Abstract
Children with sickle cell disease (SCD) are at a high risk for neurocognitive impairment. We aim to quantitatively measure cerebral tissue R2* to investigate the brain iron deposition in children and young adults with SCD in comparison to beta thalassemia major (BTM) and healthy controls and evaluate its impact on neurocognitive functions in patients with SCD. Thirty-two SCD, fifteen BTM, and eleven controls were recruited. Multi-echo fast-gradient echo sequence brain MRI was performed, and brain R2* values of both caudate and thalamic regions were calculated. SCD patients were examined for the neurocognitive functions. SCD had high iron overload 0.30 ± 0.12 mg/kg/day. 68.9% of SCD had under-threshold IQ, 12.5% had moderate to severe anxiety, and 60.8% had depression. There were no differences between SCD, BTM, and controls in brain MRI except that left thalamus R2* higher in BTM than both SCD and controls (p = 0.032). Mean right caudate R2* was higher in female than male (p = 0.044). No significant association between brain R2* and LIC or heart R2* values in SCD. Left caudate R2* directly correlate with age and HbS%, and negatively correlate with HbA% while right thalamus R2* negatively correlate with transfusion index and among SCD patients.
Conclusion: Neurocognitive dysfunction in SCD could not be explained solely by brain iron overload.
What is Known: • Children with sickle cell disease are at great risk of brain damage due to their irregularly shaped red blood cells that can interrupt blood flow to the brain. • There are a number of factors that have negative brain effects that result in learning difficulties, and this not only due to increase brain iron content. | |
What is New: • Assessment of quantitative brain iron content using MRI R2* in children and young adults with SCD in comparison to beta thalassemia major and healthy controls. • Impact of brain iron content on neurocognitive functions of children and young adults with SCD. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Central nervous system (CNS) complications are among the most devastating manifestations of sickle cell disease (SCD) with approximately 250-fold higher incidence of stroke than in the general pediatric population [1]. Cerebrovascular accidents can be the cause of the observed neurocognitive impairments [2]. However, even in the absence of overt cerebral strokes or parenchymal abnormalities in neurologically intact SCD patients; neurocognitive dysfunction could occur [3] due to recurrent micro-infarction of the CNS, hypoxic damage to the brain secondary to chronic anemia, hypoxic damage exacerbated by acute events, and chronic nutritional deficiency associated with increased metabolic demands [2].
Elevated iron in the brain, in case of iron overload syndromes, has a neurotoxic effect through the formation of reactive oxygen species (ROS) which are a source of oxidative stress that initiates apoptotic signal pathways [4]. Because of the abundance of molecular oxygen and oxidizable neurotransmitters and the presence of poor antioxidant defense mechanisms of the brain, it becomes very liable for iron-induced oxidative damages [5].
Owing to these observations, most recent evaluations of clinical trials to treat children with SCD have included neurocognitive function as a primary or secondary outcome [6]. It is clearly a priority of the pediatric SCD community to address concerns and better understand how neurocognitive function is affected and how to prevent this devastating impact from happening [7]. The primary objective of this work was to measure quantitative brain iron content, using MRI R2* values in the caudate and thalamic regions in Egyptian children and young adults with SCD in comparison to beta thalassemia major (BTM) and age and sex-matched healthy controls, while the secondary objectives were to evaluate the impact of brain iron content on neurocognitive functions assessed by neurocognitive examinations and to evaluate its association with the liver and heart iron concentrations.
Patients and methods
This is a cross-sectional case–control study conducted at the Pediatric Hematology Oncology department, Children’s Hospital, Ain Shams University. Participation was voluntary after informed consent and assent were obtained from legal guardians of all participants and their children. The procedures applied in this study were approved by the institutional regulatory board of the Pediatric and Radiology department as well as by the Ethical Committee of Human Experimentation of Ain Shams University and were in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Study population
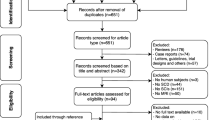
Thirty-two adolescents and young adults with SCD, 13 females (40.6%) and 19 males (59.4%), with their mean age of 15.25 ± 3.69 years, were recruited at their steady state defined as a point in time where the patient in question is not experiencing an acute painful crisis or any changes due to therapy) [8]. In addition, fifteen patients with BTM, 8 (53.3%) females and 7 (46.7%) males, with their mean age of 19.40 ± 4.31 years, were recruited as a comparative iron overload syndrome. Furthermore, eleven healthy controls—subjects who had not history of any neurological disease, blood transfusion, or any condition that would affect the body iron content, 6 females (54.5%) and 5 males (45.5%)—their mean age was 17.73 ± 4.84 years.
