Abstract
Purpose
Predicting the feasibility of platinum-based chemotherapy remains an important issue in elderly (over 70 years) patients with non-small cell lung cancer (NSCLC). The aim of this study was to identify the risk factors for the early serious adverse events (SAEs) (during cycles 1–2) in elderly receiving platinum-based chemotherapy, and to explore the clinical characteristics of patients who require early treatment termination without progressive disease (PD).
Methods
One hundred and ninety-eight consecutive elderly NSCLC patients receiving platinum-based chemotherapy were retrospectively reviewed.
Results
The median age was 73 years (range 70–83). 161 (81 %) were males, and 190 (95 %) were PS 0–1. Fifty-one (29 %) and 39 (19 %) patients developed early non-hematological SAEs and hematological SAEs, respectively. Multivariate analysis identified low serum albumin (<3.0 g/dl) as an independent risk factor for non-hematological SAEs, while low creatinine clearance (<45 ml/min) for hematological SAEs. In all, 24 (12 %) patients needed early treatment termination without PD. The major reason for this event was the development of non-hematological SAEs (4.5 %), followed by grade 2 non-hematological adverse events (AEs) (3 %). In multivariate analysis, age over 75 years and low serum albumin were associated with this event. The median overall survival (OS) in patients with this event was only 6.0 months, while the development of early SAE was not associated with poor OS.
Conclusion
Baseline serum albumin might be useful for predicting the feasibility of platinum-based chemotherapy, and the risk estimation of early treatment termination without PD might be beneficial for the treatment selection in elderly NSCLC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of death worldwide. Non-small cell lung cancer (NSCLC) accounts for 80–85 % of all lung cancers, and more than 50 % of patients with newly diagnosed advanced NSCLC are elderly (over 70 years of age) (Kaneko et al. 2003; Siegel et al. 2014).
Although platinum-based doublet chemotherapy is the standard treatment for younger patients with advanced or recurrent NSCLC (Ohe et al. 2007; Schiller et al. 2002), the optimal treatment selection for elderly NSCLC patients still remains unclear. A randomized phase III trial that compared vinorelbine monotherapy with best supportive care showed a survival benefit of vinorelbine with tolerable toxicity (The Elderly Lung Cancer Vinorelbine Italian Study Group 1999). Monotherapy with gemcitabine or docetaxel is also reported as viable option for elderly NSCLC patients (Gridelli et al. 2003; Kudoh et al. 2006). In fit elderly patients selected by the restrict eligibility criteria, platinum-based doublet chemotherapy showed survival benefit as compared to monotherapy with vinorelbine or gemcitabine (Quoix et al. 2011). However, platinum-based doublet chemotherapy was associated with a high incidence of toxicities, including treatment-related death (TRD) of 4.4 % of the patients. Moreover, in another phase III study conducted in Japan, the benefit of platinum-based doublet chemotherapy over docetaxel was observed only in patients aged 70–74, but not in those over 75 years of age, which resulted in early study termination (Tsukada et al. 2015). In a repeat phase III study conducted to evaluate the superiority of platinum-based doublet chemotherapy over docetaxel in Japan, no survival benefit was observed in either patients aged 70–74 years old or in those over 75 years of age (Abe et al. 2015).
These conflicting results might come from the diversity of feasibility for cytotoxic chemotherapy in elderly patients (Gajra and Jatoi 2014). Vincent et al. pointed out several problems in regard to the toxicity of anticancer chemotherapy, such as the difficulty in predicting toxicity in individual patients and the absence of a database of the real toxic effects observed in community practice (Vincent and Dranitsaris 2009). These problems might be even more relevant in elderly cancer patients. Therefore, attempts to predict the individual risk of serious adverse events (SAEs) in elderly patients have been made in several studies. Huria et al. conducted a prospective cohort study based on a scoring system using both geriatric assessment variables and laboratory data to predict the risk of SAE in patients with solid tumors receiving cytotoxic chemotherapy (Hurria et al. 2011). Another study showed the usefulness of the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score for predicting the toxicity of chemotherapy in elderly patients with solid tumors (Extermann et al. 2012). These studies included patients with several types of solid tumors treated with various kinds of chemotherapies (monotherapy or combined therapy, different chemotherapy regimen in each solid tumor). Therefore, it remains unclear whether these results are applicable to the specific population of elderly NSCLC patients scheduled to receive platinum-based doublet chemotherapy.
