Abstract
Shock is a state of circulatory dysfunction and its diagnosis is complex in neonates. Hemodynamic assessment using echocardiography has potential to guide better management regimes in neonates with shock. Objective of this study is to analyze changes in the echocardiographic parameters in preterm neonates with shock at presentation and after resolution. In this prospective pragmatic Cohort study, eligible neonates with shock were monitored for changes in echocardiographic parameters at onset of shock and after resolution of shock. Paired data analysis was done for observed changes in the parameters. Based on initial clinical parameters and echocardiographic parameters, infants were assigned into different types of shock. Data of 37 infants were analyzed for baseline clinical and echocardiographic parameters, and data of 31 infants were analyzed for the changes in the observed parameters after shock resolution. Statistically significant changes were observed in inferior vena cava collapsibility index (ICI), left ventricular end diastolic volume (LVEDV), isovolemic ventricular relaxation time (IVRT), left and right ventricular stroke volume, and ejection fraction (EF). There was no agreement between clinical and echocardiographic definitions of shock.
Conclusion: We noticed shock has overlapping pathophysiologic features. Our study highlights the importance of baseline documentation of echocardiographic parameters of all infants who are at risk of shock and repeat echocardiography at onset of shock to observe the changes in ICI, LVEDV, IVRT, stroke volume, and EF. This would guide pathophysiological management of shock in neonates.
What is Known: • In neonates pathophysiology of shock is overlapping. • Echocardiography can help in better understanding and management of shock. | |
What is New: • Study gives median changes in major echocardiographic parameters in neonatal shock. • These changes can guide for selection of volume and inotropes in management. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Shock in neonates is an acute physiological state in which circulatory function is inadequate to supply sufficient amounts of oxygen and nutrients to tissues to meet their metabolic demands [1, 2]. The diagnosis of shock requires multiple clinical parameters supported with laboratory and other investigations. The routine clinical parameters have limited diagnostic utility in these at risk infants and at this critical period of perinatal transition. Early diagnosis of shock will help in improving the clinical outcomes, and delayed diagnosis will have long-term consequences on neurodevelopmental outcomes [3, 4]. There is a growing interest in point-of-care echocardiography in assessment of shock [5]. Hemodynamic assessment using echocardiography has the potential to assess the underlying pathophysiology of shock. This includes the assessment of volume status, diastolic and systolic ventricular function, afterload assessment, pulmonary hypertension, and ductal patency [6, 7]. Moreover, neonatologist performing echocardiogram can assess the possible underlying pathophysiologic mechanisms of circulatory failure and can use the data to evaluate the efficacy of therapeutic interventions [8]. Previous studies on this topic are limited and have some methodological limitations. Our study focuses on observation of the changes in clinical and echocardiographic hemodynamic parameters in neonates following the routine protocol of shock management. The objectives of this study are to evaluate the changes in blood pressure (systole, diastole, mean arterial pressure, i.e., MAP) and echocardiographic markers of preload (inferior vena cava collapsibility index (ICI), left ventricular end diastolic volume (LVEDV)), diastolic function (mitral E/A ratio (E wave to A wave ratio), isovolumetric ventricular relaxation time (IVRT)), systolic function (left ventricular output, ejection fraction, right ventricular output), and SVR index in neonates with shock.
