Abstract
To assess the efficacy of double phototherapy in managing neonatal jaundice compared to single phototherapy in infants with different birth weight and gestational age. CENTRAL, PubMed, clinicaltrials.gov, and gray literature sources were searched from date of inception of these databases till August 2019. Primary outcome was decline of total serum bilirubin (TSB) per hour. Ten studies were eligible. Our meta-analysis showed significant difference between double phototherapy versus single phototherapy in decline of TSB per hour in preterm infants (standardized mean difference [SMD] = 2.28 [0.79–3.76], p = 0.003) and a significant decrease in TSB levels at 24 h of phototherapy in infants with birth weight ≥ 1500 g (mean difference [MD] = − 61.70 μmol/L, [− 107.96, − 15.43], p = <0.001).
Conclusion: Double phototherapy is effective in reducing TSB in infants of different gestational ages and birth weights with the most important finding regarding preterm infants, who are more susceptible to kernicterus.
What is Known: • Double phototherapy has shown to be more efficacious than single phototherapy in treating neonatal jaundice. • Double phototherapy efficacy on neonates with different gestational ages and birth weights still remain ambiguous in treating neonatal jaundice. What is New: • The results of this meta-analysis show that double phototherapy is effective in reducing TSB in infants of different gestational ages and birth weights with the most important finding regarding preterm infants, who are more susceptible to kernicterus. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Jaundice or hyperbilirubinemia is a common physiologic or pathologic disorder affecting over 60% of full-term and 80% of preterm babies [1]. Neonatal jaundice is caused by an excess of bilirubin in the blood [2]. Neonatal jaundice is hazardous as excess bilirubin is toxic to the basal ganglia and various brain stem nuclei [3]. Clinical manifestation of bilirubin toxicity during the first few weeks of life is denoted as acute bilirubin encephalopathy while chronic or permanent damage to the brain is denoted as kernicterus [3]. Preterm and low birth weight infants are more susceptible to kernicterus at a lower threshold of TSB (total serum bilirubin) as compared to term and normal birth weight infants [4].
The current standard for treatment of neonatal jaundice is phototherapy, owing to its safety and efficacy [3]. Phototherapy employs the use of light sources, usually LED’s (light-emitting diodes), emitting light in the blue and green spectra [2]. These wavelengths of light convert bilirubin to less toxic water-soluble photo isomers that can be safely excreted in the bile and urine [5]. Factors that influence the efficacy of phototherapy are the spectrum of light, the irradiance, and the surface area of skin exposed at any one time [6]. Types of phototherapy commonly used include single and double phototherapy with the major difference being simultaneous use of an additional phototherapy unit in the latter [7]. The two interventions also differ in surface area of exposure and intensity of light [7].
To the best of our knowledge, there has been no systematic review and meta-analysis published yet assessing the clinical evidence on the efficacy of double phototherapy against single phototherapy in management of neonatal jaundice in term and preterm, and among infants of different birth weights. This present study aims to review clinical evidence currently available and construct a meta-analysis to visualize the overall effects of double phototherapy versus single phototherapy.
Materials and methods
Data sources
This systematic review with meta-analysis was performed in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [8]. Two reviewers (MAN and ASA) separately searched from the following databases: Cochrane Library (CENTRAL), PubMed Central (MEDLINE), and National Library of Medicine (NLM) Clinical Trials library.
Literature search
Relevant studies were searched from the date of inception of the mentioned databases until August 2019. The following Medical Subject Headings (MeSH) terms were used: “Intensive Phototherapy,” “Double Intensive,” “Single Intensive,” “Fiberoptic,” “Phototherapy,” “Neonatal Jaundice,” “High Intensity,” “Double Surface,” “Hyperbilirubinemia,” “Double-sided,” “High Irradiance.” Reference lists of relevant review and original articles were assessed for any missed articles during the database searches. Any disagreements between the two reviewers were consulted with a third reviewer (ASL) until consensus was achieved. All articles extracted were compiled into Endnote X7 (Clarivate Analytics, PA) where duplicates were identified and removed.
Eligibility criteria
Articles were included in the study if they met the following set of eligibility criteria: (1) full-text available; (2) neonates only (age ≤ 1 month); (3) at least one outcome reported to be included in the meta-analysis; (4) both irradiance setting and phototherapy setting should be reported and no indications for exchange transfusion in participants prior to intervention; (5) no congenital anomalies; (6) phototherapy duration of at least 12 h. There was no language restriction. Case reports and editorials were excluded.
