Abstract
Upper respiratory tract infections (URTIs) are a condition characterized by upper airway inflammation often caused by viruses in humans. The present study aimed to assess the effectiveness of the liquid herbal drug preparation from the root extracts of Pelargonium sidoides in improving symptoms of uncomplicated URTIs. One hundred sixty-four patients with URTI were randomized and given either verum containing the root extracts of Pelargonium sidoides (n = 82) or a matching placebo (n = 82) in a single-blind manner for 7 days. The median total scores of all symptoms (TSS) showed a significant decreasing trend in the group treated with the root extracts derived from Pelargonium sidoides compared to the placebo group from day 0 to day 7 (TSS significantly decreased by 0.85 points in the root extract group compared to a decrease of 0.62 points, p = 0.018). “Cough frequency” showed a significant improvement from day 0 to day 3 (p = 0.023). There was also detected a significant recovery in “sneezing” on day 3 via Brunner-Langer model, and it was detected that the extract administration given in the first 24 h onset of the symptoms had provided a significant improvement in day 0 to day 3 (difference of TSS 0.18 point, p = 0.011).
Conclusion: The findings of the study revealed that the Pelargonium sidoides extracts are effective in relieving the symptom burden in the duration of the disease. It may be regarded as an alternative option for the management of URTIs.
What is Known: • Upper respiratory tract infections (URTIs), an inflammation on the upper airways, are the most common infectious disease in children. • Pelargonium sidoides, a traditional medicinal plant native to South Africa, is one of the ornamental geraniums that is thought to be effective in treating URTIs | |
What is New: • It may be revealed that the dried root extract of Pelargonium sidoides compared with placebo might be an alternative treatment in improving the symptoms such as dry cough, sneezing, and relieving cough frequency. • The administration of the root extract at the onset of URTIs’ signs may be regarded as an adjunctive option for the management of URTIs due to its effectiveness in decreasing the symptom burden of the disease. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Upper respiratory tract infections (URTIs) are among the most frequent infections around the world and might be defined as an inflammation on the upper airways that refer to the part of the respiratory system above the vocal cords, including nose, sinuses, pharynx, larynx, and large airways. The causative agents of URTIs are typically viruses that often cause a mild and self-limited disease. Upper respiratory tract infections are the leading cause of doctor visits and account for an estimated 10 million outpatient appointments resulting large economic burden in a year. It has also been reported that the URTIs are responsible for greater than 20 million missed days of school and work lost [1]. Preschool children often suffer from a URTI approximately 6 up to 12 times a year; those who attend daycare may have as many as 14 times, and the incidence gradually decreases with age [2].
In recent years, over-the-counter cold medications have been reported that they may be an effective treatment option to improve the symptoms of URTIs, one of which is Pelargonium sidoides root extract [3]. Pelargonium sidoides (African geranium) is a traditional medicinal plant native to South Africa. It is one of the ornamental geraniums of which roots extract have been thought to be effective in the treatment of several acute infections for centuries. The apparent effectiveness of the root extract derived from Pelargonium sidoides in the treatment of infections caused by several microorganisms has been associated with its constituents known as tannins such as gallic acid, gallocatechin, catechin, other polyphenols, and coumarins. Immune-modulatory activities of Pelargonium sidoides are mainly mediated through the release of tumor necrosis factor (TNF-alfa) and nitric oxides, the stimulation of interferon-gamma, and also the increase of natural killer cell activity [4, 5]. Due to the fact that there is no certain proof in distinguishing between bacterial and viral infections, the physicians usually prescribe antibiotics to avoid serious bacterial complications in daily practice. Therefore, there has been a high prevalence of preferring unnecessary antibiotics in URTIs [6]. The herbal liquid root extract of Pelargonium sidoides, occasionally prescribed by physicians in treating patients with acute respiratory tract infections, is a non-antibiotic alternative implementation. It has recently been shown that the use of the Pelargonium sidoides root extract and selected phytopharmaceuticals was provided to be effective in decreasing the antibiotic prescriptions in adults with acute respiratory infections in a retrospective study conducted by Martin et al. [7]. Another double-blind, placebo-controlled randomized trial published in early 2021 has reported that the root extract from Pelargonium sidoides might be an option to provide a reduction in antibiotic use in adults diagnosed with lower respiratory tract infection [8].