Patients and methods
This prospective pragmatic observational study was done from October 2017 to May 2019 at a tertiary care level 3 newborn unit, Fernandez Hospital, Hyderabad, India. Ethics approval was obtained from the Institute’s Ethics Committee (Ec Ref No- 25_2017). Data on plethysmography variability index of the same study subjects are published in the same journal as part of another research article. Consent was obtained from the parents at admission of the newborns to the NICU for a possible enrollment. All admitted newborns were eligible for enrollment if and when they developed features of shock. As there is no clear-cut diagnostic criteria for shock in neonatal period, based on the definitions used in prior published studies in neonates, shock was defined as the presence of at least 2 of the 6 criteria [1, 9,10,11,12]: Heart rate > 180 per min, decrease in blood pressure (mean arterial pressure (MAP) < 30 mm of Hg or < MAP < 5th centile for the gestational age or systolic blood pressure < 2 SD for age), oliguria < 0.5 ml/kg/h for preceding 6 h, CRT(capillary refilling time) > 3 s, central to peripheral temperature difference > 3 °C, and metabolic acidosis (base excess (BE) > − 5 or lactate > 2 times upper normal). Neonates who received fluid boluses or inotropes prior to enrollment, those with major congenital anomalies and those undergoing therapeutic hypothermia, were excluded from study. Also, non-availability of principal investigator for recording echocardiography images was one of the major reasons for exclusion from study. All the enrolled newborns were monitored for vital signs such as heart rate, oxygen saturations, blood pressures, perfusion, and respiratory status. The pulse oximeter probe was attached to the right upper limb. MAP was recorded either from invasive intra-arterial catheter or non-invasively by oscillometry (if invasive catheter could not be established) by IntelliVue MP80, Philips, the Netherlands. We used appropriate sized cuff “1” to “3” so as to cover at least 80% of arm circumference. Central to peripheral temperature difference was measured with two separate temperature probes, for central temperature probe was attached at right hypochondrium and for peripheral temperature probe was attached to one of the lower limb at sole.
Echocardiographic evaluation
All echocardiographic parameters were recorded by the principal investigator, a neonatologist, who was trained in echocardiography for 6 weeks by a pediatric cardiologist. All echocardiographic parameters were analyzed by a single pediatric cardiologist and were blinded to the patient data. Guidelines used for recording echocardiographic images in this study are very similar to international evidence-based guidelines on point-of-care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Pediatric and Neonatal Intensive Care (ESPNIC), except for ejection fraction which was calculated using “M mode” in parasternal long axis view [7]. The evaluation included recording of the echocardiography images for estimation of IVC collapsibility index (ICI), left ventricular end diastolic volume (LVEDV), E/A ratio, isovolumetric relaxation time (IVRT), left ventricular output, right ventricular output, and ejection fraction (EF). Systemic vascular resistance (SVR) index was computed by the formula: mean arterial pressure (MAP)/left ventricular output (LVO) [13, 14]. All the echocardiographic parameters were recorded before completion of the first saline bolus. All echocardiographic parameters were noted as per protocol on Philips CX50 (Koninklijke Philips N.V.,), using an 8–4 MHz high-frequency phased-array probe as per standard published literature. All enrolled neonates were assessed hourly for resolution of shock. Complete resolution of shock was defined as normalization of all clinical signs which were used as diagnostic criteria and stoppage of inotropes. All the vitals and echocardiographic findings were re-evaluated after 6 h of the resolution of shock. All the recorded images were analyzed later by a single pediatric cardiologist, who was blinded to the clinical status of the newborn. The management of shock and other neonatal morbidities were as per standard unit protocol. All neonates in shock received either one or two fluid boluses (normal saline) at 10 mL/kg over 10–20 min provided there were no clinical features of heart disease (hepatomegaly > 2 cm, murmur, diagnosed HsPDA, cardiomegaly on X-ray chest). After the fluid bolus was given, the neonates were categorized as either “fluid responsive” (heart rate reduced by 15 beat per min, BP normal as per criteria and CFT < 3 s after completion of fluid bolus(s)) or “fluid non-responsive.” Inotropes were started for neonates with “fluid non-responsive shock”. Dopamine was started initially at 2.5 μg/kg/min and increased by 2.5 μg/kg/min every 15–20 min in case of non-response. Dobutamine was started at 2.5 μg/kg/min in normotensive neonates with signs of poor peripheral perfusion and increased by 2.5 μg/kg/min every 15–20 min. Norepinephrine, epinephrine, vasopressin, and steroids were used for hypotensive infants. Milrinone and dobutamine were used for infants with presumed cardiogenic shock, provided that blood pressure was normal or were combined with dopamine and norepinephrine if they had associated hypotension. The decision to start and modify vasoactive drugs was taken by the bedside physician.