In addition, it is unclear as to what types of adverse events (AEs) might necessitate early treatment termination of platinum-based doublet chemotherapy and whether the development of SAEs is actually associated with the survival in elderly patients in community practice. In terms of the optimal number of cycles of first-line platinum-based chemotherapy, no difference in the survival benefit was observed between limited therapy (3–4 cycles) and extended therapy (6 cycles) (Park et al. 2007; Rossi et al. 2014; von Plessen et al. 2006). These evidences suggest that the maximum efficacy of platinum-based chemotherapy may be obtained after 3–4 cycles of treatment. Therefore, early treatment termination without progressive disease (PD) (during cycles 1–2) in elderly NSCLC patient receiving platinum-based chemotherapy would be an unfavorable event.
Under these circumstances, in the present multicenter retrospective cohort study, we focused on both the development of early SAEs (during cycles 1–2) and early treatment termination without PD in elderly NSCLC patients receiving platinum-based chemotherapy.
Methods
Study design
This retrospective cohort study was conducted with the approval of the ethical review committee of Nagoya University Hospital and the other participating institution. The study was supported by Central Japan Lung Study Group (Nagoya, Japan) as the CJLSG 1203 trial. A total of nine centers of the CJLSG participated in this study and performed in accordance with the principles of the Declaration of Helsinki. The end points of this study were to identify the risk factors for (1) early non-hematological SAEs, (defined as grade 3–5 AEs according to the Common Terminology Criteria for Adverse Events [CTCAE v4.0] during cycles 1–2), (2) early hematological SAEs (defined as grade 4–5 AEs according to CTCAE v4.0 during cycles 1–2), and (3) early treatment termination without PD (during cycles 1–2). In addition, to explore the clinical characteristics of patients who require early treatment termination without PD was also analyzed as an exploratory end point.
Patient selection
We retrospectively reviewed the medical records of patients with NSCLC treated with first-line chemotherapy at each center between January 2010 and June 2012. Patients for this study were selected based on the following eligibility criteria: (1) diagnosed as having stage IIIB/IV or recurrent NSCLC confirmed by histological or cytological examination, (2) over 70 years of age at the date of the start of first-line chemotherapy, (3) receiving platinum-based chemotherapy (combined administration with bevacizumab was allowed).
Data collection
Detailed review of medical records of each patient was performed. Data on the baseline clinical characteristics, including the laboratory data and comorbidities, were collected. The chemotherapy regimen used, number of cycles administered, dosage of each agent, and the date of documentation of disease progression and death were also reviewed. The scoring for comorbidities was performed using both the Charlson comorbidity index (CCI) and simplified comorbidity score (SCS). CCI was proposed by Charlson et al. and is widely used for evaluating the comorbidities in geriatric assessment (Charlson et al. 1987; Hurria et al. 2011). SCS is a specific scoring method for comorbidities in lung cancer patients (Colinet et al. 2005). In brief, the scoring is based on the presence/absence of six comorbidities (diabetes mellitus, renal insufficiency, respiratory comorbidity, cardiovascular comorbidity, neoplastic comorbidity, and alcoholism) and the history of tobacco use. SCS showed the superiority compared to the CCI in predicting survival in patients with NSCLC (Jacot et al. 2008). The cutoff values of the CCI and SCS were determined according to the original report of each (Charlson et al. 1987; Colinet et al. 2005). In terms of the AEs, the worst grade in each cycle was considered for assessment according to CTCAE v4.0. The objective tumor responses were evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1.
Statistical analysis
Differences in categorical variables were analyzed by Fisher’s exact test. The cutoff values for the continuous variables were determined based on standard values or previous reports. For this study, serum albumin (<3.0 vs. ≥3.0 g/dl), serum lactate dehydrogenase (<230 vs. ≥230 IU/dl), hemoglobin [<10 vs. ≥10 g/dl (female), <11 vs. ≥11 g/dl (male)], and CCr (<45 vs. ≥45 ml/min) were considered (Akbari et al. 2014; Hurria et al. 2011). In addition to age, sex, and PS, which are considered as potentially significant factors for the feasibility of chemotherapy in the elderly, variables with p values of <0.20 identified by univariate analysis were selected as potential predictors for the subsequently performed multivariate analyses. Multivariate analysis for the development of early non-hematological and hematological SAEs was performed using a logistic regression model. Progression-free survival (PFS) was defined as the time from the date of the start of the platinum-based chemotherapy until disease progression, death due to any cause or the last follow-up. Overall survival (OS) was defined as the time from the date of start of the platinum-based chemotherapy until death due to any cause or the date of the last follow-up. Kaplan–Meier curves for the OS were plotted, and the survival curves were compared using the log-rank test. Multivariate analysis for OS was performed using Cox proportional hazard model. All analyses were conducted using the SPSS software, version 22.0 (IBM, New York, USA).
