Abstract
Antibiotics are among the most utilized drugs in pediatrics. Nonetheless, there is a lack in pharmacokinetics information for this population, and dosing criteria may vary between healthcare centers. Physiological variability associated with maturation in pediatrics makes it challenging to reach a consensus on adequate dosing, which is further accentuated in more vulnerable groups, such as critically ill or oncology patients. Model-informed precision dosing is a useful practice that allows dose optimization and attainment of antibiotic-specific pharmacokinetic/pharmacodynamic targets. The aim of this study was to evaluate the needs of model-informed precision dosing of antibiotics in a pediatrics unit, at a pilot scale. Pediatric patients under antibiotic treatment were monitored with either a pharmacokinetic/pharmacodynamic optimized sampling scheme or through opportunistic sampling. Clindamycin, fluconazole, linezolid, meropenem, metronidazole, piperacillin, and vancomycin plasma concentrations were quantified through a liquid chromatography coupled to mass spectrometry method. Pharmacokinetic parameters were estimated using a Bayesian approach to verify pharmacokinetic/pharmacodynamic target attainment. A total of 23 pediatric patients aged 2 to 16 years were included, and 43 dosing regimens were evaluated; 27 (63%) of them required adjustments as follows: 14 patients were underdosed, 4 were overdosed, and 9 patients needed infusion rate adjustments. Infusion rate adjustments were mostly recommended for piperacillin and meropenem; daily doses were augmented for vancomycin and metronidazole, meanwhile linezolid was adjusted for under- and overdosing. Clindamycin and fluconazole regimens were not adjusted at all.
Conclusion: Results showcase a lack of antibiotic pharmacokinetic/pharmacodynamic target attainment (particularly for linezolid, vancomycin, meropenem, and piperacillin), and the need for model-informed precision dosing in pediatrics. This study provides pharmacokinetic evidence which can further improve antibiotic dosing practices.
What is Known: • Model-informed precision dosing is performed in pediatrics to optimize the treatment of antimicrobial drugs such as vancomycin and aminoglycosides, while its usefulness is debated for other groups (beta-lactams, macrolides, etc.). | |
What is New: • Vulnerable pediatric subpopulations, such as critically ill or oncology patients, can benefit the most from model-informed precision dosing of antibiotics. • Model-informed precision dosing of linezolid, meropenem, piperacillin, and vancomycin is particularly useful in pediatrics, and further research may improve dosing practices altogether. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infectious diseases have been an important healthcare issue throughout history, and the discovery of antibiotics has aided medical professionals to combat them and reduce their mortality, especially in children. Despite all the knowledge and treatment options available today, combating such diseases may still be challenging for physicians because of antibiotic resistant microorganisms [1]. Community acquired, as well as nosocomial infections, may lead to serious medical complications, prolonging hospitalization days and putting patients’ lives at risk, particularly in vulnerable pediatric subpopulations, such as oncology, HIV, cystic fibrosis, or critically ill patients [2]. It is then no surprise that antibiotics are one of the most utilized drug groups in pediatrics, with some estimates showing that between 35 and 40% of hospitalized children receive antibiotic treatment [3].
Despite the frequent use of antibiotics, establishing dosing criteria for children can be challenging due to the large variability in the pharmacokinetics (PK) between age groups and difficulties when conducting pediatric PK studies. Pediatric patients are a largely heterogenous group, and as such, they are further divided into preterm and term neonates, infants, children, and adolescents. Besides the obvious differences in body size between age groups, organ maturation can drastically change drug absorption, distribution, metabolism, and excretion processes. Although most of the changes above occur within the first 2 years of life, some can reach full maturation until adolescence [4]. Therefore, PK studies need to be conducted for specific pediatric subpopulations, and this can prove to be challenging, as caregivers may be reluctant to consent participation in studies, often a limited number of blood samples can be drawn from patients, and they need to be stratified by age group, which increases the number of subjects needed for PK modelling. Because of these challenges, pediatric drug use usually starts as off label, and specialized PK studies are performed post-marketing [5, 6].
In spite of this, even when PK studies are performed, the resulting dosing schemes may differ from one healthcare center to another in different regions, which makes it difficult to reach a consensus on adequate dosing that can be generalized globally [7, 8]. Some approaches for dose optimization include (i) allometric scaling, which considers body weight as the main criteria to dose drugs but does not take into account developmental changes in physiology; (ii) physiologically based PK modelling, which does consider maturational changes, organ size, blood flow, and function and is often used during drug development to predict PK behavior before extrapolating drug use to special subpopulations; (iii) population PK (PopPK) modeling, which is able to describe PK in specific populations with clinical evidence, incorporating anthropometric, clinical, and physiological covariates in order to predict drug disposition and establish dosing regimens, with the aforementioned limitations for its application in pediatrics; and (iv) model-informed precision dosing (MIPD), in which information from PopPK models is combined with patients’ drug concentrations to predict individual PK through Bayesian forecasting, which can be used to design an optimized dosing scheme for each patient.
