Abstract
Positional plagiocephaly (PP) denotes flattening of the skull that occurs frequently in healthy infants. Aim of this study was to estimate the prevalence of positional plagiocephaly and to identify the risk factors in a cohort of healthy infants in order to help prevention of PP. In a prospective design, all healthy full-term infants, ranging from 8 to 12 weeks of age, who presented at the public immunization clinic in Ferrara, were eligible for the study. After obtaining informed consent, we interviewed the parents and examined the infants using the Argenta’s assessment tool. Of 283 infants examined, 107 (37.8%) were found to have PP at 8–12 weeks of age. In 64.5%, PP was on the right side, 50.5% were male and 15% presented also with brachycephaly. Risk factors significantly associated were lower head circumference, advanced maternal age, Italian compared to African, and supine sleep position, in particular for infants born at 37 weeks, preference for one side of the head. In logistic regression, risk factors significantly associated were lower birth weight, advanced maternal age, and supine sleep position.
Conclusions: Positional plagiocephaly is a common issue faced by pediatricians; our results reinforce the need of improving prevention both of sudden infant death and positional plagiocephaly, through uniform messages provided prenatally and postnatally by different health professionals.
“What is Known:” •The incidence of positional plagiocephaly varies due to population studied and measuring methods. •Different factors are considered in the literature as being associated to positional plagiocephaly (infant factors, obstetric factors, infant care practices, sociodemographic factors). | |
“What is New:” •This is one of the few European studies quantifying positional plagiocephaly prevalence in a population of unselected healthy infants. •In this study, positional plagiocephaly is confirmed as a common issue, related to some factor (as supine sleep position and positional head prevalence) that should be addressed in pre and postnatal counseling. •The prone sleepers rate in our population highlight the need to improve parental awareness regarding SIDS prevention, in particular in borderline gestational age. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Positional plagiocephaly (PP) denotes a flattening of the skull, in the absence of synostosis [1]. After the “Back to Sleep” campaign, the incidence of sudden infant death syndrome (SIDS) halved from 1992 to 2001. Nevertheless, there was a dramatic increase in PP, now a relatively common issue faced by pediatricians [2, 3]. Although the sleep position is considered the leading risk factor for developing PP, not all supine sleepers develop plagiocephaly. Several factors have been linked to this problem: gestational age, obstetric factors as intrauterine position and oligohydramnios, assisted delivery, presentation at birth, birth order, male sex, ethnicity, infant neck problem, developmental delay, and various infant care practices as tummy time and maternal holding. [4,5,6].
According to results from a recent review regarding plagiocephaly in normal infant, PP is the consequence of gravity acting for a longer period of time in the same position [6]. Many of the risk factors analyzed in the review seem to be consistent to this theory, as also stated by the increase of PP incidence after the Back to Sleep campaign. It is not possible to obtain from the literature univocal environmental or lifestyle risk factors that could be addressed to prevent PP [6].
Even if the overall prognosis is good, the deformity may persist if not treated early, with adverse psychosocial implications [7,8,9,10]. Infants with PP could be less active compared with their age-matched peers [2], and some authors also found an association between plagiocephaly and early developmental delay, most commonly in motor domains, followed by language [10]. Developmental assessment is therefore suggested as a part of the management of children with this condition [2, 8, 11, 12]. Furthermore, if promptly managed, fewer infants will need physical therapy or orthotic helmet therapy, reducing discomfort and loss of time and money for the families [13].
The reported PP incidence varies with different definitions and measuring methods, and it appears to be age-dependent, with a peak of prevalence within the first 6 months of life and a tendency to decrease up to 2 years [14]. Of the few studies performed on primary care patient, three were considered without significant selection bias, on a higher grade of methodological level [6]. However, these studies used different methodologies: Hutchison et al. [15] performed a set of digital photographs to follow a population of healthy infants, mostly full term, with a PP prevalence rate of 16% at 6 weeks, 19.7% at 4 months, decreasing to 3.3% at 24 months. Van Vlimmeren et al. [16] evaluated healthy term neonates at birth and at 7 weeks with plagiocephalometry and found an increase of prevalence from 6.1 to 22.1%. Mawji et al. [17] recruited healthy term infants clinically evaluated with Argenta’s criteria at 7 to 12 weeks of age, showing a prevalence of 46.6%.