Results
Patient characteristics and chemotherapy regimen
Between January 2010 and June 2012, a total of 344 elderly NSCLC patients received first-line chemotherapy at any of the nine participating centers. Of these, a total of 198 elderly NSCLC patients receiving platinum-based chemotherapy were identified as being eligible for this study; the remaining patients were receiving monotherapy with a non-platinum agent (Fig. 1). The patient characteristics are shown in Table 1. The median age was 73 years (range 70–83 years), and 72 (36 %) patients were over 75 years of age, 161 (81 %) were male and 37 (19 %) were female. The PS was 0–1 and 2 in 190 (95 %) and 8 (5 %) patients, respectively. The histological subtype of the tumor was adenocarcinoma in the majority of the patients (n = 106, 54 %), followed by squamous cell carcinoma (n = 54, 27 %). The test for EGFR mutation was positive in 15 patients (7 %), negative in 138 patients (70 %), and unknown in 45 patients (23 %). Of the total, 59 (30 %) patients had a CCI of ≥3 and 75 (38 %) had a SCS of ≥10.
Treatment regimen and adverse events profile
Of the 198 patients, 181 (91 %) received carboplatin-based chemotherapy. The majority of drugs used in combination were pemetrexed (n = 83, 42 %) followed by paclitaxel (n = 59, 30 %). Bevacizumab was used in 11 patients (6 %) (Table 2). The ORR in the entire subject population was 31.4 % [95 % confidence interval (CI) 23.5–36.7 %]. The median PFS and median OS in the entire subject population were 5.0 months (95 % CI 4.6–5.7 months) and 11.9 months (95 % CI 9.1–14.7 months), respectively. The profile of the major AEs observed during the early phase (during cycles 1–2) is summarized in Table 3. Treatment-related death (grade 5) during cycles 1–2 was observed in four cases (2 %), including that caused by pneumonitis possibly related to chemotherapy in two cases, febrile neutropenia in one case, and pleural infection in one case.
Clinical factors associated with early development of SAEs
The incidence of patients who developed at least one early non-hematological SAE or hematological SAE was analyzed and found that there were 51 (26 %) and 39 (19 %) patients who developed early non-hematological SAEs and hematological SAEs, respectively. During the entire course of treatment, 61 (31 %) and 57 (29 %) patients developed non-hematological SAEs and hematological SAEs, respectively. In regard to the development of early non-hematological SAEs, univariate analysis identified the disease stage [Odd ratio (OR) 8.80, 95 % CI; 1.16–67.05], presence/absence of anemia (OR 2.35, 95 % CI; 1.04–5.35), and the serum albumin (OR 3.26, 95 % CI; 1.48–7.21) as significant factors. Subsequent multivariate analysis including these factors and other predetermined factors (age, sex, ECOG PS) identified low serum albumin (<3.0 mg/dl) as an independent unfavorable factor for the development of early non-hematological SAEs (adjusted OR 2.66, 95 % CI; 1.13–6.27) (Table 4). On the other hand, in regard to the development of early hematological SAEs, univariate analysis identified CCr as a significant factor (OR 7.05, 95 % CI; 1.88–26.37), and multivariate analysis with the predetermined factors of age, sex, and ECOG PS identified low CCr (<45 ml/min) as an independent unfavorable factors for early hematological SAEs (adjusted OR 6.13, 95 % CI; 1.61–23.34) (Table 5).
