Abstract
Vitamin D deficiency is common in Southeast Asia but there are limited data in pregnant women and neonates. This study aimed to determine the prevalence of vitamin D deficiency in cord blood of newborns and the association with maternal vitamin D status. A total of 94 pregnant women and their neonates were included. Clinical data and venous maternal blood for calcium, phosphate, albumin, alkaline phosphatase, magnesium, intact parathyroid hormone (iPTH), and vitamin D (25OHD) were obtained on the day of labor. Cord blood was collected following delivery to evaluate vitamin D status of newborns. Mean serum maternal and cord blood 25OHD levels were 25.42 ± 8.07 and 14.85 ± 5.13 ng/mL. The prevalence of vitamin D deficiency (25OHD < 12 ng/mL) and insufficiency (25OHD 12–20 ng/mL) in cord blood of newborns were 20.2 and 69.1%, respectively. There was a significant correlation between maternal and cord blood vitamin D levels (r = 0.86; P < 0.001). The factors associated with cord blood vitamin D deficiency were low maternal 25OHD level and no vitamin D supplement during pregnancy.
Conclusion: There is a high prevalence of vitamin D deficiency among Thai neonates. Adequate prenatal vitamin D supplementation should be implemented as routine antenatal care.
What is Known: • Vitamin D deficiency is prevalent in Southeast Asia. • There are widespread vitamin D deficiency among Thai populations including pregnant women. | |
What is New: • There is a high prevalence of vitamin D deficiency among Thai neonates. • The factors associated with cord blood vitamin D deficiency are low maternal vitamin D level and no vitamin D supplement during pregnancy. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D plays an important role in bone metabolism and maintaining bone health. The main sources of vitamin D in humans are from sunlight exposure and dietary intake [5]. Several factors contribute to the vitamin D status, including aging, the use of sunscreen, skin hyperpigmentation, and the sun intensity, including the season and the latitude [19]. Although abundant ultraviolet B (UVB) exposure is available thoughout the year, vitamin D deficiency (VDD) remains a common problem in South Asia and Southeast Asia [12]. In Thailand, there is widespread VDD among Thai populations in different age groups, including toddlers, school children, the elderly, and pregnant women [1,2,3, 13, 15, 16]. Since 25-hydroxyvitamin D (25OHD) crosses the placenta, there is a strong correlation between maternal and cord blood 25OHD levels [6,7,8]. Previous studies have reported a high prevalence of VDD in maternal serum and cord blood [6, 9, 14, 18]. To the best of our knowledge, the prevalence of VDD among newborns has never been reported in Thailand and the routine supplementation of vitamin D in pregnant women and newborns has not yet been established. Furthermore, vitamin D intake among Thais is generally low because few natural vitamin D-rich food sources are found in Thailand, and there is an absence of food fortification with vitamin D.
Most previous studies have defined VDD as 25OHD levels of < 20 ng/mL; however, global consensus recommendations on the prevention and management of nutritional rickets have been recently established that define vitamin D deficiency and insufficiency as < 12 and 12–20 ng/mL, respectively [11]. We aim to evaluate the prevalence of VDD in the cord blood of newborns according to this definition and the association with the maternal vitamin D status.
Material and methods
Patients
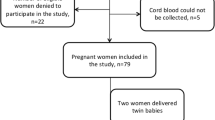
The study protocol was approved by the Institutional Review Board of Chonprathan Hospital, Srinakharinwirot University. Informed consent was obtained from all subjects. A total of 94 Thai pregnant women aged 18–45 years old and carrying a term singleton fetus and their neonates were enrolled in the study at Chonprathan Hospital in Nonthaburi, Thailand, during October 2016 to April 2017. Term pregnancy was defined as 37–41 weeks of gestation. Infants that were admitted to the Neonatal Intensive Care Unit, and born with congenital malformation and syndrome were excluded. Pregnant women were asked for their socio-demographic data, multivitamin supplementation during pregnancy, and their use of sunscreen. The obstetric history and newborn data were obtained from the medical records. Venous maternal blood samples, for calcium, phosphate, albumin, alkaline phosphatase, magnesium, intact parathyroid hormone (iPTH), and 25OHD were obtained on the day of labor. Cord blood was collected following delivery to evaluate the vitamin D status of the newborns.
Biochemical assays
The plasma levels of calcium, phosphate, magnesium, and albumin were measured using an Automated Analyzer (Cobas c501; Roche Diagnosis). Intact parathyroid hormone was measured using a chemiluminescent microparticle immunoassay (Abbott Diagnostics, Wiesbaden, Germany). 25OHD was analyzed using a chemiluminescent microparticle immunoassay (Abbott Diagnostics, Longford, Ireland). All the hormonal assays were performed according to the manufacturers’ protocols. Vitamin D deficiency was defined as 25OHD < 12 ng/mL, insufficiency as 25OHD 12–20 ng/mL, and sufficiency as 25OHD > 20 ng/mL.
