Abstract
Purpose
This study aimed to evaluate the clinical effects of percutaneous vertebroplasty (PVP) combined with postoperative radiotherapy (RT) in the treatment of spinal metastases.
Methods
Nine patients (4 males and 5 females, mean age 59.56 years) with painful pathologic compression vertebral fractures caused by metastatic cancers of the spine (5 thoracic levels, 8 lumbar levels) were admitted to our hospital between July 17, 2016 and September 25, 2018. All patients were treated with PVP via bilateral pedicle approach combined with postoperative RT to treat metastatic lesions of the centrum. The clinical records of the patients were retrospectively analyzed. Patients’ demographic features and medical conditions including the Visual Analogue Scale (VAS), Oswestry Disability Index (ODI) and Imageology data were observed.
Results
Patients’ mean VAS scores decreased from 8.67 ± 0.50 preoperatively to 1.78 ± 0.83 at 6 months after PVP. Moreover, the mean ODI score decreased from 74.07 ± 13.15 preoperatively to 31.87 ± 10.00 at 6 months after PVP. Significant improvement in the degree of pain and dysfunction among the enrolled patients were observed. Furthermore, the metastatic carcinoma lesion within the vertebral body was well controlled according to imaging.
Conclusion
PVP in conjunction with postoperative RT is a good treatment strategy for vertebral compression fractures caused by metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The vertebral column is the most vulnerable part for malignant metastatic tumor formation in the skeletal system. Malignant metastatic tumors often result in osteolytic lesions or pathological compression fractures of the vertebral body, frequently giving rise to syndromes encompassing spinal pain, mobility disorders and sensory disturbances (Bae et al. 2016; Georgy 2008). The quality of life (QOL) and survival time among patients with metastatic tumors are less. Patients with spinal metastases tend to have poorer sclerotin levels and weaker physical conditions, and they generally find difficulties in tolerating traditional open surgery (Zhang et al. 2016). Additionally, since spinal metastases usually occur in multiple segments, completely removing tumors often proves difficult (Zhang et al. 2017). Thus, the aim of clinical treatment is to focus on the retention of nerve function, palliate pain, restore spinal stability, and treat metastatic tumors via conservative treatment, such as steroids, chemotherapy, radiotherapy, PVP, radiofrequency ablation (Kam et al. 2017; Kobayashi et al. 2009; Li et al. 2015; Stephenson et al. 2016).
PVP has been widely used in the treatment of vertebral hemangioma, vertebral fractures and spinal metastases globally (Li et al. 2014). However, adjuvant radiotherapy was also used in the treatment of malignant tumors long ago. Radiotherapy has therapeutic efficacy in the treatment of single or multiple tumors, inhibiting tumor growth and delaying its progression. However, radiotherapy is ineffective to alleviate the destruction of bone caused by tumor infiltration and the resulting instability of the spine (Elnoamany 2016; Katsoulakis et al. 2017).
In our study, PVP combined with postoperative RT was used in the treatment of spinal metastases, which was found to make up for their respective shortcomings. Accordingly, this mode of therapy relieved the patients’ pain, demonstrating beneficial clinical outcomes in treatment.
Materials and methods
Patients
This retrospective study involved nine patients (including 4 males and 5 females with mean age of 59.56 years, ranging between 38 to 76 years) suffering from metastatic cancers of the spine who were admitted to our hospital between July 17, 2016 and September 25, 2018. All patients underwent plain radiography, computed tomography (CT) scanning and magnetic resonance imaging (MRI) in the preoperative and postoperative periods. Most underwent radionucleotide bone scanning of the spine, and all patients underwent pathological examinations for the excised vertebral body tissue to confirm the tumor type, and systematic examinations were conducted in order to diagnose the primary tumor. Primary tumors included three cases of breast cancer, two cases of prostate cancer, two cases of lung cancer, one case of thyroid cancer and one case of hepatocellular carcinoma (Table 1).
Patient inclusion criteria: (1) Patients having symptomatic vertebral fractures due to metastatic tumors; (2) Patients have clear consciousness, basic listening and speaking ability, and may physically tolerate PVP and radiotherapy; (3) Patients who received extracorporeal radiotherapy prior to PVP, but the treatment failed, resulting in tumor progression; (4) Patients who underwent conservative treatment which was found to be ineffective, resulting in tumor progression or serious adverse reactions, making them unable to continue conservative treatment. Patient exclusion criteria: (1) Patients with impaired consciousness and those who could not physically tolerate PVP and radiotherapy; (2) Patients who had conservative treatment, where symptoms were significantly improved; (3) Patients having a stable vertebral fracture with no obvious metastatic symptoms; 4) Patients having blood coagulation disorders, osteomyelitis of a diseased vertebral body or have no clear correlation between their symptoms and loss of vertebral height.
