Abstract
Background
Dedifferentiated liposarcoma (DDLPS) is a high-grade, clinically aggressive tumor associated with low survival probabilities. Prognostic variables for DDLPS have not been previously reported in a large patient population.
Methods
A total of 3573 patients with primary DDLPS were analyzed from the National Cancer Data Base (NCDB). The 5- and 10-year survival probabilities were calculated, and the groups were compared using log-rank comparisons and multivariable Cox hazard regression analysis. Median survival was also calculated.
Results
Males comprised 65% of the cohort, the median age at diagnosis was 64 years of age, and 65.4% of the patients were between 51 and 75 years of age. The most common site for primary tumors is the retroperitoneum or abdomen (59.5%). Head or neck tumors had the best 5-year outcomes (86.4%) followed by extremities (67.1%), pelvis (65.8%), thorax or trunk (58.9%), and finally retroperitoneum or abdomen (42.6%). Best outcomes were noted in the 26- to 50-year-old age group (5-year survival:66.8%), < 10 cm size (5-year survival:66.1%), FNCLCC grade 1 (5-year survival:69.2%), and stage II disease (5-year survival:66.7%). Radiation therapy yielded the best 5-year and 10-year survival probabilities of 59% and 39.3%, respectively. Out of all the adjuvant therapies, the use of radiation resulted in the best 5-year survival of 63.4%.
Conclusion
In the largest and most comprehensive study to date on DDLPS, major findings include primary site as a significant prognostic variable with age at presentation, sex, tumor stage, and type of adjuvant therapy significantly impacting overall survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liposarcomas represent approximately 20% of all soft tissue sarcomas (STS), making it one of the most common malignant STS (Engstrom et al. 2008). Liposarcomas have been previously noted to affect genders equally, most commonly presenting between the ages of 50 and 70 years and rarely present in children (Brennan et al. 2013). According to the World Health Organization, there are four separate types of liposarcoma based on histology: atypical lipomatous neoplasm/well differentiated, myxoid/round cell, pleomorphic, and dedifferentiated (Mangham 2004). For liposarcomas, most tumors occur in deep soft tissues, especially the extremities (Goldblum et al. 2014).
Dedifferentiated liposarcomas (DDLPS) represent 18% of all liposarcomas (Goldblum et al. 2014). DDLPS most commonly present in the retroperitoneum and peak incidence occurs in their seventies (Brennan et al. 2013; Goldblum et al. 2014). DDLPS typically have a high incidence of local recurrence (Goldblum et al. 2014). These tumors can form either de novo or from a preexisting well-defined liposarcoma (Brennan et al. 2013). Most patients present with high grades of dedifferentiation (Goldblum et al. 2014).
In a previous study of 155 patients, multivariate analysis showed that primary anatomical site was a significant variable for survival, with retroperitoneal tumors being the most lethal (Henricks et al. 1997). In that study, there were 106 cases of retroperitoneal DDPLS, 13 in the extremities, 13 in the spermatic cord, 11 in the trunk, and 1 case in the larynx. No median survival or 5- or 10-year survival probabilities were presented.
The goal of this study was to utilize the largest cancer database in the United States to compile the largest cohort and characterize the 5- and 10-year survival probabilities and median survival of different primary sites and other prognostic variables including age, tumor size, grade, tumor stage, and treatment options, including adjuvant therapy, to improve clinical outcomes.
Materials and methods
The National Cancer Database (NCDB) is a comprehensive oncology database for United States patients that was formed in 1989 by the American Cancer Society and Commission on Cancer (CoC) of the American College of Surgeons. This database contains approximately 70% of all patients in the United States diagnosed with cancer. Each of the authors was granted access to the NCDB through the Participant Use Data Files program established by the NCDB.