Recruited subjects should be able to perform MRI and neuropsychiatric assessment. Subjects known to have contraindications for MRI, those with myocardial infarction, cardiac failure, or and liver cell failure; those with history of neurological disease, head trauma, or neurosurgery; and those treated with any medications affecting the cognition, memory, and behavioral were excluded. None of SCD patients had diabetes or micro-albuminuria, and all of them had previously experienced vaso-occlusive crisis; clinical characteristics among the studied thirty-two SCD patients are illustrated in Table 1.
Study procedure
Patients with SCD were subjected to thorough clinical assessment with special emphasis neurological assessment and SCD related complications. The transfusion received was calculated as the transfusion index: volume of transfused packed red cells in milliliter per kilogram body weight per year (expressed as the mean value in the last 2 years). Thirty (93.8%) SCD patients received either mono- or combined chelation therapy. Fifteen of them received mono-chelation; fourteen received oral deferiprone (DFP) in a daily dose of 50–100 mg/kg/day, and one patient received deferoxamine (DFO) infused subcutaneously in a dose 30–45 mg/kg/day given 5 days/week. Compliance to chelation therapy was assessed by reviewing patient self-report of dose-taking, and the appropriate number of doses taken during each day was checked by prescription refills and pill count; a cutoff point below 80% was considered as poor compliance to the regimen [9]. Of the thirty SCD patients on chelation, twenty of them received concomitantly hydroxyurea therapy which was given orally in a dose of 20 mg/kg/day with escalation to a maximum tolerated dose according to the safety and response.
Laboratory analysis
Laboratory investigations included CBC using Sysmex XT-1800i (Sysmex, Kobe, Japan), hemoglobin analysis by HPLC using D-10 (Bio-Rad, Marnes La Coquette, France), liver function tests (serum albumin, total and direct bilirubin, alanine aminotransferase, and aspartate aminotransferase), and markers of hemolysis (lactate dehydrogenase and indirect bilirubin) using Cobas Integra 800 (Roche Diagnostics, Mannheim, Germany). Serum ferritin level was measured on Immulite 1000 analyzer (Siemens Healthcare Diagnostics, Marburg, Germany) at the start of the study with calculation of the mean value of the last year prior to the study in order to estimate the ferritin trend; then, the cutoff value 2500 µg/L was used to classify SCD patients into 2 groups as it was defined to be the best for prediction of thalassemia complication [10].
Radiologic evaluation
MRI examination was performed on a 1.5-Tesla superconductive MR Philips scanner (Achieva 2018, Philips, Nederland B.V., The Netherlands) at Diagnostic Radiology Department at Ain Shams University Hospital without any contrast material. Patients were prepared and were trained to remain motionless, avoid excessive swallowing, and regulate respiration and were informed that study takes about 10–15 min and that the system generates some loud noise.
Regional-brain R2* quantitative MRI assessment
was performed for fifteen SCD patients and fifteen BTM and eleven controls. Localizer images in three orthogonal planes were taken first; then, axial slices of the brain were acquired covering the regions of interest (ROIs) (both right and left caudate and thalamic nuclei); each slice was acquired by a multi-echo gradient T2* sequence (Fast Field Echo/m-FFE), and the total acquisition time was 2.15 min. Sequence parameters were as follows: twelve (TEs) spaced from 1 to 12 ms, TR 100, slice thickness = 10, FOV 225 × 225, matrix size: 140 × 150, flip angle = 15° and NSA = 6. Drawing ROIs on the caudate head and thalamic nuclei was done manually. Then, each ROI is propagated to the other (TEs), automatically. This was performed symmetrically in both hemispheres (left and right sides). The mean (SI) of a region was measured for each image and plotted against the TE. A single T2* decay curve for each ROI is obtained that generally reflects the average iron concentration in that region. The mean regional-brain T2* and R2* values were calculated manually using a simple mathematical model using Microsoft (MS) Excel spreadsheet V 2.01 where values of signal intensity (T2* values), and TEs were manually inputted into the Excel spreadsheet [11].