Before PVP, 5 patients received subcutaneous injection of morphine, and 4 patients received oral morphine hydrochloride tablets to relieve pain. However, the effect of pain relief is still poor.With the progress of PVP, the grade and dose of painkillers in all patients decreased significantly. Each patient just needs received intramuscular injection of Dezocine or oral administration of Meloxicam for analgesia after operation, the consumption changes of analgesic before and after PVP is shown in Table 2.
Before this study was conducted, the project was approved by the Independent Ethics Committee at our hospital. The informed consent form was signed with the consent of the patients and their family members.
Treatment strategy
Treatment of PVP
The patients were initially placed in the prone position, and routine sterilization was done. A C-arm machine was used to locate the projection of the vertebral pedicle on the body surface at the responsible vertebral body. After local anesthesia, two incisions with lengths of 3–5 mm were made 1–2 cm next to the surface projection area of the pedicle.
With the guidance of the C-arm X-ray machine, a puncture needle was placed into the appropriate position at the responsible vertebral body through the bilateral pedicle. Specifically, in the lateral image, the tip of the needle reached the anterior midline of the vertebral body. In the positive position, the tip of the upper needle did not pass the midline in the image. During operation, bone tissue was collected via puncture needle and sent for pathological examination. Polymethyl methacrylate (PMMA) bone cement was then injected slowly, and the puncture needle was removed until the bone cement solidified. Afterward, the skin incision was covered with sterile gauze, which ended the operation. All PVP operations were performed in 30–60 min. Antibiotics were routinely administered intravenously 3 days after operation to prevent infection.
Radiotherapy following PVP
Extracorporeal radiotherapy was conducted about 1 week after PVP for each patient. All patients recovered well before radiotherapy. Accordingly, patients adopted the lateral recumbent position, and the diseased vertebral body was accurately located by MRI or CT imaging. This determined the scope and depth of the metastatic tumor and considered the diseased vertebral body as the center, with or without the upper and lower vertebrae. After the patient was fixed, the α, β, γ rays or the X-rays, electron rays and proton beams produced by the accelerator were utilized to irradiate the tumor in vitro with a single field in the same center or multiple fields in the same center. The total radiation dose was maintained at 40-45 Gy, which was administered 5–6 times per week for a total of 10 times continuously for 2 weeks. During radiotherapy, the skin of the irradiated site should be kept clean to actively prevent skin infection and necrosis. Because the immune function of tumor patients is lower than that of normal people, and radiotherapy will inhibit the immune function of tumor patients, it is necessary to monitor hemato-immunological status of tumor patients before and after radiotherapy in order to intervene when the patients are extremely low (Table 3).
Assessment indices
The visual analogue scale (VAS) was used to rate the patient’s pain according to the previously described standard procedure. The VAS score criteria are as follows: 0 indicates no pain, while 10 indicates the most severe pain. Evaluation time was before operation, the first day, 1 week, 1 month and 3 months after operation, as well as the final follow-up.
The Oswestry Disability Index (ODI) questionnaire was used to evaluate the functional status of patients. ODI questionnaire is an effective measure of health outcomes, which has been widely used in spinal surgery. It comprehensively evaluates the functional status of patients in all aspects. The higher the ODI score, the more severe the dysfunction. The evaluation time was before operation, the first day, 1 week, 1 month and 3 months after operation, as well as the final follow-up.
Statistical analysis
Statistical analysis was performed using SPSS 23.0 software (SPSS Inc., IBM, Chicago, IL). Values were given as mean ± standard deviation. A P value < 0.05 was considered to be statistically significant.
The difference in VAS scores between the pre-operation and post-operation periods were compared using the rank sum test. Moreover, the differences in ODI between the pre-operation and post-operation periods were compared using a single factor analysis of variance (ANOVA).
Results
All nine patients were successfully treated with PVP in conjunction with postoperative RT. The average VAS scores of the enrolled patients decreased from 8.67 ± 0.50 before PVP to 2.22 ± 0.67 on the first day, 1.78 ± 0.67 at 1 week, 1.68 ± 0.70 at 1 month, and 1.56 ± 0.73 at 3 months after PVP, as well as 1.78 ± 0.83 at 6 months after PVP. A significant difference between the average VAS scores at each time point after PVP and the baseline score before PVP (p < 0.05, Fig. 1) was evident.
