CAM seems to predict a shorter survival from cancer (Risberg et al. 2003). In contrary, CAM use was not associated with breast cancer-specific mortality or total mortality in the study of Neuhouser et al. (Neuhouser et al. 2016). Another study showed that the combination of hyperthermia from 1 to 2 times a week with Gun-Chil-Jung treatment may improve survival of cancer patients treated or being treated with conventional cancer therapies (Jun et al. 2020). Therefore, it is important to remember this field of self-medication around the world and in different cultures.
In our institution, we noticed an increase in the use of plants by cancer patients. Furthermore, we detected liver toxicity even before chemotherapy and outside of liver metastases. For this, we decided to conduct this study with the main objective of studying the impact of self-plant consumption on overall survival. The secondary objective was to determine the prevalence and side effects of plant self- medication.
Methods
Study design and participant
This was a prospective study including 110 patients with breast cancer questioned between July 15, 2018 and January 15, 2019. This was a consecutive cohort of all patients during this defined period. We used a standardized questionnaire developed by experts of the working group Prevention and Integrative Oncology of the German Cancer Society which has been published before (Huebner et al. 2014a, b). The questionnaire consisted of three main sections: *Demographic data, data on the tumor and the date of diagnosis. *Patient’s lifestyle *Use of CAM and most common CAM methods. Data were collected directly from patients, but also from medical records. Furthermore, we looked for side effects. Its analysis was guided by data derived from the website of the Memorial Sloan Kettering Cancer Center “about herbs” (“Integrative Medicine: Search About Herbs|Memorial Sloan Kettering Cancer Center” 2018), the compendium of Cassileth on herb-drug interactions (Cassileth and Lucarelli 2003) and the database DrugDigest (“Drug Information—Express Scripts®” 2018). Then, we prospectively follow-up patients, and we recorded overall survival. We had included in our study patients who have been followed for histologically proven breast cancer and who are undergoing adjuvant or palliative cancer treatment (chemotherapy or targeted therapy), over the age of 18, able to answer the questions and who agreed to participate in the study.
We had excluded from this study patients who do not have breast cancer, those under 18 years old, patients under homeopathy or acupuncture to avoid interactions, those with backwardness or major cognitive impairment and patients who refused to participate in the study. All procedures performed in this study studies were in accordance with the ethical standards of the institutional and the national research committee of Habib Bourguiba and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statistical study
The study of the associations between the variables was made by the hypothesis tests. The comparison of proportions was made by Pearson’s “chi2 (χ2)” test (when the theoretical size is greater than 5) or by the “Fisher (F)” exact test (when one of the theoretical numbers is less than 5) for independent samples. The correlation between side effects and plant consumption was calculated by chi2 (χ2) test. A logistic regression was performed to determine the factors associated with the consumption of medicinal plants (variables considered as qualitative), while taking into account confounding factors. We used Wald’s top-down method. The results were expressed as Adjusted Hazard Ratio (aHR) with 95% confidence intervals (95% CI). The difference is considered significant if p < 5%.
The Kaplan–Meier method allowed us to obtain survival curves and to compare them. Overall survival (OS) was calculated from the date of diagnosis to the date of the latest news or the occurrence of death (whatever the cause). The date of the latest news was 01/06/2020. The comparison of the curves was done by the Log Rank test. A difference is statistically significant if p is less than 0.05.
Results
Patients’ characteristics
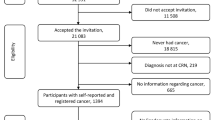
115 patients were assessed for eligibility. 5 patients were excluded and 110 patients were questioned (Fig. 1). The average age was 51 years with extremes ranging from 30 to 80 years. The origin of the patients was urban in 50.9% of cases, and rural in 49.1% of cases. The patient’s status and stage of breast cancer are summarized in Table 1. In our series, 52 patients were illiterate (47.3%) (Table 1). 72 patients underwent chemotherapy (65.4%), 19 chemotherapy and Trastuzumab (17.2%) and 19 Trastuzumab alone (17.2%). There is no patient who refuse specific anti-cancer treatment. There is no patient who stopped anti-cancer treatment.