This study analyzed patients with DDLPS from 2004 to 2015 through CoC accredited cancer programs. A total of 3,573 patients were identified using the ICD-O-3 histology code 8858. Patients who only had only one malignant neoplasm diagnosis over their lifetime were included. Patients with multiple malignant tumor diagnoses were excluded since true survival data could be skewed if other cancers were present. This study analyzed demographic and tumor statistics including sex, age, year of diagnosis, tumor size, incidence and location of metastasis, primary site of tumor, Fédération Nationale des Centres de Lutte Contre le Cancer (FNCLCC) grade, tumor staging, treatment modalities and adjuvant therapies. This study utilized ICD-O-3 topography codes to identify primary anatomical sites.
Five- and ten-year survival probabilities and visualization of Kaplan–Meier survival curves were utilized for age, sex, primary anatomical site, tumor size, FNCLCC grade, tumor stage, treatment modalities, and adjuvant therapy. Age was analyzed by separating patients into four separate groups: 0–25 years old, 26–50 years old, 51–75 years old, and > 75 years old. Sex was classified as either male or female. Primary anatomical site of presentation was separated into five groups: head or neck, extremities, pelvis, thorax or trunk, and retroperitoneum or abdomen. Tumor size was divided into either < 10 cm or ≥ 10 cm and compared. FNCLCC tumor grades included three groups: grade 1, grade 2, and grade 3. We seperated patients by analytic stage at cancer diagnosis, a variable provided by the NCDB that reflects the American Joint Committee on Cancer (AJCC) pathologic staging. When analytic stage was unavailable, clinical staging was utilized. Sub-stage groups were collapsed into the stages I, II, III, or IV. Adjuvant therapy options were divided into four groups: surgery alone, radiation therapy after surgery, chemotherapy after surgery, and chemoradiation therapy after surgery. Median survival, 5- and 10-year survival probabilities for all variables were calculated in months from the time from diagnosis until either death or last known contact.
To calculate 5- and 10-year survival probabilities, survival tables and Kaplan–Meier curves were utilized. Specifically, survival tables were used to determine 5- and 10-year survival percentages. Multivariable Cox regression models were calculated to determine differences in risk of death associated with primary anatomical site and other factors after controlling for age, gender, race, analytic stage, treatment approach, type of treatment facility and socioeconomic variables including household income, educational background, and insurance status. The functional forms of continuous variables were investigated to examine the potential of higher ordered terms, and the proportionality of hazards assumption was checked with log-negative-log survival curves. Patients with any missing data were excluded from the analysis. All analyses were conducted with SAS version 9.4 (SAS Institute Inc., Cary, NC) and version 25 of SPSS, with a statistical threshold of p < 0.05.
Results
Table 1 shows background information of the cohort. Approximately 65% of the cohort were males, while females were 35%. This resulted in a 1.86 male to female ratio. The median age at diagnosis was 64 years. The ages of all patients are listed in Table 1, with the 51- to 75-year-old group being the most prevalent with 2,335 patients (65.4%), while the 0–25-year age group had the fewest number of patients with 11 (0.3%). There was a twofold increase in diagnosed cases between the years 2010–2015 (2286) compared to the years 2004–2009 (1287).
Most of the tumors were ≥ 10 cm (64.2%) and the tumor size and metastatic characteristics are shown in Table 2. The median tumor size was 16.5 cm, while the mean tumor size was 24.5 cm. Approximately 89% of patients presented with no metastasis, while 9.1% presented with metastasis. The most common type of metastasis was distant metastasis without lymph node involvement (6.4%) and further characterizations of metastasis are presented in Table 2. The most common site of metastasis involved the lung in 90 patients (2.5%). Other common sites of metastasis in decreasing order included liver (39 patients, 1.1%), bone (32 patients, 0.9%), and finally brain (2 patients, 0.1%). There was lymphatic or vascular invasion within the primary tumor in 1.8% of the cohort.