MIPD has an important role in precision dosing for a select number of drugs with variable PK, narrow therapeutic indexes, long treatment duration, or those without a clear efficacy biomarker. Regarding antibiotics, traditionally only those with well-known toxicity issues (such as vancomycin and aminoglycosides), have been candidates for MIPD, and quick immunoassays are readily available for drug quantification. Recently, the need for MIPD on other antibiotic groups has been explored [9], and highly sensitive and specific chromatographic methods have allowed the quantification of a wide array of compounds in low sample volumes [10]. While antibiotics like β-lactams have generally been considered safe, concentration-dependent toxicity has been described [11, 12], and there is growing concern on the consequences of subtherapeutic exposure, as this is one factor involved in the rise of antibiotic-resistant microorganisms. For this reason, therapeutic targets for antibiotics are defined with pharmacokinetic/pharmacodynamic (PK/PD) indexes involving PK parameters and microorganisms’ antibiotic susceptibility profiles, i.e., minimum inhibitory concentrations (MICs). For time-dependent antibiotics (β-lactams), the PK/PD target is the fraction of the dosing interval in which the unbound drug concentration remains above the MIC (fT > MIC). For concentration-dependent antibiotics, efficacy can be described either with the maximum concentration or area under the curve over the MIC (Cmax/MIC for aminoglycosides or AUC24h/MIC for glycopeptides, fluoroquinolones, linezolid, etc.).
The aim of this study was to evaluate the needs of MIPD of antibiotics in a pediatrics unit, through a pilot scale program.
Materials and methods
In order to assess the need of MIPD in the pediatrics unit at the hospital, seven antimicrobial drugs were selected based on prescription patterns indicated by the head of Pediatric Infectious Diseases (clindamycin, fluconazole, linezolid, meropenem, metronidazole, piperacillin, and vancomycin). Selected drugs were then quantified in plasma using a liquid chromatography method coupled to tandem mass spectrometry (LC-MS/MS), and Bayesian forecasting was used to interpret plasma concentrations.
Patient recruitment
A prospective, observational pilot study was performed at Hospital Central “Dr. Ignacio Morones Prieto” in collaboration with the Biopharmaceutics and Pharmacokinetics laboratory of the Universidad Autónoma de San Luis Potosí. Patients were included during the March–June 2022 period. Inclusion criteria were age from 2 to 17 years old receiving one or more of the previously listed antibiotics, informed consent from their parents and informed assent in patients 12 years or older. Patients were not included in the study if their caregivers withdrew consent or if hospital staff had difficulties drawing blood samples.
The following information was retrieved from the patients’ clinical records: Birth date and age (years), primary diagnostic, total body weight (TBW, kg), body surface (m2) and when available, clinical laboratory test results such as serum albumin (g/dL), creatinine (mg/dL), creatinine clearance (estimated with Schwartz's formula, mL/min/1.73m2) [13], red blood cells (106 cells/µL), white blood cells (103 cells/µL), platelets (103 cells/µL), hemoglobin (g/dL), hematocrit (v/v%), isolated microorganism, and antimicrobial susceptibility, among others.
Sampling schemes
Enrolled patients were monitored with either a sampling scheme based on PK/PD targets (Table 1) or through an opportunistic approach, utilizing routine morning laboratory test samples. Blood samples were drawn with 4 mL BD Vacutainer® or 0.5 mL BD Microtainer® tubes according to patient age and vein accessibility. Samples were centrifuged at 3 100 rpm or 11 000 rpm (for 4 mL and 0.5 mL tubes, respectively) for 15 min. Plasma was separated and stored at − 80 °C until analysis.
Bioanalytical methods
Materials and reagents
Antibiotic standards were purchased from Sigma-Aldrich (MO, USA): clindamycin hydrochloride, fluconazole, linezolid, meropenem, metronidazole, piperacillin sodium, and vancomycin hydrochloride. HPLC grade water, methanol, and acetonitrile (ACN) were purchased from TEDIA (OH, USA). Formic acid was purchased from EMD Millipore (NL, México).
Analyses were performed on a Class H Waters Acquity UPLC system (Waters Co. MA, USA) with a Quaternary Solvent Manager, a Flow Through Needle Sample Manager and a XEVO TQD mass spectrometer.
Sample preparation
Working solutions were prepared at a 50 µg/mL concentration (20 µg/mL for clindamycin) from 1 mg/mL stock solutions. Calibration curves (CC) and quality control samples (QCs) were prepared using separate working solutions.