Necessitation of early treatment termination without PD
We next analyzed the incidence of requiring early treatment termination without PD. Of the 198 patients, 24 (12 %) required early treatment termination without PD. As shown in Table 6, the major reason for the early treatment termination in individual patients was the development of grade 3 non-hematological AEs (n = 9, 4.5 %), followed by that of grade 2 non-hematological AEs (n = 6, 3 %). The use of cisplatin was not associated with the high incidence of early treatment termination without PD (n = 1, 5.9 % in patients treated with cisplatin versus n = 23, 12.7 % in patients treated with carboplatin, p = 0.70, Fisher’s exact test). In terms of the use of combination drug, PTX regimen had a tendency toward the more frequent development of early treatment termination when compared to non-PTX regimen (18.6 vs. 9.4 %, p = 0.09, Fisher’s exact test). However, early treatment termination was also observed in 12 of 83 patients (14.5 %) treated with PEM regimen. We also analyzed the association between the presence of dose reduction and the early treatment termination without PD. When we consider the association between dose reduction and early treatment termination, dose reduction in cycle 2 would potentially reduce the risk of failure to go with cycle 3, and which could influence the incidence of early treatment termination. Among 178 patients received treatment of cycle 2, 37 patients (20.9 %) were treated with dose reduction. The incidence of early treatment termination was not influenced by the presence of dose reduction in cycle 2 (dose reduction in cycle 2, yes vs. no: early termination, 5.7 % [2 of 37 patients] vs. 5.0 % [7 of 141 patients], p = 1.00, Fisher’s exact test). As shown in Table 7, multivariate analysis identified higher age (≥75 years) (adjusted OR 4.00, 95 %CI; 0.65–11.52) and low serum albumin (<3.0 mg/dl) (adjusted OR 5.58, 95 % CI; 1.83–17.39) as significant factors predictive of early treatment termination without PD. Figure 2a shows the proportions of patients who require the early treatment termination without PD according to the age group (70–74 years or ≥75 years) and serum albumin (<3.0 vs. >3.0 g/dl). It is noteworthy that early treatment termination without PD was required in 58 % of patients aged over 75 years with a low serum albumin, but in only 4 % of patients aged 70–74 years with a normal serum albumin (p < 0.01, Pearson’s test). Interestingly, the proportion of patients who required early treatment termination due to PD was not statistically different between these four groups classified by age (70–74 years or ≥75 years) and serum albumin (<3.0 vs. >3.0 g/dl) (Fig. 2a). In terms of comorbidity score, 7 % of patients with CCI 0, 11 % with CCI 1–2, 19 % with CCI 3–4, and 18 % with CCI > 5 required early treatment termination, with no statistically differences (p = 0.20, Pearson’s test) (Fig. 2b). Similarly, the proportion of patients requiring early treatment termination without PD did not differ significantly according to the SCS (8 % in patients with SCS 0–7, 13 % in patients with SCS 8–9, 18 % in patients with SCS 10–11, and 13 % in patients with SCS 12) (p = 0.87, Pearson’s test) (Fig. 2c).
Incidence of early treatment termination without progressive disease (PD) (n = 188, 11 patients for whom the data on albumin were not available were excluded) in subgroups classified according to a age and serum albumin, b Charlson’s comorbidity index (CCI) (n = 198), and c simplified comorbidity score (SCS) (n = 198)
Survival analysis in subgroups divided according to early development of SAE/early treatment termination without PD
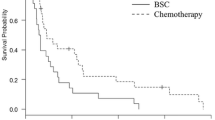
We finally performed exploratory analysis of the OS of patients who developed at least one hematological and/or non-hematological early SAE and required early treatment termination without PD. We divided the patients into three subgroups according to whether they developed early SAEs and/or required early treatment termination without PD; group 1 consisted of patients who neither developed early SAE nor required early treatment termination without PD, group 2 consisted of patients who developed early SAEs, but did not require early treatment termination without PD, and group 3 consisted of patients who required early treatment termination without PD, regardless of whether they developed early SAEs or not. The median OS of all of these patients was 11.9 months (95 % CI; 9.1–14.7 months), as mentioned above. The median OS in group 1 was 13.1 months (95 % CI; 9.4–16.8 months), while that in group 3 was 6.0 months (95 % CI 1.5–10.5 months), being statistically significantly worse than that in group 1 (p < 0.01, log-rank test; HR 2.18 [95 % CI 1.29–3.70]). On the contrary, median OS in group 2 was 12.5 months (95 % CI; 7.7–17.3 months), showing no statistically significant difference as compared to that in group 1 (p = 0.84, log-rank test; HR 1.04 [95 % CI 0.71–1.53]) (Fig. 3). To evaluate the effect of confounding factors for survival, we also performed multivariate analysis using the Cox proportional hazard model. The results revealed that early treatment termination without PD was an unfavorable independent factor for the OS [adjusted hazard ratio 2.32 (95 % CI 1.33–4.02)] even after adjustments for age, sex, ECOG PS, and the EGFR mutation status. In addition, we explored whether the early treatment termination (1–2 cycles) without PD was unfavorable event by comparing to subgroup treated with three cycles or more. In total of 198 patients, 22 patients terminated treatment due to disease progression during cycles 1–2. As mentioned above, 24 patients required early treatment termination without PD during cycles 1–2. Therefore, the other 152 patients keep disease control at completion of cycle 2 and received treatment with three cycles or more. The median OS was 6.0 months (95 % CI 1.5–10.5 months) in patients with early treatment termination without PD (1–2 cycles) and 14.6 months (95 % CI 11.7–21.5 months) in patient treated with three cycles or more (p < 0.01, log-rank test).