Data extraction
Three reviewers (MMH, SAS, and NAB) separately extracted data on standardized data collection forms from selected articles. Extracted characteristics and outcome data included first author’s name, year of publication, location of studies, total participants, and their specific characteristics (preterm/term and birth weight), study design, phototherapy settings, irradiance settings, decline of TSB per hour, duration of phototherapy, TSB levels at 24 h, length of hospitalization, and summary of results. Our primary endpoint was decline of TSB per hour and our secondary endpoints were TSB levels at 24 h from initiation of phototherapy, duration of phototherapy, and length of hospital stay. Any disagreement during extraction was resolved with discussion.
Risk of bias assessment
For quality assessment of randomized controlled trials (RCTs), Cochrane Collaboration’s risk of bias tool was used [9]. This tool evaluated the risk of bias within studies on the basis of 7 domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. For quality assessment of non-randomized controlled trials (NRCTs) and case-control studies, we used Risk of Bias in Non-randomized Studies - of Interventions (ROBINS-I) tool [10]. This tool assesses the risk of bias within studies on the basis of 7 key domains: confounding, selection bias, classification of interventions, reporting bias, deviations from interventions, missing data, and measuring outcome.
Statistical methods
All statistical analyses were executed using Review Manager (RevMan) (Version 5.3.5; Cochrane Collaboration, Oxford, UK) [11], and Stata Statistical Software: Release 13 (College Station, TX: StataCorp LP) [12]. Continuous data was presented as standardized mean difference (SMD), mean difference (MD), and 95% confidence interval (CI). Decline of TSB per hour and TSB levels at 24 h were pooled using a random-effects model. Both analyses were divided into the following subgroups: term, preterm, studies including infants with birth weight ≤ 2500 g, birth weight ≥ 2500 g, birth weight ≥ 1500 g. In the present study, some included studies did not provide decline of TSB per hour; hence, it was calculated from decline rate of TSB at 24 h by dividing the TSB levels at 24 h by 24 h. For assessment of heterogeneity the Higgins I2 statistic was used, in which, a value of I2 = 25–50% is mild, 50–75% is moderate, and > 75% is severe [13]. A p value of less than 0.05 was considered significant for all analyses. Egger’s regression test was performed to investigate publication bias [14]. Sensitivity analyses was done to investigate heterogeneity such as leave one out sensitivity analysis and random effects model meta-regression. Gestational age may be a potential confounder in our analyses. However, it has been reported previously that gestational age has no significant effect in response to phototherapy [15]. For a robust sensitivity analysis, we performed a random-effects model meta-regression in which we used the mean gestational age as a covariate. Repeated studies with the same dataset occurring in separate subgroups were excluded before assessing publication bias and heterogeneity.
Results
Search results
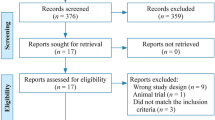
A total of 885 potential articles were identified through database search, from which 812 articles were retained after duplicates were removed. Articles were further excluded (n = 787) if they were abstracts only (n = 10), results were not reported (n = 2) or had irrelevant titles (n = 775). Out of twenty-five remaining articles, full-texts were assessed and fifteen articles were excluded for not measuring irradiance (n = 4), did not include only neonates (n = 1), were case reports (n = 2), had irrelevant interventions (n = 7), and had duration of phototherapy of less than 12 h (n = 1). This resulted in a final sample of ten articles in the systematic review and meta-analysis. The PRISMA flow chart (Fig. 1) outlines the literature search process.
Characteristics of included studies
Study characteristics of included studies are summarized in Table 1. Out of ten studies selected, six were randomized controlled trials, three were non-randomized controlled trials and only one was a case-control study. For the double phototherapy setting, four studies used fiberoptic pads/blankets, three studies used a setting in which there was a single panel (similar to the single phototherapy setting) alongside an addition panel placed at a different angle, one study used a fluid bed and another study increased the number of lamps and changed from white halogen lamps to blue fluorescent tubes. Seven studies reported decline of TSB per hour, five studies reported TSB levels at 24 h, three studies reported the duration of phototherapy, and only two studies reported length of stay.
