Abstract
Purposes
Metformin, currently undergoing clinical trials as an adjuvant for the treatment of breast cancer, modulates the activity of key intracellular signalling molecules which affect 2-[18F]Fluoro-2-deoxy-d-glucose ([18F]FDG) incorporation. Here, we investigate the effect of drugs used in the treatment of breast cancer combined with metformin on [18F]FDG incorporation in HER2- or HER1-overexpressing breast cancer cells to determine whether or not metformin may obscure changes in [18F]FDG incorporation induced by clinically utilised anticancer drugs in the treatment of breast cancer.
Methods
Three breast cancer cell lines expressing HER2 and one HER2 negative but HER1 positive were exposed to metformin, doxorubicin and trastuzumab or cetuximab. Cytotoxicity was measured by the MTT assay. Expression of active (phospho-) AMPK, PKB (Akt) and ERK was determined by Western blotting. [18F]FDG incorporation by cells exposed to drug combinations with metformin was determined. Glucose transport was assessed by measuring the initial rate of uptake of [3H]O-methyl-d-glucose ([3H]OMG). Phosphorylation of [18F]FDG was determined in intact cells after exposure to [18F]FDG.
Results
Phospho-AMPK was increased by metformin in all cell lines whilst phospho-Akt and phospho-ERK expressions were decreased in two. Metformin treatment increased [18F]FDG incorporation in all cell lines, and treatment with anti-HER antibodies or doxorubicin only produced minor modulations in the increase induced by metformin alone. Glucose transport was increased in BT474 cells and decreased in SKBr3 and MDA-MB-468 cells after treatment with metformin. The fraction of phosphorylated [18F]FDG was increased in metformin-treated cells compared with controls, suggesting that hexokinase efficiency was increased by metformin.
Conclusion
This is the first study to show that increased [18F]FDG incorporation by breast cancer cells induced by metformin overwhelms the effect of doxorubicin and anti-HER treatments on [18F]FDG incorporation. Metformin-induced increased [18F]FDG incorporation was consistently associated with enhanced [18F]FDG phosphorylation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The biguanide metformin is used in the treatment of type 2 diabetes (T2D) as it decreases blood glucose levels by inhibiting hepatic gluconeogenesis and stimulating glucose uptake by muscle cells (Viollet et al. 2012). T2D is associated with increased cancer risk including that of breast cancer possibly due to increased plasma insulin levels (Jalving et al. 2013; Pollak 2013). A seminal study (Evans et al. 2005) reported that cancer incidence in T2D patients prescribed metformin was lower than in those not receiving metformin. More recently, metformin use by women with T2D was shown to reduce the risk of breast cancer (Bodmer et al. 2010) even when patients who administered insulin, a possible causative cancer agent, were removed from the analysis.
Studies also suggest that metformin may be used as a cancer treatment. The website clinicaltrials.gov details 29 clinical trials underway on breast cancer patients treated with metformin, either in combination treatment with other anticancer drug regimens or prior to surgical resection. An example of a completed study reported in the literature has found that metformin treatment, when used as an adjuvant, is associated with increased pathological complete response in early breast cancer (Jiralerspong et al. 2009).
Metformin inhibits the mitochondrial respiratory chain complex 1 resulting in decreased cellular energy status (Batandier et al. 2006) and activation of AMPK (AMPK-activated protein kinase) which has been shown to be associated with decreased mTOR activation resulting in inhibition of protein synthesis and proliferation (Dowling et al. 2007) as the cell reverts to an energy-saving state. Other intracellular signalling kinases may be involved in the anticancer effect of metformin (Vazquez-Martin et al. 2011; Liu et al. 2011; Soares et al. 2013; Wurth et al. 2013; Queiroz et al. 2014; Li et al. 2014; Buac et al. 2013) in some cases independently of AMPK, e.g., it has been shown (Zhu et al. 2014) that metformin inhibits the PI3K/Akt/mTOR pathway in HER2- and EGFR-overexpressing cells by interfering with, e.g., HER2/insulin-like growth factor (IGF)-1R receptor interactions. Metformin has also been shown to inhibit Akt in MCF7 (Queiroz et al. 2014) and glioblastoma (Wurth et al. 2013) cells and ERK in MCF7 (Queiroz et al. 2014). However, other studies have demonstrated increased activation of Akt in MDA-MB-231 breast cancer cells (Buac et al. 2013) and ERK in immortalised keratinocytes (Li et al. 2014). Taken together, these findings suggest that the effects of metformin on the Akt and MAPK pathways are context related.