Based on initial clinical evaluation and complete clinical course during the hospitalization, shock in each of the newborns was classified as:
-
1.
Hypovolemic: Improved with only fluid bolus
-
2.
Cardiogenic: Improved with inotropic agents
-
3.
Mixed shock: Improved with fluids and or inotropes or vasopressor action
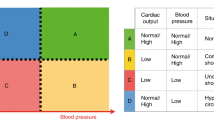
Also shock was categorized into 4 groups based on the echo parameters at onset [14,15,16,17]:
-
1.
Hypovolemia
-
IVC size < 2.1 mm
-
IVC collapsibility index > 50%
-
-
2.
Cardiogenic
-
EF < 55%
-
LVO or RVO < 130 ml/kg/min
-
-
3.
Mixed: If both above mentioned criteria were fulfilled
-
4.
Distributive: Shock in the absence of hypovolemic and cardiogenic features on echocardiography
LVEDV was not used to define hypovolemic shock as there is no normal cutoff values available for neonatal population. The management of shock and other neonatal morbidities was as per standard unit protocol. Data on perinatal variables, onset and resolution of shock, management of shock (fluids, inotropes, vasopressors, and steroids), etiology of shock (blood loss, sepsis, and patent ductus arteriosus), and neonatal morbidities and outcomes were collected prospectively in a pre-designed case reported form. The primary outcome of the study was the changes in echocardiographic parameters at onset and after resolution of shock.
Sample size and statistics
In absence of data on changes in echocardiographic parameters in newborns with shock, we took expected changes in IVC collapsibility for sample size calculation. Expecting a mean difference of 11% with a standard deviation of 15 from a previous study on IVC collapsibility index (before and after volume infusion) [18], the required sample size was 30 infants in two groups (shock and control patients) with a power of 80% and a level of significance of 5% (two sided). We planned to enroll 30 patients for before and after analysis, as a paired data. Standard descriptive statistics were used for analysis of baseline variables. Changes in clinical parameters and echocardiographic parameters, at shock and after resolution of shock, were analyzed using “Wilcoxon signed-rank test.” All the analysis was done using statistical software packages SPSS version 23.0.
Results
A total 37 of infants are enrolled in this study (Fig. 1). The demographics of this cohort is depicted in Table 1. Echocardiographic evaluation was performed only after enrollment of infant in the study. Twenty-five (67.5%) infants had received complete antenatal steroid coverage and 8 (21.6%) partial steroid coverage. Median APGAR scores at 1 and 5 min were 7 and 8, respectively. At baseline, we assessed score for neonatal acute physiology with perinatal extension (SNAPPE-II). Median SNAPPE-II score was 20 (13,30). Overall, 32 (86%) infants had septic shock. Twenty six of the 37 infants in study (70%) had culture positive sepsis, and 6 (16.2%) infants had probable sepsis (blood culture negative). Two (6%) infants were on invasive respiratory support at onset of shock, i.e., at initial recording of IVC collapsibility index. Six (16.2%) infants with septic shock had hemodynamically significant patent ductus arteriosus (HsPDA). In the remaining 5 (14%) infants, hypovolemia was the reason for shock. Infants without features of sepsis but with clinical features of dehydration (significant weight loss), who responded only to fluid bolus/es, were diagnosed to have hypovolemic shock. The average age at enrollment of neonates is 4.2 days (± 2.4) (Table 1).
The mean blood pressure (MAP) and pulse pressures were 45 mm of Hg (± 4) and 28 mm of Hg (± 6), respectively. None of the infants in our cohort presented with hypotension. The mean blood gas pH was 7.20 ± 0.07, and the mean base excess was − 9.87 ± 2.53 at onset of shock. Only two (5%) infants were on invasive ventilation at the time of enrolment.
Echocardiographic parameters at onset of shock
-
1.