The aim of this study was to estimate the prevalence and risk factors for PP in a cohort of full-term infants who attended a public health immunization clinic in Ferrara, Italy, from January to July 2015.
Methods
Subjects
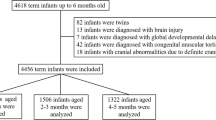
For this research, we used a prospective cohort design approved by the Ethics Committee of Ferrara University Hospital. All the healthy infants born at term who presented at the public immunization clinic in Ferrara at 8 to 12 weeks of age were considered for the study. Infants affected by craniosynostosis, malformations, neurological diseases, or admitted to the neonatal intensive care unit were considered non-eligible and excluded from the study.
After giving written informed consent, parents provided demographic and perinatal data. Detailed information was extracted from the infant discharge letter. Risk factors included in the analysis were anthropometric measures at birth, growth percentiles according to the Italian charts [18], sex, gestational age, maternal delivery type, multiple gestation, oligohydramnios, premature rupture of membrane, and infant birth order. Additional risk factors included were maternal age, origin and education, infant sleep position, infant head positional preference noticed by parents, feeding modalities or difficulties (breastfeeding or bottle feeding, presence of gastroesophageal reflux needing therapy), and infant tummy time (at least two to three times per day of prone positioning when the infant is awake for more than a few minutes each time, for at least 1 week).
To define the prevalence of PP and brachycephaly, we chose Argenta’s assessment tool [19] for its reliability, simplicity, and ease of use [20, 21]. According to the author, five stages of occipital plagiocephaly are defined with a progression from minimal to severe deformity: type I is limited to the posterior flattening of the skull, type II adds malposition of the ipsilateral ear, type III adds forehead deformity, type IV adds malar deformity, and type V adds vertical or temporal compensatory growing of the brain [19]. The same progression is in brachycephaly levels: type I is restricted to the central posterior skull; type II presents widening of the posterior skull lateral to the central depression; and in type III, there is compensatory temporal or vertical growth of skull [19].
All the assessments were performed by the primary author (EB) or by one of the co-authors (GG).
Statistical analyses
The differences in quantitative data were analyzed with the Student’s t test and the values were given as mean ± standard deviation (SD). The Shapiro-Wilk test was applied to check for normal distribution and the Bartlett test to check for equal variances across samples. Fisher’s exact test was used to examine the significance of the association in 2 × 2 contingency tables. Values are reported with 95% confidence interval (CI). Statistical analysis was managed with the software R version 3.2.2 (www.r-project.org). The Mantel-Haenszel test was performed to estimate the association between two variables taking into account a third one. The R package “irr” version 0.84 was used to calculate the ICC and inter-rater agreement between the two examiners (EB and GG) reported as Cohen’s kappa coefficient.
A multiple logistic regression was fitted to the data to determine the significance of covariates through the stepwise method of R package “MASS” version 7.3–19. A p value < 0.05 was considered statistically significant.
Results
During the study period, 340 infants went to the immunization clinic and 35 infants have been excluded due to exclusion criteria, mainly prematurity. Of the eligible infants, 283 were recruited (83.2%) while 57 parents refused to enter the project, 26 (46%) of these were of non-Italian nationality. The difference in proportion of lost infants between Italian and non-Italian mothers was not significant (p = 0.33). The main perinatal and postnatal characteristics of the participants are presented in Tables 1 and 2. Of note, borderline gestational age (37 + 0 to 37 + 6) was present in 24 infants (8.5%). The inter-rater agreement between the two observer was 0.83.
Prevalence
The prevalence of PP was 37.8% (107 infants), being more common on the right side (64.5%). The type and the side of plagiocephaly, according to Argenta’s assessment tool, are represented in Fig. 1. Of the 24 infants born at 37 weeks of gestation, 11 presented PP (45.8%). Brachycephaly was identified in 34 infants (12% of the population examined). In 16 of them, both plagiocephaly and brachycephaly were present. This means that nearly 15% of infants presenting plagiocephaly showed also brachycephaly.