Visual analog scale (VAS) change of patients of at each pre- and postoperative follow-up time. Data are expressed as mean ± standard deviation. The differences between the VAS scores prior to PVP and at 1 day, 1 week, and 1, 3 and 6 months, respectively, are statistically significant (p < 0.05). Pre-, preoperative; PVP, percutaneous vertebroplasty
Similar results were observed among patients in terms of ODI score (Fig. 2). The average ODI score decreased from 74.07 ± 13.15 before PVP to 37.36 ± 5.92 on the first day, 34.89 ± 5.28 at 1 week, 31.04 ± 6.64 at 1 month, and 32.78 ± 7.91 at 3 months after PVP, as well as 31.87 ± 10.00 at 6 months after PVP. A significant difference was observed between the average ODI score at each time point after PVP and the baseline score before operation (p < 0.05).
Oswestry disability index (ODI) scores change of patients of at each pre- and postoperative follow-up time. Data are expressed as mean ± standard deviation. The differences between the ODI scores prior to PVP and at 1 day, 1 week, and 1, 3 and 6 months, respectively, are statistically significant (p < 0.05). Pre preoperative, PVP percutaneous vertebroplasty
Typical case
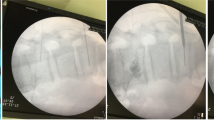
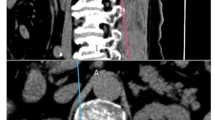
A 55-year-old male patient underwent lobectomy outside our hospital for lung cancer in August 2016. Since December 2016, the patient developed lower back pain, for which an MRI showed L3 vertebral metastatic cancer (Fig. 3a, b). After completing two cycles of radiotherapy, his symptoms were not significantly relieved and were gradually aggravated. Moreover, neurological symptoms, such as progressive bilateral limbs numbness and muscle weakness of the both lower extremities, started to appear. On Feb. 9, 2017, an MRI showed significant tumor progression, where a pathological compression fracture was observed in the L3 vertebra. The tumor protruded into the spinal canal and compressed the spinal cord (Fig. 4a–c). At that time, the VAS score of the patient was 9 points, and his muscle strength of both lower limbs were at level 2, The numbness of both lower limbs is aggravated, and the low back pain worsened obviously during exercise, so that he could not walk. According to the symptoms of the patients and the results of imaging examination, we believed that the symptoms of the patients are mainly caused by spinal instability and nerve stimulation by tumor tissue. Accordingly, we developed a treatment plan employing PVP combined with postoperative radiotherapy,which can improve the vertebral stability, calcify tumor tissue, control tumor progression, and reduce the symptoms of nerve stimulation. On the first day following PVP, the patient’s VAS score reduced to 5, The numbness of both lower limbs has been improved. Postoperative imaging demonstrated that PMMA bone cement was uniformly dispersed in the diseased vertebral body, and the partial height of the diseased vertebral body was restored(Fig. 7a, b). Furthermore, the stability of the vertebral body was found to be significantly improved. Vertebral tumor immunohistochemistry also confirmed that the tumor originated from small cell lung cancer (SCLC) (Fig. 5a–c). One week following PVP, extracorporeal radiotherapy was performed, where the total radiotherapy dose given was 40-45 Gy, which was administered 5-6 times per week for 10 times over two weeks. After postoperative RT, regular CT scanning and follow-ups(1 week, 1 months, 3 months, 6 months, 1 year, 1.5 year, 2 years)were carried out in order to observe the efficacy of PVP with postoperative RT. Three months after radiotherapy, most of the numbness of both lower limbs disappeared and the muscle strength of right lower limb recovered to level 4, and the left lower limb recovered to level 5, so that he can walk again. After his one-year follow-up, the patient’s lower back pain and bilateral lower limb numbness were completely relieved, and his VAS score dropped to 0 with satisfactory clinical outcomes. CT scan imaging prior to RT was compared to that of his last follow-up, which illustrated that the tumor lesion was significantly reduced, and the surrounding area of the tumor was obviously calcified (Fig. 6a, b vs Fig. 6c, d). However, the patient developed brain metastasis 1.5 years after operation and died of brain metastasis two years later.