Statistical analysis
Statistical analysis was performed using SPSS version 22. Normally distributed data were expressed as the mean ± standard deviation. We performed analysis of variance (ANOVA) and Chi-square test statistics to compare the continuous and categorical data between the groups. Pearson’s correlation analysis was used to explore relationships. A P value < 0.05 was considered significant.
Results
In total, 94 Thai pregnant women, mean age 28.59 ± 5.91 years, were included in the study. There were 37 primiparous (30.4%) and 57 multiparous women (60.6%). The mean gestational age was 38.6 ± 1.01 weeks. Forty-six women (49%) were taking vitamin D supplements during pregnancy with an average dose of 400 IU/day. The mean BMI before pregnancy was 22.42 ± 4.38 kg/m2. There were 31 women (33%) reported to routinely use sunscreen. Of the newborns, 47 (50%) were females and 81 (86.2%) were classified as appropriate for their gestational age. The mean birth weight and length were 3096.38 ± 374.3 g and 52.04 ± 1.92 cm, respectively.
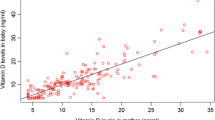
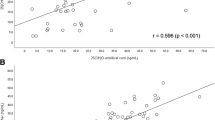
The mean serum maternal and cord blood 25OHD levels were 25.42 ± 8.07 and 14.85 ± 5.13 ng/mL, respectively. On average, the serum cord blood 25OHD level accounted for 57% of the maternal 25OHD level. The prevalence of vitamin D deficiency and insufficiency in newborns, defined as 25OHD < 12 and 12–20 ng/mL, were 20.2 and 69.1%, respectively. There was a significant correlation (r = 0.86; P < 0.001) between the maternal and cord blood vitamin D levels (Fig. 1). There was no association between the vitamin D level in cord blood with the birth weight (r = − 0.019, P = 0.86), birth length (r = 0.068, P = 0.51), and head circumference (r = − 0.102, P = 0.33).
When comparing between the groups, the mothers of infants with a deficient or insufficient level of vitamin D in cord blood had a lower 25OHD level (Table 1). The lowest percentage of maternal supplementation was found in the deficient group. There was no difference in the maternal levels of calcium, phosphate, magnesium, and intact parathyroid hormone. The birth weight and length were not different between the groups.
As shown in Table 2, mothers supplemented with vitamin D demonstrated a higher 25OHD level. In the group of mothers supplemented with vitamin D during pregnancy (n = 46), vitamin D insufficiency was noted in 9 mothers (19.6%) and 39 neonates (84.8%). Although the 25OHD levels in cord blood were not different, the prevalence of cord blood VDD was significant lower in the supplemented group.
Discussion
To the extent of our review, this is the first study in Thailand evaluating the vitamin D status in cord blood using the definition and diagnosis of global consensus recommendations on the prevention and management of nutritional rickets and the association with maternal vitamin D status. Our study showed a high prevalence of VDD and insufficiency in the cord blood of newborns and a significant correlation between maternal and cord blood vitamin D levels. A total of 20.2% of these newborns had VDD and 69.1% had vitamin D insufficiency, despite 49% of their mothers reporting the use of multivitamin supplements during pregnancy. Several studies have evaluated the vitamin D status in cord blood. In a study in Brazil, 29.2% of the infants tested had VDD and 51.3% had vitamin D insufficiency at birth [4]. A large cohort study from the Netherlands also showed a high prevalence of VDD in neonates (46%), especially among those with a non-European ethnic background. Another study from India showed a large proportion of neonates (95.7%) had hypovitaminosis D (serum 25OHD < 20 ng/mL) [17].
In our study, the maternal 25OHD level and use of vitamin D supplements during pregnancy were associated with the vitamin D status in neonates. A large study in Canada reported that the key factors associated with the neonatal 25OHD level were maternal age, dairy intake, supplement use, and 25OHD level [20]. Marshall et al. reported that a younger maternal age and an increased number of pregnancies were associated with cord blood vitamin D deficiency or insufficiency [10]. Another study also found that the risk factors of VDD in newborns were the maternal 25OHD and alkaline phosphatase levels [4].