We have recently shown that the Akt pathway plays an important role in influencing [18F]FDG incorporation (Fleming et al. 2014). However, the relationship between Akt (PKB) activation and [18F]FDG incorporation is likely to be modulated by drugs that influence several intracellular signalling pathways. Metformin is a safe compound (with only minor gut-related side effects) which is administered to T2D patients over long periods. However, as an anticancer drug, metformin is likely to be administered as an adjuvant with established chemotherapy agents, which in breast cancer include the anthracycline doxorubicin and in the case of HER2-overexpressing breast cancer, the humanised anti-HER2 antibody, trastuzumab. Both of these drugs can induce cardiomyopathy (Slamon et al. 2001), so early detection of response to these drugs is imperative. The most sensitive, non-invasive technique for monitoring chemotherapy response is [18F]FDG–PET (Mghanga et al. 2013) with response generally accompanied by decreased incorporation of [18F]FDG, but metformin can increase [18F]FDG (Habibollahi et al. 2013) incorporation possibly interfering with the changes in [18F]FDG incorporation induced by conventional treatments, effects that have so far not been examined.
With so many clinical trials underway, it is important to establish how metformin might modify the effect of the more aggressive anticancer drugs on [18F]FDG if PET is to be utilised in their clinical response assessment. In this study, the effect of metformin alone and combined with trastuzumab (or cetuximab) on pAMPK, pPKB and pERK1/2 expression in four breast cancer cell lines, three of which overexpress HER2 (Fleming et al. 2014) and one HER1, was characterised. The effect of combined treatment with doxorubicin, trastuzumab (or cetuximab) and metformin on [18F]FDG incorporation was then examined. Apoptosis is often activated by anticancer treatment and can influence glucose metabolism (Aide et al. 2009). As this study used a variety of anticancer treatments, the level of activation of caspase 3/7, an early event in apoptosis, was determined during treatment.
Materials and methods
Materials and chemicals
[18F]FDG was prepared by the Aberdeen PET centre at the University of Aberdeen. All chemicals were obtained from Sigma-Aldrich (Poole, UK) unless otherwise stated.
Cell culture
Cells were maintained in Dulbeccos Modified Eagle’s medium (Gibco, Life Technologies Ltd., UK) supplemented with 10 % foetal bovine serum (Gibco) and penicillin (100µ/ml)/streptomycin (100 µg/ml). Cells were grown until confluent in 75-cm2 tissue culture flasks, and individual experimental flasks (25 cm2) were seeded from trypsinised flasks prior to experiments.
Cytotoxicity
The growth-inhibitory effect of metformin on each cell line was determined using the MTT ((3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazonium Bromide) assay as described previously (Fleming et al. 2014). Cells were plated into 96-well pates at a seeding density of 50 × 103 cells/ml (MDA-MB-453, MDA-MB468 and SKBr3) or 75 × 103 cells/ml (BT474; 0.1 ml per well). They were left overnight at 37 °C in a CO2 incubator and then treated with a range of doses of metformin (1–20 mM) for 72 h. In combination studies, the clinically relevant dose of 200 nM [based on plasma levels of patients receiving doxorubicin (Kontny et al. 2013)] with and without trastuzumab (5 µg/ml)/cetuximab (5 µg/ml; Cheyne et al. 2011) and/or metformin (10 mM) for 72 h was used.
Western blotting
MDA-MB-453, BT474, MDA-MB-468 and SKBr3 cells were seeded at 0.5 × 106 cells/60 mm plate and grown for 3 days. Cells were exposed to metformin (10 mM), in the presence or absence of trastuzumab/cetuximab (5 µg/ml), for 24 h. Western blots were performed as described previously (Fleming et al. 2014; Smith et al. 2013). Antibodies were sourced from cell signalling (pAMPK, AKT, phospho-Ser473 AKT, p44/42 ERK1/2, phospho-Thr202/Tyr204 p44/42 ERK1/2), Insight Biotechnology (AMPK) and Sigma (actin). W. blotting was carried out at least three times using independent samples, and representative blots are shown.
Caspase 3 and 7 activation
Cells were plated into dark-walled 96-well plates (Sigma-Aldrich, UK) at a density of 150 × 103 cells/ml (0.1 ml per well) and treated with drugs as for the MTT assay. After 24 or 48 h, cells were lysed by addition of 25 µl of lysis buffer consisting of 4-(2-hydroxyethyl)-1-piperazineethanesulphonic acid (HEPES; 10 mM), phenylmethylsulphonyl fluoride (PMSF; 1 mM), 3-[(3-cholamidopropyl) dimethylammonio]-1-propanesulphonate (CHAPS; 5 mM), ethylene-diamine-tetra-acetic acid (EDTA; 2 mM) and β-mercaptoethanol (5 mM). After 30 min on ice, 125 µl of assay buffer was added consisting of HEPES (20 mM), EDTA (2 mM), and the cleavage substrate of caspase 3 and 7, Ac-DEVD-AMC (20 mM) and the cells left at 37 °C for 4 h. Fluorescence was determined in a fluorescence microplate reader FLx800TBI (BioTek) with excitation/emission wavelengths of 360/460 nm.