The median IVC collapsibility index was 42% (IQR: 23–48), IVC collapsibility index ≥ 50% was seen in 7 (18.9%) patients, and an IVC diameter ≤ 2.1 mm was seen in 2 (5.4%). The median LVEDV was 5.8 ml (IQR: 2.9–9.6).
-
2.
Median IVRT was 42 ms (IQR: 39–47), and the median E/A ratio was 0.77 (IQR: 0.7–0.8).
-
3.
The median LVO was 165 ml/kg/min (IQR: 115–213), and median RVO was 246 ml/kg/min (IQR: 181–298). The median left and right ventricular stroke volumes were 1 ml (IQR: 0.7–1.3) and 1.4 ml (IQR: 1.2–1.8), respectively. Median ejection fraction was 69% (IQR: 62–74). LVO < 130 ml/kg/min was present in 11 (29.7%) infants, and none of the infants had RVO < 130 ml/kg/min. Two (6.4%) infants were having EF <55%.
-
4.
The median SVR index was 0.27(IQR: 0.22–0.38) mmHg/ml/kg/min.
Four infants died before complete resolution of shock, and 2 infants got transferred to other centers. The time for complete resolution of shock was between 12 hours and 24 hours in 4 (13%) infants, between 24hours and 48 hours in 17 (55%) infants, between 48 hours and 72 hours in 9 (29%) infants, and more than 72 hours in 1 (3.2%) infant. Among the infants with complete resolution (n = 31) of shock, 27 (87%) infants received IV fluid as bolus, 29 (93.54%) infants received dopamine, 30 (96.77%) infants received dobutamine, and 4 (12.9%) infants received noradrenalin. Ten (32.2%) infants received steroids for the management of inotrope resistant shock. None of the infants received epinephrine, vasopressin, milrinone, or blood transfusion.
Based on initial clinical evaluation and complete clinical course, the etiology of shock was hypovolemia in 5 (13.5%) infants, cardiogenic in 3 (8.1%) infants, and mixed shock in 29 (78.3%) infants. Even though shock was diagnosed clinically as hypovolemic, these patients received low-dose inotrope/s initially for a brief period of time. Hemodynamically significant PDA at the time of shock was present in 6 (16.2%) infants. After echocardiographic evaluation, out of 37 infants, as per the existing definitions of shock, three (8.1%) infants were found to have hypovolemic shock, 8 (21.6%) infants were having cardiogenic shock, 11 (29.7%) infants were having mixed shock, and 15 (40.5%) infants were having distributive shock.
Changes in the heart rate, mean arterial pressure, IVC collapsibility, systolic (LSV, RSV, EF), diastolic ventricular function (IVRT), and SVR index are significant in the 31 infants evaluated for these parameters at and after resolution of shock (Fig. 2) (Table 2). The change in volume status was assessed by measuring changes in IVC collapsibility index and LVEDV. Twenty four (77.4%) infants had increase IVC collapsibility index at shock, and the median changed from 42% (IQR: 39–47) to 39 (IQR: 34–44) after resolution of shock. Reduced LVEDV was seen in 25 (80.6%) infants at shock, and the median LVEDV increased from 5.8(IQR: 2.9–9.6) to 8 (IQR: 5–13) after resolution of shock.
Box plot showing changes in echo parameters in paired analysis. [ICI1, ICI at shock. ICI2, ICI after resolution of shock. LVEDV1, LVEDV at shock. LVEDV2, LVEDV after resolution of shock. IVRT1, IVRT at shock. IVRT2, IVRT after resolution of shock. EF1, EF at shock. EF2, after resolution of shock. LSV1, LSV at shock. LSV2, LSV after resolution of shock. RSV1, RSV at shock. RSV2, RSV after resolution of shock.]
The change in diastolic function was assessed by measuring changes in IVRT and mitral E/A ratio. Twenty-four (77.4%) infants showed increased IVRT with the onset of shock, and the median decreased from 42 (IQR: 39–47) to 39 (IQR: 34–44) after shock resolution. Overall 20 (64.5%) infants showed increase in mitral E/A ratio. But this change in mitral E/A ratio was not statistically significant.