Preoperative imaging examination. Preoperative Lumbar MRI showing an obvious metastasis of third lumbar vertebra body and the tumor has compressed the same level spinal canal(A&B). Preoperative CT scan showing an obvious metastasis of Third lumbar vertebra body at the horizontal plane, and the tumor have invaded the spinal cord(C).(the arrow points to the tumor site.)
HE stain of lumbar tumor tissue showed an extensive distribution of adenocarcinoma cells ,magnify 200 times (a). Immunohistochemistry of lumbar tumor tissue showed the positive expression of Keratin, Keratin(+) (b). Immunohistochemistry of lumbar tumor tissue showed the positive expression of Carcino-Embryonic antigen CEA(+) (c).All above reports confirmed that the vertebral tumor originated from the Small Cell Lung Cancer(SCLC)
CT scans before postoperative radiotherapy showed that the PMMA bone cement was properly filled in the affected third lumbar vertebra body (a, b). After postoperative radiotherapy reexamination of CT scans showed that a high-quality calcification in the Third lumbar vertebra body and tumor Lesions were evidently reduced (c, d). (the arrow points to the tumor site.)
Discussion
Spinal metastases often lead to severe back pain and destruction of the vertebral body, causing mechanical instability and neurological dysfunction (Yin et al. 2004). About 30% of patients with cancer develop symptomatic spinal metastases during the course of the disease, with pain being the chief complaint (Fourney et al. 2003; Stephenson et al. 2016). A central modality in the treatment of spinal metastasis is to relieve pain, inhibit the further growth of the tumor and restore the strength of the vertebral body over time. Many patients find it difficult to accept traditional open surgery due to its disadvantages in short survival time or due to the patients’ poor physiques. Radiotherapy, chemotherapy and minimally invasive surgery are more easily accepted, however. PVP has advantages in that it involves less trauma, is relatively simple, relieves pain, and restores the height of the vertebral body while increasing its strength. In this study, symptoms of lower back pain in all patients were significantly relieved following PVP. Moreover, their average VAS scores decreased from 8.44 ± 0.72 before PVP to 2.22 ± 0.67 on the first day after PVP, which was found to be statistically significant (p < 0.05). Accordingly, the improvement in pain as assessed by VAS scores was found to be roughly the same as that of Han et al. (2019), Cortet et al. (1997), and Zhang et al. (2016). Here, all patients underwent in vitro radiotherapy about 1 week following PVP surgery. Compared to the CT scan results of patients before PVP and 1 week after PVP, the anterior, middle and posterior height of involved vertebral bodies of the patients were recovered to a certain extent (Table 4, p < 0.05), which was consistent with the basic results of previous studies.(Hiwatashi et al. 2003, 2009; Shengzhong et al. 2012; Sun et al. 2020).
And compared to the CT scan results of patients before radiotherapy and at their last follow-up, metastatic tumors of the spine in all patients were found to be under adequate local control. Tumors within the vertebral bodies shrank, and the tumor margins were significantly calcified. The improvement of the patients’ ODI scores were observed to be similar, with statistically significant differences present between the average ODI score at each postoperative period and preoperative baseline score (p < 0.05).
However, various tumors remain insensitive to radiotherapy, making them unable to achieve local control and continue to develop following radiotherapy alone, which leads to pathological fractures of vertebral body as well as related neurological symptoms. The prognosis in such patients is often poor, and no definite treatment for spinal metastasis in this type of tumor exists. (Gong et al. 2019; Joaquim et al. 2013; Sahgal et al. 2011). The typical case as presented in this study is Similar to the above case. The patient was diagnosed with small cell lung cancer and suffered spinal metastasis after lobectomy, which was followed up by external radiotherapy for a period of time. However, his spinal metastatic cancer was not locally controlled; it progressed along with the rise of pain and associated neurological symptoms. However, the patient was treated with extracorporeal radiotherapy again after PVP and followed up regularly thereafter. The spinal metastatic tumor in this patient was found to be well controlled locally in that the tumor shrank and the surrounding area of the tumor was clearly calcified (Fig. 6c, d), indicating its potential use for curative PVP combined with RT for such patients. Taking into account the results of previous studies, this investigation suggests the following reasons in view of the improved clinical outcomes among patients suffering from spinal metastases insensitive to radiotherapy who were given PVP combined with postoperative RT: (1) The polymerization of PMMA bone cement injected during PVP can release a large amount of heat, which is higher than the temperature threshold of heat-labile tumor cells, promoting tumor cells to be thermally necrotic (Hu et al. 2018); (2) After the injection of bone cement, because of its fluidity, it may be able to surround the tumor cells and oppress the blood vessels in the vertebral body, interrupting vascular supply, hypoxia and nutrition for tumor cells in the lesion area and accelerating the necrosis of tumor cells (Hu et al. 2018); (3) The radiation involved produces an interfacing effect at the border between the tumor and bone cement, which increases the dose of radiation and enhances the killing effect of radiation on the tumor (Alghamdi et al. 2017; Wang et al. 2013). And Usually, the immune function of tumor patients is relatively low, and radiotherapy will further inhibit the immune function, but the immune function of 9 patients in this study didn’t decrease significantly. We think that it may be due to the obvious relief of pain in patients after PVP, and early ground exercise after operation is helpful to the recovery of immune function of patients.