Matrix blanks, CC standards, QCs, and patient samples were processed by mixing 100 µL of plasma with 100 µL of ACN and vortexing for 10 s. Samples were then centrifuged at 14,000 rpm/4 °C for 20 min to separate precipitated protein. Supernatant was then transferred to Eppendorf tubes and centrifuged twice at 14,000 rpm for 10 min. Finally, 50 µL of clear supernatant were transferred to glass vials and diluted with 350 µL of HPLC grade water. Processed samples were kept in the autosampler at 10 °C for 1 h before injection.
LC-MS/MS conditions
Chromatographic separation was performed on a Waters Acquity HSS-T3 column (2.1 × 100 mm, 1.7 µm) through gradient elution of ACN and a 0.1% formic acid aqueous solution (Online Resource 1). Mass spectrometry detection conditions are described in Online Resource 2. Data acquisition was performed with MassLynx v 4.0.
Method validation was performed in accordance with FDA guidelines [36]. Details on the method’s linearity, precision, and accuracy are reported in Online Resource 3.
Drug concentration interpretation
Bayesian forecasting was performed with Abbotbase Pharmacokinetics Systems (PKS) v 1.10. Table 1 shows PK/PD targets and toxicity thresholds chosen for each antibiotic. PopPK models for Bayesian estimation were selected from the literature based on the reported population characteristics (age range, disease-specific studies, etc.) and the covariates describing the PK. Patient’s drug concentrations were then fitted to each model. Fit was evaluated with a visual inspection of predicted PK profiles and observed concentrations and metrics such as sum of squares and number of iterations for Bayesian estimation. Models with the best performance in current population are reported in Table 1. AUC24h and fT > MIC were calculated from individual PK parameters and concentration profiles.
As β-lactam antibiotics require unbound drug concentrations to evaluate PK/PD target attainment, protein binding of 3% and 30% was assumed for meropenem and piperacillin, respectively [37]. For clindamycin, a protein binding of 60% was assumed if its use was prophylactic, and 88% in suspected or confirmed infections, considering that α1-acid glycoprotein (α1-agp) is an acute phase reactant, and its concentrations are known to increase during infections. Additionally, an α1-agp ontogeny function [38] coupled to protein binding estimates by Kays et al. [39] supported these assumptions.
When a microorganism was isolated and its susceptibility profile was known, MICs were taken from clinical records. If not available, epidemiological cut-off values (ECOFF) for suspected pathogens were taken from MIC distributions reported by the European Committee for Antimicrobial Susceptibility Testing (EUCAST) [40] (Table 2). Due to their toxicity threshold, maximum MICs of 2 and 1 mg/L were assumed for linezolid and vancomycin, respectively, even if the reported ECOFFs were higher.
Results
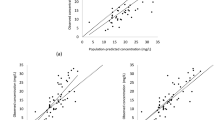
Baseline characteristics of the patients included in the current study are presented in Table 3. Although 23 patients were included, 8 patients were hospitalized several times with different antibiotic treatment and clinical profiles and thus were recorded as 32 independent MIPD events. Further, 10 patients received multiple antibiotics simultaneously, resulting in a total of 43 dosing regimens evaluated. PK/PD indexes estimated for each patient are shown on Fig. 1.
Summary of PK/PD parameters calculated for each antibiotic. Boxplots of individual PK/PD indexes: median and interquartile range, whiskers: 95% confidence intervals. Blue areas represent PK/PD target non-attainment, green areas represent therapeutic range, and red areas represent overexposure. Only individual observations are shown when n ≤ 3. Clindamycin MIC = 0.25 mg/L for Staphylococcus aureus. Fluconazole MIC = 2 mg/L covering Candida albicans, C. dubliniensis, C. tropicalis, and C. parapsilosis. Linezolid MIC = 2 mg/L (AUC was not estimated on one patient with low concentrations). Meropenem MIC = 2 mg/L for Pseudomonas aeruginosa. Metronidazole MIC = 8 mg/L for Bacteroides fragilis (AUC24h was not estimated on one patient with low concentrations). Piperacillin MIC = 16 mg/L for Pseudomonas aeruginosa (two overdosed patients are not shown in the boxplot as toxicity is not defined by fT > MIC). Vancomycin MIC = 1 mg/L (AUC was not estimated on one patient with low concentrations)
The most frequent cause of hospitalization for patients undergoing antimicrobial therapy was neutropenic fever on oncology patients, which is a medical emergency, as treatment with antineoplastic agents often leaves patients immunocompromised and suspected infections should be treated as soon as possible [41]. First-line antibiotics include cefepime, piperacillin/tazobactam, or meropenem for gram-negative microorganisms, vancomycin or linezolid for gram-positive bacteria, and fluconazole when suspecting fungal etiology [42]. The second most common diagnostic was acute appendicitis and appendicectomy post-operatory state, which is often treated with metronidazole and amikacin or ceftriaxone [25].