Changes in cardiac systolic function were assessed by measuring left ventricular output (LVO), right ventricular output (RVO), and ejection fraction (EF). There were 17 (54.8%) infants who showed reduced LVO and 16 (51.6%) infants who showed reduction in RVO at the onset of shock but neither were statistically significant. However, results are statistically significant when left and right ventricular stroke volumes (at shock and after resolution of shock) were subjected for paired data analysis (Table 2). Twenty-seven (87%) infants had reduced EF during shock and the median increased from 69 (IQR: 62–74) to 75 (IQR: 71–79) after resolution.
Systemic vascular resistance (SVR) index was computed with the formula: MAP/LVO [13, 14]. The changes in SVRI from onset of shock to complete shock resolution were not significant in the 31 infants, in whom it was evaluated.
Discussion
In this study, we enrolled 37 infants at onset of shock, and in 31 infants, we have data at and after resolution of shock. Using the most appropriate definition of shock, the incidence of shock in our study is 42 per 1000 infants admitted to NICU. Sepsis, PDA, and hypovolemia were the common reasons for shock in our study population. Mortality was only 4 (11%) in our study and is low when compared with other studies [10, 11]. Exclusive enrollment of inborn infants, early detection of shock, differences in the severity of shock, and aggressive management are some of the probable reasons for better outcomes in our study. None of the infants in present study had hypotension, whereas in the study by Saini et al., 63% infants had hypotension at presentation of shock [10]. All infants with shock in the present study had significant changes in HR, SBP, DBP, MAP, and pulse pressure at and after resolution of shock. As the previous two trials have noted the changes in the above parameters at onset and after 45 min to 1 h of starting inotropes, direct comparison of these changes with them is not appropriate [10, 11]. However, at the onset of shock, HR, SBP, DBP, and MAP were higher in the present study compared with studies done by Saini et al.10 and Baske et al.11.
In the present study, there were significant changes in ICI, LVEDV, IVRT, left ventricular stroke volume (LSV), right ventricular stroke volume (RSV), and EF at onset and after resolution of shock. The changes in LVO, RVO, and E/A ratio were not statistically significant. Increased heart rate at onset of shock compensated for decreased stroke volume; this may be the reason for non-significant changes in LVO and RVO in paired analysis. In general, LVO was less compared with RVO, and this may be due to delayed transition of cardiac hemodynamics from fetal to neonatal state, patent foramen ovale shunting blood from left to right and to the problem with the angle of insonation (which should be as close to 0° as possible) while calculating LVO [19]. Another explanation to this finding could be that LVO and RVO were calculated in different cardiac cycles. This finding from our study is similar to that reported by others [10, 19]. Changes in echo parameters cannot be compared with the other two studies as there was no control group in their studies [10, 11], and the changes reported by them at and after 45 to 1 h of inotropes are unlikely to be similar to our findings.
In this study, neither clinical nor echocardiographic parameters were able to differentiate the pathophysiology of shock based on the existing guidelines. There was an overlap of clinical and echocardiographic parameters of shock in almost all infants. This study demonstrated the changes in echocardiographic parameters and clinical parameters at and after resolution of shock (considered as baseline for the infant). These changes in clinical and echocardiographic parameters may be used to evaluate shock on the pathophysiological basis redefining the current guidelines.
From the findings in this study, we need to validate the pathophysiology of shock management in future studies by identifying at risk infants, evaluating echocardiographic parameters at baseline (after resolution of transitional circulation) and at onset of shock.
Uniform study protocol, standard definition of shock, assessment of clinical and echocardiographic parameters at onset and resolution of shock, cardiologist evaluating echocardiographic parameters blinded to the clinical details, and enrollment of infants with shock due to sepsis, hypovolemia, and PDA are the merits of this study.
Study limitations
Inclusion of only inborn infants and small sample size are the main limitations of this study. Non-invasive arterial blood pressure measurements [20, 21] and use of “M mode” method for EF calculation are the other limitations of this study. Echocardiographic parameters differ significantly among different types of shock, as evident from literature on adult population with shock [22, 23]. Our study did not demonstrate significant difference in echocardiographic parameters among different types of shock.