Kaplan–Meier survival curves for the overall survival; group 1: patients with neither early serious adverse events (SAEs) nor early treatment termination without progressive disease (PD) (n = 118); group 2: patients with at least one early SAE, but not requiring early treatment termination without PD; group 3 (n = 56): patients who required early treatment termination without PD, regardless of the presence/absence of SAEs (n = 24)
Discussion
In the present study, we explored the risk factors for the development of early SAEs and early treatment termination without PD in elderly NSCLC patients receiving platinum-based chemotherapy. A low baseline serum albumin was identified as an independent predictor of early non-hematological SAEs, and a low baseline CCr as that of early hematological SAEs. In addition, it is noteworthy that 7 of 12 (58 %) patients over 75 years with a low serum baseline albumin required early treatment termination without PD. Our results might suggest that we need a careful consideration regarding the indication of platinum-based chemotherapy in those patients. To the best of our knowledge, this is the first study to show the importance of baseline serum albumin for predicting early treatment termination without PD in elderly NSCLC patients.
Previous studies have shown that the serum albumin sharply reflects the nutritional status, which has been identified as an independent factor influencing the risk of development of adverse events during cytotoxic chemotherapy (Arrieta et al. 2010; Gioulbasanis et al. 2011). In addition, low serum albumin has been reported to be associated with cachexia as defined by Fearon et al. (2011). These data are consistent with our identification of the serum albumin as a predictor of the development of non-hematological SAEs in the early phase of treatment. In regard to the development of hematological toxicities, a low CCr was identified as an independent unfavorable factor, which was consistent with previous reports. In a randomized phase II/III trial for advanced urothelial cancer, impaired renal function, but not a poor PS, was associated with a higher incidence of SAEs (neutropenia, thrombocytopenia, etc.) in patients receiving carboplatin plus gemcitabine (De Santis et al. 2009, 2012). Because of the affordable cost and convenience of measurement of these parameters, further validation studies to evaluate the usefulness of the serum albumin and CCr for predicting the feasibility of platinum-based chemotherapy in elderly NSCLC patients are warranted.
On the contrary, neither the CCI nor the SCI was associated with either development of early SAEs or early treatment termination without PD in our cohort. While previous reports have indicated the existence of an association between these comorbidity scores and the survival in patients with NSCLC, our results suggest that the presence of comorbidities may not be sufficient reason for withholding platinum-based chemotherapy in elderly NSCLC patients (Charlson et al. 1987; Jacot et al. 2008).
Quinox et al. mentioned that most of the patients enrolled in their phase III study were “fit” elderly patients; therefore, the positive results of platinum-based chemotherapy could not be generalized to non-fit elderly patients with poor geriatric conditions (Quoix et al. 2011). We certainly agree with this argument, but how do we distinguish “non-fit elderly” from “fit” elderly for administering platinum-based chemotherapy in community practice? Several studies have investigated approaches for predicting the development of SAEs in elderly patients receiving cytotoxic chemotherapy (Extermann et al. 2012; Hurria et al. 2011). However, few studies have assessed the influence of the development of SAEs on definitely clinical meaningful end points such as survival. Indeed, the development of SAEs per se, even in the early phase (during cycles 1–2), was found to have no influence on the overall survival in our analysis. In addition, early development of hematological SAEs necessitated early treatment termination without PD in only two patients, while nine patients who developed grade 3 non-hematological SAEs and seven who developed non-hematological grade 2 or less severe toxicities required early treatment termination without PD. Based on these results, it might be important to investigate not only how to predict the development of toxicities, but also determine what types of toxicities are clinically meaningful in elderly patients receiving chemotherapy.