Adjustments were deemed necessary on 27 occasions: 23 due to subtherapeutic exposures and 4 of them due to overdosing. Results for each antibiotic are listed:
-
Clindamycin (n = 3) and fluconazole (n = 2): no dose adjustments were made.
-
Linezolid (n = 7): 3 patients were underdosed and 2 were overdosed.
-
Meropenem (n = 7): 4 patients did not reach target fT > MIC > 70% (2 were underdosed and 2 needed prolonged infusions).
-
Metronidazole (n = 5): 2 patients did not reach target AUC24h/MIC.
-
Piperacillin (n = 11): 7 patients did not reach target fT > MIC > 70% and needed prolonged infusions, while 2 patients were overexposed and daily dose was reduced by half.
-
Vancomycin (n = 8): Only one patient reached target AUC24h/MIC, the remaining 7 were underdosed.
Discussion
To understand antibiotic MIPD needs in the target population, it is essential to know common diagnostics and antibiotic usage. From prescription patterns alone, the proposed MIPD program seems to cover the most used antibiotics. Beyond prescription frequency, results expose a notable lack of PK/PD target attainment, which are discussed for each antibiotic.
First, clindamycin is often prescribed for less prevalent illnesses such as soft tissue and oral infections, with doses ranging from 20 to 40 mg/kg/day QID depending on the indication. No patients needed dose adjustments, although it is worth noting that clindamycin plasma concentration interpretation heavily depends on the unbound fraction estimation, since it has high and variable α1-agp binding percentages, which has a great effect on fC50ss (free mid concentration at steady state) estimation. Even if the previously mentioned strategy to estimate unbound drug concentrations from measured total drug concentrations is a well-founded approach, it is still an assumption. Therefore, free drug quantification may be necessary to interpret results more precisely.
Regarding fluconazole, the hospital’s standard dose of 6 mg/kg/day QD proved to be enough to attain an AUC24h/MIC of 50 for MICs up to 2 mg/L. Although no dose adjustments were deemed necessary given the most likely Candida species (Table 2) and clinical evolution of patients, it has been reported that 8 mg/L MICs should be targeted in pediatric oncology [16, 17], and monitored patients did not reach this higher target. Some authors argue that because of fluconazole’s low PK variability and toxicity, MIPD is not necessary if higher doses (up to 12 mg/kg/day) are used [43, 44]. However, more evidence is needed to verify this, since only two patients were monitored.
Linezolid results showcased its PK variability, as 30 mg/kg/day TID standard doses yielded a wide AUC24h range, from 78 to 658 mg*h/L, encompassing both overdosing and PK/PD target non-attainment. Such variability, combined with linezolid’s narrow therapeutic range of AUC24h between 100 (depending on the assumed MIC) and 280 mg*h/L [19,20,21], suggest it is a good candidate for MIPD.
Meropenem and piperacillin showed similar patterns, with most patients not achieving PK/PD targets with the initial dosing regimens (90 mg/kg/day TID for meropenem and 300 mg/kg/day QID for piperacillin). Recommendations often were to prolong infusion times up to 4 h, while these typically range from 30 to 90 min (depending on nursing staff criteria) and proved to be insufficient to achieve adequate fT > MIC. Extended or continuous infusions have been proposed as a useful strategy to maintain high β-lactam concentrations, especially given the short half-life of piperacillin and meropenem [45] (which is further accentuated by augmented renal clearance in pediatric oncology patients). Nonetheless, this approach is not always a viable option, particularly in pediatric patients with limited venous accesses and multiple intravenous drugs and parenteral liquid administration, as well as with antibiotics with notorious room temperature instability (such as meropenem). While it would be worthwhile to investigate whether prolonging infusion times as a standard practice would help most patients to achieve PK/PD targets, the need for β-lactam MIPD should not be discarded, especially since overdosage with piperacillin was observed on some patients, and in some cases, extended infusions without a dose increase may not be enough. The main obstacle to implement β-lactam MIPD worldwide is the lack of a consensus on the best PK/PD target [23]. Meropenem and piperacillin fT > MIC targets can be defined as 40 and 50%, respectively [28, 29, 46,47,48], although some studies state that higher exposures up to 70 and even 100% fT > MIC are needed to ensure clinical efficacy on vulnerable populations [23, 49, 50]. For this study, a fT > MIC > 40 – 50% target was selected for non-severe infections and fT > MIC > 70% in critically ill or immunocompromised patients, as it was considered a more feasible target than 100% fT > MIC, but the selection of a particular PK/PD target largely influences MIPD results interpretation.
Most patients undergoing treatment with metronidazole are those diagnosed with appendicitis and tend to recover from appendicectomies in less than 5 days without complications. Despite this, two patients with other diagnostics (such as intestinal transposition) and prolonged hospitalizations did not achieve the AUC24h/MIC target of 70 (assuming an 8 mg/L MIC) with the standard doses of 30 mg/kg/day TID. [25]. These results suggest that even if routine metronidazole MIPD may not be necessary for most patients, special cases may benefit from it if subtherapeutic exposures are suspected.
