Abstract
This study aims to assess the role of methotrexate-related gene polymorphisms in children with acute lymphoblastic leukemia (ALL) during high-dose methotrexate (HD-MTX) therapy and to explore their effects on serum metabolites before and after HD-MTX treatment. The MTHFR 677C>T, MTHFR 1298A>C, ABCB1 3435C>T, and GSTP1 313A>G genotypes of 189 children with ALL who received chemotherapy with the CCCG-ALL-2020 regimen from January 2020 to April 2023 were analyzed, and toxic effects were reported according to the Common Terminology Criteria for Adverse Events (CTCAE, version 5.0). Fasting peripheral blood serum samples were collected from 27 children before and after HD-MTX treatment, and plasma metabolites were analyzed by liquid chromatography-tandem mass spectrometry (LC–MS). The results of univariate and multivariate analyses showed that MTHFR 677C>T and ABCB1 3435 C>T gene polymorphisms were associated with the delayed MTX clearance (P < 0.05) and lower platelet count after treatment in children with MTHFR 677 mutation compared with wild-type ones (P < 0.05), and pure mutations in ABCB1 3435 were associated with higher serum creatinine levels (P < 0.05). No significant association was identified between MTHFR 677C>T, MTHFR 1298A>C, ABCB1 3435 C>T, and GSTP1 313A>G genes and hepatotoxicity or nephrotoxicity (P > 0.05). However, the serum metabolomic analysis indicated that the presence of the MTHFR 677C > T gene polymorphism could potentially contribute to delayed MTX clearance by influencing L-phenylalanine metabolism, leading to the occurrence of related toxic side effects.
Conclusion: MTHFR 677C>T and ABCB1 3435 C>T predicted the risk of delayed MTX clearance during HD-MTX treatment in children with ALL. Serum L-phenylalanine levels were significantly elevated after HD-MTX treatment in children with the MTHFR 677C>T mutation gene.
Trial registration: This study was registered at the Chinese Clinical Trial Registry (registration number: ChiCTR2000035264; registration: 2020/08/05; https://www.chictr.org.cn/).
What is Known: • MTX-related genes play an important role in MTX pharmacokinetics and toxicity, but results from different studies are inconsistent and the mechanisms involved are not clear. | |
What is New: • Characteristics, prognosis, polymorphisms of MTX-related genes, and metabolite changes were comprehensively evaluated in children treated with HD-MTX chemotherapy. • Analysis revealed that both heterozygous and pure mutations in MTHFR 677C>T resulted in a significantly increased risk of delayed MTX clearance, and that L-phenylalanine has the potential to serve as a predictive marker for the metabolic effects of the MTHFR 677C>T polymorphism. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphoblastic leukemia (ALL) is one of the most common childhood malignancies, characterized by the abnormal proliferation of lymphoblasts. Over the years, advancements in combination chemotherapy regimens have significantly improved the prognosis for children with ALL. The survival rate has remarkably increased from less than 10% in the 1960s to more than 90% in the present era [1, 2]. There are three main phases of treatment for ALL: induction, consolidation, and maintenance [3]. Among them, high-dose methotrexate (HD-MTX) has proven to be an effective therapy for managing extramedullary infiltration and systemic consolidation in children with ALL. The utilization of HD-MTX has shown promising results in improving the long-term survival rate of children with ALL [4].
In recent decades, improvements in MTX treatment and dosing regimens have led to significant improvements in the survival rates of patients with ALL. Nonetheless, the mucosal toxicity, hematotoxicity, and hepatotoxicity produced by high-dose MTX in children undergoing HD-MTX treatment may lead to serious complications and even interruption of treatment [5, 6]. CCCG-ALL-2020 is a prospective, randomized, and multicenter study conducted by the Chinese Pediatric Oncology Group. In this chemotherapy regimen of HD-MTX treatment, MTX-related toxicity and delayed clearance occurred in a large proportion of children despite dose adjustment during treatment based on creatinine clearance (CCR) and MTX concentrations at 44 h (C44h) after the child’s first HD-MTX chemotherapy [5]. MTX-related toxicity in patients is influenced by various factors, including the dose and duration of treatment as well as genetic factors [7, 8]. A growing number of studies suggested that MTX-related genes play an important role in MTX pharmacokinetics and toxicities, while the results are unidentical across studies, which may be related to factors such as the ethnicity of the study population, sample size, and chemotherapy dose [9,10,11]. The available studies do not provide clear evidence of a link between delayed early clearance of MTX and toxicity. Nevertheless, genetic polymorphisms of MTX-related genes may be potential predictors of personalized HD-MTX therapy.