[18F]FDG incorporation
[18F]FDG incorporation by cells was measured after different treatments. 25-cm2 tissue culture flasks were seeded with MDA-MB-453, MDA-MB-468, BT474 or SKBr3 cells (106 cells per flask) in 5 ml of medium and allowed to incubate for 24 h at 37 °C. Media was then removed and the cells treated by addition of media containing metformin (usually 10 mM), trastuzumab (5 ug/ml)/cetuximab (10 ug/ml), doxorubicin (usually 200 nM) or combinations of these drugs for 4 h, 24 h or 72 h. The media was then replaced with 1 ml of medium containing [18F]FDG was administered to each flask. Incubation was continued for 20 min after which the medium was removed from the flasks and the cells washed 5× with warm PBS (5 ml) over a 5-min period to facilitate washout of non-metabolised tracer (to simulate the conditions of PET scans). The cells were then detached by addition of 0.5 ml of trypsin (0.05 %)/EDTA (0.2 %) and neutralised with 0.5 ml of medium. The cell suspension was recovered into microfuge tubes and incorporated [18F]FDG measured using a well counter with a Nuclear Instruments (Oakland, UK) interface until >1,000 counts accumulated. The cells were then pelleted by centrifugation at 200g for 5 min, washed once with PBS and the pellet resuspended in 100 μl of NaOH (1 M) and left overnight at 37 °C. After neutralisation with 100 μl of HCl (1 M), a protein assay was carried out on the dissolved tissue using a BCA kit (Sigma-Aldrich, UK). The [18F]FDG incorporation was then normalised by dividing by the protein value.
[3H]-o-methylglucose (OMG) uptake assay
O-methylglucose is transported by glucose transporters but not metabolised. Its initial rate of uptake is a measure of glucose transport. Here, uptake is measured over a period of 5 s at which time we have previously shown its uptake is still increasing with time in the cell lines used in this study (Fleming et al. 2014; Cheyne et al. 2011), so uptake at 5 s is a measure of glucose transport rate. Flasks (25 cm2) were seeded with cells and treated in quadruplicate as described for [18F]FDG incorporation experiments. Media was removed from cells, and the assay started by adding 1 ml of DMEM containing [3H]-OMG (37KBq/ml) at 37 °C. After exposure of the cells to [3H]-OMG for 5s, 5 ml of ice-cold PBS containing (200 µM) phloretin was immediately added to the flasks and decanted. Three further rapid washes were carried out, prior to cell detachment by trypsinisation and transfer to scintillation vials containing 5 ml of Ultima Gold scintillation fluid (Perkin-Elmer, UK). Cellular [3H] uptake was determined on a Packard (UK) Tri-Carb 2100TR scintillation counter. Radioactive counts were normalised to protein content determined on the cell suspension.
[18F] FDG phosphorylation
To determine the rate of phosphorylation of [18F]FDG in intact cells, cells incubated with and without metformin for 4 h were exposed to [18F]FDG in 1 ml medium for 10 s or 1 min and then washed 6× rapidly with ice-cold PBS. One millilitre of PBS was added, and the cells incubated for 2 min at 37 °C to facilitate efflux of non-phosphorylated [18F]FDG. PBS was then removed and placed in a microfuge tube for radioactive counting. Cells were trypsinised and placed in another microfuge tube for radioactive counting. To check that the procedure gave a true measure of % phosphorylated [18F]FDG, MDA-MB-453 cells were incubated with [18F]FDG for 1 min, washed 6× with ice-cold PBS and the cells immediately treated with 0.5 ml of NaOH (1 M) and left for 3 h at 37 °C. The NaOH-digested cells were then neutralised with 0.5 ml HCl (1 M) and divided into two 0.5 ml samples. To one sample was added 0.2 ml of 0.3 M Ba(OH)2 and 0.2 ml of 5 % w/v ZnSO4 to precipitate phosphate (so [18F]FDG-phosphate) and the precipitate pelleted down by centrifuging at 12,000g for 5 min. [18F] activity was measured in 100 µl of the supernatant and compared with activity in 100 µl of the non-treated sample. The phosphorylated [18F]FDG is the difference between the total (non-treated sample) and the supernatant (Kletzien and Perdue 1974). This procedure gave the same value of % [18F]FDG-phosphate in cells incubated with [18F]FDG for 1 min as the efflux method.
Lysate and mitochondrial preparation and hexokinase activity
Cells treated with metformin (10 mM) were lysed, and the lysate fractionated into cytoplasmic and mitochondrial fractions using a mitochondrial isolation kit following the manufacturer’s instructions (Sigma-Aldrich, Poole, UK). Total hexokinase was determined on the cell lysate after a slow centrifugation (600g) to remove cell debris. Hexokinase activity was determined as previously described (Cheyne et al. 2011).