Although there has been declared that Pelargonium sidoides may be effective in alleviating symptoms in adults who suffered from acute rhinosinusitis and the common cold and has been reported that there was a relief for the symptoms of acute bronchitis in adults and children, the clinical effectiveness of Pelargonium sidoides in children with acute URTIs has not been clearly defined yet [3]. Thus, the placebo-controlled study was planned to evaluate the effectiveness of the Pelumm©—a solution derived from the dried root extract of Pelargonium sidoides—in relieving the symptoms associated with URTIs in children.
Materials and methods
Setting
The study was performed from January 2019 to January 2020 in the outpatient department of Ege University, Medical School, Children’s Hospital, Izmir, Turkey, as a randomized, single-blind, placebo-controlled, phase III clinical search, with 2 parallel treatment groups. The study was conducted according to Good Clinical Practice, the declaration of Helsinki Somerset West 1997 (World Medical Association Declaration of Helsinki, 1997), and legal regulations. Approvals of the Ethics Committee, Ministry of Health of Turkey [19-AKD-45], and the regulatory authorities were obtained before starting the study. During the enrolment period, the investigators registered all screened patients with symptoms of acute URTI.
The baseline characteristics of the subjects, study design, and medication
Male or female 164 (aged 1–18 years) patients who fulfilled the inclusion criteria (inclusion and exclusion criteria shown in Additional material-1) were evaluated, and it was taken a provision of written informed consent from parents for the study. After written informed consent, as part of the baseline data, investigators recorded the patient’s past medical history, baseline symptoms of the URTIs, and demographic data (age, sex, the symptoms, etc.) at the initial visit. All subjects had no past medical history and chronic illness. The individual duration of the study was 7 days. During this time, 4 visits were scheduled (day 0; day 3; day 5; day 7) and the investigator examined each patient to follow-up and for clinical evaluation during the first three visits, and the last visit (day 7) was fulfilled on the phone. A computer-aided random series program was used to generate the random allocation sequence, a list of unique integer random numbers identified as patient code. Following the randomization, the subjects were given verum containing a herbal drug preparation named Pelumm© ((Pelumm©; 1:8–10; dried, extraction solvent: ethanol 11% (w ⁄ w); 1 cc = 20 drops = 0.018468 g)—a solution derived from the dried root extract of Pelargonium sidoides (n = 82)—or placebo (n = 82) that was matched with respect to solvent composition, appearance, taste, viscosity, and color. Dosing of the study drug was 3 × 10 drops (patients 1–5 years old), 3 × 20 drops (patients 5–12 years old), or 3 × 30 drops (patients > 12 years old) of Pelumm© or placebo, at least 30 min before or after meals, from day 1 and continuing until day 7. In the case of fever (> 39 °C), paracetamol was allowed for the patients.
Total symptom score
The total symptom score (TSS) consisted of 13 symptoms considered to be associated with the URTI [9, 10]. (Patient evaluation form-Additional material-2).
Patient’s symptoms
The severity of the listed eight symptoms was scored according to the following system:
Fever (Axillary and/or tympanic, °C): 1 point ≤ 37; 2 point = 37–38; 3 point = 38–3; 4 point ≥ 39.
Malaise: 0 point = None; 1 point = Slight; 2 point = Moderate; 3 point = Pronounced; 4 point = Very pronounced; 5 point = Exceptionally severe.
Headache: 1 point = None; 2 point = Mild; 3 point = Moderate; 4 point = Severe; 5 point = Very severe.
Sneezing: 0 point = None; 1 point = Infrequent, mild; 2 point = More frequent, mild; 3 point = Moderate; 4 point = Pronounced, quite frequent; 5 point = Very pronounced and frequent.
Myalgia: 1 point = None; 2 point = Mild; 3 point = Moderate; 4 point = Pronounced; 5 point = Very Pronounced.
Rhinorrhea: 0 point = None; 1 point = Not so much; 2 point = Moderate; 3 point = Pronounced; 4 point = Very pronounced.
Sore throat: 0 point = None; 1 point = Mild; 2 point = Moderate; 3 point = Pronounced; 4 point = Very Pronounced; 5 point = Unbearable.
Feeling dry throat: 0 point = None; 1 point = Mild; 2 point = Moderate; 3 point = Pronounced; 4 point = Very Pronounced.