Quantitative liver iron concentration (LIC) and myocardial T2* MRI assessment
were performed for fifteen SCD and fifteen BTM only. Myocardial T2* was measured through multi-echo turbo field echo black and white blood short axis, and patients were then classified into normal T2* levels (> 20 ms), low (15–20 ms), intermediate (10–15 ms), and high risk T2* < 10 ms calculated [12]. LIC was performed through multi-echo gradient axial cuts through the upper abdomen. According to liver iron T2* values, patients are classified normal T2* levels (> 11.4 ms), low (3.8–11.4 ms), intermediate (1.8–3.8 ms), and high T2* (< 1.8 ms) [13].
Neurocognitive and psychiatric assessment
Psychiatric interviews and assessments were conducted by experienced qualified psychologist using the following instruments.
Wechsler intelligence scale for children–fourth edition (WAIS-IV)
is an intelligence quotient (IQ) test designed to measure intelligence and cognitive ability and to assess verbal comprehension, visual-perceptive performance, working memory, and processing speed and finally provides a global scale to get the IQ [14]. Findings were classified as under threshold if values were < 90, normal, or average 90–109, over the threshold if > 109 [15].
Brief psychiatric rating scale (BPRS)
is a 24-item BPRS (version 4.0) that assesses 24 psychiatric symptoms including depression and anxiety. The presence and severity of psychiatric symptoms were rated on a Likert scale ranging from 1 (not present) to 7 (extremely severe). A separate score for the degree of pathology in each of the symptoms areas is obtained in this way [16].
Benton visual retention test
is an individually administered test that measures visual perception and visual memory. It can also be used to help identify possible learning disabilities among other afflictions that might affect an individual’s memory. The individual examined is shown 10 designs, one at a time, and asked to reproduce each one as exactly as possible on plain paper from memory. The test is untimed, and the results are professionally scored by form, shape, pattern, and arrangement on the paper. The test has cutoff point at ≥ 4, and those values are the same for the difference between the obtained correct and the expected correct, and the difference between the obtained error and expected error [17].
Statistical analysis
Data were entered, processed, and analyzed using software IBM® SPSS® Statistics 23 version. Descriptive statistics for quantitative variables were described as mean and standard deviation or median and interquartile range (IQR; 75th and 25th percentiles). Qualitative variables were described as number and percent. The Kolmogorov–Smirnov test was used for testing the distribution of normality. The Student’s T-test was used to compare between two groups for numerical variables and chi-square test for categorical variables. The comparison between two independent groups with qualitative data was performed using chi-square test, and the comparison between more than two independent groups with quantitative data and parametric distribution was performed by one-way ANOVA test followed by post hoc analysis using LSD test. Pearson correlation coefficients were used to assess the correlation between two quantitative parameters in the same group. The confidence interval was set to 95%, and the margin of error accepted was set to 5%, and the probability of < 0.05 was used as a cutoff point for significant test meaning that P-value < 0.05 were significant.
Results
Neurocognitive and psychiatric characteristics among the studied patients with SCD are illustrated in Table 2. Nearly two-thirds of SCD had IQ under threshold (IQ value < 90). 12.5% of SCD patients had moderate to severe anxiety, and 60.8% had of SCD patients had depression.
Only two male patients with SCD had history of stroke, with headache in one patient and limb weakness affecting the left side in the other patient were the presenting symptoms. Both had confirmed radiological diagnosis of stroke showing lacunar infarctions (watershed infarctions). At the time of assessment, both had no functional neurological deficit and normal TCD assessment.
Radiological characteristics of the studied groups are illustrated in Table 3. There were no significant differences between the three studied groups with respect to age (p = 0.261). Left thalamus R2* value was higher in patients with BTM than both patients with SCD and healthy controls.
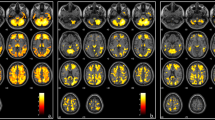
Correlation study between R2* values of different regions of the brain in patients with SCD and the studied neurocognitive parameters showed no significant correlation except positive correlation between left caudate R2* and anxiety value (r = 0.724, p = 0.012). There were positive correlation between hemoglobin S% and both left caudate R2* (r = 0.015, p = 0.031) and right thalamus R2* (r = 0.612, p = 0.105) and a negative correlation between hemoglobin A% and left caudate R2* (r = −0.568, p = 0.027). There were positive correlation between left caudate R2* and age and negative correlation between transfusion index and right thalamus R2* as shown in Fig. 1. However, there was non-significant correlation between mean pre-transfusion hemoglobin and the R2* values of different regions of the brain.