Perinatal factors
Head circumference (HC) and maternal age appeared to be significantly associated to PP (Table 1).
In infants with PP, the mean HC at birth was 0.4 cm less than in infant without PP (no-PP group), and their mothers were 1 year older (p = 0.02). Plagiocephalic infants at birth weighed 100 g less than no-PP group, but this difference was not significant (p = 0.07). When excluding infants at 37 weeks, the difference in HC (p = 0.09) and weight (p = 0.72) were not significant. No correlations were found between maternal age and birth weight.
Italian infants were three times more likely to have PP than African infants, the most frequently represented ethnic group after the Italians.
In the group that performed tummy time regularly, the association between PP and ethnicity persisted, even when the supine position while sleeping was taken into account (Mantel-Haenszel test).
As shown in Table 1, there were no differences between groups regarding other perinatal factors.
Postnatal factors
In our population, 78.8% of the infants slept in supine position. In PP group, the percentage increases to 89.7%, while in no-PP group, the value is 72.2%. There was a significant difference between the two groups in supine sleepers’ rate (p < 0.001). The probability to develop PP is about 3-fold higher for supine sleepers than for prone sleepers (OR = 3.35, 95% CI 1.61–7.54, p < 0.01). Conversely, sleeping in prone position or in alternate side made PP, respectively, seven times and four times less probable.
Of the 24 infants born at 37 weeks, only 14 slept in the supine position (58.3 vs 78.8% in the whole population). They had an increased risk of developing PP (10/14 = 71.4%) compared to infants born at 38 weeks or more who slept supine (85/202 = 42.1%) (OR 3.56, 95% CI 1.1–13.4, p = 0.04).
In the PP group, 69% showed an infant head positional preference noticed by parents during first weeks of life (vs 40.3% in the no-PP group) and had a 4.77-fold probability of developing PP. In particular, when the right side was preferred, the probability was 3.78-fold higher (95% CI 2.1–6.8, p < 0.01), while for the left side, it was 2.07-fold (95% CI 1–4.28, p = 0.04). About 90% of the infants who had a right-side head positional preference had ipsilateral plagiocephaly, while 81% of those who had a left-side postural preference had ipsilateral plagiocephaly.
Considering the whole population, 63.3% of parents performed tummy time and 49% reported to be informed regarding its importance, while 8.5% alternated the end of the crib to prevent the maintenance of the same head position: no differences were found between infants with or without PP.
The multivariable logistic regression showed that PP was significantly associated to sleeping position (OR = 1.3), maternal age (OR = 1.1), and birth weight (OR = 1.1).
Discussion
This study reports prevalence and risk factors for PP in a cohort of unselected healthy infants, born in Italy, who presented at 8 to 12 weeks of age to receive routine immunization. The prevalence of PP in our study was 37.8%, lower than that reported by Mawji et al. (46.6%) who applied, like us, the Argenta’s criteria to a cohort of healthy infants aged from 7 to 12 weeks of life [17]. The two other studies of good qualities [15, 16] reported by the two reviews of the literature [6, 14] are scarcely comparable with this study, as cited in the “Introduction” section. Other authors reported a prevalence ranging from 7.7% (Aarnivala [22]), 13% (Peitsch [23]), to 20% (Pogliani [24]) at birth, 29% at 9 weeks (Leung [25]) to 37.5% at 22 weeks of life (Hutchison [26]). Therefore, it appears that there is a great variability depending on age, definition, and measurement tools.
Even when considering risk factors for PP, there is scarce agreement between studies, maybe due to poor methodological quality [6]. Only two determinants reach a concordance rate of more than 50% between studies considered by De Bock et al. [6]: male sex and supine sleeping position, while there is still scarce data regarding the potential influence of the everyday care environment of the baby.
In our study, head circumference, maternal age, ethnicity, positional preference of the head in the first weeks of life, and sleeping position seem to be related to PP. The multiple logistic regression showed that the PP was significantly associated to sleeping position, maternal age, and lower birth weight. A smaller head circumference and the tendency to a lower birth weight (100 g less in PP) found in our study could be due to the higher prevalence of PP in infants born at 37 weeks.
