Abstract
Cryptococcosis is a rare pediatric disease. The aim of the study is to describe clinical characteristics and prognosis of pediatric cryptococcosis from 2002 to 2014 in Beijing Children’s Hospital. A total of 53 cases of cryptococcosis were identified, 69.8% of which were males. The mean age was 7 years. Forty-one (77.4%) patients had no underlying conditions. Fever, headache, and vomiting were the most common symptoms. The most common sites were the central nervous system (CNS), followed by the lungs. Most patients received a combination of amphotericin B and fluconazole with or without flucytosine as their initial regimen. Twenty-seven patients received a follow-up and six patients (22.2%) had died. The factors associated with neurological complications or death were headache (P = 0.008), seizures (P = 0.006), visual impairment (P = 0.011), neck stiffness (P = 0.008), low erythrocyte sedimentation rate (ESR) (P = 0.024), and a cerebral spinal fluid (CSF) cryptococcal antigen titer ≥ 1:1024 (P = 0.038).
Conclusions: The majority of cryptococcosis cases in China occurred in children without underlying conditions, causing multiple organ damage. The CNS was the most common site. Patients who had headaches, seizures, or high CSF antigen titers experienced neurological complications or died.
What is known: • Cryptococcosis is a rare cause of infection in children. |
What is new: • This review gives a brief overview over pediatric cryptococcosis in China. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cryptococcosis is an invasive mycotic infection caused by the Cryptococcus species, an encapsulated, yeast-like fungus with the ability to infect a number of sites, and primarily results in meningitis with significant morbidity and mortality [30]. It is often reported to develop in immunocompromised hosts, specifically adult patients with AIDS. However, the majority of cryptococcosis cases in China are reported to have occurred in immunocompetent hosts [7].
Many large-scale studies have been conducted in adult patients with cryptococcosis, but there are limited studies focusing on pediatric populations. To our knowledge, fewer than 1000 cases of pediatric cryptococcal infection have been reported in English-language studies [1, 11, 14, 16, 18, 20, 22, 25, 34, 36], most of which occurred in non-HIV-infected but immunocompromised hosts. The clinical characteristics of pediatric patients with cryptococcosis differ between reports. Accordingly, we conducted a retrospective study to investigate the clinical manifestations and outcomes of pediatric cryptococcosis at Beijing Children’s Hospital.
Materials and methods
Study design
We reviewed data from children (younger than 18 year old) confirmed cryptococcosis who admitted to Beijing Children’s Hospital (a 970-bed tertiary health care hospital) between January 2002 and September 2014 in this retrospective study.
We reviewed patient records for demographic data, clinical manifestations, and laboratory findings from the Medical Records and Statistics Room. All imaging studies were reviewed by a single radiologist and the initial treatment.
Case definition
Cryptococcosis cases were defined by (1) positive culture of Cryptococcus from a normally sterile site, (2) a positive India ink staining of cerebrospinal fluid (CSF), (3) positive cryptococcal antigen in CSF and/or in the blood, and (4) a pathological diagnosis. Disseminated cryptococcosis was defined when at least two noncontiguous organs were affected [31].
Cryptococcal antigen assay: The Immy Latex-Crypto Antigens (Immuno-Mycologics, Inc.) were used to perform the antigen assay.
Long-term outcomes
Long-term prognosis was assessed in April 2015 by contacting the families by telephone. Following items were asked: outcome: dead or alive; symptoms: (1) headache, (2) nausea and vomiting, (3) sight, (4), hearing, and (5) epilepsy; dysthymic disorders: (1) irritability, (2) anxious, and (3) depression; dyskinesia: (1) limb paralysis, (2) facial paralysis, (3) ataxia, and (4) dysphonia. Patients who had neurological complications (blindness and personality changes, e.g., irritability) or had passed away were categorized as having a poor status; all others were determined to be in good status.
Statistical analysis
Mean and standard deviations (SDs) are shown when distributions were confirmed normal; median and interquartile range (IQRs) are reported otherwise. The categorical variables were compared using the Chi-square test or Fischer’s exact test, as appropriate. Continuous variables within two groups were compared using the independent t test for parametric data and the Mann-Whitney U test for non-parametric data. P values < 0.05 were considered statistically significant. All of the statistical analyses were conducted using Statistical Product and Service Solutions (SPSS), version 19.0 (IBM, NY, USA).