Purulent rhinorrhea, purulent eyes, frequent cough, dry cough, and purulent cough were evaluated as “the present” or “absent” and were scored; the “present”: 1 point; the “absent”: 0 points. Then, from the beginning to the seventh day, drops of the root extract of Pelargonium sidoides were investigated whether there was an influence to improve the symptoms of URTIs according to the value of the total mean symptom score (the mean symptom score value was found by dividing the total points to 13). Symptoms were assessed on baseline days (day 0), 3, 5, and 7 of the treatment period. At each of the follow-up visits, the investigator evaluated the patients for their clinical status, defined the adverse events, and examined whether there was a progression to the other diagnoses (Pneumonia, etc.).
Outcomes
The primary outcome criterion was to define whether there could be an improvement in the TSS from day 0 to day 7 in the patients given the liquid root extract from Pelargonium sidoides. Secondary outcome criteria for effectiveness were as follows: whether there could be a decrease in the severity and duration of the individual symptoms between visit intervals in the active treatment groups compared with the placebo group, and determination of whether it could be a benefit on the administration of the liquid herbal preparation derived from Pelargonium sidoides in the early stage of URTIs.
Statistical analysis
Regarding the variables and onset time of the treatment effectiveness in improving, descriptive and other statistical methods were used to compare the groups. Statistical analyses were performed using IBM SPSS version 21.0 for personal computers (Chicago, IL, USA). The Shapiro–Wilk test was used to check the normality assumption of the continuous variables. We used Fisher’s exact test, Pearson chi-square test, and Mc Nemar test for categorical data. In cases of non -normally distributed data, the Mann–Whitney U test was utilized, and the T-test was used in cases of normally distributed data to determine whether the difference between the two groups was statistically significant. A two-tailed probability value p < 0.05 was considered to be statistically significant.
In order to test the global effect of the factors group, time point, and group-time interaction, a repeated-measures analysis of variance was performed. Nonparametric Brunner and Langer model (F1-LD-F1) was used to testing group and dependent group effects by using web-based software (R software, version 3.5.2, package: nparLD, R Foundation for Statistical Computing, Vienna, Austria; http://r-project.org) [11]. The model was expected to answer the question as to what extent the difference in improvement between the treatment group and placebo group could affect the results in the repeated evaluation of patients by day. In the case of one additional factor, side time, a separate model was performed for each group. Then a Mann–Whitney U test was performed for each time point. Data were presented with the median and minimum–maximum or interquartile range (IQR). The test was performed only for the symptoms showing a statistically significant difference among groups in the Brunner and Langer model. All p values were corrected for multiple testing by Bonferroni-Holm adjustment. The level of significance was set at 0.05.
Results
Disposition of patients and baseline characteristics
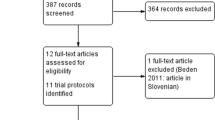
A total of 164 patients were included in screening and subsequently randomized to receive a solution, herbal preparation containing the dried root extract from Pelargonium sidoides (n = 82) or placebo (n = 82). Table 1 has shown the demographic data and baseline median symptom scores of the patients. The median age of the study group was 4.8 (5.2) years; 93 (56.7%) patients were male, and 71 (43.3%) were female. The demographic data showed no significant differences between the group treated with the herbal drug preparation from Pelargonium sidoides and the group treated with placebo. In addition, the baseline (day 0) median scores of the 13 symptoms were similar between the groups except for the fever. The median score of the fever was significantly higher in the placebo group than in the verum group.
Primary outcome measure: symptom scores
The total symptom scores of all available patients in both the treatment and placebo groups were shown in Table 2. No statistically significant differences between the individual total TSS of participants of the treatment group and the placebo group on baseline (day 0), day 3, and day 5 were found. However, comparing the median TSS within groups between day 0 and day 7, it was found that the median of TSS significantly decreased by 0.85 points in the root extract group compared to a decrease of 0.62 points in the placebo group (p = 0.018).
Secondary outcome measures: effectiveness of the solution derived from the dried root extract of Pelargonium sidoides in the individual symptoms, and administration time of the solution (Pelumm©)
According to the presence or absence of all symptoms among the visit day intervals, Table 3 has shown the improvement situation in each group. There was a relief in symptoms including “Fever,” “Malaise,” “Headache,” “Sneezing,” “Myalgia,” “Rhinorrhea,” “Sore throat,” and “Feeling dry throat” in both groups on all visit day intervals. It was also detected that there was no superiority of the verum for “purulent eyes” and “purulent cough.” However, “cough frequency” showed a statistically significant decrease in the Pelargonium sidoides group compared with the placebo on day 3 (p = 0.023). The item dry coughing the improvement at day 0–day 5 (p = 0.001) was more pronounced in the treatment group. The purulent rhinorrhea revealed a statistically significant decline in the Pelargonium sidoides group compared to the placebo on day 7 (p = 0.023).