In our study, we focused on the development of early treatment termination without PD in addition to early serious SAEs (during cycles 1–2). The patients who required early treatment termination without PD showed significantly poorer survival as compared to those who did not develop the event. Because no clinical trials have been reported comparing early treatment termination (1–2 cycles) to longer treatment (3–6 cycles) of platinum-based chemotherapy, we do not have any conclusive evidences whether early termination without PD is an unfavorable event or not. However, in our study, the median OS in patients with early termination without PD (during cycles 1–2) was only 6.0 months, which was statistically shorter compared to the ones in patients who received treatment with three cycles or more. These results might suggest early termination without PD would be an unfavorable event and the risk estimation of early treatment termination without PD might be beneficial in deciding whether to go ahead with platinum-based chemotherapy or not in elderly NSCLC patients. Of course, these results should be interpreted with caution, because the decision for early treatment termination in the presence of grade 2 or less AEs could be influenced by factors other than the clinical parameters, such as the patient’s own preferences, doctor’s judgment based on their experience, and the extent of family support available. However, when taking into consideration the importance of predicting the clinical meaningful events, it is necessary to keep trying to identify the risk of early treatment termination in elderly NSCLC patients including not only clinical factors but also social and mental factors in the future.
Our study had several limitations because of the retrospective nature of the study. Firstly, the incidence of AEs might be underestimated, even though we minutely reviewed the individual charts. Second, because of small sample size in each subgroup according to specific combination drug, our study would have limitation to analyze the specific toxicity of each combination drug which could influence the feasibility. Finally, our results were dependent on the data from a single cohort. Therefore, a validation study using another prospective cohort of elderly NSCLC patients is needed to test the robustness of our results. To resolve these limitations, we initiated another prospective cohort trial in elderly NSCLC patients, including evaluation by Vulnerable Elders Survey-13 and Mini-Mental State Examination, and the trial is now ongoing (Fukuse et al. 2005; Min et al. 2006).
In conclusion, baseline albumin would be useful for predicting the development of both early non-hematological SAEs and early treatment termination without PD in elderly NSCLC patients receiving platinum-based chemotherapy. Because the early treatment termination without PD was associated with a significantly poorer survival, the risk estimation of the event might be beneficial in deciding whether to go ahead with platinum-based chemotherapy or not in elderly NSCLC patients. Further studies to validate our results are warranted, and our ongoing prospective study may be expected to bring more robust information regarding these issues.
References
Abe T et al (2015) Randomized phase III trial comparing weekly docetaxel plus cisplatin versus docetaxel monotherapy every 3 weeks in elderly patients with advanced non-small-cell lung cancer the intergroup trial JCOG0803/WJOG4307L. J Clin Oncol. doi:10.1200/JCO.2014.55.8627
Akbari A et al (2014) Canadian society of nephrology commentary on the KDIGO clinical practice guideline for CKD evaluation and management. Am J Kidney Dis. doi:10.1053/j.ajkd.2014.10.013
Arrieta O et al (2010) Association of nutritional status and serum albumin levels with development of toxicity in patients with advanced non-small cell lung cancer treated with paclitaxel-cisplatin chemotherapy: a prospective study. BMC Cancer 10:50. doi:10.1186/1471-2407-10-50