A univariate linear regression model was built between certain variables (age, transfusion frequency, Hb S%, Hb A%, Benton visual retention test), and the left caudate R2* showed that the most important factor influenced by the level of left caudate R2* is the Benton visual retention for the difference of correct (t = 5.687, p = 0.011).
The correlation coefficients between R2* values of different regions of the brain in SCD subgroup with patients showed no significant association that was found between brain R2* values LIC or heart R2* values. R2* values of different regions of brain in relation with the studied parameters of patients with SCD were not significant except for sex; mean right caudate R2* value was higher in female (17.38 ± 0.83) than in male (15.58 ± 1.68) (p = 0.044).
Illustrative case
A seventeen-year-old female patient with SCD, on regular blood transfusion, had serum ferritin level equal 7426 ng/mL. Her liver iron content equals 7.49 mg/g, cardiac T2* equals 41 ms, cardiac R2* equals 24.4 Hz, and her calculated MIC equal 0.48 mg/g. Figure 2 showed that her estimated left thalamus T2* was 69.1 ms, R2* 14.5 Hz, and calculated left thalamus R2* was 14.5 Hz (within the normal range of R2* of healthy controls (13.3–16.9)).
Multi-echo fast gradient echo brain MRI T2* sequence. Left: region of interest is drawn at the left thalamus (highlighted in red) for measuring the mean signal intensity throughout multiple echo times to calculate the R2*. Right: data analysis using Microsoft Excel spreadsheet V 2.01: the signal intensity (TE) is plotted against multiple TE values. The exponential signal decay curve is then constructed. T2* and R2* values are calculated automatically in the left thalamic region
Discussion
Sickle cell disease (SCD) is common among people from Africa, the Middle East, and the Mediterranean [18]. Although the wider use of hydroxycarbamide and newer therapeutic approaches offer hope for decreased mortality and improved health-related quality of life, SCD in lower source countries still carries poor prognosis and is associated with high early childhood mortality [19]. Transfusion is a frequently employed therapy in SCD, but its best-validated uses have been in preoperative prophylaxis, treatment of acute chest syndrome (ACS), prophylaxis, and treatment of stroke [20], and nearly more than 90% of adults are receiving at least one transfusion in their lifetimes [19]. While transfusion may improve disease complications, iron overload is an inevitable consequence of transfusion therapy and iron deposited in the different body organs leading to their cellular damage [21]. Chronically transfused iron overloaded patients with SCD have significantly higher mortality than less transfused counterparts without iron overload [22].
Studies and data concerning the brain iron deposition in SCD patients are still limited and conflicting. Multiple studies showed increased iron levels in certain brain regions which were normal in the other studies. Although MRI is the most reliable and non-invasive method for early detection of the organic iron overload with sensitivity of 96% and specificity of 80% [23], there are still no international guidelines that set the cutoff values of brain R2* values for the brain iron assessment in patients with iron overload as those established in the liver and heart. Anatomical networks are mostly studied using a model-driven seed-based approach with a priori hypotheses of manually selected regions of interest and their connected networks [24, 25]. The basal ganglia and thalamus were chosen to be the region of interest (ROIs) as they are known to be the main sources of brain iron accumulation [26, 27].
A 2D T2* multi-echo fast-gradient echo pulse sequence was used in the current study for assessment of brain iron content, the same technique used by Akhlaghpoor and his team [5] while other researchers used a 3D gradient-echo sequence [28]. An early study showed that R2* is more sensitive to R2 in evaluation of the brain iron content comparing both to chemically determined brain iron concentrations in a postmortem study [29]. A subsequent study found that SWI was the most sensitive in detecting iron accumulation in the choroid plexus, followed by GRE T2* sequence in comparison to T2-weighted [30].