Results
Figure 1a shows the effect of increasing concentrations of metformin on the growth of each cell line. A dose of 10 mM metformin decreased growth of MDA-MB-453 and MDA-MB-468 cells to about 40 % of control, but the growth of BT474 and SKBr3 cells was only decreased to about 60 % of control.
a Growth-inhibitory effect of metformin on breast cancer cell lines BT474 (diamonds), MDA-MB-453 (squares), SKBr3 (triangles) and MDA-MB-468 (circles). b Growth of untreated cells (white) and treated with trastuzumab (BT474, MDA-MB-453 and SKBr3 cells) or cetuximab (MDA-MB-468 cells; black) metformin (10 mM; chequed) and or in combination (diagonal lines) on the growth of breast cancer cell lines
Figure 1b shows the effect of metformin and trastuzumab/cetuximab on the growth of four breast cancer cells overexpressing HER2 (BT474, SKBr3 and MDA453) or HER1 (MDA468). Trastuzumab decreased cell growth by about 30 % in each of the HER2-overexpressing tumour cells whilst cetuximab decreased MDA-MB-468 cell growth by 14 %. The growth-inhibitory effect on BT474 cells of combined metformin and trastuzumab was significantly (metformin + trastuzumab vs trastuzumab t = 4.4, p < 0.01; metformin + trastuzumab vs metformin t = 22, p < 0.001) greater than either treatment alone. Inclusion of metformin with trastuzumab on SKBr3 (t = 7.74, p < 0.001) or MDA453 (t = 7.59, p < 0.001) cells or of metformin with cetuximab on MDA468 (t = 15.2, p < 0.001) cells increased the growth-inhibitory effect. However, conversely, the effect of metformin on the growth of these three cell lines was not enhanced by inclusion of trastuzumab or cetuximab.
Western blotting established that AMPK and pAMPK are present in normal growth conditions in all four cell lines (Fig. 2). Metformin increased pAMPK levels in all four cell lines, with the greatest increases observed in MDA453 and BT474 cells. Whilst pAMPK expression is not affected by cetuximab/trastuzumab in any cell line, combination treatment caused a clear enhancement of the metformin effect in BT474 cells, and a modest increase in MDA468 cells. As expected (Normanno et al. 2002), PKB (Akt) phosphorylation is sensitive to trastuzumab and cetuximab treatment, but metformin only decreases Akt phosphorylation in MDA468 cells and in BT474, MDA-MB-453 and SKBr3 the combination of metformin and trastuzumab appears to counter the effect of trastuzumab alone. ERK phosphorylation is only affected by cetuximab treatment of MDA-MB-468 cells or metformin treatment of MDA453 cells.
Representative Western blot demonstrating changes in protein expression of total and phospho-AMPK, Akt and ERK1/2 in lysates of control cells (lane 1), or cells treated with metformin (lane 2; 10 mM), trastuzumab (5 µg/ml)/cetuximab (10 µg/ml) (lane3) or both metformin and/or trastuzumab (5 µg/ml)/cetuximab (10 µg/ml) (lane 4). Result is representative of three independent experiments
Figure 3a shows the growth-inhibitory effect of combining metformin and/or trastuzumab (or cetuximab) with a clinically relevant dose (Kontny et al. 2013) of doxorubicin 200 nM (as this dose only inhibited the growth of BT474 cells by a few % (results not shown), these cells were treated with a dose of 500 nM (within the clinically relevant dose range)). Doxorubicin inhibited cell growth to 50 % of untreated cells (t = 15.8, p < 0.001). Addition of trastuzumab decreased growth to 39 % (compared with doxorubicin alone: t = 2.14, ns) of control whilst the combination of metformin with trastuzumab decreased growth rate to 27 % of control which was significantly greater than doxorubicin alone (t = 4.1, p < 0.01). Doxorubicin (200 nM) treatment of MDA453 cells decreased cell growth to 60 % of control (t = 4.58, p < 0.05). Inhibition of growth of MDA453 cells was enhanced by addition of trastuzumab (t = 8.6, p < 0.001) or metformin (t = 3.59, p < 0.05), but the combination did not produce a significantly greater inhibition of cell growth compared with either doxorubicin and trastuzumab or doxorubicin and metformin.
a Growth-inhibitory effect of 200 µM doxorubicin (for BT474 cells 500 µM) doxorubicin alone (white) or with trastuzumab/cetuximab (black), metformin (chequed) or with both metformin and trastuzumab/cetuximab (diagonals). b Caspase 3/7 activation in control (diamond) by 200 µM doxorubicin (for BT474 cells 500 µM) alone (white) or with trastuzumab/cetuximab (black), metformin (chequed) or with both metformin and trastuzumab/cetuximab (diagonals) treatments
Figure 3b shows the effect of doxorubicin with and without metformin and trastuzumab or cetuximab on caspase 3/7 activity. In common with other studies on breast cancer cell lines, metformin did not induce activation of caspase 3/7 (Zordoky et al. 2014). Doxorubicin increases caspase 3/7 activity in SKBr3 cells and to a lesser extent in MDA468 cells. Interestingly, these cell lines are more sensitive to doxorubicin than are BT474 or MDA-MB-453 cells in which caspase 3/7 activity is not increased by doxorubicin. Neither metformin nor trastuzumab or cetuximab increases caspase 3/7 expression, suggesting that they do not induce apoptosis in these cell lines. Similar results were seen after 48-h drug treatment (results not shown).