Fourty-eight patients (43.6%) reported plant consumption. Both groups (plant-users and no-users) are comparable regarding the status and stage of the cancer disease. The consumer patients’ knowledge of these plants was mainly made by those around them (83.3% of cases) and then by internet (16.7% of cases). The majority of patients (58.1%) consumed these plants before and during systemic therapy.
The consumption of these plants was before systemic treatment in 15 cases (31.2%) with an average period of 20 days (1–30 days), during cancer treatment in 20 cases (41.6%) and before (1–30 days) and during cancer treatment in 13 cases (27%). 19 patients consumed Graviola (39.6%) and 29 Alenda (60.4%). There is no case of other plant consumption. The average duration of consumption was 6 months with extremes ranging from 1 to 36 months. These plants were in capsule form in 15 cases, fruit in 4 cases and broth in 29 cases.
We performed univariate analysis of plant consumption by age, marital status, educational level, urban or rural origin, treatment and stage of disease. Significant factors related to plant consumption were rural origin and metastatic stage with p = 0.013 and 0.04, respectively (Table 2). The geographical origin was significantly related to Alenda consumption (χ2 = 9.035, ddl = 1, α = 0.05, p = 0.004) with 22 patients with a rural origin versus 14 with urban origin. In multivariate analysis, only rural origin significantly influenced plant consumption (p = 0.01).
The side effects identified during the consumption of these plants were diarrhea in 5 cases (10.4%), hypertension in 7 cases (14.5%), hepatic cytolysis in 5 cases (10.4%), cholestasis in 6 cases (12.5%), thrombocytosis in 7 cases (14.5%), leukocytosis in 8 cases (16.6%), hypertension in 7 cases (14.5%) and anemia in 6 cases (12.5%).
Significant plant-correlated toxicities were diarrhea, hypertension and leukocytosis (p = 0.039, 0.002 and 0.001, respectively) (Table 3).
Overall survival
The overall mean survival was 96 months. Overall survival at 3 years and 5 years were 87.1% and 87.1%, respectively. Overall survival at 3 years and at 5 years were respectively 96.2% and 82.4% in the absence of plant consumption versus 78.5% and 78.5% in the case of plant consumption (Fig. 2) with p = 0.015. Factors significantly influencing overall survival were: plant consumption (p = 0.015) and metastatic stage (p = 0.01) (Table 4).
Discussion
Our population was characterized by the use of Alenda or Graviola in 43.6%. There is no case of other plant consumption. In fact, Tunisian cancer patients think that Graviola or Alenda may treat cancer or may potentialize the action of specific anti-cancer treatment. They used herbs-independently from education and social status. Our principal finding was the statistically significant decrease of OS in case of plant consumption. The use of complementary medicine in cancer patients ranges from 7% to more than 95%, depending on the studies and countries (Chabosseau and Derbré 2016; John et al. 2016). According to data of the literature, patients often use CAM in the hope that it will lead to tumor growth suppression and cure (Frenkel et al. 2010). This heterogeneity of prevalence can be explained by different methodologies, differences in the definition of CM and the use of non-standardized questionnaires. The most used types of CAM were homeopathy, dietary supplements, herbal medicine and acupuncture in literature. The use of medicinal plants, especially Graviola, ranges from 0.01% to 67% (Ernst and Cassileth 1998). There are no data on the frequency of consumption of Alenda. The correlated factors with plant intake in our series were the rural origin and metastatic stage with p = 0.013 and 0.04, respectively. In multivariate analysis, only the rural origin significantly influenced the consumption of plants (p = 0.01). In the Johnson et al. study published in 2018, the factors correlated with plant consumption were the type of cancer (mammary, pulmonary and colorectal versus prostate) and the advanced stage (Johnson et al. 2018). The geographical origin was significantly related to Alenda consumption (χ2 = 9.035, ddl = 1, α = 0.05, p = 0.004). This can be explained by the availability of Alenda in the Tunisian Sahara. According to literature data, Graviola may be responsible for hypotensive, vasodilatory and cardiodepressant activities in animals. No case of hypotension was observed in our study. A study in rats receiving Graviola revealed an increase in dopamine, norepinephrine and Monomine oxidase activity, as well as serotonin release inhibition in stress-induced rats (Woo et al. 1999; Peters et al. 2005). Alenda can cause tachycardia, hypertension, sweating, bronchodilatation, agitation and mydriasis. The use of Alenda (Ephedra) is also known to be associated with gastrointestinal and psychiatric manifestations (Chen et al. 2010; Caveny et al. 2001). Therefore, Ephedra is contraindicated for long-term use (Danciu et al. 2018). In our cohort, significant plant-correlated toxicities were diarrhea, hypertension and leukocytosis (p = 0.039, 0.002 and 0.001, respectively). Plant consumption may increase diarrhea caused by chemotherapy. In fact, there are documented interactions between some herbal medicines and other conventional medicines (Werneke et al. 2004), and those taking prescribed medication for other co-morbidities may experience harmful interactions when using herbal medicines.