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Colinet B, Jacot W, Bertrand D, Lacombe S, Bozonnat MC, Daures JP, Pujol JL (2005) A new simplified comorbidity score as a prognostic factor in non-small-cell lung cancer patients: description and comparison with the Charlson’s index. Br J Cancer 93:1098–1105. doi:10.1038/sj.bjc.6602836
De Santis M et al (2009) Randomized phase II/III trial assessing gemcitabine/carboplatin and methotrexate/carboplatin/vinblastine in patients with advanced urothelial cancer “unfit” for cisplatin-based chemotherapy: phase II–results of EORTC study 30986. J Clin Oncol 27:5634–5639. doi:10.1200/JCO.2008.21.4924
De Santis M et al (2012) Randomized phase II/III trial assessing gemcitabine/carboplatin and methotrexate/carboplatin/vinblastine in patients with advanced urothelial cancer who are unfit for cisplatin-based chemotherapy: EORTC study 30986. J Clin Oncol 30:191–199. doi:10.1200/JCO.2011.37.3571
Extermann M et al (2012) Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 118:3377–3386. doi:10.1002/cncr.26646
Fearon K et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495. doi:10.1016/S1470-2045(10)70218-7
Fukuse T, Satoda N, Hijiya K, Fujinaga T (2005) Importance of a comprehensive geriatric assessment in prediction of complications following thoracic surgery in elderly patients. Chest 127:886–891. doi:10.1378/chest.127.3.886
Gajra A, Jatoi A (2014) Non-small-cell lung cancer in elderly patients: a discussion of treatment options. J Clin Oncol. doi:10.1200/JCO.2014.55.3099
Gioulbasanis I, Baracos VE, Giannousi Z, Xyrafas A, Martin L, Georgoulias V, Mavroudis D (2011) Baseline nutritional evaluation in metastatic lung cancer patients: Mini Nutritional Assessment versus weight loss history. Ann Oncol Off J Eur Soc Med Oncol/ESMO 22:835–841. doi:10.1093/annonc/mdq440
Gridelli C et al (2003) Chemotherapy for elderly patients with advanced non-small-cell lung cancer: the Multicenter Italian Lung Cancer in the Elderly Study (MILES) phase III randomized trial. J Natl Cancer Inst 95:362–372
Hurria A et al (2011) Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 29:3457–3465. doi:10.1200/JCO.2011.34.7625
Jacot W, Colinet B, Bertrand D, Lacombe S, Bozonnat MC, Daures JP, Pujol JL (2008) Quality of life and comorbidity score as prognostic determinants in non-small-cell lung cancer patients. Ann Oncol 19:1458–1464. doi:10.1093/annonc/mdn064
Kaneko S et al (2003) Projection of lung cancer mortality in Japan. Cancer Sci 94:919–923
Kudoh S et al (2006) Phase III study of docetaxel compared with vinorelbine in elderly patients with advanced non-small-cell lung cancer: results of the West Japan Thoracic Oncology Group Trial (WJTOG 9904). J Clin Oncol 24:3657–3663. doi:10.1200/JCO.2006.06.1044
Min LC, Elliott MN, Wenger NS, Saliba D (2006) Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc 54:507–511. doi:10.1111/j.1532-5415.2005.00615.x
Ohe Y et al (2007) Randomized phase III study of cisplatin plus irinotecan versus carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer Four-Arm Cooperative Study in Japan. Ann Oncol 18:317–323. doi:10.1093/annonc/mdl377
Park JO et al (2007) Phase III trial of two versus four additional cycles in patients who are nonprogressive after two cycles of platinum-based chemotherapy in non small-cell lung cancer. J Clin Oncol 25:5233–5239. doi:10.1200/jco.2007.10.8134
Quoix E et al (2011) Carboplatin and weekly paclitaxel doublet chemotherapy compared with monotherapy in elderly patients with advanced non-small-cell lung cancer: IFCT-0501 randomised, phase 3 trial. Lancet 378:1079–1088. doi:10.1016/S0140-6736(11)60780-0
Rossi A et al (2014) Six versus fewer planned cycles of first-line platinum-based chemotherapy for non-small-cell lung cancer: a systematic review and meta-analysis of individual patient data. Lancet Oncol 15:1254–1262. doi:10.1016/S1470-2045(14)70402-4
Schiller JH et al (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. New Engl J Med 346:92–98. doi:10.1056/NEJMoa011954
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64:9–29. doi:10.3322/caac.21208