Early in the 2000s, the first study was performed to evaluate the MRI brain iron content in patients with BTM; the study found that the T2 relaxation rates (R2) were higher in the caudate, putamen, and motor and temporal cortex in BTM patients than in the controls [31]. A decade later, another study confirmed that BTM patients had significantly lower T2* values in basal ganglia, thalamus, and adenohypophysis compared to controls and no correlation between liver T2* values and T2* values of basal ganglia (striatum) and the thalamus [5]. In 2018, a study found that BTM patients showed significantly higher susceptibility value in the red nucleus and choroid plexus indicating more iron deposition in both areas [28]. In the same year, another study used voxel-based high-resolution whole-brain MRI study in addition to regional analysis of the grey matter subcortical regions. In this study, compared to the controls group, both TDT (transfusion-dependent thalassemia) and NTDT (non-transfusion-dependent thalassemia) groups show only small areas of higher iron deposition; these areas were the anterior hippocampal formation, areas around Luschka foramina and dorsal thalamic nuclei (in TDT; left thalamic region) [32].
In 2014, Brown et al. found that only the choroid plexus showed a significant increase in iron content in the SCD group, and the levels correlated well with serum ferritin and liver R2* while no significant iron elevation in the subcortical nuclei and no correlation between the iron levels in the subcortical structures and the liver R2* when corrected for age [33]. In 2018, Miao et al. measured the brain iron content of the asymptomatic SCD patients using R2*-regional based brain iron quantification including caudate nucleus, putamen, globus pallidus, red nucleus, substantia nigra, and the dentate nucleus and found that only the R2* values of the substantia nigra and the dentate nucleus were significantly higher in the SCD group than the controls [34].
In the current study, three subgroups that performed MRI assessment were age- and sex-matched. No significant differences were found between the SCD and control groups in all regions including the left thalamus. However, in BTM subgroup, patients had significantly higher R2* values compared to the controls and SCD patients as regards to the left thalamic region. There is a conflicting result as regard differential iron content; one research concluded that left hemisphere showed greater iron content than the right hemisphere [27] while others found that there were no significant differences between both hemispheres [31]. Our study showed no correlation between the measured R2* values in all the selected ROIs and liver iron concentrations in both SCD and BTM patients, which may indicate that LIC is not good indicator of the brain iron content. Also, our study showed that no significant correlation was found between the serum ferritin and R2* values in all selected ROIs in SCD group. In general, most of the studies indicate that serum ferritin as well as LIC and MIC are not good predictors of brain iron overload [5, 32, 33].
The different findings in different studies regarding brain iron content could be explained by the hypothesis that the brain has a protective mechanism against iron overload by decreasing the transferrin receptors when the serum iron level increases. So, iron deposition cannot exceed a certain saturation level in certain brain areas. Also, differences in the T2* values among the various brain regions indicate that the iron uptake into the brain differs depending on the brain region [5, 31]. Differences could also be explained by sample characteristics: different demography, environmental and dietary factors, and guidelines of treatment in different countries with different chelation therapy as well as different study design and MRI sequences.
The Cooperative Study of Sickle Cell Disease (CSSCD) began examining neurocognitive function and neuroimaging patterns in a large SCD cohort over a 10-year period. The CSSCD found that nearly 22% of children with HbSS experienced a clinical stroke or silent cerebral infarct prior to 15 years of age, and that there were measureable differences in global cognitive function and specific neuropsychological function associated with these events [35]. In addition, the CSSCD found that, in children who had no evidence of brain abnormality on MRI over the 10 years of participation, there was still a mean decline of 16 IQ points over time [36]. This strongly suggested that something besides vascular occlusion/infarction placed children with SCD at risk, and mechanisms involving chronic anemia, hypoxia, or interference with oxygen perfusion and diffusion have been considered [37]. A literature review in 2007 revealed that there was a decrease in the neurocognitive functions in SCD patients evidenced by impairment in Full Scale IQ (FSIQ), Verbal IQ (VIQ), or Performance IQ (PIQ) and impaired attention and executive functions together with academic achievement [38]. Children with SCD are at a high risk for neurocognitive impairment, which has potential implications for overall HRQL. A meta-analysis indicated that children with SCD often scored lower on general IQ measures than healthy children, with 51% of studies reporting significant differences. When examining specific cognitive abilities, more robust and consistent differences were found, with 71% of studies reporting significant deficits in at least one cognitive domain [39]. Deficits have been found most often in attention, processing speed, and working memory, as well as verbal and language domains [36, 40]. In agreement with previous studies, our study showed that 68.9% of our SCD patients had under-threshold TIQ scores. Furthermore, 50% of the patients showed mild anxiety, 8.3% moderate anxiety, and 4.3% showed severe anxiety.