In our series, the 5-year-survival was 82.4% in the absence of plant consumption versus 78.5% in the case of plant consumption. (p = 0.015). In the Johnson et al. study, the 5 year overall survival was 82.2% for CM (95% CI 76.0% to 87.0%) vs. 86.6% in the absence of CM (95% CI 84.0% to 88.9%), p = 0.001; hazard (HR) 1.70; 95% CI 1.24–2.34 compared to CM. MC consumption was associated with a higher risk of death (HR 2.08, 95% CI 1.50–2.90). The results suggest that the risk of death associated with CAM was mediated by the refusal of allotherapy (Johnson et al. 2018). Furthermore, in the study of Ma et al. herbal remedy use was associated with poorer survival and a poorer physical component score for health-related QOL among women who have survived breast cancer for at least 10 years. (Ma et al. 2011).
In our series, patients consuming Graviola or Alenda did not refuse treatment and there was no significant difference according to the timing of plant consumption. However, metastatic stage was a significant factor related to plant consumption, which may explain the decrease of overall survival.
Shorter survival among CAM users might be explained by the patients’ correct perception of the gravity of their disease. Indeed, patients may estimate the gravity of their situation more accurately than their physicians. This might explain why, after adjusting for disease-specific parameters, users of CAM expressed less hope and more mental distress, and in the end might have a shorter survival than non-users. Furthermore, one important reason for lower survival might be interaction between CAM and conventional treatment.
This study also has limitations. First, the nonrandomized study design made it is difficult to draw firm conclusions from the findings. Second, the size sample is small. Third, while we obtained data on self-reported use of natural products, it is not possible to collect dosage information due to the lack of uniformity. Furthermore, the method to collect data on CAM might have influenced the result as women may not have disclosed CAM usage. Further randomized studies are needed to confirm these results.
References
Cassileth BR, Lucarelli CD (2003) Herb–drug interactions in oncology. BC Decker Inc, Hamilton
Caveny S, Charlet D, Freitqg H, Maier-Stolete M, Starratt A (2001) New observations on the secondarychemistry of world Ephedra (Ephedraceae). Am J Botan 88:1199–1208
Chabosseau S, Derbré S (2016) Cancer du sein: recommandations sur l’usage de la phytothérapie. Actual Pharm 55(552):45–49
Chen W, Tsai T, Yang C, Kuo T (2010) Effects of ephedra on autonomicnervous modulation in healthy young adults. J Ethnopharmacol 130:563–568
Complementary, alternative, or integrative health: what’s in a name? | NCCIH (2016) National center for complementary and integrative health. https://nccih.nih.gov/health/integrative-health. Accessed 30 Nov 2017
Danciu C, Muntean D, Alexa E, Farcas C, Oprean C, Zupko I et al (2018) Phytochemical characterization and evaluation of the antimicrobial, antiproliferative and pro-apoptotic potential of ephedra alata decne. Hydroalcoholic extractagainst the MCF-7 breast cancer cell line. Molecules 1:20–24
DiGianni LM, Garber J, Winer EP (2002) Complementary and alternative medicine use among women with breast cancer. J Clin Oncol 20:34S-48S
Drug information—express scripts ® (2018) https://www.expressscripts. com/medco/consumer/ehealth/druginfo/dlmain. jsp?WC=N. Accessed 5 Jan 2018
Ernst E, Cassileth BR (1998) The prevalence of complementary/alternative medicine in cancer: a systematic review. Cancer 83:777–782