Metabolomics is a valuable approach for investigating biochemical processes associated with metabolites. Given that metabolites can be easily detected in accessible biofluids, metabolomics has been extensively utilized for cancer diagnosis and prediction of adverse effects caused by anticancer drugs [12], such as lung cancer [13], breast cancer [14], and lymphoma [15]. In ALL, significant alterations in metabolite profiles have been found in pre- and post-induction and consolidation therapy [16]. The effects of MTX-related genes, contributing to patient-related toxicity and delayed clearance, on serum metabolites were further investigated through combined metabolomics and gene polymorphism analysis.
In the present study, the effects of MTHFR 677C>T, MTHFR 1298A>C, ABCB1 3435 C>T, and GSTP1 313A>G gene polymorphisms on MTX-related toxicity and delayed MTX clearance during HD-MTX treatment were analyzed in 189 children with ALL. The potential metabolic pathways affected by genes influencing delayed MTX clearance and toxicity were explored by examining changes in associated plasma metabolites before and after HD-MTX treatment.
Methods
Patients
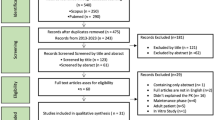
This study included 189 patients who were hospitalized at Qilu Hospital of Shandong University (Jinan, China) from January 2020 to April 2023. All patients included in the study were diagnosed with ALL and fulfilled the inclusion criteria of the CCCG-ALL-2020 protocol, receiving treatment accordingly. All patients were tested for MTHFR 677C>T, MTHFR 1298A>C, ABCB1 3435C>T, and GSTP1 313A>G polymorphisms by PCR-microarray hybridization prior to initiating HD-MTX chemotherapy. Patients who died or discontinued treatment prior to HD-MTX chemotherapy were excluded. From the eligible patients, a random selection of 27 individuals was made, and serum samples were collected before and after HD-MTX chemotherapy for metabolomic analysis. Informed consent was obtained from patients’ legal guardians, and the study was approved by the Ethics Committee of Shandong University Qilu Hospital (Approval No. ChiCTR2000035264). Detailed HD-MTX-specific data can be found in the supplementary materials. Detailed HD-MTX-specific programs can be found in the supplementary materials.
Data collection and definition
Patients’ demographic data, immunophenotype, MTX-related genes, risk stratification, HD-MTX chemotherapy details, and follow-up data were extracted from electronic medical records. The chemotherapy details for HD-MTX included the administered dose of MTX, C20h, C44h, and C68h and relevant tests, such as neutrophil count (NEU), glutamic-pyruvic transaminase (ALT), glutamic oxalacetic transaminase (AST), and creatinine (Cr) during HD-MTX. Delayed clearance of MTX was defined as MTX concentration at C44h > 1.0 µmol/L or at C68h ≥ 0.2 µmol/L during any HD-MTX chemotherapy session. Other toxic effects were reported according to the Common Terminology Criteria for Adverse Events (CTCAE, version 5.0) [17].
Serum sample collection and metabolite extraction and processing
Fasting peripheral blood serum samples were collected before HDMTX treatment (day 1) and after HDMTX treatment (day 3). Samples were collected in EDTA tubes. The samples were thawed and vortexed for 30 s. For tissue homogenate preparation, the samples were gradually added to H2O and homogenized. Cells were added to water and sonicated for 10 min at 4 °C. In the case of metabolites, sample volumes of 200 µL were extracted using MeOH to ACN (1:1, v/v). The samples were then vortexed for 30 s and sonicated for 10 min. To precipitate proteins, the samples were incubated at − 20 °C for 1 h, followed by a 15-min centrifugation at 20,000 g and 4 °C. The resulting supernatant was discarded, and the remaining solution was evaporated to dryness in a vacuum concentrator. The dry extracts were reconstituted in ACN to H2O (1:1, v/v) at a ratio of 40 µL per milligram of protein. The reconstituted extracts were vortexed for 30 s and sonicated for 10 min. After centrifugation for 15 min at 20,000 rpm and 4 °C to remove insoluble debris, the supernatants were transferred to HPLC vials and stored at − 80 °C until liquid chromatography-tandem mass spectrometry (LC–MS) analysis.
Data analysis
Unconditional logistic regression was employed to calculate odds ratios (OR) and 95% confidence intervals (95% CI) for the incidence of delayed clearance and hematotoxicity following HD-MTX treatment. The Shapiro–Wilk test was employed to assess the normal distribution of methotrexate plasma concentration and other indicators related to hematology, liver function, and kidney function. For normally distributed data, one-way analysis of variance (ANOVA) was utilized to compare the differences between groups. For abnormally distributed data, the Kruskal–Wallis test was employed. A relevant trend was considered for P-value < 0.1, while P-value < 0.05 was considered statistically significant. SPSS 26.0 software (IBM, Armonk, NY, USA) was utilized to carry out statistical analysis, and GraphPad Prism 9.0 software (GraphPad Software Inc., San Diego, CA, USA) was used for image rendering, unless otherwise specified.