Exposure to sunlight is the main source of vitamin D and sunscreen use could contribute to VDD [5]. However, our data showed no association between VDD and sunscreen use. This is similar to the study in Brazil, which reported that sun exposure and the use of a sunscreen were not associated with VDD in women and newborns [4]. Our study showed no significant differences in the maternal levels of calcium, phosphate, magnesium, and intact parathyroid hormone between vitamin D-deficient and -sufficient mother; however, there was a trend that low vitamin D levels in the mother lead to higher PTH values as is observed in other studies.
In the present study, the use of vitamin D supplements decreased the prevalence of cord blood VDD but not vitamin D insufficiency. Despite taking vitamin D supplements during pregnancy, cord blood VDD was found as 6.5% and vitamin D insufficiency was noted as 19.6% in mothers and 84.8% in their neonates. These could be due to an inadequate dose of vitamin D since the average dose of vitamin D intake in our subjects was only 400 IU/day. Recently, global consensus guidelines have recommended that pregnant women should receive 600 IU/day of vitamin D [11].
Sufficiency limit of 25OHD is still debated. The Endocrine Society recommends that 25OHD value of 30 ng/mL should be the actual lower normal limit for adults, whereas the Institute of Medicine defines this limit as 20 ng/mL. Our study showed that mean maternal 25OHD levels of the newborns with deficient, insufficient, and sufficient vitamin D status were 15.3, 26.6, and 37.1 ng/mL, respectively. Also, mean 25OHD level of 14.8 ng/mL in cord blood is about 57% of maternal level. These data suggest that maternal 25OHD level should be above 30 ng/mL for sufficient vitamin D status in newborns and maternal 25OHD level greater than 20 ng/mL seems to be adequate for preventing cord blood vitamin D deficiency. In conclusion, serum 25OHD level of 20 ng/mL might be the lower normal limit for general population, but based on the results of our study, we might propose that this limit should be at least 30 ng/mL for pregnant women that must supply their offspring.
We acknowledge the potential limitations of our study. First, our study was conducted only in an urban area thus could not represent the overall Thai population. Second, we did not evaluate the adherence of taking multivitamin supplements and did not record the dietary vitamin D intake. Finally we did not collect all the maternal data that may correlate with cord blood vitamin D status, including maternal skin color and sunlight exposure. However, it is unlikely that these factors will have overly affected the results because all the studied mothers were of the same ethnicity and the sunlight exposure data obtained from the questionnaires may be inaccurate because they self-reported information and therefore there was a possibility of recall bias.
In summary, although Thailand is located in a tropical area, a high prevalence of VDD is found among Thai neonates. Consequently, it is recommended that adequate prenatal vitamin D supplementation should be implemented as part of routine antenatal care.
Abbreviations
- 25OHD:
-
25-Hydroxyvitamin D
- iPTH:
-
Intact parathyroid hormone
- UVB:
-
Ultraviolet B
- VDD:
-
Vitamin D deficiency
References
Chailurkit LO, Aekplakorn W, Ongphiphadhanakul B (2011) Regional variation and determinants of vitamin D status in sunshine-abundant Thailand. BMC Public Health 11:853. https://doi.org/10.1186/1471-2458-11-853
Chailurkit LO, Kruavit A, Rajatanavin R (2011) Vitamin D status and bone health in healthy Thai elderly women. Nutrition 27(2):160–164. https://doi.org/10.1016/j.nut.2009.12.001
Charatcharoenwitthaya N, Nanthakomon T, Somprasit C, Chanthasenanont A, Chailurkit LO, Pattaraarchachai J, Ongphiphadhanakul B (2013) Maternal vitamin D status, its associated factors and the course of pregnancy in Thai women. Clin Endocrinol 78(1):126–133. https://doi.org/10.1111/j.1365-2265.2012.04470.x
do Prado MR, Oliveira Fde C, Assis KF, Ribeiro SA, do Prado Junior PP, Sant’Ana LF, Priore SE, Franceschini Sdo C (2015) Prevalence of vitamin D deficiency and associated factors in women and newborns in the immediate postpartum period. Rev Paul Pediatr 33(3):287–294. https://doi.org/10.1016/j.rpped.2015.01.006
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281. https://doi.org/10.1056/NEJMra070553
Jacquemyn Y, Ajaji M, Karepouan N (2013) Vitamin D levels in maternal serum and umbilical cord blood in a multi-ethnic population in Antwerp, Belgium. Facts Views Vis Obgyn 5(1):3–5