Therefore, PVP combined with postoperative RT is suggested to be an effective treatment for spinal metastatic cancer. Its mechanism should be further investigation, especially in spinal metastatic cancer insensitive to sole radiotherapy. However, the conclusions of this study possess certain limitations. First, this study is a retrospective analysis. Although the symptoms of the patients were significantly improved, and the prognosis was shown to be favorable following PVP with RT, the sample size was only nine patients, which was too small to eliminate the influence of other factors. In the future, a larger study should verify the safety and efficacy of PVP combined with RT, especially in those with spinal metastatic cancer insensitive to single radiotherapy. Second, though this study offers comparisons to previous research, it may lack thoroughness, which may result in the conclusions not being particularly convincing. Further investigations are required to ascertain definitive answers.
Conclusion
PVP in conjunction with postoperative RT is a good treatment strategy for vertebral compression fractures caused by metastases.
References
Alghamdi M et al (2017) Postoperative stereotactic body radiotherapy for spinal metastases. Chin Clin Oncol 6:S18. https://doi.org/10.21037/cco.2017.06.27
Bae JW, Gwak H-S, Kim S, Joo J, Shin SH, Yoo H, Lee SH (2016) Percutaneous vertebroplasty for patients with metastatic compression fractures of the thoracolumbar spine: clinical and radiological factors affecting functional outcomes. Spine J 16:355–364. https://doi.org/10.1016/j.spinee.2015.11.033
Cortet B et al (1997) Percutaneous vertebroplasty in patients with osteolytic metastases or multiple myeloma. Rev Rhum Engl Ed 64:177–183
Elnoamany H (2016) Percutaneous selective vertebroplasty: state of the art management in well-confined metastatic vertebral lesions Asian. Spine J 10:869–876. https://doi.org/10.4184/asj.2016.10.5.869
Fourney DR et al (2003) Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg 98:21–30. https://doi.org/10.3171/spi.2003.98.1.0021
Georgy BA (2008) Metastatic spinal lesions: state-of-the-art treatment options and future trends. AJNR Am J Neuroradiol 29:1605–1611. https://doi.org/10.3174/ajnr.A1137
Gong Y et al (2019) Efficacy and safety of different fractions in stereotactic body radiotherapy for spinal metastases: a systematic review. Cancer Med 8:6176–6184. https://doi.org/10.1002/cam4.2546
Han XX, Tao F, Wang GW, Li LL, Zhang C, Ren ZW, Ma YL (2019) Effect of combined treatment including surgery and postoperative adjuvant therapy on spinal metastases of Tomita type 7. Clin Neurol Neurosurg 181:112–118. https://doi.org/10.1016/j.clineuro.2019.04.007
Hiwatashi A, Moritani T, Numaguchi Y, Westesson PL (2003) Increase in vertebral body height after vertebroplasty AJNR. Am J Neuroradiol 24:185–189
Hiwatashi A et al (2009) Kyphoplasty and vertebroplasty produce the same degree of height restoration. AJNR Am J Neuroradiol 30:669–673. https://doi.org/10.3174/ajnr.A1442
Hu KZ, Chen SC, Xu L (2018) Comparison of percutaneous balloon dilation kyphoplasty and percutaneous vertebroplasty in treatment for thoracolumbar vertebral compression fractures. Eur Rev Med Pharmacol Sci 22:96–102. https://doi.org/10.26355/eurrev_201807_15370
Joaquim AF, Ghizoni E, Tedeschi H, Pereira EB, Giacomini LA (2013) Stereotactic radiosurgery for spinal metastases: a literature review. Einstein (Sao Paulo) 11:247–255. https://doi.org/10.1590/s1679-45082013000200020
Kam NM et al (2017) Combined vertebral augmentation and radiofrequency ablation in the management of spinal metastases: an update. Curr Treat Opt Oncol. https://doi.org/10.1007/s11864-017-0516-7