Risk of bias in included studies
None of the six randomized controlled trials reported blinding of outcome assessors. However, one article had high risk of allocation concealment. Only one trial reported plausible effect size. Supplementary figure 1 and 2 show the risk of bias within these RCTs. Out of three NRCTs and one case control, only one had low risk, while another had a serious risk of bias. Supplementary table shows the risk of bias within these studies.
Decline of TSB per hour
A total of seven studies were included in the pooled analysis reported this outcome. (Fig. 2) The analysis of this outcome was divided into subgroups; preterm, term, birth weight ≥ 2500 g, birth weight ≥ 1500 g, and birth weight ≤ 2500 g. Preterm had a total of three studies which significantly favored double phototherapy over single phototherapy (SMD = 2.28, 95% CI = 0.79–3.76, p = 0.003, I2 = 91%). Term included four studies in which double phototherapy had a significant difference when compared to single phototherapy (SMD = 2.01, 95% CI = 0.93–3.10, p ≤0.001, I2 = 97%). In the subgroup, infants with birth weight ≥ 2500 g had three studies that significantly favored double phototherapy (SMD = 2.07, 95% CI = 0.62–3.52, p = 0.005, I2 = 97%). Only two studies included infants whose birth weight was less than 2500 g which also significantly favored double phototherapy over single phototherapy (SMD = 1.70, 95% CI = 0.25–3.15, p = 0.02, I2 = 89%). There were five studies in the subgroup birth weight ≥ 1500 g in which double phototherapy also had a highly significant difference when compared to single phototherapy (SMD = 1.35, 95% CI = 0.65–2.05, p ≤ 0.001, I2 = 94%). Overall effect size of these subgroups was significant towards double phototherapy (SMD = 1.78, 95% CI = 1.36–2.21, p = <0.001). However, there was an overall substantial heterogeneity present (I2 = 94%). Overall subgroup differences showed that there was no heterogeneity between the subgroups (I2 = 0%).
TSB levels at 24 h
Total five studies were included in the pooled analysis which reported this outcome. (Fig. 3) The analysis was divided into subgroups; term, birth weight ≥ 2500 g, birth weight ≥ 1500 g, and birth weight ≤ 2500 g. Three studies that included term infants only showed a greater reduction of TSB at 24 h in the double phototherapy group than single phototherapy group (MD = − 51.75 μmol/L, 95% CI = − 107.81, 4.31, p = 0.07, I2 = 97%) although it was not statistically significant. Birth weight ≥ 2500 g had only two studies included also showing greater reduction in TSB levels at 24 h in the double phototherapy group, however, it was not statistically significant (MD = − 62.61 μmol/L, 95% CI = − 151.79, 26.57, p = 0.17, I2 = 98%). In birth weight ≤ 2500 g, only one study was present, in which the TSB levels at 24 h were significantly lower than single phototherapy (MD = − 67.00 μmol/L, 95% CI = − 82.74, − 51.26, p ≤ 0.001). Four studies that included infants with birth weight ≥ 1500 g had a significant decrease in TSB levels in 24 h in double phototherapy compared to single phototherapy (MD = − 61.70 μmol/L, 95% CI = − 107.96, − 15.43, p ≤ 0.001, I2 = 97%). Overall effect between the subgroups showed a greater reduction of TSB levels at 24 h, significantly favoring double phototherapy over single phototherapy (MD = − 59.42 μmol/L, 95% CI = − 85.32, − 33.52, p ≤ 0.001, I2 = 96%). Subgroup difference shows that there was no heterogeneity present between the subgroups (I2 = 0%).
Duration of phototherapy
Three studies reported duration of phototherapy [17, 19, 25]. The analysis was divided into subgroups; preterm, term, birth weight ≥ 1500 g, and birth weight ≤ 2500 g. Both subgroups of preterm and birth weight ≤ 2500 g consisted of only one study in which there was a significant outcome favoring double phototherapy. (MD = − 43.50 h, 95% CI = − 63.00, − 24.00, p ≤ 0.001). Similarly, both subgroups of term and birth weight ≥ 1500 g, which consisted of only two studies in each, favored double phototherapy significantly in reducing phototherapy duration. (MD = − 9.71 h, 95% CI = − 15.21, − 4.20, p = <0.001). The total overall effect size favored significantly towards double phototherapy than single phototherapy (MD = − 16.67 h, 95% CI = − 24.26, − 9.08, p ≤ 0.001). However, there was considerable heterogeneity between the subgroups (I2 = 86%). (Supplementary Fig. 3).