Conclusion
Neonatal shock is a state of complex pathophysiological process and has overlapping features irrespective of the etiology. Our study highlights the need for baseline documentation of clinical and echo parameters and to observe their changes at onset of shock. Future validation is needed to manage infants with shock based on the changes observed in this study.
Abbreviations
- CRT:
-
Capillary refilling time
- EF:
-
Ejection fraction
- EF1:
-
EF at shock
- EF2:
-
After resolution of shock
- E/A ratio:
-
Mitral valve E wave to A wave ratio
- HR:
-
Heart rate
- ICI:
-
Inferior vena cava collapsibility index
- ICI1:
-
ICI at shock
- ICI2 :
-
ICI after resolution of shock
- IVC:
-
Inferior vena cava
- IVRT:
-
Isovolemic ventricular relaxation time
- IVRT1:
-
IVRT at shock
- IVRT2 :
-
IVRT after resolution of shock
- LSV:
-
Left ventricular stroke volume
- LSV1:
-
LSV at shock
- LSV2 :
-
LSV after resolution of shock
- LVEDV:
-
Left ventricular end diastolic volume
- LVEDV1:
-
LVEDV at shock
- LVEDV2:
-
LVEDV after resolution of shock
- LVO:
-
Left ventricular output
- MAP:
-
Mean arterial pressure
- NICU:
-
Neonatal intensive care unit
- RSV:
-
Right ventricular stroke volume
- RSV1:
-
RSV at shock
- RSV2 :
-
RSV after resolution of shock
- RVO:
-
Right ventricular output
- SVR:
-
Systemic vascular resistance
References
Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc 6(1):2–8
Giliberti P, Giordano L, Chello G, De Leonibus C, Giliberti P (2010) The scenarios of shock in newborn infants. 23(Suppl 3):27
Sinniah D, Subramaniam T, MyintSoe-Hsiao M (2013) Shock in the neonate. IeJSME 7(2):17–28
de Cássia SR, Clarice G, Soibelmann PR (2010) Sepsis and septic shock in the neonatal period: updating and review of concepts. Rev Bras Tue Intensive. [cited 2020 May 04]; 22(3):280–290. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-507X2010000300011&lng=pt. https://doi.org/10.1590/S0103-507X2010000300011
Sehgal A, McNamara P (2008) Does point-of-care functional echocardiography enhance cardiovascular care in the NICU? J Perinatol 28:729–735. https://doi.org/10.1038/jp.2008.100
Soleymani S, Borzage M, Seri I (2010 Oct) Hemodynamic monitoring in neonates: advances and challenges. J Perinatol Off J Calif Perinat Assoc. 30(Suppl):S38–S45
Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, Sanchez-de-Toledo J, Brierley J, Colunga JM, Raffaj D, da Cruz E, Durand P, Kenderessy P, Lang HJ, Nishisaki A, Kneyber MC, Tissieres P, Conlon TW, de Luca D (2020) International evidence-based guidelines on point of care ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24:65. https://doi.org/10.1186/s13054-020-2787-9
de Boode WP, van der Lee R, Horsberg Eriksen B et al (2018) The role of neonatologist performed echocardiography in the assessment and management of neonatal shock. Pediatr Res 84(Suppl 1):57–67. https://doi.org/10.1038/s41390-018-0081-1
Seri I (2001) Neonatal shock: etiology, pathophysiology and management. Prenat Neonatal Med 6. https://doi.org/10.1080/13598630108500263
Saini SS. Hemodynamic changes in preterm neonates with septic shock: a prospective observational study*. - PubMed - NCBI. [cited 2019 Jun 20]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/24717905
Baske K, Saini SS, Dutta S, Sundaram V (2018) Epinephrine versus dopamine in neonatal septic shock: a double-blind randomized controlled trial. Eur J Pediatr 177(9):1335–1342
Deshpande SA, Platt MP (1997) Association between blood lactate and acid-base status and mortality in ventilated babies. Arch Dis Child Fetal Neonatal Ed 76(1):F15–F20. https://doi.org/10.1136/fn.76.1.f15