Older maternal age, also observed by others [27], appears to be an independent risk factor for PP, as suggested also by the logistic regression, even if this is one of the contradicting results in the literature [28].
Ethnicity could be related to PP because of compliance to sleeping position and cultural habits [29], while in our study, Italian ethnicity continued to be a risk factor even after correcting for main parental care habits (supine sleeping position and tummy-time period). This study cannot exclude influence from other ethnicity-related cultural habits such as babywearing. From the literature, we cannot define exactly the direct effect of ethnicity on infant gross motor milestones acquisition and on plagiocephaly development [30, 31].
The positional preference of the head in the first weeks of life was evident in our PP group, similarly to what reported in the literature [15, 32]. According to Leung et al. [33], parents show a good ability in identifying head orientation asymmetry, consistent with clinical evaluation at 3 weeks. Other authors showed that, if not managed, the head preference increases the risk and the severity of PP [34, 35]. Recently, Leung et al. showed that asymmetrical head orientation at 3 and 6 weeks of age was associated to PP at 9 weeks [25]. In our study, plagiocephaly occurred in particular when the right side was noticed as preferred from parents, a result already observed by others [25, 36]. The right-side preference and the right PP predominance could be related to the latter period of pregnancy when the fetus turns and engages the birth canal, and most often the vertex of the head lies with a left occipital anterior presentation [1, 16]. Behavioral asymmetries in arm movements, thumb sucking, and head orientation have been showed earlier in the pregnancy, evolving in intrinsic predominance of the lateralization towards the right side of neonates and in right-hand preference [1, 37, 38]. Approximately half of the parents that we interviewed remembered the instructions received about tummy time, and the great majority never changed crib end position. However, half of them had noticed a preferred position of the baby’s head. Improving parental awareness of side preference could be relevant in prevention of PP.
Tummy time is known to be an important factor to improve motor development and prevent PP [2, 16]. In this study, there was no difference in terms of tummy time between infants who developed PP and those who did not, which is similar to other studies [15, 35]. We suppose that tummy time was advised at the time of the pediatrician’s visit, close to the time of our evaluation.
Prolonged supine lying and long supine sleeping time were associated to PP [33], and we observed the same result. In our population, supine sleepers were 89.7% in PP group, but 72.2% in no-PP group, and 58.3% in no-PP group born at 37 weeks of gestation. It is necessary to improve awareness of preventive measure for SIDS while strengthening the need for alternating head position and other parental habits to prevent PP (i.e., periodically changing the orientation of the infant to outside activity, improve period of tummy time, reduce time in car seat) [2, 33]. These interventions are perfectly compatible with prevention of SIDS. Even if parents interviewed in our study were all conscious of the importance of put their baby in supine position, 11.7% of infants were prone sleepers. Our data resemble those of The National Infant Sleep Position Study, 2007–2010 [39], that reports in the USA at 4 months a percentage of supine sleepers of 72.6%, the same as in Norway, New Zealand, Canada, and the United Kingdom [40]. In Aarnivala’s study, the supine sleepers reached 67% [13].
Plagiocephaly worried most parents and they could decide to use sleeping products or sleeping positions that are contraindicated. Thus, the importance of counseling to prevent both conditions is advisable [41]. Health care providers should deliver consistent information during prenatal courses, at the time of birth, and during the early postpartum period. This information would be regarding the deformability of the skull and prevention methods, in particularly supervised tummy time and repositioning techniques [35]. Aarnivala et al. [13] demonstrated that providing detailed instructions in the postpartum time (intervention group) can reduce the prevalence and severity of PP in early infancy, when compared with children of a control group whose parents were not informed. The role of the pediatrician and of other primary care professionals is crucial in giving the right advice to prevent both SIDS and plagiocephaly.
Prevention of SIDS is even more important for preterm infants, in whom the risk of PP is higher [34]. In our study, infants of borderline gestational age (37 weeks) presented a statistically significant increased risk of plagiocephaly, despite the fact that only 58% of them slept supine. Probably infants born at 37 weeks share some characteristics of preterm infants. This could explain the increased risk showed in this study, compared to infant of 38–41 weeks of gestational age.