The reasons behind cognitive dysfunctions in SCD patients are still not fully understood. Despite, we reported cognitive dysfunctions in SCD patients, and there were no statistically significant differences between the SCD and control groups as regard the brain iron deposition. Previous studies showed that these neurological abnormalities may be due to neurotoxicity of DFO, chronic hypoxia, chronic illness, multiple hospitalizations, or silent strokes [2, 3].
With the study limitations, the relative small sample size, the lack of comparative neurocognitive tests for BTM cohort, the usage of ME-GRE T2* sequence and not the susceptibility-weighted images sequence (SWI), and the lack of whole-brain quantitative MRI study, we conclude that the brain iron deposition as the sole cause for neurocognitive impairment in patients with SCD could not be proved.
Availability of data and material
All authors make sure that all data and materials as well as software application or custom code support their published claims and comply with field standards.
Abbreviations
- CNS:
-
Central nervous system
- SCD:
-
Sickle cell disease
- ROS:
-
Reactive oxygen species
- LIC:
-
Liver iron concentration
- ROIs:
-
Regions of interest
- WAIS-IV:
-
Wechsler Intelligence Scale for Children-Fourth Edition
- BPRS:
-
Brief Psychiatric Rating Scale
References
Ohene-Frempong K (1991) Stroke in sickle cell disease: demographic, clinical, and therapeutic considerations. Semin Hematol 28(3):213–219
Brown RT, Davis PC, Lambert R, Hsu L, Hopkins K, Eckman J (2000) Neurocognitive functioning and magnetic resonance imaging in children with sickle cell disease. J Pediatr Psychol 25(7):503–513
Vichinsky EP, Neumayr LD, Gold JI, Weiner MW, Rule RR, Truran D, Kasten J, Eggleston B, Kesler K, McMahon L, Orringer EP, Harrington T, Kalinyak K, De Castro LM, Kutlar A, Rutherford CJ, Johnson C, Bessman JD, Jordan LB, Armstrong FD (2010) Neuropsychological dysfunction and neuroimaging adult sickle cell anemia study group. Neuropsychological dysfunction and neuroimaging abnormalities in neurologically intact adults with sickle cell anemia. JAMA 303(18):1823–1831
Hare D, Ayton S, Bush A, Lei PA (2013) A delicate balance: iron metabolism and diseases of the brain. Front Aging Neurosci 5:34
Akhlaghpoor S, Ghahari A, Morteza A, Khalilzadeh O, Shakourirad A, Alinaghizadeh MR (2012) Quantitative T2* magnetic resonance imaging for evaluation of iron deposition in the brain of β-thalassemia patients. Clin Neuroradiol 22(3):211–217
Thompson BW, Miller ST, Rogers ZR, Rees RC, Ware RE, Waclawiw MA, Iyer RV, Casella JF, Luchtman-Jones L, Rana S, Thornburg CD, Kalpatthi RV, Barredo JC, Brown RC, Sarnaik S, Howard TH, Luck L, Wang WC (2010) The pediatric hydroxyurea phase III clinical trial (BABY HUG): challenges of study design. Pediatr Blood Cancer 54(2):250–255
Steinberg MH, McCarthy WF, Castro O, Ballas SK, Armstrong FD, Smith W, Ataga K, Swerdlow P, Kutlar A, DeCastro L, Waclawiw MA (2010) Investigators of the multicenter study of hydroxyurea in sickle cell anemia and MSH patients’ follow-up. The risks and benefits of long-term use of hydroxyurea in sickle cell anemia: a 17.5 year follow-up. Am J Hematol 85(6):403–408
Ballas SK, Lieff S, Benjamin LJ (2010) Definitions of the phenotypic manifestations of sickle cell disease. Am J Hematol 85:6–13
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK (2008) Medication compliance and persistence: terminology and definitions. Value Health 11:44–47
Silvilairat S, Sittiwangkul R, Pongprot Y, Charoenkwan P, Phornphutkul C (2008) Tissue doppler echocardiography reliably reflects severity of iron overload in pediatric patients with beta thalassemia. Eur J Echocardiogr 9:368–372
Fernandes JL, Sampaio EF, Verissimo M, Pereira FB, Alvaro da Silva J, de Figueiredo GS, Kalaf JM, Coelho OR (2011) Heart and liver T2* assessment for iron overload using different software programs. Eur Radiol 21:2503–2510