In order to determine the significance of the scores change in eight symptoms, known as the Brunner and Langer model, a repeated measures analysis of variance was utilized to test the global effect group, time point, and interaction of the factors. According to the model, the interaction of variables was firstly evaluated, and it was found that the time-dependent progression in groups was similar for malaise, headache, myalgia, sore throat, and the feeling dry throat due to the fact that the interaction p values were not significant. The p values of the Group, Time, and Interaction from baseline day to 7th respectively; malaise: p = 0.888, p < 0.001, and p = 0.154; headache: p = 0.621, p < 0.001, and p = 0.694; myalgia: p = 0.383, p < 0.001, and p = 0.843; sore throat: p = 0.190, p < 0.001, and p = 0.748; and feeling dry throat: p = 0.175, p < 0.001, and p = 0.730. There were no treatment effects of verum on the five symptoms (Fig. 1).
However, it was detected a significant interaction (p < 0.10) via Brunner and Langer model in rhinorrhea, sneezing, and fever. The p values of the Group, Time, and Interaction from baseline day to 7th, respectively; sneezing: p = 0.377, p < 0.001, and p = 0.014; rhinorrhea: p = 0.954, p < 0.001, and p = 0.064; and fever: p = 0.001, p < 0.001, and p = 0.001. There was a significant recovery in “sneezing” on day 3 and in “fever” on day 5 (Table 4; Fig. 2) in the binary comparisons of each time point in the three symptoms, following Bonferroni-Holm correction. Although “Rhinorrhea” showed a significant “interaction,” there was no significant difference in visit day intervals between the two groups.
Differences of TSS in the visit days related to the onset time of the symptoms in both treatment and placebo have been evaluated, and concerning the onset time of the URTI symptoms (also the same time for administrations), the participants were divided into 3 groups. When analyzing the differences of TSS between the visit days for each drug start time among the groups; the liquid herbal drug that was given in the first 24 h after the onset of the symptoms has provided a statistically significant reduction in the symptoms scores of the treatment group compared to the placebo. Within 48–72 h after the onset of the symptoms, a reduction in TSS was found in Pelargonium sidoides group compared with placebo. The total score change values at the end of treatment indicated significantly greater improvement in the treatment group than the placebo group in day 0 to day 3 and in day 0 to day 7 (difference of TSS 0.18 and 0.17 point, p = 0.011; p = 0.023, respectively).
The overall effect size of a solution derived from the dried root extract of Pelargonium sidoides on difference symptom scores was also found to be high than the placebo on day 0–day 3 and day 0–day 7 days. The d values of the effect size indicated that the effect of a solution derived from the dried root extract of Pelargonium sidoides was Big-intermediate effect ((df = 85, t = 2.600, d = 0.56; p = 0.011; 95% CI 0.04033–0.30257) and (df = 69.492, t = 2.332, d = 0.56; p = 0.023; 95% CI 0.026659–0.31116)) (Effect size (d): \(2t /\surd df\)) [12].
Discussion
The results of this randomized, single-blind, placebo-controlled, single-center clinical study demonstrated the impact on decreasing the burden of the symptoms during URTIs in pediatric patients aged 1–18 years suffering from URTIs. The primary outcome parameter was that a significant superiority of Pelargoniım sidoides on reducing the median total symptom score from day 0 to day 7 in the active treatment group compared with the placebo group. The second outcome parameter, the administration of the solution derived from the dried root extract of Pelargonium sidoides (Pelumm©; a solution derived from the dried root extract of Pelargonium sidoides), was a favorable treatment compared with placebo for dry cough, sneezing, reducing the frequency of cough, and fever. Moreover, the early administration of the herbal drug preparation Pelargonium sidoides has been shown to relieve the symptoms and be an initiator in alleviating the symptoms.