Finally, most patients under treatment with standard 40 mg/kg/day QID vancomycin doses did not achieve the target AUC24h/MIC of 400. While these standard dosing regimens at the hospital match some published recommendations of 40–60 mg/kg/day [33, 45], it has been shown that augmented renal clearance present in pediatric oncology or critically ill patients has a similar effect on vancomycin PK as it does with β-lactams. Therefore, higher doses up to 80 or 90 mg/kg/day have been proposed for special pediatric subpopulations [51, 52], which match dose adjustments derived from MIPD in the current study. Because these recommendations were so frequent, it might be necessary to validate new standard dosing schemes different from those currently in use at the hospital, although it will likely not eliminate the need for MIPD as toxicity will be a concern with higher doses [53].
In summary, results and patterns observed from each antibiotic allowed to prioritize MIPD needs in the pediatric population. First, meropenem, piperacillin, linezolid, and vancomycin needed most of the dose adjustments. Even if it might be debatable whether MIPD or redefining dosing and administration schemes is the better approach for β-lactams, the fact that these antibiotics are frequently prescribed in vulnerable pediatric subpopulations might justify monitoring drug concentrations to ensure PK/PD target attainment. MIPD of metronidazole might be important in selected patients who do not initially respond to treatment, though it may not be necessary in most cases. More fluconazole data is needed to properly assess the need for MIPD at the hospital, although it probably would not be a high priority given reported PK data and tolerability to higher doses. Finally, MIPD of clindamycin does not appear to be crucial, as it is often prescribed in non-critical patients, although unbound drug quantification might be necessary to verify this.
The main limitation of this study is its scale, as it is a single-center pilot study with a low sample size for each antibiotic. For this reason, external PopPK model validation could not be performed to select the most adequate model for Bayesian estimation, and fit to available models was evaluated on a case-by-case basis. Additionally, PK/PD target attainment was not verified after emitting dose recommendations. Nonetheless, this work showcases notable therapeutic target non-attainment with standard doses and describes antibiotic MIPD needs in pediatrics, providing valuable information which will serve to guide future antibiotic PK studies (PopPK modeling, external model validation, and proposal of new standard dosing regimens through stochastic simulations). Furthermore, the implemented MIPD program can still be refined, by adding antibiotics initially not considered, further reducing sample volumes, quantifying unbound drug concentrations, and exploring alternative biological matrices such as dried blood spots. This initial study included patients from 2 years of age or older, and the proposed modifications will facilitate expanding the target population to include neonates and infants which will likely show different PK behaviors and have different needs altogether.
Conclusion
This study provides important information regarding the need for MIPD of antibiotics in pediatrics, particularly linezolid, vancomycin, meropenem, and piperacillin. Results show a concerning lack of PK/PD target attainment in vulnerable pediatric populations, and individual treatment optimization through MIPD is a useful approach to reach therapeutic targets. This initial pilot approach also may serve as a starting point to further study local PK behavior and redefine standard pediatric dosing practices.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on request.
Abbreviations
- α1-agp:
-
α1-Acid glycoprotein
- AUC24h :
-
24-h area under de curve
- Cmax :
-
Maximum plasma concentration
- ECOFF:
-
Epidemiological cut-off
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- fC50ss :
-
Mid free drug concentration at steady state
- FDA:
-
Food and Drug Administration
- fT > MIC:
-
Fraction of dosing interval free drug concentration is above the minimum inhibitory concentration (%)
- HIV:
-
Human immunodeficiency virus
- HPLC:
-
High performance liquid chromatography
- LC:
-
Liquid chromatography
- MIC:
-
Minimum inhibitory concentration
- MIPD:
-
Model-informed precision dosing
- MS/MS:
-
Tandem mass spectrometry
- PD:
-
Pharmacodynamic/pharmacodynamics
- PK:
-
Pharmacokinetic/pharmacokinetics
- PopPK:
-
Population pharmacokinetics
- QD:
-
Once daily
- QID:
-
Four times a day