Ma M, Noori S, Maarek J-M, Holschneider DP, Rubinstein EH, Seri I (2015) Prone positioning decreases cardiac output and increases systemic vascular resistance in neonates. J Perinatol Off J Calif Perinat Assoc 35(6):424–427
Stark MJ, Clifton VL, Wright IMR (2008) Microvascular flow, clinical illness severity and cardiovascular function in the preterm infant. Arch Dis Child Fetal Neonatal Ed 93(4):F271–F274
Walther FJ, Siassi B, King J, Wu PYK (1986) Echocardiographic measurements in normal preterm and term neonates. Acta Paediatr 75(4):563–568
Washio Y, Uchiyama A, Nakanishi H, Totsu S, Masumoto K, Kusuda S (2013 Oct) Hemodynamic analysis in infants with late-onset circulatory collapse. Pediatr Int Off J Jpn Pediatr Soc 55(5):582–588
van Laere D, van Overmeire B, Gupta S, El Khuffash A, Savoia M, McNamara PJ et al (2018) Application of NPE in the assessment of a patent ductus arteriosus. Pediatr Res 84(Suppl 1):46–56
Kieliszczyk J, Baranowski W, Kosiak W (2016) Usefulness of ultrasound examination in the evaluation of a neonate’s body fluid status. J Ultrason 16(65):125–134
Meyer S, Todd D, Shadboldt B (2010) Non-invasive cardiac output monitoring in neonates. Arch Dis Child Fetal Neonatal Ed 95(6):F464–F464
Dannevig I, Dale HC, Liestøl K, Lindemann R (2005) Blood pressure in the neonate: three non-invasive oscillometric pressure monitors compared with invasively measured blood pressure. Acta Paediatr 94:191–196. https://doi.org/10.1111/j.1651-2227.2005.tb01889.x
Werther T, Aichhorn L, Baumgartner S, Berger A, Klebermass-Schrehof K, Salzer-Muhar U (2018) Discrepancy between invasive and non-invasive blood pressure readings in extremely preterm infants in the first four weeks of life. PLoS One 13(12):e0209831. https://doi.org/10.1371/journal.pone.0209831
McLean AS (2016) Echocardiography in shock management. Crit Care 20:275. https://doi.org/10.1186/s13054-016-1401-7
De Backer D, Giglioli S (2020) Echocardiographic approach to shock. J Emerg Crit Care Med [Online], 3 (2019): n.pag. Web. 10 JUL. 2020. https://jeccm.amegroups.com/article/view/5264
Author information
Authors and Affiliations
Contributions
Dr Dinesh Pawale was a Principal Investigator who collected all data, drafted initial manuscript and revised the manuscript. Dr Srinivas Murki conceptualised and designed study, critically reviewed the manuscript and approved the final version of manuscript. Dr Dattatray Kulkarni helped in data collection and manuscript writing. Dr Venkateshwarlu Vardhelli helped in identifying subjects and managment and anlysis of data. Dr Deepak Sharma helped in developing protocol and drafting initial manuscript. Dr Tejopratap Oleti helped in designing study, drafting initial protocol and reviewed final version of manuscript. Dr Sai Kiran coordinated data collection and data analysis and critically reviewed manucript. Dr Shweta Bakhru analysed all stored echocardiograhic data and reviewed final manuscript. Dr Nageswar Rao Koneti reviewed echocardiographic data, helped in drafting intitial manuscript and analysis of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. Ethics approval obtained from the Institute’s Ethics Committee (Ec Ref No- 25_2017).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Pawale, D., Murki, S., Kulkarni, D. et al. Echocardiographic assessment of hemodynamic changes in preterm neonates with shock: a prospective pragmatic cohort study. Eur J Pediatr 179, 1893–1899 (2020). https://doi.org/10.1007/s00431-020-03775-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03775-5