Despite its high prevalence, however, there is no effective treatment of the virus originated URTIs in children. Due to the fact that the causative agents of these infections are often viruses, antibiotics are ineffective to treat, except for seconder bacterial infections and their severe complications. Through defined inflammatory pathways, setting targets for the development of new treatment strategies increases and will provide a comfortable recovery of symptoms in URTIs. The effectiveness of dried extract of Pelargonium sidoides has been confirmed in the studies for the management of URTIs in patients with different types of URTIs. The meta-analyses reported that a herbal drug preparation from the roots of Pelargonium sidoides was effectiveness, safe, and well-tolerated during acute respiratory tract infections in children, adolescents, and adults [13,14,15]. In addition, there was a clinically significant advantage in the treatment of acute rhinosinusitis with Pelargonium sidoides in adult patients evaluated with a double-blind, randomized, placebo-controlled, parallel-group, multicenter study [16]. A recent study conducted by Roth et al. [17] revealed that the Pelargonium sidoides reduced the viral docking proteins in rhinoviruses, particularly associated with bronchitis exacerbations, asthma, and chronic obstructive pulmonary disease. A recent study showed that Pelargonium sidoides induced IL-22 production by CD4 + memory T cells and provided bacterial airway protection [18].
As known, in the early stages of the inflammatory reaction, patients with URTI are particularly suffered from a cough. The inflammation during the URTIs can cause damage to the mucociliary system, causing congestion of mucus secretion in the nose and the paranasal sinuses and triggering a cough. Through the main ingredients, Pelargonium sidoides might promote the defense mechanism of the mucociliary system provides a decrease in mucus viscosity, hence decrease the intensity and frequency of the cough, and it has also been detected that the extracts of Pelargonium sidoides—as a modulator of upper respiratory tract associated immunological responses—might relieve the symptoms by increasing the production of monocyte-related and decreasing the production of neutrophil-related chemokines in acute postviral rhinosinusitis [7, 14, 19]. The above hypothesis is confirmed by the fact that it was found that there was a reducing the frequency of cough via administration of Pelargonium sidoides in our study. Additionally, there was also detected that significant relief in dry cough and sneezing.
In conclusion, the study indicated that the dried root extract of Pelargonium sidoides compared with placebo may be a support treatment option in relieving cough frequency, dry cough, and sneezing during the uncomplicated URTIs, and it might also be effective as an early improver implementation at the onset of signs. The herbal liquid root extracts from Pelargonium sidoides could be a new therapeutical concept in the management of URTIs. As a result of this, the patients would benefit not only from its effectiveness in relieving the symptoms but also from reducing the burden of the symptoms during URTIs.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
IBM SPSS version 21.0 for personal computers (Chicago, IL, USA) and web-based software [R software, version 3.5.2, package: nparLD, R Foundation for Statistical Computing, Vienna, Austria; http://r-project.org].
Abbreviations
- H1N1, H3N2:
-
Influenza A virus strains
- TNF-alfa:
-
Tumor necrosis factor
- TSS:
-
Total symptom score
- URTIs:
-
Upper respiratory tract infections
References
Thomas M, Bomar PA. (2020) Upper respiratory tract infection. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Feb 4. Available from https://pubmed.ncbi.nlm.nih.gov/30422556 (PMID: 30422556, NBK532961)
Turner RB (1997) Epidemiology, pathogenesis and treatment of the common cold. Ann Allergy Asthma Immunol 78(6):531–540. https://doi.org/10.1016/S1081-1206(10)63213-9
Timmer A, Günther J, Rücker G, Motschall E, Antes G, Kern WV (2008) Pelargonium sidoides extract for acute respiratory tract infections. Cochrane Database Syst Rev 16(3):CD006323. https://doi.org/10.1002/14651858.CD006323.pub2
Kolodziej H, Kayser O, Radtke OA, Kiderlen AF, Koch E (2003) Pharmacological profile of extracts of Pelargonium sidoides and their constituents. Phytomedicine 10(4):18–24. https://doi.org/10.1078/1433-187x-00307