- TID:
-
Three times a day
- UPLC:
-
Ultra high performance liquid chromatography
References
Dadgostar P (2019) Antimicrobial resistance: implications and costs. Infect Drug Resist 12:3903–10. Available from: https://www.dovepress.com/antimicrobial-resistance-implications-and-costs-peer-reviewed-fulltext-article-IDR
de Moraes-Pinto MI, Ferrarini MAG (2020) Opportunistic infections in pediatrics: when to suspect and how to approach. Elsevier Editora Ltda [cited 2021 Feb 10]. Jornal de Pediatria 96:47–57. Available from: https://pubmed.ncbi.nlm.nih.gov/31790645/
Downes KJ, Hahn A, Wiles J et al (2013) Dose optimisation of antibiotics in children: application of pharmacokinetics/pharmacodynamics in paediatrics. Int J Antimicrob Agents. Available from: https://doi.org/10.1016/j.ijantimicag.2013.11.006
Le J, Bradley JS (2017) Optimizing antibiotic drug therapy in pediatrics: current state and future needs. J Clin Pharmacol 2018(58):S108–S122
Novak E, Allen PJ (2007) Prescribing medications in pediatrics: concerns regarding FDA approval and pharmacokinetics. Pediatr Nurs 33(1):64–70
Food and Drug Administration (2022) Population Pharmacokinetics. Guidance for Industry. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/population-pharmacokinetics
Rashed AN, Jackson C, Gastine S et al (2019) Pediatric pharmacokinetics of the antibiotics in the access and watch groups of the 2019 WHO model list of essential medicines for children: a systematic review. Expert Rev Clin Pharmacol 12(12):1099–106. Available from: https://doi.org/10.1080/17512433.2019.1693257
Hartman SJF, Brüggemann RJ, Orriëns L et al (2020) Pharmacokinetics and target attainment of antibiotics in critically Ill children: a systematic review of current literature. Vol. 59, Clinical Pharmacokinetics. Springer International Publishing pp. 173–205. Available from: https://doi.org/10.1007/s40262-019-00813-w
Reeves D, Lovering A, Thomson A (2016) Therapeutic drug monitoring in the past 40 years of the Journal of Antimicrobial Chemotherapy. J Antimicrob Chemother 71(12):3330–3332
Ates HC, Roberts JA, Lipman J et al (2020) On-site therapeutic drug monitoring. Trends Biotechnol. Available from: https://doi.org/10.1016/j.tibtech.2020.03.001
Imani S, Buscher H, Marriott D et al (2017) Too much of a good thing: a retrospective study of β-lactam concentration-toxicity relationships. J Antimicrob Chemother [cited 2021 May 20] 72(10):2891–7. Available from: https://academic.oup.com/jac/article/72/10/2891/3952632
Roger C, Louart B (2021) Beta-lactams toxicity in the intensive care unit: an underestimated collateral damage? Microorganism 9(7):1505. Available from: https://www.mdpi.com/2076-2607/9/7/1505/htm
Schwartz GJ, Haycock GB, Edelmann CM et al (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58(2):259–63. Available from: https://pubmed.ncbi.nlm.nih.gov/951142/
Smith MJ, Gonzalez D, Goldman JL et al (2017) Pharmacokinetics of clindamycin in obese and nonobese children. Antimicrob Agents Chemother 61(4). Available from: https://doi.org/10.1128/AAC.02014-16
Gonzalez D, Melloni C, Yogev R et al (2014) Use of opportunistic clinical data and a population pharmacokinetic model to support dosing of clindamycin for premature infants to adolescents. Clin Pharmacol Ther 96(4):429–37. Available from: https://doi.org/10.1038/clpt.2014.134
Autmizguine J, Guptill JT, Cohen-Wolkowiez M et al (2014) Pharmacokinetics and pharmacodynamics of antifungals in children: clinical implications. Vol. 74, Drugs. Springer International Publishing, p. 891–909
Van Der Elst KCM, Pereboom M, Van Den Heuvel ER et al (2014) Insufficient fluconazole exposure in pediatric cancer patients and the need for therapeutic drug monitoring in critically Ill children. Clin Infect Dis 59(11):1527–1533
Seay RE, Larson TA, Toscano JP et al (1995) Pharmacokinetics of fluconazole in immune-compromised children with leukemia or other hematologic disease. Pharmacother J Hum Pharmacol Drug Ther 15(1):52–58
Dou L, Meng D, Dong Y et al (2020) Dosage regimen and toxicity risk assessment of linezolid in sepsis patients. Int J Infect Dis 1(96):105–111
Alsultan A (2019) Determining therapeutic trough ranges for linezolid. Saudi Pharm J 27(8):1061–1063
Boak LM, Rayner CR, Grayson ML et al (2014) Clinical population pharmacokinetics and toxicodynamics of linezolid. Antimicrob Agents Chemother 58(4):2334–43. Available from: https://journals.asm.org/journal/aac
Garcia-Prats AJ, Schaaf HS, Draper HR et al (2019) Pharmacokinetics, optimal dosing, and safety of linezolid in children with multidrug-resistant tuberculosis: combined data from two prospective observational studies. PLOS Med 16(4):e1002789. Available from: https://doi.org/10.1371/journal.pmed.1002789