Results
Patients’ clinical characteristics
Table 1 summarizes patients’ characteristics. The study group consisted of 189 children with a median age of 6.7 (interquartile range, 3.7–9.4) years old. The risk classification of ALL was based on factors, such as age, leukocyte count, immunophenotype, central nervous system status, karyotype analysis, molecular status, and end induction minimal residual disease (MRD) level. Among patients, 89 (44.4%) were classified as standard risk, while 100 (55.6%) were classified as intermediate or high-risk. Fasting plasma samples were collected from 27 newly diagnosed children at two time points: (1) on the day before HD-MTX treatment and (2) after completion of HD-MTX treatment, specifically on day 3 of chemotherapy. The dose of MTX administered varied based on patients’ risk level, with the low-risk group receiving 3 g/m2 and the intermediate- or high-risk group receiving 5 g/m2 of MTX chemotherapy. The MTX-related genotypes of the children included in the study were analyzed, and all genotypes were found to be consistent with Hardy–Weinberg equilibrium.
Association of MTX-related gene polymorphisms with delayed MTX clearance and C44h
As depicted in Fig. 1, the MTHFR 677CT/TT genotype exhibited a higher likelihood of delayed clearance compared with the wild-type (OR = 3.056/3.456, P = 0.019/0.009). In the ABCB1 3435C>T gene, homozygous mutations were more prone to exhibit delayed MTX clearance compared with the wild-type (OR = 2.82, P = 0.042), whereas no significant difference was noted in genotypes with heterozygous mutations. Similarly, in the C44h study, higher MTX concentrations were found in children with the MTHFR 677CT/TT genotype (P = 0.007/0.017). However, no significant differences were identified in MTHFR 1298A>C and GSTP1 313A>G genes regarding MTX clearance delay. Notably, children with pure mutations in the MTHFR1298 gene displayed lower C44h levels, possibly due to the smaller sample size of this genotype in the present study (Fig. 2).
To exclude the effects of confounding factors, multifactorial analysis was performed using logistic regression models for the four gene polymorphisms (Fig. 3), with the MTHFR 677TT genotype having a higher risk of delayed MTX clearance compared with wild-type children (OR = 2.841, P = 0.045) and the ABCB1 3435C>T pure mutation having a higher chance of delayed clearance compared with the heterozygous mutation (OR = 3.136, P = 0.036).
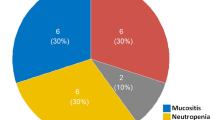
Association of MTX-related gene polymorphisms with side effects of HDMTX treatment
MTX-related toxicities, including myelosuppression, hepatotoxicity, and nephrotoxicity were evaluated during HD-MTX treatment in 188 children with ALL, as illustrated in Fig. 4. Children with the MTHFR 677 mutation exhibited lower platelet levels after treatment compared with the wild-type (CC vs CT+TT, P = 0.044), and those with a pure mutation in ABCB1 3435 showed higher serum creatinine levels (P = 0.016). However, no significant differences were identified between genotypes in the analysis of transaminases and other indicators.
Notably, when renal damage was evaluated as dichotomous variables, no significant effect of MTX-related gene polymorphisms was found, indicating that the elevated serum Cr levels caused by mutations in these genes are not sufficient to cause pathological changes in patients but still need to be brought to the attention of clinicians. Unlike the results of single-factor analysis, children with the MTHFR1298A>C heterozygous mutation were found to have a higher likelihood of developing myelosuppression (P = 0.049). However, this association was not observed in patients with the pure mutation, which could be attributed to the small number of children with the pure mutation included in the study (Fig. 5).
MTX-related genes could affect serum metabolite changes before and after HD-MTX treatment
A random selection of 27 children was made for the metabolomic analysis of peripheral blood serum before and after HD-MTX treatment (Table 2). The results revealed a significant increase in serum L-phenylalanine level in children with the MTHFR677 CT/TT mutation after treatment, whereas no similar alteration was found in other genotypes (Fig. 6).