Primary site, tumor stage, FNCLCC grade, and treatment modalities are shown in Table 3. The most common primary site was the retroperitoneum or abdomen with 2125 patients (59.5%), followed by the pelvis (16.5%), extremities (14.4%), thorax or trunk (6.2%), head or neck (0.7%), and finally overlapping primary sites representing 0.6% of the cohort. Of the 2125 patients with retroperitoneal or abdominal dedifferentiated tumors, 1365 were coded as retroperitoneal tumors.
FNCLCC grade 3 and advanced stage III tumors were most common, at 34.8% and 40%, respectively. Stage IV was the least common stage with 292 patients (8.2%), while grade 1 tumors were the least common grade with 147 patients (4.1%).
Surgery was the most common treatment modality with 3244 patients or 90.8% of the patients utilizing this option, while radiation was the second most common modality with 1264 patients (35.4%), followed by chemotherapy with 589 patients (16.5%). Surgery alone with no adjuvant therapy was utilized by 67.6% of patients, while 23.6% used surgery with radiation. Surgery and chemotherapy were used in 6.1% of patients and only 2.6% were treated with surgery and chemoradiation.
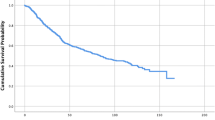
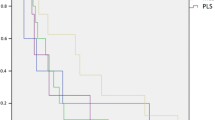
Overall 5- and 10-year survival probabilities for the 3,112 patients with primary DDLPS were 51.5% and 34.8%, respectively, and a Kaplan–Meier curve for overall survival for the cohort as a whole is shown in Fig. 1. A Kaplan–Meier curve by sex is shown in Fig. 2. Males showed 5- and 10-year survival probabilities of 52.0% and 36.1%, while females exhibited 5- and 10-year survival probabilities of 50.9% and 32.8%.
As age increased, the overall survival probability decreased, shown in both Table 4 and with a Kaplan–Meier curve in Fig. 3. The age group of 26–50 years had the best 5- and 10- year survival probabilities (66.8% and 52.9%, respectively) and a significantly higher median survival compared to all other age groups at 124.6 ± 9.7 months. This resulted in an almost doubling of median survival compared with patients 51–75 years old (65.2 ± 3.9 months), and almost a fourfold increase compared to patients > 75 years (35.1 ± 3.0 months).
Head or Neck primary site had the best overall survival with 86.4% at both 5- and 10 years and the results are shown in Fig. 4 and Table 4. Median survival data were not available for head or neck tumors, but the best median survival was seen in tumors of the pelvis (131.7 ± 7.9 months), followed by extremities (110.2 ± 11.0 months), thorax or trunk (85.3 ± 9.6 months), and finally the retroperitoneum or abdomen (45.5 ± 2.3 months). With minor exceptions, 5- and 10-year survivals parallel these median survivals. Followed by the head or neck, the extremities showed the best 5-year survival (67.1%) and the pelvis had the best 10-year survival probability at 50.2%. The worst 5- and 10-year survival probabilities were seen in retroperitoneal or abdominal primary sites with 42.6% and 25.7%, respectively.
Tumor size survival probabilities are graphed as a Kaplan–Meier curve in Fig. 5. Tumor size was found to significantly affect survival probabilities, with tumors less than 10 cm having better 5- and 10- year survival probabilities (66.1% and 46%) and a median survival (102.8 ± 9.8 months) double that of tumors greater than or equal to 10 cm (median survival of 51.1 ± 2.9 months and 5- and 10-year survivals of 46.2% and 29.6%).
Survival probabilities by stage are plotted as Kaplan–Meier curves in Fig. 6. As expected, Stage IV had the worst survival probabilities with a median survival of 10.2 ± 1.9 months and 5- and 10-year survival probabilities of 18.1% and 11.8%, respectively. Stage I had the highest median survival of 95.8 ± 13.7 months and best 10-year survival probability of 46.6%. Stage II had the best 5-year survival probability of 66.7%.