Length of hospital stay
Two studies reported length of hospital stay [23, 25]. The pooled analysis showed that double phototherapy significantly favored in reduction of hospital stay than single phototherapy (MD = − 18.30 h, 95% CI = − 25.95, − 10.65, p ≤ 0.001, I2 = 14%). (Supplementary Fig. 4).
Additional analysis
Egger regression showed no publication bias present in decline in TSB per hour (p = 0.206) and TSB levels at 24 h (p = 0.636). A sensitivity analysis was performed in which only RCTs were included. This did not significantly change the total overall effect size of our primary endpoint. However, in the subgroups; preterm, birth weight ≥ 2500 g, and birth weight ≥ 1500 g the outcome was still favoring double phototherapy but not significantly. Secondary endpoints did not significantly change when RCTs were only included in the analysis. Meta-regression analyses showed that the gestational age was not significantly associated with the effect size of double phototherapy on decline of TSB per hour (coefficient = 0.686, 95% CI = − 1.65, − 0.302, p = 0.541) and TSB levels at 24 h (coefficient = − 0.183, 95% CI = − 0.383, 0.346, p = 0.911). Leave one out sensitivity analysis was done for the meta-analyses performed in which there was no significant change in overall estimate when each particular study was omitted except when Kang et al. was omitted from TSB levels at 24 h the results favored double phototherapy but non-significantly. (Supplementary Figure 5 and 6).
Discussion
Our meta-analysis of total 1104 participants shows that the decline of TSB per hour and TSB levels at 24 h overall significantly favored double phototherapy. A notable finding involving preterm infants was a substantial difference in the decline of TSB per hour during double phototherapy as compared to single phototherapy.
Preterm infants have a higher chance to develop jaundice than term infants [2]. Double phototherapy does play a beneficial role in reducing high bilirubin levels in preterm infants at a faster rate than single phototherapy.
Studies including infants with birth weight ≥ 1500 g and ≤ 2.500 g only showed commendatory outcome in decline of TSB per hour and TSB levels at 24 h towards double phototherapy in the present study. Our results point towards double phototherapy being more advantageous over single phototherapy in infants with low birth weight. A multicenter randomized trial by Morris et al. [26] which included 1974 participants compared aggressive phototherapy versus conventional phototherapy by means of increasing irradiance. It stratified the participants into two subgroups: 501–700 g and 701–1000 g. The trial concluded that it did not find any significant difference in risk of impaired neurodevelopment between aggressive and conventional phototherapy in both the subgroups. Low birth weight infants seem to benefit with the use of high irradiance double phototherapy with little to no risk [27].
Our systematic review showed that all the studies that reported duration of phototherapy favored double phototherapy. This is a valuable finding as a reduction in time of phototherapy decreases the use of phototherapy equipment per patient which can reduce electrical consumption. This can also increase availability of staff and phototherapy equipment where resources are limited and there is a busy patient inflow. Additionally, this can also be attributed to the length of hospital stay decreasing with double phototherapy, as described in our findings.
In the present study, nine studies adopted double phototherapy setting while increasing surface area exposure [16,17,18,19,20,21,22, 24, 25]. By providing greater surface exposure, emitted light has a higher chance to breakdown bilirubin proficiently and at a faster pace. This finding supports those guidelines that recommend greater skin exposure for effective phototherapy [1, 3].
It is known that high irradiance tends to deplete TSB levels at a faster rate [28] and the studies that we observed generally showed a higher irradiance in double phototherapy than single phototherapy.
Some studies included in our meta-analysis used halogen lamps. When dealing with halogen lights, decreasing distance should be managed with caution as they can cause skin burns. Instead, as a preferred alternative, LEDs or fluorescent tubes are considered innocuous if brought close to the skin [29,30,31]. LEDs have proved to be more purposive by reducing side effects, consuming considerably less energy and having a greater lifespan. A simple installment of LEDs, which cost lower than fluorescent or halogen lights, can prove to be beneficial in treatment of neonatal jaundice for families or health care centers looking to be more cost-effective [32,33,34]. Despite this, in our meta-analysis only one included study opted for the use of LED’s. Clinicians opting for either single or double phototherapy in managing neonatal hyperbilirubinemia should consider type of light source cautiously with regard to its side effects and cost effectiveness.