Discussion
The survival rate of children with ALL has reached a high level; however, the long-term combination chemotherapy is accompanied by significant toxic side effects that can remarkably impact the quality of life. Therefore, there is a need to predict chemotherapy-related toxic effects prior to treatment and make timely adjustments to the chemotherapy dosage [18]. HD-MTX plays a crucial role in the treatment and prevention of extramedullary leukemia, while it may also lead to significant toxic reactions that should not be overlooked. The occurrence and severity of MTX-related toxicity may be influenced by various factors, including the dosage and duration of treatment and genetic factors [19]. Among them, genetic factors may be involved in the activities of MTX-associated enzymes, which may affect the metabolism and intracellular transport of the drug, thereby inducing the associated toxicity [20]. In the present study, the potential impact of MTX-related gene polymorphisms on MTX-related toxicity and clearance delay during HD-MTX treatment was analyzed in 189 Chinese children with ALL. Additionally, the serum metabolomics impact underlying the toxic reactions, and clearance delay associated with MTX-related gene polymorphisms was explored through metabolomics analysis.
Methylenetetrahydrofolate reductase (MTHFR) is a folate-dependent enzyme that plays an important role in the conversion of homocysteine (Hcy) to methionine [21]. To date, several polymorphic sites have been reported in the MTHFR gene, with the most extensively studied SNP sites being primarily 677C>T (rs1801133) and 1298A>C (rs1801131). The substitution of C>T at MTHFR rs1801133 could result in an alanine to valine change, enhancing the enzyme’s thermogenicity and disrupting flavin adenine dinucleotide (FAD) binding, thereby reducing catalytic activity [22], and this missense mutation could result in approximately 70% and 35% reduction in normal MTHFR enzymatic activity in TT and CT genotype carriers, respectively [23]. In addition, the A>C substitution at MTHFR rs1801131 could lead to the substitution of glutamate with alanine in the regulatory binding domain of the enzyme. This alteration could reduce the binding affinity of the enzyme for S-adenosylmethionine (SAM) and subsequently result in the decreased enzymatic activity [24]. The findings of the present study revealed an association between the MTHFR 677C>T mutation and an elevated risk of delayed MTX clearance following HD-MTX treatment. These results are consistent with the findings reported by Imanishi et al. [25] and Mahmoud et al. [26]. There were also significant differences in C44h concentrations, so increasing the dose of calcium folinate rescue in children with MTHFR 677C >T mutation may help reduce the adverse reactions of HD-MTX. However, no such change was found in the case of the 1298A>C mutation. Notably, when evaluating C44h as a continuous variable, it was revealed that children with the 1298A>C mutation gene had lower 44-h MTX blood concentrations. This observation could be attributed to the smaller number of children included in the study with the 1298A>C mutation. Conducting larger clinical studies can provide further insights into this relationship. Ilan S. Weisberg et al. showed that the 1298A>C mutation could affect the enzyme to a lesser extent than 677C>T [27], which could also be one of the possible reasons for the insignificant effect of 1298A>C on the delayed clearance of MTX. No significant correlation between MTHFR gene polymorphisms and MTX toxic response in patients was found in the most of studies [11], which is similar to the findings of the present study and may be due to the fact that MTX-related toxicity depends on a combination of factors, including folate status, dosing regimen, and dietary and environmental factors. This problem may be eliminated by establishing a complex multi-factor prediction model.
ABCB1 is a gene that encodes P-glycoprotein (P-gp) [28]. P-gp is an ATP-dependent membrane glycoprotein that transports intracellular xenobiotics to the extracellular compartment and acts as a pump for drug transport [29]. This gene plays an important role in the bioavailability of toxic substances and metabolites and prevents their intracellular accumulation. The ABCB1 3435C>T polymorphism (rs1045642) decreases the enzymatic activity of P-gp and reduces the number of carriers, leading to intracellular accumulation of drugs with associated toxic effects [30]. ABCB1 corresponds to a wide range of drug substrate actions that affects the toxic response of several antineoplastic drugs, such as carboplatin [31], cisplatin [32], MTX [33], fluorouracil [34], and adriamycin [35]. In the present study, children with ALL who were treated with HD-MTX were analyzed, and it was revealed that homozygous mutations in the ABCB1 3435C>T gene were more likely to have delayed MTX clearance compared with wild-type ones and had higher serum Cr levels compared with heterozygous mutations. Previous research reported that ABCB1 3435C>T could increase the risk of MTX-related toxicity [36]; however, the present study showed no significant increase in toxicity in patients with both pure and heterozygous mutant genotypes, which is in accordance with Melikoglu and Balkan’s findings [37]. This may be related to the ethnicity of the study population, MTX dosing regimen, etc. On the other hand, numerous studies confirmed that the P-gp was associated with other polymorphisms in the ABCB1 gene, such as ABCB1 1236C>T, 2677 G>T/A, and 1199G>A [38], so that simultaneous detection of multiple ABCB1 SNPs for multifactorial analysis will be necessary in the future studies.