[18F]FDG incorporation was determined in cells treated for 4 h as this is when direct effects from intracellular signalling pathway modulation are likely to be observed prior to other changes related to cell death or decreased proliferation. Trastuzumab also affects intracellular signalling pathways (Fleming et al. 2014), so was included in combination with metformin at this time point. Twenty-four and 72-h treatments included doxorubicin, and the results shown in Fig. 4 (and statistical significance of changes shown in Table 1). [18F]FDG incorporation was decreased by MDA-MB-468 cells treated with cetuximab and BT474 and MDA-MB-453 cells treated with trastuzumab as previously reported (Fleming et al. 2014) corresponding with decreased expression of pAkt. Metformin increased [18F]FDG incorporation at all times in each cell line except MDA-MB-468 cells at 24 h.
[18F]FDG incorporation by control cells or by cells treated for a 4 h with trastuzumab/cetuximab, metformin, trastuzumab/cetuximab and metformin b 24 h with trastuzumab/cetuximab, metformin, trastuzumab/cetuximab and metformin, doxorubicin, doxorubicin and metformin c 72 h with trastuzumab/cetuximab, metformin, trastuzumab/cetuximab and metformin, doxorubicin, doxorubicin and metformin. (control: dark blue; red: trastuzumab or cetuximab; green: metformin; purple: metformin + trastuzumab or cetuximab; light blue: doxorubicin; orange: doxorubicin + metformin)
The treatment of cells for 4 h with trastuzumab/cetuximab and metformin significantly decreased [18F]FDG incorporation compared with metformin alone in BT474, MDA-MB-453 cells and MDA-MB-468 cells, an effect still apparent in the latter two cell lines at 24 h. The effect of doxorubicin on [18F]FDG incorporation was most apparent at 72 h decreasing [18F]FDG uptake in BT474 and MDA-MB-468 cells and increasing it by MDA-MB-453 cells. However, in all four cell lines, the combination of doxorubicin with metformin for 72 h further increased [18F]FDG incorporation when compared to metformin alone.
[18F]FDG incorporation was also measured after 11-day treatment with lower doses of metformin in BT474 cells (Fig. 5). Incorporation was found to be increased even after treatment with the 5 µM metformin after 11 days, suggesting that chronic exposure to low-dose metformin can also induce increased [18F]FDG incorporation and remain increased for long periods.
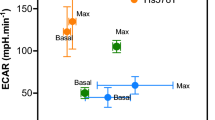
To explore how metformin treatment increases [18F]FDG incorporation, glucose transport and hexokinase activity were measured in each cell line after treatment with metformin. Glucose transport was determined by measuring the initial rate of uptake of the non-metabolised glucose analogue, [3H]OMG, by control and metformin-treated cells. Treatment with metformin increased glucose transport by BT474 cells, but decreased it in MDA-MB-468 and SKBr3 cells (Fig. 6a). Total hexokinase activity was found to be unchanged in lysates from each cell line that had been treated with metformin (results not shown). In two cell lines, the distribution of hexokinase activity in cytoplasm and mitochondria was determined and found to be unchanged by treatment of cells with metformin [BT cells: control 22 % (±2) and metformin treated 24 % (±5) and in MDA-MB-453 cells: control 31 % (±4) and metformin treated 31 % (±10)]. Metformin effects may only be apparent in intact cells (El-Mir et al. 2000), so to measure phosphorylation rate in intact cells, the level of phosphorylated [18F]FDG in control and metformin-treated cells incubated with [18F]FDG for short times was determined (Fig. 6b, c) and found to be significantly higher in metformin-treated cells than in control cells, suggesting that [18F]FDG phosphorylation is occurring more rapidly in metformin-treated cells.
a Glucose transport by breast cancer cell lines untreated (white) and treated with metformin (black). b, c Phosphorylated FDG in control (white) and metformin-treated cells (black) incubated with [18F]FDG medium for 10 s (b) and 1 min (c) then washed rapidly 5× with ice-cold PBS containing o-methylglucose to block the glucose transporters. They were then incubated with 1 ml of PBS at 37 °C for 5 min to release non-phosphorylated [18F]FDG from the cells (statistically significant change compared with control at *p < 0.05 or **p < 0.01 level)
Discussion
In common with other studies (Thompson 2014), AMPK activation was found to be enhanced in each cell line after treatment with metformin whilst the level of activated Akt and ERK were each only changed in one cell line. The mechanism of increased AMPK activation has been suggested to be due to inhibition of mitochondrial respiration inducing a cellular energy crisis and the resulting decrease in ATP levels activating AMPK (Guigas et al. 2014). Phosphorylation of Akt on Thr308 is increased by overexpression of HER, and metformin has been shown (Zhu et al. 2014) to decrease Akt activity by interfering with HER/IGF receptor interaction amongst other mechanisms (Ning and Clemmons 2010). Here, metformin decreased pAkt-Thr308 expression in MDA-MB-468 cells which overexpresses HER1, and this effect was increased by combining metformin with cetuximab. We have previously shown that decreased Akt activation can result in decreased [18F]FDG incorporation, an effect induced by trastuzumab. However, in BT474 and MDA-MB-453, metformin when combined with trastuzumab maintained pAkt levels, an effect which may partially explain the impact of metformin on [18F]FDG incorporation. The inhibitory effect of metformin on either pERK (MDA-MB-453) or pAkt (MDA-MB-468) which are survival pathways may be why these two cell lines are more sensitive to metformin than are BT474 or SKBr3 cells.