Survival by FNCLCC grade is shown in Fig. 7, with grade 1 and grade 2 having significantly better survival than grade 3 DDLPS. The data were limited as grade 1 and grade 2 tumors never dropped below 50% survival thus preventing reporting of median survival. The overall survival for FNCLCC grade only extended to 80 months thus preventing a 10-year survival probability calculation. Grade 1 DDLPS had the best 5-year survival probability of 69.2% followed by grade 2 at 64.7% and grade 3 at 44.9%.
Radiation treatment yielded the best 5- and 10-year survival probabilities (59% and 39.3%) and median survival (85.9 ± 6.2 months), while those patients treated with chemotherapy had the worst 5- and 10-year survival probabilities (37.6% and 23.9%) and median survival (35.0 ± 4.0 months). Adjuvant therapies and their survival probabilities were plotted in Fig. 8. Out of the adjuvant therapies, surgery with radiation offered the best 5-year survival (63.4%) and median survival (93.6 ± 9.3 months), while surgery with chemoradiation yielded the best 10-year survival percentage (46%). Surgery with chemotherapy resulted in the worst 5- and 10-year survival outcomes at 37.8% and 23.9%, and the worst median survival of 41.3 ± 6.0 months.
Results from the Cox hazard regression model are shown in Table 5. Several results are notable. Controlling for all other variables, there was an associated 3.3% increase in the risk of death for every one year increase in age (95% CI: 2.2% to 4.5%; p < 0.001). It was also found that males had a 19.6% increased risk of death in comparison to females (95% CI: 3.0% to 38.9%; p = 0.019). In the comparison of stage groups, stage IV disease compared to stage I disease resulted in the highest risk of death, which was 3.097 times higher (95% CI: 2.126 to 4.510; p < 0.001). A retroperitoneal or abdominal primary site demonstrated increased hazard ratios compared to each of the other primary sites including extremities (HR = 1.932; 95% CI: 1.479–2.255; p < 0.001), pelvis (HR = 1.938; 95% CI: 1.420–2.645; p < 0.001), and thorax/trunk (HR = 1.605; 95% CI: 1.142–2.255; p = 0.006). For treatment options, surgery with adjuvant radiation showed a decreased risk of death in comparison to surgery alone (HR = 0.785; 95% CI: 0.649 to 0.950; p = 0.013); adjuvant chemotherapy vs. adjuvant radiation was affiliated with increased risk of death (HR = 1.896; 95% CI: 1.339 to 2.685; p < 0.001). A comparison of all the primary sites to head or neck resulted in hazard ratios greater than > 99.999.
Discussion
To the best of our knowledge, this is the largest and most comprehensive study on DDLPS. The previous largest study on DDLPS was in 1997 utilizing 155 patients and there have been no large-scale studies utilizing United States databases including the NCDB, Surveillance, Epidemiology, and End Results (SEER) Program, or any other country’s database. Previous studies have focused primarily on retroperitoneal DDLPS.
The literature has debated whether DDLPS affect the sexes equally or if there is a male predominance (Goldblum et al. 2014; Lahat et al. 2008). In this cohort, 65% of the patients were males, while 35% were females with a 1.86 ratio of male to female patients. A previous study at University of Texas MD Anderson Cancer Center also found a male predominance with 68.8% of their patients being males (Lahat et al. 2008). The effect of gender and tumor size on survival for DDLPS has been questioned, but with the small number of patients in those reports, previous studies could not accurately determine the extent of these factors (Tirumani et al. 2015; Lahat et al. 2008). Our study shows not only an increased incidence among males, but a higher mortality, with an increased hazard ratio of 1.196, which translates to a 19.6% increased chance of mortality in male patients. This finding is contradictory to our survival probabilities. This difference could be related to patients with missing data being excluded from the multivariate analysis.