Glutathione S-transferases (GST) are a group of multifunctional drug-metabolizing enzymes, of which GST Pi1 (GSTP1) is widely present in human tissues and is involved in cell repair and drug metabolism. This enzyme can bind to lipophilic cytotoxic drugs to enhance their water solubility and promote drug excretion [39]. The association between the GSTP1 genetic polymorphism (rs1695, 313A>G) and the toxic response to various chemotherapeutic agents has been extensively studied [40]. For instance, Woorim Kim et al. evaluated the relationship between the GSTP1 gene polymorphism and the toxicity of platinum-based chemotherapeutic agents and showed that the GSTP1 313A>G gene mutation was associated with a significant increase in gastrointestinal response and hematologic toxicity compared with wild-type mutations [41]. Similarly, Gong et al. found similar findings in their study of toxic reactions to cyclophosphamide chemotherapy, and their study also showed that patients with the GSTP1 313A>G gene mutation had an increased risk of infection when treated with cyclophosphamide [42], while MTX-related toxicity was less studied. The significance of GSTP1 313A>G polymorphism in HD-MTX treatment was investigated for the first time in the present study. However, no relevant effects of GSTP1 313A>G on MTX clearance delay and associated toxicity were found. This could potentially be attributed to the extensive hydration and alkalinization administered during HD-MTX, counteracting the adverse effects of GSTP1 genes. To further understand the exact role of GSTP1 in HD-MTX treatment, additional in vivo and in vitro experiments are warranted.
The changes in serum metabolites before and after HD-MTX treatment were studied in 27 ALL patients, and a combined analysis was conducted with MTX-related genes. The analysis revealed that patients with the MTHFR 677CT/TT genotype exhibited significantly higher serum L-phenylalanine levels after HD-MTX treatment, as well the increased risk of delayed MTX clearance and liver damage. However, no significant correlation was noted in relation to other genes. Amino acids play a crucial role in tumor growth, prognosis, and therapeutic response. They act as regulators of gene expression and are essential components in protein synthesis [43, 44]. In drug synthesis, the introduction of amino acids into natural products is one of the structural modification strategies to increase water solubility, enhance pharmacological activity, and reduce toxicity [45]. Schulpis et al. showed that in patients with the MTHFR 677C>T mutation and elevated blood levels of Hcy, there was an increase in the activity of cell membrane Na+-K+-ATPase. Furthermore, incubation with L-phenylalanine demonstrated a protective effect on the enzyme, preventing its activation [46], thereby reducing the occurrence of associated mucosal damage. Similarly, a study conducted by Heikal et al. indicated that L-phenylalanine intake improved vascular endothelial function in a mouse model of hypertension [47]. Elevated serum levels of L-phenylalanine were found in patients with the MTHFR 677CT/TT genotype after treatment. There was a tendency for delayed clearance of MTX and the increased risk of liver damage in these patients. This observation may be attributed to the effect of L-phenylalanine on cell membrane permeability, leading to the enhanced translocation of intracellular MTX to the extracellular compartment and resulting in higher concentrations of MTX in the serum. However, further validation through more robust in vivo and ex vivo experiments is necessary to confirm this finding. In order to mitigate the delayed clearance of MTX and associated toxic effects, it may be beneficial for patients to reduce their intake of L-phenylalanine-rich foods during HD-MTX treatment.
There are certain limitations to this study that need to be acknowledged. Firstly, a higher incidence of toxic reactions may not have been observed in patients with delayed MTX clearance because toxic responses were only assessed within 48 h of HD-MTX treatment. Future clinical studies with larger samples are needed to analyze and further assess the effect of delayed clearance on MTX long-term toxic responses. Secondly, for patients with relevant high-risk mutations, further intervention trials will be conducted to explore the feasibility of reducing delayed MTX clearance by increasing the folinic acid rescue dose early. In addition, the serum metabolomics of only 27 patients were randomly analyzed, which is a relatively small sample size, and the causal relationship between L-phenylalanine and delayed MTX clearance is unclear. Further animal experiments and large-sample clinical trials are needed to clarify the possibility of L-phenylalanine as an intervention target during HD-MTX therapy. Notwithstanding the aforementioned limitations, the study demonstrated a number of strengths. For the first time, the relationship between serum metabolite changes and delayed MTX clearance, as well as related gene polymorphisms, was analyzed before and after HD-MTX treatment in ALL patients. This provides a new idea to further investigate how to mitigate the toxic side effects in patients receiving HD-MTX chemotherapy.