Katsoulakis E, Laufer I, Bilsky M, Agaram NP, Lovelock M, Yamada Y (2017) Pathological characteristics of spine metastases treated with high-dose single-fraction stereotactic radiosurgery. Neurosurg Focus 42:E7. https://doi.org/10.3171/2016.10.FOCUS16368
Kobayashi T et al (2009) Phase I/II clinical study of percutaneous vertebroplasty (PVP) as palliation for painful malignant vertebral compression fractures (PMVCF): JIVROSG-0202. Ann Oncol 20:1943–1947. https://doi.org/10.1093/annonc/mdp242
Li Z, Ni C, Chen L, Sun Z, Yang C, Zhao X, Wang Y (2014) Kyphoplasty versus vertebroplasty for the treatment of malignant vertebral compression fractures caused by metastases: a retrospective study. Chin Med J (Engl) 127:1493-1496 https://insights.ovid.com/pubmed?pmid=24762595
Li Y, Qing Y, Zhang Z, Li M, Xie J, Wang G, Wang D (2015) Clinical efficacy of percutaneous vertebroplasty combined with intensity-modulated radiotherapy for spinal metastases in patients with NSCLC. Onco Targets Ther 8:2139–2145. https://doi.org/10.2147/OTT.S86270
Sahgal A et al (2011) Stereotactic body radiotherapy for spinal metastases: current status, with a focus on its application in the postoperative patient. J Neurosurg Spine 14:151–166. https://doi.org/10.3171/2010.9.SPINE091005
Shengzhong M, Dongjin W, Shiqing W, Yang S, Peng R, Wanli M, Chunzheng G (2012) Modification of percutaneous vertebroplasty for painful old osteoporotic vertebral compression fracture in the elderly: preliminary report. Injury 43:486–489. https://doi.org/10.1016/j.injury.2011.12.021
Stephenson MB, Glaenzer B, Malamis A (2016) Percutaneous minimally invasive techniques in the treatment of spinal metastases. Curr Treatment Opt Oncol. https://doi.org/10.1007/s11864-016-0433-1
Sun X, Liu X, Wang J, Tao H, Zhu T, Jin W, Shen K (2020) The effect of early limited activity after bipedicular percutaneous vertebroplasty to treat acute painful steoporotic vertebral compression fractures. Pain Physician 23:E31–E40
Wang X et al (2013) Effect of spine hardware on small spinal stereotactic radiosurgery dosimetry. Phys Med Biol 58:6733–6747. https://doi.org/10.1088/0031-9155/58/19/6733
Yin FF et al (2004) Image-guided procedures for intensity-modulated spinal radiosurgery. Tech Note J Neurosurg 101(Suppl 3):419–424. https://doi.org/10.3171/jns.2004.101.supplement%203.0419
Zhang C, Wang G, Han X, Ren Z, Duo J (2016) Comparison of the therapeutic effects of surgery combined with postoperative radiotherapy and standalone radiotherapy in treating spinal metastases of lung cancer. Clin Neurol Neurosurg 141:38–42. https://doi.org/10.1016/j.clineuro.2015.12.011
Zhang HT, Chen GD, Yang HL, Luo ZP (2017) Percutaneous kyphoplasty in the treatment of osteoblastic-related spinal metastases. Clin Spine Surg 30:80–84. https://doi.org/10.1097/BSD.0b013e3182a35745
Acknowledgements
Thanks for Xiaobing Yu conceived and designed the study.
Funding
This work was not supported by any funding sources.
Author information
Authors and Affiliations
Contributions
XY conceived and designed the study. MQ, TL and RD collected the data. WH and Miaoman Lin analysed and interpretated the data.Miaoman Lin analyzed the statistical and wrote the paper. Yashuai Yuan,Junxiao Gao,Meng Zhang and Xiaobing Yu reviewed and edited the manuscript. Mingjia Qu played a very important role in the revision of the manuscript.All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, M., Qu, M., Huang, W. et al. Clinical effectiveness of percutaneous vertebroplasty in conjunction with postoperative radiotherapy in the treatment of spinal metastases. J Cancer Res Clin Oncol 147, 835–844 (2021). https://doi.org/10.1007/s00432-020-03371-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03371-y