Side effects of phototherapy can include retinal damage, burns, disturbed circadian rhythm, conjunctivitis, rashes, dehydration, hyper- and hypothermia, loose stools, patent ductus arteriosus, melanotic nevus, bronze baby syndrome, and electrolyte disturbances [35]. However, in almost all the studies, no side effects were observed, except Donneborg et al. [24], which observed loose stools. Boonyarittipong et al. [20] reported that loose stools were significantly higher in the single phototherapy group without a given reason, though it did not significantly affect the body weight. Kang et al. [17] and Boonyarittipong et al. [20] reported that weight loss was mostly observed in the single phototherapy group with no particular reason specified. Only Al-Hafidh et al. [23] reported the need for blood exchange transfusion due to failure of phototherapy in which the study showed that 91.66% of participants in the single phototherapy group underwent exchange transfusion while 0% of participants in the double phototherapy group underwent exchange transfusion. A separate study conducted by Granati et al. [36] reported a follow up after 6 years assessing the adverse effects of high surface area exposure phototherapy which concluded that such a phototherapy setting is safe and effective in management of neonatal jaundice.
Increasing the intensity of phototherapy has been reported to cause imbalance on oxidative and antioxidative capacity thus increasing oxidative stress [37]. This is supported by a randomized clinical trial by El-Farrash et al. [38] including 120 neonates which found that intensive phototherapy had greater oxidative stress markers when compared with conventional phototherapy. However, none of the included studies assessed oxidant/antioxidant status hence these effects also need to be addressed when conducting intensive phototherapy over conventional.
Biological plausibility
It is well-known that an increase in exposed body surface area, at the same irradiance level, would increase the spectral power by its definition. In the treatment of neonatal jaundice an increase in spectral power would cause a greater widespread serum bilirubin degradation into its metabolites that would lead to a rapid decline in total serum bilirubin [39]. Double phototherapy implication in treating neonatal jaundice would provide these results than single phototherapy due to its high spectral power making single phototherapy inferior in providing rapid decline of total serum bilirubin. A meta-analysis by Tridente et al. [40] discussed that an included RCT by Kumar et al. [41] showed that there was no significant difference when irradiance was increased and spectral power was unchanged. The trial showed that increasing spectral power than irradiance would provide a greater efficacious outcome.
Limitations were present in our study. Firstly, not all studies included were randomized controlled trials. There was substantial variation between the irradiance between the included studies. In the pooled analysis of “decline of TSB per hour” and “TSB levels at 24 hours” there was considerable heterogeneity within the subgroups. Rate of TSB decline per hour was not reported by some of the studies despite being important clinical indicators for assessing efficiency of phototherapy. Funnel plots could not be performed due to studies included in all the meta-analyses being less 10 than [42]. Meta-regressions for duration of phototherapy and length of hospital stay could not be performed due to studies being less than 10 in the meta-analyses [43].
Conclusions
Double phototherapy is superior to single phototherapy when achieving a faster decline of TSB per hour and lower TSB levels at 24 h from initiation of phototherapy in infants who are term, preterm and having birth weight ≥ 2500 g, ≥ 1500 g, and ≤ 2500 g. It also reduces hospital stay and duration of treatment. However, caution and patient safety should be considered when employing double phototherapy and implementation should be based on clinicians’ assessment. Future multicenter randomized controlled trials can assess the adverse effects of double phototherapy with regard to gestational age and birth weight of infants for a more supporting clinical evidence.