[18F]FDG uptake was increased in all four cells lines after 4-h treatment, but there was no relationship with sensitivity to metformin as BT474 and SKBr3 cells which were less sensitive to metformin than were MDA-MB-453 or MDA-MB468 cells showed similar increases. There was a sustained high [18F]FDG incorporation, at all time points, associated with metformin treatment of MDA-MB-453 and BT474 cells. Interestingly, these two cell lines show higher increases in pAMPK expression induced by metformin than do MDA-MB-468 and SKBr3 cells. At 24 h and 72 h, the higher uptake of [18F]FDG compared with was far less pronounced by SKBr3 and MDA-MB-468 cells than MDA-MB-453 and BT474 cells. The decreases in [18F]FDG incorporation by inclusion of anti-HER antibodies, compared with metformin alone, though significant in BT474 and MDA-MB-453 cells are very small. Inclusion of doxorubicin does not generally decrease [18F]FDG incorporation compared with metformin treatment alone and in some cases especially at 72 h further increased [18F]FDG incorporation. This may be related to the effect of metformin on giant cells which are formed by treatment with doxorubicin (Sliwinska et al. 2009) and which were evident in our cells after 72-h doxorubicin treatment.
Habibollahi et al. (2013) also demonstrated increased [18F]FDG incorporation by human and mouse colorectal tumour cells after 24 h of incubation with metformin. [18F]FDG incorporation was carried out in RPMI 1640 medium which contains glucose. Marini et al. (2013) treated MDA-MB-231 cells with metformin for 24 and 48 h and demonstrated decreased [18F]FDG incorporation. However, in their experiments, [18F]FDG was incubated with cells in glucose-free PBS rather than medium containing a known concentration of glucose, typically 5 mM, so the transport and hexokinase activity would be operating outside their physiological and optimum operating conditions (Km of hexokinases I and II is in the mM range). Under the conditions used in our study, we found that metformin treatment of MDA-MB-231 cells for 24 h increased [18F]FDG incorporation by about 80 % (control 91,795 ± 5,110 cpm/mg protein to 158,113 ± 11281; p < 0.001).
Metformin only increased glucose transport in BT474 cells and decreased glucose transport in SKBr3 and MDA-MB-468 cells both of which demonstrate high levels of glucose transport, compared with MDA-MB-453 and BT474 cells, which are unlikely to be rate limiting (Fleming et al. 2014). Glucose transport was also found to be even higher by MDA-MB-468 cells (3,054 cpm/mg protein) than by SKBr3 cells (SKBr3 cells 2,393 cpm/mg protein). Total hexokinase activity was not increased in lysates from cells treated with metformin nor was the distribution of hexokinase activity between cytosol and mitochondria altered. However, glycolytic flux, which will modulate hexokinase activity, is influenced by the concentration of glycolytic intermediates, but this effect is lost when cells are lysed. Also protein effects from the modulation of membrane properties by metformin (Schafer 1976; Wiernsperger 1999) have been shown to be lost in non-intact cells (El-Mir et al. 2000). Using intact cells exposed to [18F]FDG, the percentage of phosphorylated [18F]FDG was significantly higher in each cell line after treatment with metformin. The more efficient phosphorylation of [18F]FDG in metformin-treated cells may reflect higher rates of membrane hexokinase activity due to modifications to the mitochondrial membrane environment or an increase in the glycolytic flux reducing product inhibition of hexokinase. Another possibility is that the rate of diffusion of [18F]FDG is faster in metformin-treated cells. It is known that plasma membrane properties affect the rate of diffusion of molecules within the adjacent cytosol (Swaminathan et al. 1996), and [18F]FDG may reach hexokinase in metformin-treated cells more rapidly.