Dhaese S, Van Vooren S, Boelens J et al (2020) Therapeutic drug monitoring of β-lactam antibiotics in the ICUm, pp. 1155–64. Available from: https://doi.org/10.1080/14787210.2020.1788387
Hassan HE, Ivaturi V, Gobburu J et al (2020) Dosage regimens for meropenem in children with pseudomonas infections do not meet serum concentration targets. Clin Transl Sci 13(2):301–8. Available from: https://doi.org/10.1111/cts.12710
Child J, Chen X, Mistry RD et al (2019) Pharmacokinetic and pharmacodynamic properties of metronidazole in pediatric patients with acute appendicitis: a prospective study. J Pediatric Infect Dis Soc 8(4):297–302
Cohen-Wolkowiez M, Ouellet D, Smith PB et al (2012) Population pharmacokinetics of metronidazole evaluated using scavenged samples from preterm infants. Antimicrob Agents Chemother 56(4):1828–1837
Sprandel KA, Drusano GL, Hecht DW et al (2006) Population pharmacokinetic modeling and Monte Carlo simulation of varying doses of intravenous metronidazole. Diagn Microbiol Infect Dis 55(4):303–309
Thibault C, Lavigne J, Litalien C et al (2019) Population pharmacokinetics and safety of piperacillin-tazobactam extended infusions in infants and children. Antimicrob Agents Chemother 63(11):1-12. Available from: https://journals.asm.org/doi/10.1128/AAC.01260-19
Béranger A, Benaboud S, Urien S et al (2018) Piperacillin population pharmacokinetics and dosing regimen optimization in critically Ill children with normal and augmented renal clearance. Clin Pharmacokinet 58(2):223–33. Available from: https://doi.org/10.1007/s40262-018-0682-1
Thorsted A, Kristoffersson AN, Maarbjerg SF et al (2019) Population pharmacokinetics of piperacillin in febrile children receiving cancer chemotherapy: the impact of body weight and target on an optimal dosing regimen. J Antimicrob Chemother 74(10):2984–2993
Zhang T, Cheng H, Pan Z et al (2020) Desired vancomycin trough concentration to achieve an AUC0–24/MIC ≥400 in Chinese children with complicated infectious diseases. Basic Clin Pharmacol Toxicol 126(1):75–85. Available from: https://doi.org/10.1111/bcpt.13303
Le J, Ny P, Capparelli E et al (2015) Pharmacodynamic characteristics of nephrotoxicity associated with vancomycin use in children. J Pediatric Infect Dis Soc 4(4):e109–16. Available from: https://academic.oup.com/jpids/article/4/4/e109/2580148
Smit C, Goulooze SC, Brüggemann RJM et al (2021) Dosing recommendations for vancomycin in children and adolescents with varying levels of obesity and renal dysfunction: a population pharmacokinetic study in 1892 children aged 1–18 years. AAPS J 23(3):1–10. Available from: https://doi.org/10.1208/s12248-021-00577-x
Alsultan A, Abouelkheir M, Alqahtani S et al (2018) Optimizing vancomycin monitoring in pediatric patients. Pediatr Infect Dis J 37(9):880–5. Available from: https://journals.lww.com/pidj/Fulltext/2018/09000/Optimizing_Vancomycin_Monitoring_in_Pediatric.8.aspx
Santos Buelga D, Del Mar Fernandez De Gatta M, Herrera EV et al (2005) Population pharmacokinetic analysis of vancomycin in patients with hematological malignancies. Antimicrob Agents Chemother 49(12):4934–41. Available from: https://journals.asm.org/journal/aac
Food and Drug Administration (2018) Bioanalytical Method Validation. Guidance for Industry. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioanalytical-method-validation-guidance-industry
Patel BM, Paratz J, See NC et al (2012) Therapeutic drug monitoring of beta-lactam antibiotics in burns patients-a one-year prospective study. Ther Drug Monit 34(2):160–4. Available from: https://journals.lww.com/drug-monitoring/Fulltext/2012/04000/Therapeutic_Drug_Monitoring_of_Beta_Lactam.8.aspx
Maharaj AR, Gonzalez D, Cohen-Wolkowiez M et al (2018) Improving pediatric protein binding estimates: an evaluation of α1-acid glycoprotein maturation in healthy and infected subjects HHS Public Access. Clin Pharmacokinet 57(5):577–589
Kays MB, White RL, Gatti G et al (1992) Ex vivo protein binding of clindamycin in sera with normal and elevated α1-acid glycoprotein concentrations. Pharmacother J Hum Pharmacol Drug Ther 12(1):50–5. Available from: https://doi.org/10.1002/j.1875-9114.1992.tb02671.x
EUCAST. MIC Breakpoints. [cited 14 Apr 2021]. Available from: https://mic.eucast.org
Burns B, Hartenstein M, Lin A et al (2019) Optimizing time to antibiotic administration in children with possible febrile neutropenia through quality improvement methodologies. Pediatr Qual Saf 4(6):e236