Carpenter JP, He T, Kirk P, Roughton M, Anderson LJ, de Noronha SV, Sheppard MN, Porter JB, Walker JM, Wood JC, Galanello R, Forni G, Catani G, Matta G, Fucharoen S, Fleming A, House MJ, Black G, Firmin DN, St Pierre TG, Pennell DJ (2011) On T2* magnetic resonance and cardiac iron. Circulation 123(14):1519–1528
Garbowski MW, Carpenter JP, Smith G, Roughton M, Alam MH, He T, Pennell DJ, Porter JB (2014) Biopsy-based calibration of T2* magnetic resonance for estimation of liver iron concentration and comparison with R2 Ferriscan. J Cardiovasc Magn Reson 16(1):40
Wechsler D (2003) Wechsler Intelligence Scale for Children – fourth edition (WISC-IV). The Psychological Corporation, San Antonio, TX
Weiss LG, Saklofske DH, Prifitera A, Holdnack JA (2006) WISC-IV Advanced Clinical Interpretation. Academic Press, Burlington (MA)
Ventura J, Lukoff D, Nuechterlein KH, Liberman RP, Green M, Shaner A (1993) Brief Psychiatric Rating Scale (BPRS) Expanded version (4.0) scales, anchor points and administration manual. Int J Methods Psychiatr 3:227–244
Benton AL (1992) Benton Visual Retention Test, 5th edn. The Psychological Corporation, San Antonio
Agha M, Eid AF, Sallam M (2013) Sickle cell anemia: imaging from head to toe. Egypt J Radiol Nucl Med 44:547–561
Ware RE, Montalembert MD, Tshilolo L, Abboud MR (2017) Sickle cell disease. Lancet 390:311–323
Raghupathy R, Manwani D, Little JA (2010) Iron overload in sickle cell disease. Adv Hematol 1–10
Fibach E, Rachmilewitz EA (2017) Iron overload in hematological disorders. Presse Med 46(12 Pt 2):e296–e305
Fung EB, Harmatz P, Milet M, Ballas SK, De Castro L, Hagar W, Owen W Olivieri N, Smith-Whitley K, Darbari D, Wang W, Vichinsky E and the Multi-Center Study of Iron Overload Research Group (2007) Morbidity and mortality in chronically transfused subjects with thalassemia and sickle cell disease. Am J Hematol 82:255–265
Farhangi H, Badiei Z, Moghaddam HM, Keramati MR (2017) Assessment of heart and liver iron overload in thalassemia major patients using T2* magnetic resonance imaging. Indian J Hematol Blood Transfus 33(2):228–234
Zielinski BA, Anderson JS, Froehlich AL, Prigge MB, Nielsen JA, Cooperrider JR, Cariello AN, Fletcher PT, Alexander AL, Lange N, Bigler ED, Lainhart JE (1012) scMRI reveals large-scale brain network abnormalities in autism. PLoS One 7(11):e49172
Soriano-Mas C, Harrison BJ, Pujol J, López-Solà M, Hernández-Ribas R, Alonso P, Contreras-Rodríguez O, Giménez M, Blanco-Hinojo L, Ortiz H, Deus J, Menchón JM, Cardoner N (2013) Structural covariance of the neostriatum with regional gray matter volumes. Brain Struct Funct 218(3):697–709
Argyropoulou MI, Metafratzi Z, Kiortsis DN, Bitsis S, Tsatsouis A, Efremidis S (2000) T2 relaxation rate as an index of pituitary iron overload in patients with beta-thalassemia major. AJR Am J Roentgenol 175:1567–1569
Xu X, Wang Q, Zhang M (2008) Age, gender, and hemispheric differences in iron deposition in the human brain: an in vivo MRI study. Neuroimage 40:35–42
Qiu D, Chan GC, Chu J et al (2014) MR quantitative susceptibility imaging for the evaluation of iron loading in the brains of patients with β-thalassemia major. AJNR Am J Neuroradiol 35(6):1085–1090
Langkammer C, Krebs N, Goessler W, Scheurer E, Ebner F, Yen K, Fazekas F, Ropele S (2010) Quantitative MR imaging of brain iron: a postmortem validation study. Radiology 257(2):455–462
Hasiloglu ZI, Asik M, Ure E, Ertem F, Apak H, Albayram S (2017) The utility of susceptibility-weighted imaging to evaluate the extent of iron accumulation in the choroid plexus of patients with β-thalassaemia major. Clin Radiol 72(10):903.e1-903.e7
Metafratzi Z, Argyropoulou MI, Kiortsis DN, Tsampoulas C, Chaliassos N, Efremidis SC (2001) T(2) relaxation rate of basal ganglia and cortex in patients with beta-thalassaemia major. Br J Radiol 74(881):407–410