Strengths of this study are the following: (1) to our knowledge, this study is one of the few reporting the prevalence of PP in a European unselected population of healthy infants at an early age, the first in Italy and (2) the prevalence of PP is obtained through a clinical tool, useful even in a primary care setting.
Limitations of the study include the relatively small number of infants enrolled and the use of the Argenta’s criteria, a very easy clinical tool, which, however, does not provide objective measures.
Conclusion
This is one of the few European studies reporting the prevalence of positional plagiocephaly using a reliable clinical tool in healthy infants aged 8 to 12 weeks, the first in Italy. Positional plagiocephaly appears to be a relatively common issue faced by pediatricians, associated with the supine sleep position, especially at 37 weeks of gestation, head positional preference, particularly to the right side, older maternal age, and Italian ethnicity. Exploring parent’s habits, a considerable percentage of prone sleepers still emerge.
The results reinforce the need of improving prevention both of SIDS and positional plagiocephaly, through uniform messages provided prenatally and postnatally by different health professionals.
Abbreviations
- PP:
-
Positional plagiocephaly
SIDS
Sudden infant death syndrome
SD
Standard deviation
CI
Confidence interval
References
Losee JE, Corde Mason A (2005) Deformational plagiocephaly: diagnosis, prevention, and treatment. Clin Plast Surg 32:53–64. https://doi.org/10.1016/j.cps.2004.08.003
Laughlin J, Luerssen TG, Dias MS (2011) Prevention and Management of Positional Skull Deformities in infants. Pediatrics 128:1236–1241. https://doi.org/10.1542/peds.2011-2220
Shweikeh F, Nuño M, Danielpour M et al (2013) Positional plagiocephaly: an analysis of the literature on the effectiveness of current guidelines. Neurosurg Focus 35:1–9. https://doi.org/10.3171/2013.8.FOCUS13261
Looman WS, Kack Flannery AB (2012) Evidence-based Care of the Child with Deformational Plagiocephaly, part I: assessment and diagnosis. J Pediatr Heal Care 26:242–250. https://doi.org/10.1016/j.pedhc.2011.10.003
Pogliani L, Mameli C, Fabiano V, Zuccotti GV (2011) Positional plagiocephaly: what the pediatrician needs to know. A review. Childs Nerv Syst 27:1876–1876. https://doi.org/10.1007/s00381-011-1493-y
De Bock F, Braun V, Renz-Polster H (2017) Deformational plagiocephaly in normal infants: a systematic review of causes and hypotheses. Arch Dis Child 102:535–542. https://doi.org/10.1136/archdischild-2016-312018
Hutchison BL, Stewart AW, Mitchell EA (2011) Deformational plagiocephaly: a follow-up of head shape, parental concern and neurodevelopment at ages 3 and 4 years. Arch Dis Child 96:85–90. https://doi.org/10.1136/adc.2010.190934
Andrews BT, Fontana SC (2016) Plagiocephaly and developmental delay. J Craniofac Surg 27:1381–1382. https://doi.org/10.1097/SCS.0000000000002872
Cabrera-Martos I, Valenza MC, Valenza-Demet G et al (2016) Repercussions of plagiocephaly on posture, muscle flexibility and balance in children aged 3–5 years old. J Paediatr Child Health 52:541–546. https://doi.org/10.1111/jpc.13155
Martiniuk ALC, Vujovich-dunn C, Park M et al (2017) Plagiocephaly and developmental delay: a systematic review. J Dev Behav Pediatr 38:67–78. https://doi.org/10.1097/DBP.0000000000000376
Hutchison L (2012) Deformational plagiocephaly is associated with developmental delay in toddlers. J Pediatr 160:527–528. https://doi.org/10.1016/j.jpeds.2012.01.005
Fontana SC, Daniels D, Greaves T et al (2016) Assessment of deformational Plagiocephaly severity and neonatal developmental delay. J Craniofac Surg 27:1934–1936. https://doi.org/10.1097/SCS.0000000000003014