Conclusions
In conclusion, the present study confirmed that both heterozygous and homozygous mutations in MTHFR 677C>T could lead to a significantly increased risk of delay in MTX clearance, and the results showed that L-phenylalanine has the potential to serve as a predictive marker for the metabolic effects of the MTHFR 677C>T polymorphism. Homozygous mutations of ABCB1 3435C>T also significantly increased the risk of delayed MTX clearance, while heterozygous mutations did not exhibit such effect, and the current evidence does not support the involvement of the GSTP1 313A>G gene in the reference value for HD-MTX treatment.
Data availability statement
The original data supporting the conclusions of this paper will be provided by the authors, where ethical requirements are met.
Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- ALT:
-
Glutamic-pyruvic transaminase
- AST:
-
Glutamic oxalacetic transaminase
- CCR:
-
Creatinine clearance
- Cr:
-
Creatinine
- GST:
-
Glutathione S-transferases
- Hcy:
-
Homocysteine
- HD-MTX :
-
High-dose methotrexate
- LC–MS :
-
Liquid chromatography-tandem mass spectrometry
- MTHFR:
-
Methylenetetrahydrofolate reductase
- MRD:
-
Minimal residual disease
- NEU:
-
Neutrophil count
- P-gp:
-
P-glycoprotein
References
Lavasidis G et al (2021) Therapeutic interventions for childhood cancer: an umbrella review of randomized evidence. Crit Rev Oncol Hematol 164:103414. https://doi.org/10.1016/j.critrevonc.2021.103414
Ivanov AV et al (2023)Pediatric acute lymphoblastic leukemia emerging therapies-from pathway to target. Int J Mol Sci 24. https://doi.org/10.3390/ijms24054661
Toksvang LN, Lee SHR, Yang JJ, Schmiegelow K (2022) Maintenance therapy for acute lymphoblastic leukemia: basic science and clinical translations. Leukemia 36:1749–1758. https://doi.org/10.1038/s41375-022-01591-4
Wu SY, Short NJ, Nasr L, Dabaja BS, Fang PQ (2022) Central nervous system prophylaxis and treatment in acute leukemias. Curr Treat Options Oncol 23:1829–1844. https://doi.org/10.1007/s11864-022-01032-5
Shen YQ et al (2022) Dose-individualization efficiently maintains sufficient exposure to methotrexate without additional toxicity in high-dose methotrexate regimens for pediatric acute lymphoblastic leukemia. Curr Med Sci 42:769–777. https://doi.org/10.1007/s11596-022-2589-1
Wight J et al (2022) Toxicity associated with high-dose intravenous methotrexate for hematological malignancies. Leuk Lymphoma 63:2375–2382. https://doi.org/10.1080/10428194.2022.2074987
Wu Z, Li Z, Qiu X, Zhong M, Ding T (2023) Germline genetic variations in methotrexate pathway are associated with pharmacokinetics, outcome, and toxicity in patients with primary central nervous system lymphoma. Expert Rev Clin Pharmacol 16:371–381. https://doi.org/10.1080/17512433.2023.2194630
Niinimäki R et al (2022) Reduced dose folinic acid rescue after rapid high-dose methotrexate clearance is not associated with increased toxicity in a pediatric cohort. Support Care Cancer 30:127–133. https://doi.org/10.1007/s00520-021-06395-3
Tan Y et al (2023) Relationship between methylenetetrahydrofolate reductase gene polymorphisms and methotrexate drug metabolism and toxicity. Transl Pediatr 12:31–45. https://doi.org/10.21037/tp-22-671
Ramalingam R et al (2022) Evaluation of cytogenetic and molecular markers with MTX-mediated toxicity in pediatric acute lymphoblastic leukemia patients. Cancer Chemother Pharmacol 89:393–400. https://doi.org/10.1007/s00280-022-04405-7
Song Z et al (2021) The role of genetic polymorphisms in high-dose methotrexate toxicity and response in hematological malignancies: a systematic review and meta-analysis. Front Pharmacol 12:757464. https://doi.org/10.3389/fphar.2021.757464
Danzi F et al (2023) To metabolomics and beyond: a technological portfolio to investigate cancer metabolism. Signal Transduct Target Ther 8:137. https://doi.org/10.1038/s41392-023-01380-0
Chen S et al (2023) Serum metabolomic profiles for distinguishing lung cancer from pulmonary tuberculosis: identification of rapid and noninvasive biomarker. J Infect Dis. https://doi.org/10.1093/infdis/jiad175