Abbreviations
- CI:
-
Confidence interval
- LED:
-
Light-emitting diode
- MD:
-
Mean difference
- RCT:
-
Randomized controlled trial
- SMD:
-
Standardized mean difference
- TSB:
-
Total serum bilirubin
References
Overview | Jaundice in newborn babies under 28 days | Quality standards | NICE. Nice.org.uk. https://www.nice.org.uk/guidance/qs57. Published 2014. Accessed 1 Oct 2019
Infant jaundice - diagnosis and treatment - Mayo Clinic. Mayoclinic.org. https://www.mayoclinic.org/diseases-conditions/infant-jaundice/diagnosis-treatment/drc-20373870. Published 2016. Accessed 1 Oct 2019
Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114(1):297–316. doi:https://doi.org/10.1542/peds.114.1.297
Bhutani V, Wong R. UpToDate. Uptodate.com. https://www.uptodate.com/contents/hyperbilirubinemia-in-the-preterm-infant-less-than-35-weeks-gestation. Published 2018. Accessed 1 Oct 2019
Porter M, Dennis M. Hyperbilirubinemia in the Term Newborn. Aafp.org. https://www.aafp.org/afp/2002/0215/p599.html. Published 2000. Accessed 1 Oct 2019
Maisels M (1996) Why use homeopathic doses of phototherapy? Pediatrics. 98(2):283–287 https://pediatrics.aappublications.org/content/98/2/283. Accessed 1 Oct 2019
Hansen T. Neonatal jaundice treatment & management: approach considerations, medical care, diet. Emedicine.medscape.com. https://emedicine.medscape.com/article/974786-treatment#d6. Published 2015. Accessed 1 Oct 2019
Moher D, Liberati A, Tetzlaff J, Altman D (2009) Preferred Reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097
Higgins JP, Green S (2011) Cochrane handbook for systematic reviews of interventions. Wiley, New York Accessed 1 Oct 2019
JAC S, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JPT (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014
StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in metaanalyses. BMJ. 327(7414):557–560
Egger M, Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ. 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
TAN K (1977) The influence of gestational age and birth weight on the infant response to phototherapy for neonatal hyperbilirubinaemia. J Paediatr Child Health 13(1):22–24
Holtrop P, Ruedisueli K, Maisels M (1992) Double Versus single phototherapy in low birth weight newborns. Pediatrics. 90(5):674–677 https://pediatrics.aappublications.org/content/90/5/674. Accessed 1 Oct 2019
Kang J, Shankaran S (1995) Double phototherapy with high irradiance compared with single phototherapy in neonates with hyperbilirubinemia. Am J Perinatol 12(03):178180. https://doi.org/10.1055/s-2007-994446
Garg A, Prasad R, Hifzi A (1995) A controlled trial of high-intensity double-surface phototherapy on a fluid bed versus conventional phototherapy in neonatal jaundice. Pediatrics. 95(6):914–916 https://pediatrics.aappublications.org/content/95/6/914. Accessed October 1, 2019
Uit Sarici S, Alpay F, Unay B, Ozcan O, Gokcy E (2000) Double versus single phototherapy in term newborns with significant hyperbilirubinemia. J Trop Pediatr 46(1):36–39. https://doi.org/10.1093/tropej/46.1.36
Boonyarittipong P, Kriangburapa W, Booranavanich K (2008) Effectiveness of double-surface intensive phototherapy versus single-surface intensive phototherapy for neonatal hyperbilirubinemia. J Med Assoc Thail 91(1):50–55 https://www.ncbi.nlm.nih.gov/pubmed/18386544. Accessed October 1, 2019
Silva I, Luco M, Tapia J et al (2009) Single vs. double phototherapy in the treatment of fullterm newborns with nonhemolytic hyperbilirubinemia. J Pediatr 85(5):455458. https://doi.org/10.2223/JPED.1927
Milyana N, Tjipta G, Ali M et al (2011) Effectiveness of single and double phototherapy on indirect hyperbilirubinemia in neonates. Paediatr Indones 51(6):316–321. https://doi.org/10.14238/pi51.6.2011.316-21
Al-Hafidh N, Ali Z, Saeed R (2013) Double-surface intensive phototherapy versus single-surface conventional phototherapy in treatment of neonatal hyperbilirubinemia. Ann Coll Med Mosul 39(1):25–31. https://doi.org/10.33899/mmed.2013.75912
Donneborg M, Vandborg P, Hansen B, Rodrigo-Domingo M, Ebbesen F (2017) Double versus single intensive phototherapy with LEDs in treatment of neonatal hyperbilirubinemia. J Perinatol 38(2):154–158. https://doi.org/10.1038/jp.2017.167