In common with most laboratory-based work, this study used metformin doses in the low mM range for time periods of 4 h to several days as these doses produced appreciable growth inhibition within a practical experimental timeframe. Serum concentrations of subjects receiving metformin are up to tens of µM. However, metformin is administered to patients over long time periods and, due to its positive charge, accumulates in tissues, probably mitochondria, reaching concentrations several orders of magnitude greater than in serum, so cells in tissues may conceivably be exposed to mM concentrations of metformin (Owen et al. 2000). Otto et al. (2003) have shown that longer incubations of cells with low concentrations of metformin can induce similar cellular effects as higher doses over shorter time periods. We show that clinically relevant doses of metformin for periods of 11 days can induce increased [18F]FDG.
Conclusion
[18F]FDG incorporation by breast cancer cell lines overexpressing HER1 or HER2 was increased by treatment with metformin, and the increase at early time points did not correlate with relative sensitivity to metformin. Combinations with anticancer drugs typically used in the treatment of breast cancer modulated this increase by significant but small amounts. Increased [18F]FDG incorporation after metformin treatment most consistently corresponded with increased [18F]FDG phosphorylation but not with glucose transport.
References
Aide N, Poulain L, Briand M et al (2009) Early evaluation of the effects of chemotherapy with longitudinal FDG small-animal PET in human testicular cancer xenografts: early flare response does not reflect refractory disease. Eur J Nucl Med Imaging 36:396–405
Batandier C, Guigas B, Detaille D, El-Mir MY, Fontaine E, Rigoulet M, Leverve XM (2006) The ROS production induced by a reverse-electron flux at respiratory-chain complex 1 is hampered by metformin. J Bioenerg Biomembr 206(38):33–42
Bodmer M, Meier C, Krahenbuhl S, Jick SS, Meier CR (2010) Long-term metformin use is associated with decreased risk of breast cancer. Diabetes Care 33:1304–1308
Buac D, Kona FR, Seth AK, Dou QP (2013) Regulation of metformin response by breast cancer associated gene 2. Neoplasia 15:1379
Cheyne RW, Trembleau L, McLaughlin AC, Smith TAD (2011) Changes in 2-Fluoro-2-deoxy-d-glucose incorporation, hexokinase activity and lactate production by breast cancer cells responding to treatment with the anti-HER-2 antibody trastuzumab. Nucl Med Biol 38:339–346
clinicaltrials.gov. Accessed 20 Aug 2014
Dowling RJ, Zakikhani M, Fantus IG, Pollak M, Sonenberg N (2007) Metformin inhibits mammalian target of rapamycin-dependent translation initiation in breast cancer cells. Cancer Res 67:10804–10812
El-Mir MY, Nogueira V, Fontaine E, Averet N, Rigoulet M, Leverve X (2000) Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J Biol Chem 275:223–228
Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk cancer in diabetic patients. BMJ 330:1304–1305
Fleming IN, Andriu A, Smith TAD (2014) Early changes in [18F]FDG incorporation by breast cancer cells treated with trastuzumab in normoxic conditions: role of the Akt-pathway, glucose transport and HIF-1 alpha. Breast Cancer Res Treat 144:241–248
Guigas B, Detaille D, Chauvin C et al (2014) Metformin inhibits mitochondrial permeability transition and cell death: a pharmacological in vitro study. Biochem J 382:877–884
Habibollahi P, van den Berg NS, Kuruppu D, Loda M, Mahmood U (2013) Metformin-an adjunct antineoplastic therapy-divergently modulates tumor metabolism and proliferation, interfering with early response prediction by F-18-FDG PET imaging. J Nucl Med 54:252–258
Jalving M, Gietema JA, Lefrandt JD, de Jong S, Reyners AK, Gans RO, de Vries EG (2010) Metformin: taking away the candy for cancer? Eur J Cancer 46:2369–2380
Jiralerspong S, Palla SL, Giordano SH, Meric-Bernstam F, Liedtke C, Barnett CM et al (2009) Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol 27:3297–3302
Kletzien RF, Perdue JF (1974) Sugar transport in chick embryo fibroblasts. J Biol Chem 249:3366–3374
Kontny NE, Wurthwein G, Joachim B et al (2013) Population pharmacokinetics of doxorubicin: establishment of a NONMEM model for adults and children older than 3 years. Cancer Chemother Pharmacol 71:749–763
Li WN, Ma WY, Zhong H, Liu WB, Sun Q (2014) Metformin inhibits proliferation of human keratinocytes through a mechanism associated with activation of the MAPK signaling pathway. Exp Ther Med 7:389–392
Liu BL, Fan ZY, Edgerton SM, Yang XH, Lind SE, Thor AD (2011) Potent anti-proliferative effects of metformin on trastuzumab-resistant breast cancer cells via inhibition of ErbB2/IGF-1 receptor interactions. Cell Cycle 10:2959–2966