Rushing BR, Wiggs A, Molina S, Schroder M, Sumner S (2023) Metabolomics analysis reveals novel targets of chemosensitizing polyphenols and omega-3 polyunsaturated fatty acids in triple negative breast cancer cells. Int J Mol Sci 24. https://doi.org/10.3390/ijms24054406
Alfaifi A et al (2023) Metabolomics: a new era in the diagnosis or prognosis of B-cell non-Hodgkin’s lymphoma. Diagnostics (Basel) 13. https://doi.org/10.3390/diagnostics13050861
Fu J et al (2023) Metabolic profiling reveals metabolic features of consolidation therapy in pediatric acute lymphoblastic leukemia. Cancer Metab 11:2. https://doi.org/10.1186/s40170-023-00302-6
Reeve BB et al (2020) Validity and reliability of the pediatric patient-reported outcomes version of the common terminology criteria for adverse events. J Natl Cancer Inst 112:1143–1152. https://doi.org/10.1093/jnci/djaa016
Sadee W, Wang D, Hartmann K, Toland AE (2023) Pharmacogenomics: driving personalized medicine. Pharmacol Rev. https://doi.org/10.1124/pharmrev.122.000810
Hansson K et al (2021) Simultaneous determination of folate and methotrexate metabolites in serum by LC-MS/MS during high-dose methotrexate therapy. J Chromatogr B Analyt Technol Biomed Life Sci 1186:123007. https://doi.org/10.1016/j.jchromb.2021.123007
Zhang W et al (2021) MTHFR Polymorphism is associated with severe methotrexate-induced toxicity in osteosarcoma treatment. Front Oncol 11:781386. https://doi.org/10.3389/fonc.2021.781386
Yang B et al (2017) Geographical and ethnic distribution of MTHFR gene polymorphisms and their associations with diseases among Chinese population. Clin Genet 92:243–258. https://doi.org/10.1111/cge.12929
Rozen R (1996) Molecular genetics of methylenetetrahydrofolate reductase deficiency. J Inherit Metab Dis 19:589–594. https://doi.org/10.1007/bf01799831
Castro R et al (2004) 5,10-methylenetetrahydrofolate reductase (MTHFR) 677C-->T and 1298A-->C mutations are associated with DNA hypomethylation. J Med Genet 41:454–458. https://doi.org/10.1136/jmg.2003.017244
Froese DS et al (2018) Structural basis for the regulation of human 5,10-methylenetetrahydrofolate reductase by phosphorylation and S-adenosylmethionine inhibition. Nat Commun 9:2261. https://doi.org/10.1038/s41467-018-04735-2
Imanishi H et al (2007) Genetic polymorphisms associated with adverse events and elimination of methotrexate in childhood acute lymphoblastic leukemia and malignant lymphoma. J Hum Genet 52:166–171. https://doi.org/10.1007/s10038-006-0096-z
Mahmoud LB et al (2018) Use of MTHFR C677T polymorphism and plasma pharmacokinetics to predict methotrexate toxicity in patients with acute lymphoblastic leukemia. Adv Clin Exp Med 27:1061–1068. https://doi.org/10.17219/acem/69802
Weisberg IS et al (2001) The 1298A-->C polymorphism in methylenetetrahydrofolate reductase (MTHFR): in vitro expression and association with homocysteine. Atherosclerosis 156:409–415. https://doi.org/10.1016/s0021-9150(00)00671-7
Cheema Y, Kiani YS, Linton KJ, Jabeen I (2023) Identification and empiric evaluation of new inhibitors of the multidrug transporter P-glycoprotein (ABCB1). Int J Mol Sci 24. https://doi.org/10.3390/ijms24065298
Engle K, Kumar G (2022) Cancer multidrug-resistance reversal by ABCB1 inhibition: a recent update. Eur J Med Chem 239:114542. https://doi.org/10.1016/j.ejmech.2022.114542
Ibrahim MAA et al (2023) Potential drug candidates as P-glycoprotein inhibitors to reverse multidrug resistance in cancer: an in silico drug discovery study. J Biomol Struct Dyn 1–16. https://doi.org/10.1080/07391102.2023.2176360
Ferracini AC et al (2021) GSTP1 and ABCB1 polymorphisms predicting toxicities and clinical management on carboplatin and paclitaxel-based chemotherapy in ovarian cancer. Clin Transl Sci 14:720–728. https://doi.org/10.1111/cts.12937
Zheng Z et al (2023) SORL1 stabilizes ABCB1 to promote cisplatin resistance in ovarian cancer. Funct Integr Genomics 23:147. https://doi.org/10.1007/s10142-023-01075-3
Li M, Kong XY, Wang SM (2023) Effects of splicing-regulatory polymorphisms in ABCC2, ABCG2, and ABCB1 on methotrexate exposure in Chinese children with acute lymphoblastic leukemia. Cancer Chemother Pharmacol 91:77–87. https://doi.org/10.1007/s00280-022-04498-0