The only previously reported significant finding on the effect of age on DDLPS was that patients older than 65 years showed worse outcomes (Lahat et al. 2008). In well-differentiated liposarcoma tumors, several studies showed old age and larger tumor size were noted to be significantly worse prognostic indicators, but the magnitude of that effect was unclear (Knebel et al. 2017; Lahat et al. 2008). This current study is the largest cohort to date and clearly demonstrated that as age increased, median survival and 5-year and 10-year survival probabilities decreased. The 26–50 year age group had the best survival (excluding the 0–25 age group, which only had 11 patients). In fact, the median survival in that 26–50 year group (125 months) was almost twofold better than the survival of 51- to 75-year-old patients (65 months) and almost fourfold better than the median survival in patients older than 75 (35 months). As age increased by each year, patients with DDLPS showed a statistically significant 3.3% increased risk of mortality. Regarding age at presentation, Henricks et al. reported a median age at diagnosis of 61.5 years, which was similar to our study’s median age of 64 years (1997).
Median tumor size in the previous large study of DDLPS was 19 cm and another study found the median tumor size to be 17 cm (Henricks et al. 1997; Lahat et al. 2008). This current study found a similar median tumor size of 16.5 cm. Size is important for survival probabilities and our results showed that the median survival of a tumor < 10 cm at presentation (103 months) was twofold better than the median survival of a tumor ≥ 10 cm (51 months).
Henricks et al. found that the retroperitoneal primary site had the highest disease related mortality of 34%, while spermatic cord/scrotum had 18% mortality, and the extremities, trunk and head/neck demonstrated 11% mortality (1997). Median survival and 5- or 10-year survival probabilities were not presented and the bundling of extremities, trunk, and head/neck into one group make further comparisons limited. This current study confirmed that tumors located in the retroperitoneum or abdomen had the worst 5- and 10-year survival probabilities and median survival, while tumors located in the head or neck, extremities, pelvis, and thorax or trunk, had much better outcomes. While head or neck tumors had the best 5- and 10-year survival, there were only 24 patients in that group (0.7%) and median survival was not available. DDLPS tumors in the pelvis had the best median survival at 131.7 months and an overall 5-year survival of 65.8%, while the retroperitoneum or abdominal tumors had the worst median survival of 45.5 months. In a study of 57 patients with retroperitoneal DDLPS, Mussi et al. (2008) reported a 5-year disease-specific survival to be 42%, which is remarkably similar to our overall 5-year survival of 42.6% in 2125 patients with retroperitoneal and abdominal DDLPS. When comparing all other primary sites to retroperitoneal tumors, there was a 93.8% increase in mortality when retroperitoneal tumors were compared to pelvic origin, 93.2% increase compared to extremities, and a 60.5% increase compared to primaries in the thorax or trunk. The head or neck primary site resulted in extremely high hazard ratios when compared to all other primary sites, which could be related to the head or neck group consisting of < 1.0% of the patient cohort. Further analysis in the Surveillance, Epidemiology, and End Results Program database may be indicated to further quantify the risk of mortality in cases of dedifferentiated liposarcoma localized to the head or neck.
In previous studies, the incidence of metastases has ranged from 15 to 30%, with the lung reported as the most common site of metastasis (Thway et al. 2016; Tirumani et al. 2015). Our current study found a much lower rate of metastasis at 8.9% but confirmed the lung as the most common site.
Regarding histologic grade, Dantey et al. (2017) found in 55 patients that low-grade (grade 1) dedifferentiated tumors had much better survival outcomes compared to high-grade DDPLS (combination of grades 2 and 3). Their reported median survival for low-grade and high-grade dedifferentiated tumors were 113 and 48 months, respectively (Dantey et al. 2017). In our study with 3,573 patients, grade 3 DDLPS tumors had exactly the same median survival of 48.79 ± 3.5 months and an overall 5-year survival of 44.9%. Grade 1 and 2 tumors had much higher 5-year survival probabilities of 69.2% and 64.7%, respectively, thus confirming that higher histologic grades demonstrated worse outcomes when compared to low-grade DDLPS.