Schotz K, Noldner M (2007) Mass spectroscopic characterisation of oligomeric proanthocyanidins derived from an extract of Pelargonium sidoides roots (EPs 7630) and pharmacological screening in CNS models. Phytomedicine 14(6):32–39. https://doi.org/10.1016/j.phymed.2006.11.019
Bätzing-Feigenbaum J, Schulz M, Schulz M et al (2016) Outpatient antibiotic prescription: a population-based study on regional age-related use of cephalosporins and fluoroquinolones in Germany. Dtsch Arztebl Int 113(26):454–459. https://doi.org/10.3238/arztebl.2016.0454
Martin D, Konrad M, Adarkwah CC, Kostev K (2020) Reduced antibiotic use after initial treatment of acute respiratory infections with phytopharmaceuticals- a retrospective cohort study. Postgrad Med 132(5):412–418. https://doi.org/10.1080/00325481.2020.1751497
Willcox M, Simpson C, Wilding S et al (2021) Pelargonium sidoides root extract for the treatment of acute cough due to lower respiratory tract infection in adults: a feasibility double-blind, placebo-controlled randomised trial. BMC Complement Med Ther 29 21(1):48. https://doi.org/10.1186/s12906-021-03206-4
Jackson GG, Dowling HF, Spiesman IG, Boand AV (1958) Transmission of the common cold to volunteers under controlled conditions. Arch Intern Med 101(2):267–278 (PMID: 13497324)
Gabrielian ES, Shukarian AK, Goukasova GI, Chandanian GL, Panossian AG, Wikman G, Wagner H (2002) A double blind, placebo-controlled study of Andrographis paniculata fixed combination Kan Jang in the treatment of acute upper respiratory tract infections including sinusitis. Phytomedicine 9(7):589–597. https://doi.org/10.1078/094471102321616391
Brunner E, Domhof S, Langer F (2002) Nonparametric analysis of longitudinal data in factorial experiments. Wiley, Published in 2002 in New York NY: J Wiley https://lib.ugent.be/catalog/rug01:001356910
Cohen J (1992) A power primer. Psychol Bull 112(1):155–159. https://doi.org/10.1037//0033-2909.112.1.155
Agbabiaka TB, Guo R, Ernst E (2008) Pelargonium sidoides extract for acute bronchitis: a systematic review and meta-analysis. Phytomedicine 15(5):378–385. https://doi.org/10.1016/j.phymed.2007.11.023
Matthys H, Lehmacher W, Zimmermann A, Brandes J, Kamin W (2016) EPs 7630 in acute respiratory tract infections -a systematic review and meta-analysis of randomized clinical trials. J Lung Pulm Respir Res 3(1):415. https://doi.org/10.15406/jlprr.2016.03.00068
Anheyer D, Cramer H, Lauche R, Saha FJ, Dobos G (2018) Herbal medicine in children with respiratory tract infection: systematic review and meta-analysis. Acad Pediatr 18(1):8–19. https://doi.org/10.1016/j.acap.2017.06.006
Bachert C, Schapowal A, Funk P, Kieser M (2009) Treatment of acute rhinosinusitis with the preparation from Pelargonium sidoides EPs 7630: a randomized, double-blind, placebo-controlled trial. Rhinology 47(1):51–59 (PMID: 19382496)
Roth M, Fang L, Stolz D, Tamm M (2019) Pelargonium Sidoides Radix extract EPs 7630 reduces Rhinovirus infection through modulation of viral binding proteins on human bronchial epithelial cells. PLoS One 14(2):e0210702. https://doi.org/10.1371/journal.pone.0210702
Witte K, Koch E, Volk HD, Wolk K, Sabat R (2020) The herbal extract EPs® 7630 increases the antimicrobial airway defense through monocyte-dependent induction of IL-22 in T cells. J Mol Med 98(10):1493–1503. https://doi.org/10.1007/s00109-020-01970-3
Perić A, Vezmar Kovačević S, Barać A, Gaćeša D, Perić AV, Vojvodić D (2020) Effects of Pelargonium sidoides extract on chemokine levels in nasal secretions of patients with non-purulent acute rhinosinusitis. J Drug Assess 9(1):145–150. https://doi.org/10.1080/21556660.2020.1838176
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. ŞG, BED: collect data, data analysis, writing manuscript. ŞG, BED, AY: collect data. ZK: review manuscript. The first draft of the manuscript was written by ŞG, and all authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed according to the ethical standards of the Ministry of Health of Turkey, Ethics Committee, and the 1964 Helsinki Declaration. The study was approved by the Ethics Committee of the Ministry of Health of Turkey [19-AKD-45].
Consent to participate
Written informed consent was obtained from the parents.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Nicole Ritz
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gökçe, Ş., Dörtkardeşler, B.E., Yurtseven, A. et al. Effectiveness of Pelargonium sidoides in pediatric patients diagnosed with uncomplicated upper respiratory tract infection: a single-blind, randomized, placebo-controlled study. Eur J Pediatr 180, 3019–3028 (2021). https://doi.org/10.1007/s00431-021-04211-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04211-y