Tartaglione I, Perrotta S, Caiazza M, Casale M, Di Concilio R, Ciancio A, De Michele E, Amendola G, Gritti P, Carafa PA, Ferrantino T, Centanni A, Ippolito N, Caserta V, Oliveto T, Granato I, Femina G, Esposito F, Ponticorvo S, Russo A, Russo C, Cirillo M, Elefante A, Manara R (2018) Cerebral iron overload in beta thalassemia: does it really matter? Poster session presented at the 23rd Annual Congress of European Hematology Association, Stockholm
Brown RC, Qiu D, Hayes L, Barry V, Jones R (2014) Quantitation of iron in brain structures of children with sickle cell disease and transfusion hemosiderosis. Blood 124(21):1393
Miao X, Choi S, Tamrazi B, Chai Y, Vu C, Coates TD, Wood JC (2018) Increased brain iron deposition in patients with sickle cell disease: an MRI quantitative susceptibility mapping study. Blood 132(15):1618–1621
Armstrong FD, Thompson RJ Jr, Wang W, Zimmerman R, Pegelow CH, Miller S, Moser F, Bello J, Hurtig A, Vass K (1996) Cognitive functioning and brain magnetic resonance imaging in children with sickle cell disease. Neuropsychology committee of the cooperative study of sickle cell disease. Pediatrics 97(6 Pt 1):864–870
Wang W, Enos L, Gallagher D, Thompson R, Guarini L, Vichinsky E, Wright E, Zimmerman R, Armstrong FD (2001) Cooperative study of sickle cell disease. Neuropsychologic performance in school-aged children with sickle cell disease: a report from the cooperative study of sickle cell disease. J Pediatr 139(3):391–397
Armstrong FD, Pavlakis S, Goldman ML, Thompson W, Cuadra A, Sulc W (2010) Neurocognitive outcomes in sickle cell disease. In: Nass R, Frank Y (eds) Cognitive and behavioral abnormalities of pediatric diseases. Oxford University Press, NY, USA, pp 285–292
Berkelhammer LD, Williamson AL, Sanford SD, Dirksen CL, Sharp WG, Margulies AS, Prengler RA (2007) Neurocognitive sequelae of pediatric sickle cell disease: a review of the literature. Child Neuropsychol 13(2):120–131
Schatz J, Finke RL, Kellett JM, Kramer JH (2002) Cognitive functioning in children with sickle cell disease: a meta-analysis. J Pediatr Psychol 27:739–748
Bernaudin F, Verlhac S, Fréard F, Roudot-Thoraval F, Benkerrou M, Thuret I, Mardini R, Vannier JP, Ploix E, Romero M, Cassé-Perrot C, Helly M, Gillard E, Sebag G, Kchouk H, Pracros JP, Finck B, Dacher JN, Ickowicz V, Raybaud C, Poncet M, Lesprit E, Reinert PH, Brugières P (2000) Multicenter prospective study of children with sickle cell disease: radiographic and psychometric correlation. J Child Neurol 15(5):333–343
Author information
Authors and Affiliations
Contributions
The corresponding author, on behalf of all authors, hereby states that all authors have made substantial contributions to the design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work. They drafted the work, revised it critically for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Fatma Soliman Elsayed Ebeid, Ghada Samir Ibrahim, and Hanaa Midhat Abdel Gader Hussein. The first draft of the manuscript was written by Fatma Soliman Elsayed Ebeid, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The procedures applied in this study were approved by the institutional regulatory board of the Pediatric and Radiology department as well as by the Ethical Committee of Human Experimentation of Ain Shams University and were in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Consent to participate
Participation was voluntary after informed consent and assent were obtained from legal guardians of all participants and their children.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elalfy, M.S., Ibrahim, A.S., Ibrahim, G.S. et al. Hidden brain iron content in sickle cell disease: impact on neurocognitive functions. Eur J Pediatr 180, 2677–2686 (2021). https://doi.org/10.1007/s00431-021-04189-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04189-7