Not unexpectedly, as tumor stage increased, median survival and both 5- and 10-year survival probabilities decreased. Stage I and stage II tumors had similar hazard ratios and while the highest overall 5-year survival probability was stage II tumors with 66.7%, stage I was close behind at 63%. Higher stages dropped precipitously, with stage III at 49.1% and stage IV at 18.1%. Stage IV DDLPS had a median survival of 10.2 months. In a comparison between the early stage I and most advanced stage IV tumors, there was a 209.7% increased chance of mortality. When compared to stage III and stage IV, stage II tumors had a 38.7% and 70.6% decrease in the probability of mortality.
This study’s overall survival of 63.57 months was the highest reported in the literature with previous studies reporting overall survival of approximately 45 months (Lahat et al. 2008; Livingston et al. 2017). Our 5-year survival of 51.5% is higher than the previous study’s 5-year survival at 34.8% (Lahat et al. 2008). In fact, our 10-year survival of 34.8% is closer to their reported 5-year survival. It is unclear if these differences are related to differences in tumor behavior or improvements in treatment and long-term survival. Further research may be indicated in this area.
Treatment options are determined in large part by the extent of disease, which can be difficult to ascertain in a retrospective study. Surgical treatment remains the primary and most prevalent treatment option, utilized by 90.8% of the cohort. Radiation is commonly used preoperatively to shrink retroperitoneal and intra-abdominal tumors (Brennan et al. 2013). In this cohort, 35.4% of patients were treated with radiation therapy. Chemotherapy was utilized by 16.5% of patients and is typically reserved for metastatic or distant disease. A recent study, however, suggested that chemotherapy can be effective in shrinking the tumor (Livingston et al. 2017).
Of all treatments and adjuvant therapies, primary radiation and adjuvant radiation resulted in the highest median survival (93 months) and 5-year survival probabilities (63.4%). In our cohort, adjuvant radiation was used by 23.6% of patients and adjuvant chemotherapy was utilized by only 6.1% of patients. For adjuvant therapies, no overall survival benefit has been found with adjuvant chemotherapy for DDLPS, but adjuvant radiation has been shown to benefit the patient, especially in extremities (Cesne et al. 2014; O’Sullivan et al. 2002; Brennan et al. 2013). Of all the therapy options and adjuvant therapies, primary chemotherapy and adjuvant chemotherapy resulted in the worst 5- and 10-year survival probabilities and median survival. This could be related to the low response rate of DDLPS to chemotherapy and may indicate that patients requiring chemotherapy have more distant or metastatic disease and, therefore, poorer prognoses. Through multivariate analysis, adjuvant chemotherapy, compared to surgery alone and surgery with radiation, resulted in an increased probability of mortality of 11.7% and 89.6%, respectively. Surgery and radiation compared to surgery alone, resulted in a decreased mortality probability of 21.5%. Adjuvant chemotherapy demonstrated increased hazard ratios compared to surgery alone. These findings suggest an increased role for adjuvant radiation irrespective of primary site, stage, age, and sex, and potentially decreasing the role of the less effective chemotherapy.
A major limitation is the retrospective design and a further randomized prospective study confirming the adjuvant therapy findings may be warranted. Data compiled in the database may be incompletely, improperly, or inaccurately recorded from the patients’ charts. Pathology in NCDB is performed by pathologists at many different CoC accredited cancer programs and since there is no review of pathologic findings, there is potential for inter-observer error. Selection bias is inherent by only adding patients from CoC accredited cancer programs, although since the NCDB represents approximately 70% of all new cancer patients in the United States, this bias is likely minimal. Finally, survivorship information is defined as overall survival and unrelated causes of death may be recorded. The large number of patients in this study hopefully minimizes the risks of bias based on inaccurate survival data. A study utilizing the NCDB to further investigate socioeconomic prognostic factors might be helpful to determine their effects on survival.