Aarnivala H, Vuollo V, Harila V et al (2015) Preventing deformational plagiocephaly through parent guidance: a randomized, controlled trial. Eur J Pediatr 174:1197–1208. https://doi.org/10.1007/s00431-015-2520-x
Bialocerkowski AE, Vladusic SL, Wei Ng C (2008) Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol 50:577–586. https://doi.org/10.1111/j.1469-8749.2008.03029.x
Hutchison BL, Hutchison LAD, Thompson JMD, Mitchell EA (2004) Plagiocephaly and Brachycephaly in the first two years of life: a prospective cohort study. Pediatrics 114:970–980. https://doi.org/10.1542/peds.2003-0668-F
van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM et al (2007) Risk factors for deformational Plagiocephaly at birth and at 7 weeks of age: a prospective cohort study. Pediatrics 119:e408–e418. https://doi.org/10.1542/peds.2006-2012
Mawji A, Vollman AR, Hatfield J et al (2013) The incidence of positional Plagiocephaly: a cohort study. Pediatrics 132:298–304. https://doi.org/10.1542/peds.2012-3438
Bertino E, Spada E, Occhi L et al (2010) Neonatal anthropometric charts: the Italian neonatal study compared with other European studies. J Pediatr Gastroenterol Nutr 51:353–361. https://doi.org/10.1097/MPG.0b013e3181da213e
Argenta L, David L, Thompson J (2004) Clinical classification of positional Plagiocephaly. J Craniofac Surg 15:368–372. https://doi.org/10.1097/00001665-200405000-00004
Branch LG, Kesty K, Krebs E et al (2015) Argenta clinical classification of deformational Plagiocephaly. J Craniofac Surg 26:606–610. https://doi.org/10.1097/SCS.0000000000001511
Spermon J, Spermon-Marijnen R, Scholten-Peeters W (2008) Clinical classification of deformational plagiocephaly according to Argenta: a reliability study. J Craniofac Surg 19:664–668. https://doi.org/10.1097/SCS.0b013e31816ae3ec
Aarnivala H, Valkama AM, Pirttiniemi PM (2014) Cranial shape, size and cervical motion in normal newborns. Early Hum Dev 90:425–430. https://doi.org/10.1016/j.earlhumdev.2014.05.007
Peitsch WK, Keefer CH, LaBrie RA, Mulliken JB (2002) Incidence of cranial asymmetry in healthy newborns. Pediatrics 110:e72–e72. https://doi.org/10.1542/peds.110.6.e72
Pogliani L, Cerini C, Vivaldo T et al (2014) Deformational plagiocephaly at birth: an observational study on the role of assisted reproductive technologies. J Matern Fetal Neonatal Med 27:270–274. https://doi.org/10.3109/14767058.2013.814629
Leung AYF, Mandrusiak A, Watter P et al (2016) Clinical assessment of head orientation profile development and its relationship with positional plagiocephaly in healthy term infants - a prospective study. Early Hum Dev 96:31–38. https://doi.org/10.1016/j.earlhumdev.2016.03.001
Hutchison B, Stewart AW, Mitchell EA (2009) Characteristics, head shape measurements and developmental delay in 287 consecutive infants attending a plagiocephaly clinic. Acta Paediatr 98:1494–1499. https://doi.org/10.1111/j.1651-2227.2009.01356.x
McKinney CM, Cunningham ML, Holt VL et al (2009) A case-control study of infant, maternal and perinatal characteristics associated with deformational plagiocephaly. Paediatr Perinat Epidemiol 23:332–345. https://doi.org/10.1111/j.1365-3016.2009.01038.x
Hutchison BL, Thompson JMD, Mitchell EA (2003) Determinants of Nonsynostotic Plagiocephaly: a case-control study. Pediatrics 112:e316–e316. https://doi.org/10.1542/peds.112.4.e316
Smith MG, Liu JH, Helms KH, Wilkerson KL (2012) Racial differences in trends and predictors of infant sleep positioning in South Carolina, 1996-2007. Matern Child Health J 16:72–82. https://doi.org/10.1007/s10995-010-0718-0
WHO Multicentre Growth Reference Study Group (2006) Assessment of sex differences and heterogeneity in motor milestone attainment among populations in the WHO multicentre growth reference study. Acta Paediatr 450:66–75. https://doi.org/10.1080/08035320500495530