Marini C, Salani B, Massollo M et al (2013) Direct inhibition of hexokinase activity by metformin at least partially impairs glucose metabolism and tumor growth in experimental breast cancer. Cell Cycle 12:3490–3499
Mghanga FP, Lan XL, Bakari KH, Li CJ, Zhang YX (2013) Fluorine-18 fluorodeoxyglucose positron emission tomography-computed tomography in monitoring the response of breast cancer to neoadjuvant chemotherapy: a meta-analysis. Clin Cancer Res 13:271–279
Ning J, Clemmons DR (2010) AMP-activated protein kinase inhibits IGF-I signaling and protein synthesis in vascular smooth muscle cells via stimulation of insulin receptor substrate 1 S794 and tuberous sclerosis 2 S1345 phosphorylation. Mol Endocrinol 24:1218–1229
Normanno N, Campiglio M, De Luca A et al (2002) Cooperative inhibitory effect of ZD1839 (Iressa) in combination with trastuzumab (Herceptin) on human breast cancer cell growth. Ann Oncol 13:65–72
Otto M, Breinholt J, Westergaard N (2003) Metformin inhibits glycogen synthesis and gluconeogenesis in cultured rat hepatocytes. Diabetes Obes Metab 5:189–194
Owen MR, Doran E, Halestrap AP (2000) Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem J 348:607–614
Pollak M (2013) Potential applications for biguanides in oncology. J Clin Investig 123:3693–3700
Queiroz EAIF, Puukila S, Eichler R, Sampaio SC, Forsyth HL, Lees SJ, Barbosa AM, Dekker RFH, Fortes ZB, Khaper N (2014) Metformin induces apoptosis and cell cycle arrest mediated by oxidative stress, AMPK and FOXO3a in MCF-7 breast cancer cells. PLoS One 9:e98207
Schafer G (1976) Mechanism of action of hypoglycemia-producing biguanides—re-evaluation and a molecular theory. Biochem Pharmacol 25:2005–2014
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792
Sliwinska MA, Mosieniak G, Wolanin K, Babik A, Piwocka K, Magalska A, Szczepanowska J, Fronk J, Sikora E (2009) Induction of senescence with doxorubicin leads to increased genomic instability of HCT1 16 cells. Mech Ageing Dev 13:24–32
Smith TAD, Zanda M, Fleming IN (2013) Hypoxia stimulates 18F-Fluorodeoxyglucose uptake in breast cancer cells via hypoxia inducible factor-1 and AMP-activated protein kinase. Nucl Med Biol 40:858–864
Soares HP, Ni Y, Kisfalvi K, Sinnett-Smith J, Rozengurt E (2013) Different patterns of Akt and ERK feedback activation in response to rapamycin, active-Site mTOR inhibitors and metformin in pancreatic cancer cells. PLoS One 8:e57289
Swaminathan R, Bicknese S, Periasamy N, Verkman AS (1996) Cytoplasmic viscosity near the cell plasma membrane: translational diffusion of a small fluorescent solute measured by total internal reflection-fluorescence photobleaching recovery. Biophys J 71:1140–1151
Thompson AM (2014) Molecular pathways: preclinical models and clinical trials with metformin in breast cancer. Clin Cancer Res 20:2508–2515
Vazquez-Martin A, Oliveras-Ferraros C, Del Barco S, Martin-Castillo B, Menendez JA (2011) The anti-diabetic drug metformin suppresses selfrenewal and proliferation of trastuzumab-resistant tumor-initiating breast cancer stem cells. Breast Cancer Res Treat 126:355–364
Viollet B, Guigas B, Garcia NS, Leclerc J, Foretz M, Andreelli F (2012) Cellular and molecular mechanisms of metformin: an overview. Clin Sci 122:253–270
Wiernsperger NF (1999) Membrane physiology as a basis for the cellular effects of metformin in insulin resistance and diabetes. Diabetes Metab 25:110–163
Wurth R, Pattarozzi A, Gatti M, Bajetto A, Corsaro A, Parodi A, Sirito R, Massollo M, Marini C, Zona G, Fenoglio D, Sambuceti G, Filaci G, Daga A, Barbieri F, Florio T (2013) Metformin selectively affects human glioblastoma tumor-initiating cell viability: a role for metformin-induced inhibition of Akt. Cell Cycle 12:145–156
Zhu P, Davis M, Blackwelder AJ et al (2014) metformin selectively targets tumor-initiating cells in ErbB2-overexpressing breast cancer models. Cancer Prev Res 7:199–210
Zordoky BNM, Bark D, Soltys CL, Sung MM, Dyck JRB (2014) The anti-proliferative effect of metformin in triple-negative MDA-MB-231 breast cancer cells is highly dependent on glucose concentration: implications for cancer therapy and prevention. Biochim Biophys Acta 1840:1943–1957
Conflict of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooper, A.C., Fleming, I.N., Phyu, S.M. et al. Changes in [18F]Fluoro-2-deoxy-d-glucose incorporation induced by doxorubicin and anti-HER antibodies by breast cancer cells modulated by co-treatment with metformin and its effects on intracellular signalling. J Cancer Res Clin Oncol 141, 1523–1532 (2015). https://doi.org/10.1007/s00432-015-1909-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-015-1909-2