This is the largest study to date on dedifferentiated liposarcoma and major prognostic factors include primary site, age, sex, stage, and adjuvant therapy. Out of all the primary anatomical sites, retroperitoneal or abdominal DDLPS tumors resulted in the highest risk of mortality. This increased risk with retroperitoneal or abdominal DDLPS tumors ranged from 60.5% to 93.8% when compared to other anatomical primary sites. In a comparison between adjuvant therapies, adjuvant radiation gave the best 5-year survival probability of 63.4% and led to a 21.5% decreased risk of mortality when compared to surgery alone. Adjuvant chemotherapy resulted in a 48.9% increased risk of mortality when compared to adjuvant radiation therapy. In conclusion, the retroperitoneal or abdominal primary site, increasing age, male sex, increasing stage, and adjuvant chemotherapy were all associated with a higher risk of mortality, while adjuvant radiation resulted in a lower chance of mortality.
References
Brennan M, Antonescu C, Maki R (2013) Management of soft tissue sarcoma. New York, United States
Cesne AL, Ouali M, Leahy MG et al (2014) Doxorubicin-based adjuvant chemotherapy in soft tissue sarcoma: pooled analysis of two STBSG-EORTC phase III clinical trials. Ann Oncol 25(12):2425–2432
Dantey K, Schoedel K, Yergiyev O, Bartlett D, Rao U (2017) Correlation of histological grade of dedifferentiation with clinical outcome in 55 patients with dedifferentiated liposarcomas. Hum Pathol 66:86–92
Engström K, Bergh P, Gustafson P et al (2008) Liposarcoma Cancer 113(7):1649–1656
Goldblum J, Enzinger F, Folpe A, Weiss S (2014) Enzinger and Weiss’s soft tissue tumors (6th ed.). Philadelphia, United States
Henricks WH, Chu YC, Goldblum JR, Weiss SW (1997) Dedifferentiated liposarcoma: a clinicopathological analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol 21:271–281
Knebel C, Lenze U, Pohlig F et al (2017) Prognostic factors and outcome of Liposarcoma patients: a retrospective evaluation over 15 years. BMC Cancer 17(1):410
Lahat G, Anaya D, Wang A et al (2008) Resectable well-differentiated versus dedifferentiated liposarcomas: two different diseases possibly requiring different treatment approaches. Ann Surg Oncol 15(6):1585–1593
Livingston J, Bugano D, Barbo A et al (2017) Role of chemotherapy in dedifferentiated liposarcoma of the retroperitoneum: defining the benefit and challenges of the standard. Sci Rep 7(1):11836
Mangham D (2004) World Health Organisation classification of tumours: Pathology and genetics of tumours of soft tissue and bone. J Bone Joint Surg Am 86(3):466
Mussi C, Collini P, Miceli R et al (2008) The prognostic impact of dedifferentiation in retroperitoneal liposarcoma. Cancer 113(7):1657–1665
O’Sullivan B, Davis AM, Turcotte R et al (2002) Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet 359:2235–2241
Thway KL, Jones RB, Noujaim J, Zaidi S, Miah A, Fisher C (2016) Dedifferentiated liposarcoma: updates on morphology, genetics, and therapeutic strategies. Adv Anat Pathol 23(1):30–40
Tirumani SH, Tirumani H, Jagannathan JP et al (2015) Metastasis in dedifferentiated liposarcoma: predictors and outcome in 148 patients. Eur J Surg Oncol 41(7):899–904
Funding
This manuscript had no funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Gootee, J., Aurit, S., Curtin, C. et al. Primary anatomical site, adjuvant therapy, and other prognostic variables for dedifferentiated liposarcoma. J Cancer Res Clin Oncol 145, 181–192 (2019). https://doi.org/10.1007/s00432-018-2777-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-018-2777-3