Nomura H et al (2020) ABCB1 and ABCC2 genetic polymorphism as risk factors for neutropenia in esophageal cancer patients treated with docetaxel, cisplatin, and 5-fluorouracil chemotherapy. Cancer Chemother Pharmacol 86:315–324. https://doi.org/10.1007/s00280-020-04118-9
Chen Z et al (2020) The lncRNA-GAS5/miR-221–3p/DKK2 axis modulates ABCB1-mediated adriamycin resistance of breast cancer via the Wnt/β-catenin signaling pathway. Mol Ther Nucleic Acids 19:1434–1448. https://doi.org/10.1016/j.omtn.2020.01.030
Plaza-Plaza JC et al (2012) Pharmacogenetic polymorphisms contributing to toxicity induced by methotrexate in the southern Spanish population with rheumatoid arthritis. Omics 16:589–595. https://doi.org/10.1089/omi.2011.0142
Melikoglu MA, Balkan E (2022) Can we predict unresponsiveness to methotrexate in rheumatoid arthritis? A pharmacogenetic study. Inflammopharmacology 30:193–197. https://doi.org/10.1007/s10787-021-00921-9
Megías-Vericat JE et al (2016) Positive impact of ABCB1 polymorphisms in overall survival and complete remission in acute myeloid leukemia: a systematic review and meta-analysis. Pharmacogenomics J 16:1–2. https://doi.org/10.1038/tpj.2015.79
Mazari AMA et al (2023) The multifaceted role of glutathione S-transferases in health and disease. Biomolecules 13. https://doi.org/10.3390/biom13040688
Cui J et al (2020) GSTP1 and cancer: expression, methylation, polymorphisms and signaling (Review). Int J Oncol 56:867–878. https://doi.org/10.3892/ijo.2020.4979
Kim W, Cho YA, Kim DC, Lee KE (2022) Association between genetic polymorphism of GSTP1 and toxicities in patients receiving platinum-based chemotherapy: a systematic review and meta-analysis. Pharmaceuticals (Basel) 15. https://doi.org/10.3390/ph15040439
Gong JY et al (2021) Evaluating the role of GSTP1 genetic polymorphism (rs1695, 313A>G) as a predictor in cyclophosphamide-induced toxicities. Medicine (Baltimore) 100:e24423. https://doi.org/10.1097/md.0000000000024423
Häusler RE, Ludewig F, Krueger S (2014) Amino acids--a life between metabolism and signaling. Plant Sci 229:225–237. https://doi.org/10.1016/j.plantsci.2014.09.011
Li X, Zhang HS (2023) Amino acid metabolism, redox balance and epigenetic regulation in cancer. FEBS J. https://doi.org/10.1111/febs.16803
Chen XH et al (2023) Transporter proteins knowledge graph construction and its application in drug development. Comput Struct Biotechnol J 21:2973–2984. https://doi.org/10.1016/j.csbj.2023.05.001
Schulpis KH et al (2006) Erythrocyte membrane Na+,K+-ATPase and Mg2+-ATPase activities in subjects with methylenetetrahydrofolate reductase (MTHFR) 677 C-->T genotype and moderate hyperhomocysteinaemia. The role of L-phenylalanine and L-alanine. Clin Chem Lab Med 44:423–427. https://doi.org/10.1515/cclm.2006.069
Heikal L et al (2018) l-phenylalanine restores vascular function in spontaneously hypertensive rats through activation of the GCH1-GFRP complex. JACC Basic Transl Sci 3:366–377. https://doi.org/10.1016/j.jacbts.2018.01.015
Funding
This work was supported by the Shandong Provincial Natural Science Foundation (ZR202010220039).
Author information
Authors and Affiliations
Contributions
Y. Z and H. H analyzed the results and wrote the manuscript. L. D, T. W, X. L and M. Z organized the data and revised the manuscript. A. Z and J. F conceived the topic and critically reviewed the manuscript. All the authors approved the manuscript for publication. #Y. Z and H. H contributed equally.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The study involving human participants was reviewed and approved by the Institutional Review Board of Qilu Hospital, Shandong University. Written informed consent was obtained from all participants or their parents.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhou, Y., He, H., Ding, L. et al. Effects of gene polymorphisms on delayed MTX clearance, toxicity, and metabolomic changes after HD-MTX treatment in children with acute lymphoblastic leukemia. Eur J Pediatr 183, 581–590 (2024). https://doi.org/10.1007/s00431-023-05267-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05267-8