Ertem IO, Krishnamurthy V, Mulaudzi MC et al (2018) Similarities and differences in child development from birth to age 3 years by sex and across four countries: a cross-sectional, observational study. Lancet Glob Heal 6:e279–e291. https://doi.org/10.1016/S2214-109X(18)30003-2
Boere-Boonekamp MM, van der Linden-Kuiper LT (2001) Positional preference: prevalence in infants and follow-up after two years. Pediatrics 107:339–343. https://doi.org/10.1542/peds.107.2.339
Leung A, Mandrusiak A, Watter P et al (2017) Impact of parent practices of infant positioning on head orientation profile and development of positional Plagiocephaly in healthy term infants. Phys Occup Ther Pediatr 2638:1–14. https://doi.org/10.1080/01942638.2017.1287811
Oh AK, Hoy EA, Rogers GF (2009) Predictors of severity in deformational plagiocephaly. J Craniofac Surg 20:685–689. https://doi.org/10.1097/SCS.0b013e318193d6e5
Mawji A, Robinson Vollman A, Fung T et al (2014) Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging. Paediatr Child Heal 19:423–427
Joganic JL, Lynch JM, Littlefield TR, Verrelli BC (2009) Risk factors associated with deformational Plagiocephaly. Pediatrics 124:e1126–e1133. https://doi.org/10.1542/peds.2008-2969
Fagard J (2013) The nature and nurture of human infant hand preference. Ann N Y Acad Sci 1288:114–123. https://doi.org/10.1111/nyas.12051
Beuter CR, Pedroso FS, Mazetto RC et al (2007) Association between dynamic asymmetry of the newborn’s head and intrauterine factors. Arq Neuropsiquiatr 65:218–221. https://doi.org/10.1590/S0004-282X2007000200006
Shapiro-Mendoza CK, Colson ER, Willinger M et al (2015) Trends in infant bedding use: National Infant Sleep Position study, 1993-2010. Pediatrics 135:10–17. https://doi.org/10.1542/peds.2014-1793
Rivarola MR, Reyes P, Henson C et al (2016) Impact of an educational intervention to improve adherence to the recommendations on safe infant sleep. Arch Argent Pediatr 114:223–231. https://doi.org/10.5546/aap.2016.eng.223
Martiniuk A, Jacob J, Faruqui N, Yu W (2016) Positional plagiocephaly reduces parental adherence to SIDS guidelines and inundates the health system. Child Care Health Dev 42:941–950. https://doi.org/10.1111/cch.12386
Acknowledgments
The authors would like to thank The Public Health Immunization clinic of the AUSL (Azienda Unità Sanitaria Locale) of Ferrara and Mr. Manuel Higginbotham for editing the manuscript.
Funding
We do not have a sponsor, and costs necessary to collect data were covered by funds from the Pediatric Department at the University of Ferrara.
Author information
Authors and Affiliations
Contributions
EB and GG performed the physical examinations; MB helped with the data collection. MS was the referral physiotherapist for the severe forms of plagiocephaly. NB was the physiotherapist who supervised the study. CBP had the idea of performing the study and contributed to its design. AB performed the statistical analysis. EB, AB, CBP, MS, and GG wrote the article.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
This project was approved by the Ethics Committee of Ferrara University Hospital, on September 2014. All parents received an informative letter together with the vaccine invitation and an informative report at the visit day. Then who accepted signed a consent form.
Additional information
Communicated by Mario Bianchetti
Rights and permissions
About this article
Cite this article
Ballardini, E., Sisti, M., Basaglia, N. et al. Prevalence and characteristics of positional plagiocephaly in healthy full-term infants at 8–12 weeks of life. Eur J Pediatr 177, 1547–1554 (2018). https://doi.org/10.1007/s00431-018-3212-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3212-0