Arnolda G, Chien T, Hayen A et al (2018) A comparison of the effectiveness of three LED phototherapy machines, single- and double-sided, for treating neonatal jaundice in a low resource setting. PLoS One 13(10):e0205432. https://doi.org/10.1371/journal.pone.0205432
Morris B, Oh W, Tyson J et al (2008) Aggressive vs. Conservative phototherapy for infants with extremely low birth weight. N Engl J Med 359(18):1885–1896. https://doi.org/10.1056/nejmoa0803024
Maisels M. Treatment of jaundice in low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2003;88(6):459F-463. doi:https://doi.org/10.1136/fn.88.6.f459
Hart G (2005) The importance of irradiance and area in neonatal phototherapy. Arch Dis Child Fetal Neonatal Ed 90(5):F437–F440. https://doi.org/10.1136/adc.2004.068015
Vandborg P, Hansen B, Greisen G, Ebbesen F (2012) Dose-response relationship of phototherapy for hyperbilirubinemia. Pediatrics. 130(2):e352–e357. https://doi.org/10.1542/peds.2011-3235
Pratita W, Supriatmo S, Tjipta G (2016) Phototherapy for neonatal jaundice at distances of 20 cm vs 40 cm. Paediatr Indones 53(5):278. https://doi.org/10.14238/pi53.5.2013.27882
Cline B, Vreman H, Faber K et al (2013) Phototherapy device effectiveness in Nigeria: irradiance assessment and potential for improvement. J Trop Pediatr 59(4):321325. https://doi.org/10.1093/tropej/fmt027
Yilmaz A, Ozkiraz S, Akcan A, Canpolat M (2015) Low-cost home-use light-emitting-diode phototherapy as an alternative to conventional methods. J Trop Pediatr 61(2):113118. https://doi.org/10.1093/tropej/fmu076
McBride B. Comparing LED vs CFL vs incandescent light bulbs. Viribright® LED light bulbs. https://www.viribright.com/lumen-output-comparing-led-vs-cfl-vsincandescent-wattage/. Accessed 1 Oct 2019
M.K. M, Khan S, Saldanha P, Mohamed R (2017) Comparison of light emitting diode and compact fluorescent lamp phototherapy in treatment of neonatal hyperbilirubinemia. Int J Contemp Pediatr 4(2):341–345. https://doi.org/10.18203/2349-3291.ijcp20170083
Xiong T, Qu Y, Cambier S, Mu D (2011) The side effects of phototherapy for neonatal jaundice: what do we know? What should we do? Eur J Pediatr 170(10):12471255. https://doi.org/10.1007/s00431-011-1454-1
Granati B, Largajolli G, Rubaltelli F, Pollazzon P, Bottos M, Sartori E (1984) Efficacy and safety of the “integral” phototherapy for neonatal hyperbilirubinemia. Clin Pediatr (Phila) 23(9):483–486. https://doi.org/10.1177/000992288402300905
Gathwala G, Sharma S (2000) Oxidative stress, phototherapy and the neonate. Indian J Pediatr 67(11):805–808. https://doi.org/10.1007/bf02726223
El-Farrash R, El-Shimy M, Tawfik S et al (2019) Effect of phototherapy on oxidant/antioxidant status: a randomized controlled trial. Free Radic Res 53(2):179–186. https://doi.org/10.1080/10715762.2018.1549364
Stokowski L (2011) Fundamentals of Phototherapy for Neonatal Jaundice. Adv Neonatal Care 11:S10–S21
Tridente A, De Luca D (2012) Efficacy of light-emitting diode versus other light sources for treatment of neonatal hyperbilirubinemia: a systematic review and meta-analysis. Acta Paediatr 101(5):458–465
Kumar P, Murki S, Malik G, Chawla D, Deorari A, Karthi N et al (2010) Light-emitting diodes versus compact fluorescent tubes for phototherapy in neonatal jaundice: A multi-center randomized controlled trial. Indian Pediatr 47(2):131–137
Lau J, Ioannidis J, Terrin N, Schmid C, Olkin I (2006) The case of the misleading funnel plot. BMJ 333(7568):597–600. https://doi.org/10.1136/bmj.333.7568.597
9.6.4 Meta-regression [Internet]. Handbook-5-1.cochrane.org. 2019 [cited 12 January 2020]. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_6_4_meta_regression.htm
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MMH, SAS, NAB, and ASL. The first draft of the manuscript was written by MAN and ASA and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 121 kb)
Rights and permissions
About this article
Cite this article
Nizam, M.A., Alvi, A.S., Hamdani, M.M. et al. Efficacy of double versus single phototherapy in treatment of neonatal jaundice: a meta-analysis. Eur J Pediatr 179, 865–874 (2020). https://doi.org/10.1007/s00431-020-03583-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03583-x