Firkins R, Eisfeld H, Keinki C, Buentzel J, Hochhaus A, Schmidt T et al (2018) The use of complementary and alternative medicine by patients in routine care and the risk of interactions. J Cancer Res Clin Oncol 144(3):551–557
Frenkel M, Ben-Arye E, Cohen L (2010) Communication in cancer care: discussing complementary and alternative medicine. Integr Cancer Ther 9:177–185
Huebner J, Muenstedt K, Prott FJ, Stoll C, Micke O, Buentzel J et al (2014a) Online survey of patients with breast cancer on complementary and alternative medicine. Breast Care (Basel Switzerland) 9(1):60–63
Huebner J, Micke O, Muecke R, Buentzel J, Prott FJ, Kleeberg U et al (2014b) User rate of complementary and alternative medicine (CAM) of patients visiting a counseling facility for CAM of a German comprehensive cancer center. Anticancer Res 34(2):943–948
Integrative medicine: search about herbs | Memorial Sloan Kettering Cancer Center (2018) https://www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine/herbs/search. Accessed 5 Jan 2018
John G, Hershman D, Falci L et al (2016) Complementary and alternative medicine use among US cancer survivors. J Cancer Surviv 10:850–864
Johnson S, Park H, Gross C, Yu J (2018) Complementary medicine, refusal of conventional cancer therapy, and survival among patients with curable cancers. JAMA Oncol 10:1375–1381
Jun HJ, Park SJ, Kang HJ, Lee GY, Lee N, Park JH et al (2020) The survival benefit of combination therapy with mild temperature hyperthermia and an herbal prescription of Gun-Chil-Jung in 54 cancer patients treated with chemotherapy or radiation therapy: a retrospective study. Integr Cancer Ther 19:1534735420926583
Ma H, Carpenter CL, Sullivan-Halley J, Bernstein L (2011) The roles of herbal remedies in survival and quality of life among long-term breast cancer survivors—results of a prospective study. BMC Cancer 6(11):222
Matthews AK, Sellergren SA, Huo D, List M, Fleming G (2007) Complementary and alternative medicine use among breast cancer survivors. J Altern Complement Med 13(5):555–562
Neuhouser ML, Smith AW, George SM et al (2016) Use of complementary and alternative medicine and breast cancer survival in the health, eating, activity, and lifestyle study. Breast Cancer Res Treat 160:539–546
Pedersen CG, Christensen S, Jensen AB, Zachariae R (2009) Prevalence, socio-demographic and clinical predictors of post-diagnostic utilisation of different types of complementary and alternative medicine (CAM) in a nationwide cohort of Danish women treated for primary breast cancer. Eur J Cancer 45(18):3172–3181
Peters C, O’neill J, Young J (2005) Is there an association between ephedra and heartfailure? a case series. J Cardiac Fail 11:9–11
Risberg T, Lund E, Wist E, Kaasa S, Wilsgaard T (1998) Cancer patients use of nonproven therapy: a 5 year follow-up study. J Clin Oncol 16:6–12
Risberg T, Vickers A, Bremnes RM, Wist EA, Kaasa S, Cassileth BR (2003) Does use of alternative medicine predict survival from cancer? Eur J Cancer 39:372–377
Werneke U, Ladenheim D, McCarthy T (2004) Complementary alternative medicine for cancer: a review of effectiveness and safety. Cancer Ther 2:475–500
Woo M, Chung S, Kim D (1999) Cis-annonacin and (2,4)-cis-and trans-isoannonacins: cytotoxic monotetrahydrofuran annonaceous acetogenins from the seeds of Annona cherimolia. Arch Pharm Res 5:524–528
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and the national research committee of Habib Bourguiba and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben Kridis, W., Mnif, A., Khmiri, S. et al. Self-medication with herbal medicine and breast cancer survival: a prospective monocentric study. J Cancer Res Clin Oncol 147, 3401–3407 (2021). https://doi.org/10.1007/s00432-021-03600-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03600-y