The Elderly Lung Cancer Vinorelbine Italian Study Group (1999) Effects of vinorelbine on quality of life and survival of elderly patients with advanced non-small-cell lung cancer. J Natl Cancer Inst 91:66–72
Tsukada H et al (2015) Randomized controlled trial comparing docetaxel-cisplatin combination with weekly docetaxel alone in elderly patients with advanced non-small-cell lung cancer: Japan Clinical Oncology Group (JCOG) 0207dagger. Jpn J Clin Oncol 45:88–95. doi:10.1093/jjco/hyu176
Vincent MD, Dranitsaris G (2009) The price function of toxicity. Lancet Oncol 10:299–303. doi:10.1016/S1470-2045(09)70067-1
von Plessen C et al (2006) Palliative chemotherapy beyond three courses conveys no survival or consistent quality-of-life benefits in advanced non-small-cell lung cancer. Br J Cancer 95:966–973. doi:10.1038/sj.bjc.6603383
Acknowledgments
This work was supported by Central Japan Lung Study Group.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have received no funding support for this work. Information about financial relationships outside the work is as follows: Dr. Morise has received speaking honoraria from Chugai Pharmaceutical Co., TAIHO Pharmaceutical Co., Eli Lilly Japan, and Pfizer Inc.; Dr. Ando has received speaking honoraria from Merck Serono Co.; Dr. Ogasawara has received speaking honoraria from Pfizer Inc., KYORIN Pharmaceutical Co., Glaxo Smith Kline K.K., Novartis Pharma Co., Meiji Seika Pharma Co., and Boehringer Ingerheim; Dr. Shindo has received speaking honoraria from Daiichi Sankyo, KYORIN Pharmaceutical Co., TAIHO PHARMACEUTICAL CO., MSD K.K., Kyowa Hakko Kirin co., Glaxo Smith Kline K.K., and Nippon Boehringer Ingelheim Co; Dr. Matsumoto has received speaking honoraria from TEIJIN LIMITED., Philips Respironics GK., Chugai Pharmaceutical Co., and DAIICHI SANKYO Co; Dr. Sugino has received speaking honoraria from Astellas Pharma Inc., Ono Pharmaceutical Co., Shionogi & Co., Abbott Japan Co., Ltd., MSD K.K., Sanofi, GlaxoSmithKline plc., Mitsubishi Tanabe Pharma., Pfizer Inc., Novartis Pharma K.K., AstraZeneca, and KYORIN Pharmaceutical Co.; Dr. Hase has received speaking honoraria from Chugai Pharmaceutical Co., AstraZeneca, Boehringer Ingerheim, Novartis Pharma, DAIICHI SANKYO COMPANY; Dr. Kondo has received speaking honoraria from Chugai Pharmaceutical Co., AstraZeneca, Boehringer Ingerheim, Novartis Pharma K.K., TAIHO Pharmaceutical Co., Pfizer Inc., and Eli Lily Japan K.K.; Dr. Saito reported a grant from ONO PHARMACEUTICAL CO., Merck Serno, TAIHO Pharmaceutical Co., Daiichi Sankyo, Daiichi Sankyo; Dr. Hasegawa reported receiving grant from Boehringer Ingelheim., Pfizer Inc., Astellas Pharma Inc., ONO PHARMACEUTICAL CO., Shionogi & Co., AstraZeneca, Sanofi K.K., TEIJIN LIMITED, MSD K.K., Meiji Seika Pharma Co., DAIICHI SANKYO COMPANY, LIMITED., GlaxoSmithKline K.K., Otsuka Pharmaceutical Co., KYORIN Pharmaceutical Co., Ltd., Sumitomo Dainippon Pharma Co., Novartis Pharma K. K., Kyowa Hakko Kirin Co., Eli Lilly Japan K.K., Chugai Pharmaceutical Co. that was paid to Nagoya University.
Ethical standards
All procedures performed in studies were in accordance with the ethical standards of the Institutional Research Board and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
This study design was the retrospective observational cohort study with no invasiveness for patients. All data were obtained by reviewing medical charts. Therefore, informed consent for each patient was not required according to the Japanese guideline of cohort study. This study was approved by Ethics Committee of all institutions.
Additional information
Toshio Kato and Masahiro Morise have contributed equally to this article
Rights and permissions
About this article
Cite this article
Kato, T., Morise, M., Ando, M. et al. Can we predict the development of serious adverse events (SAEs) and early treatment termination in elderly non-small cell lung cancer (NSCLC) patients receiving platinum-based chemotherapy?. J Cancer Res Clin Oncol 142, 1629–1640 (2016). https://doi.org/10.1007/s00432-016-2170-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-016-2170-z