Kovacs CS (2008) Vitamin D in pregnancy and lactation: maternal, fetal, and neonatal outcomes from human and animal studies. Am J Clin Nutr 88(2):520S–528S
Kumar P, Shenoi A, Kumar RK, Girish SV, Subbaiah S (2015) Vitamin D deficiency among women in labor and cord blood of newborns. Indian Pediatr 52(6):530–531
Manzano Varo C, Garcia-Algar O, Mur Sierra A, Ferrer Costa R, Carrascosa Lezcano A, Yeste Fernandez D, Ortigosa Gomez S (2017) Plasma 25-OH vitamin D concentrations in cord blood after summer months, Spain. Rev Esp Salud Publica 91
Marshall I, Mehta R, Ayers C, Dhumal S, Petrova A (2016) Prevalence and risk factors for vitamin D insufficiency and deficiency at birth and associated outcome. BMC Pediatr 16(1):208. https://doi.org/10.1186/s12887-016-0741-4
Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Makitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Savendahl L, Khadgawat R, Pludowski P, Maddock J, Hypponen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Hogler W (2016) Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab 101(2):394–415. https://doi.org/10.1210/jc.2015-2175
Nimitphong H, Holick MF (2013) Vitamin D status and sun exposure in Southeast Asia. Dermato-endocrinology 5(1):34–37. https://doi.org/10.4161/derm.24054
Nimitphong H, Chailurkit LO, Chanprasertyothin S, Sritara P, Ongphiphadhanakul B (2013) The association of vitamin D status and fasting glucose according to body fat mass in young healthy Thais. BMC Endocr Disord 13:60. https://doi.org/10.1186/1472-6823-13-60
Parlak M, Kalay S, Kalay Z, Kirecci A, Guney O, Koklu E (2015) Severe vitamin D deficiency among pregnant women and their newborns in Turkey. J Matern Fetal Neonatal Med 28(5):548–551. https://doi.org/10.3109/14767058.2014.924103
Pratumvinit B, Wongkrajang P, Wataganara T, Hanyongyuth S, Nimmannit A, Chatsiricharoenkul S, Manonukul K, Reesukumal K (2015) Maternal vitamin D status and its related factors in pregnant women in Bangkok, Thailand. PLoS One 10(7):e0131126. https://doi.org/10.1371/journal.pone.0131126
Rojroongwasinkul N, Kijboonchoo K, Wimonpeerapattana W, Purttiponthanee S, Yamborisut U, Boonpraderm A, Kunapan P, Thasanasuwan W, Khouw I (2013) SEANUTS: the nutritional status and dietary intakes of 0.5-12-year-old Thai children. Br J Nutr 110(Suppl 3):S36–S44. https://doi.org/10.1017/S0007114513002110
Sachan A, Gupta R, Das V, Agarwal A, Awasthi PK, Bhatia V (2005) High prevalence of vitamin D deficiency among pregnant women and their newborns in northern India. Am J Clin Nutr 81(5):1060–1064
Vinkhuyzen AA, Eyles DW, Burne TH, Blanken LM, Kruithof CJ, Verhulst F, Jaddoe VW, Tiemeier H, McGrath JJ (2015) Prevalence and predictors of vitamin D deficiency based on maternal mid-gestation and neonatal cord bloods: The Generation R Study. J Steroid Biochem Mol Biol 164:161–167. https://doi.org/10.1016/j.jsbmb.2015.09.018
Wacker M, Holick MF (2013) Sunlight and vitamin D: a global perspective for health. Dermato-endocrinology 5(1):51–108. https://doi.org/10.4161/derm.24494
Woolcott CG, Giguere Y, Weiler HA, Spencer A, Forest JC, Armson BA, Dodds L (2016) Determinants of vitamin D status in pregnant women and neonates. Can J Public Health 107(4–5):e410–e416. https://doi.org/10.17269/cjph.107.5629
Acknowledgments
We would like to thank the patients and their families for participation in this study and Dr. Somchit Jaruratanasirikul for her constructive comments on our work and her editing of the text.
Funding
This study was supported by the Panyananthaphikkhu Chonprathan Medical Center research funding.
Author information
Authors and Affiliations
Contributions
KA conceived of the study, participated in its design, analysis and interpretation of data, and drafted the manuscript. PL participated in the design of study, acquisition of data and coordination of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
All procedures were performed according to the Declaration of Helsinki and approved by the Ethics Committee, Panyananthaphikkhu Chonprathan Medical Center, Srinakharinwirot University. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest and do not have a financial relationship with the organization that sponsored the research.
Disclosure statement
The authors have nothing to disclose.
Additional information
Communicated by Peter de Winter
Rights and permissions
About this article
Cite this article
Ariyawatkul, K., Lersbuasin, P. Prevalence of vitamin D deficiency in cord blood of newborns and the association with maternal vitamin D status. Eur J Pediatr 177, 1541–1545 (2018). https://doi.org/10.1007/s00431-018-3210-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-018-3210-2