White L, Ybarra M (2017) Neutropenic fever. Hematol Oncol Clin North Am 31(6):981–93. Available from: https://doi.org/10.1016/j.hoc.2017.08.004
Cohen-Wolkowiez M, Benjamin DK (2014) Fluconazole therapeutic drug monitoring in children with cancer: not today. Vol. 59, Clinical Infectious Diseases. Oxford University Press; p. 1534–6
Stockmann C, Constance JE, Roberts JK et al (2014) Pharmacokinetics and pharmacodynamics of antifungals in children and their clinical implications. Vol. 53, Clinical Pharmacokinetics. Springer International Publishing; p. 429–54
Costenaro P, Minotti C, Cuppini E et al (2020) Optimizing antibiotic treatment strategies for neonates and children: does implementing extended or prolonged infusion provide any advantage? Vol. 9, Antibiotics. MDPI AG; p. 1–20
Chongcharoenyanon T, Wacharachaisurapol N, Anugulruengkitt S et al (2021) Comparison of piperacillin plasma concentrations in a prospective randomised trial of extended infusion versus intermittent bolus of piperacillin/tazobactam in paediatric patients. Int J Infect Dis 1(108):102–108
Steffens NA, Zimmermann ES, Nichelle SM et al (2021) Meropenem use and therapeutic drug monitoring in clinical practice: a literature review. J Clin Pharm Ther 6(3):610–621. Available from: https://doi.org/10.1111/jcpt.13369
Germovsek E, Lutsar I, Kipper K et al (2018) Plasma and CSF pharmacokinetics of meropenem in neonates and young infants: results from the NeoMero studies. J Antimicrob Chemother 73(7):1908–16. Available from: https://academic.oup.com/jac/article/73/7/1908/4978317
Huttner A, Harbarth S, Hope WW et al (2015) Therapeutic drug monitoring of the β-lactam antibiotics: what is the evidence and which patients should we be using it for? J Antimicrob Chemother 70(12):3178–83. Available from: https://academic.oup.com/jac/article/70/12/3178/2363621
Scharf C, Paal M, Schroeder I et al (2020) Therapeutic drug monitoring of meropenem and piperacillin in critical illness—experience and recommendations from one year in routine clinical practice. Antibiotics 9(3):131. Available from: www.mdpi.com/journal/antibiotics
Guilhaumou R, Marsot A, Dupouey J et al (2016) Pediatric patients with solid or hematological tumor disease: vancomycin population pharmacokinetics and dosage optimization. Ther Drug Monit 38(5):559–66. Available from: https://pubmed.ncbi.nlm.nih.gov/27631462/
Zhao W, Zhang D, Fakhoury M et al (2014) Population pharmacokinetics and dosing optimization of vancomycin in children with malignant hematological disease. Antimicrob Agents Chemother 58(6):3191–9. Available from: https://journals.asm.org/journal/aac
Marsot A, Gallais F, Galambrun C et al (2018) Vancomycin in pediatric patients with solid or hematological malignant disease: predictive performance of a population pharmacokinetic model and new optimized dosing regimens. Paediatr Drug 20(4):375–81. Available from: https://pubmed.ncbi.nlm.nih.gov/29736878/
Acknowledgements
The authors would like to thank the residents and nurses of the Pediatrics division at Hospital Central “Dr Ignacio Morones Prieto” for their support during patient recruitment, as well as the patients and their family members who agreed to participate in the study.
Funding
The present study was supported by Mexico’s Office of Public Education through the government program: “Programa para el Desarrollo Profesional Docente, PRODEP” (511-6/2020-8585). A master’s fellowship was granted to Rodrigo Velarde-Salcedo by the Technological Research Council of Science (CONACyT) from Mexico (Grant 782280).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Rodrigo Velarde-Salcedo, Susanna Edith Medellín-Garibay, Silvia Romano-Moreno, Rosa del Carmen Milán Segovia, Luis Fernando Pérez-González, Francisco Javier Arriaga García, and Ana Socorro Rodríguez-Báez. The first draft of the manuscript was written by Rodrigo Velarde-Salcedo, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was carried out in line with ethical principles of the Declaration of Helsinki. Approval was granted by the Research and Ethics Committee of Hospital Central “Dr. Ignacio Morones Prieto,” SLP, México (Registration number 69-21; August 26th, 2021).
Consent to participate
Written informed consent was obtained from patients’ parents, and informed assent was obtained from patients over 12 years of age.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Velarde-Salcedo, R., Pérez-González, L.F., Rodríguez-Báez, A.S. et al. Model-informed precision dosing of antimicrobial drugs in pediatrics: experiences from a pilot scale program. Eur J Pediatr 182, 4143–4152 (2023). https://doi.org/10.1007/s00431-023-05103-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05103-z