Results
Demographic data and underlying conditions
A total of 53 hospitalized children were diagnosed with cryptococcosis during the 13.75-year study period. The cases originated from 11 provinces in the mainland, mostly from North China and Central China (Fig. 1). The temporal trend over the years was shown in Fig. 2. Table 1 describes the demographic characteristics of the sample. All of the children were Han Chinese, and 37 (69.8%) were male. The average age was 7 years, with only two patients being younger than 2 years. Additionally, 19 (35.8%) cases had a history of exposure to poultry, including 11 who were exposed to pigeons and 8 to chickens. The underlying conditions included in the analysis are presented in Table 1; however, 77.4% (41) of the patients had no underlying disease.
Organ involvement and clinical manifestations
The most commonly affected organs were the central nervous system (CNS) (42 cases; 79.2%) and lungs (28 cases; 52.8%). Compared with patients with cryptococcal meningitis (CM), non-CM patients were more likely to present from January to March (63.6 vs. 9.5%) (Table 1). Other involved sites included the lymph nodes (24 cases; 45.2%) (17 abdominal, 16 pulmonary, and two cervical), liver (9 cases; 17.0%), spleen (9 cases; 17.0%), and kidneys (2 cases; 3.8%), and the skin, skeleton, and costal cartilage were involved in one case each (1.9%). Disseminated cryptococcosis was identified in 25 (47.2%) patients.
The time to diagnosis ranged from 2 days to 20 months, with an average of 35 days. The common clinical manifestations were as follows: fever, in 53 cases (100%); headache, 33 (62.3%); vomiting, 30 (56.6%); confusion, 19 (35.8%); and cough, 19 (35.8%), as shown in Table 2. Fever and headache were the predominant symptoms. Four of 42 (9.5%) CM cases did not show any neurological symptoms, and 9 of 28 (31.2%) patients with pulmonary disease had no respiratory symptoms.
Laboratory examinations
The median white blood cell (WBC) count at presentation on the peripheral smear was 11,700 (interquartile range, 9000–16,000) cells per mm3, with a median neutrophil percentage of 69%. The average eosinophil count was 1870 (± 1500) cells per mm3 (normal range, 50–500 cells per mm3), with an elevated eosinophil count in 27/45 (60.0%) of the patients: 17 (37.8%) were mildly elevated (500 to 1500 cells per mm3), 9 (22.2%) were moderately elevated (1500 to 5000 cells per mm3), and 1 (2.2%) was severely elevated (greater than 5000 cells per mm3). The median C-reactive protein (CRP) level was 32 (interquartile range, 8–64) mg/L (normal range, < 8 mg/L), and CRP was elevated in 38 (71.7%) of the patients. The average erythrocyte sedimentation rate (ESR) was 46.5 mm/h (± 30.2 mm/h) (normal range, < 20 mm/h), and ESR was elevated in 47 (88.9%) patients. Immunoglobulin levels were obtained in 42 (79.2%) patients. IgA and IgG were all within the normal range, with the exception of a patient with X-linked agammaglobulinemia (XLA), in whom they were significantly decreased. Lymphocyte subsets were determined in 41 (77.4%) patients. CD4% was 35% (interquartile range, 28–38%) (normal range, 27–57). All CD4+ lymphocyte counts were more than 500 cells/μL, except for in the one HIV-infected patient, in whom the count was 241 cells/μL.
Pathogen findings
The blood culture was positive in 53.3% (16/30) of the patients. The serum latex agglutination test was positive for Cryptococcus in 36/42 (85.7%) patients, with titers ranging from 1:8 to > 1:1024. Of the 42 CM patients, CSF cultures, India Ink staining, and antigen tests were positive in 82.9% (34/41), 85.7% (36/42), and 82.4% (28/34), respectively.
Other positive culture sites included bone, sputum, and soft tissue abscess. Histologic examinations showed cryptococcosis in abdominal lymph nodes (three cases), mediastinal lymph nodes (three cases), cervical lymph nodes (two cases), the liver (two cases), marrow (one case), and skin (one case).
Radiological findings
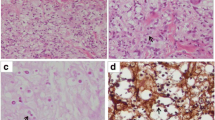
The abnormalities found through imaging and ultrasounds are listed in Table 3. The typical abnormalities on chest CT/X-ray and cranial magnetic resonance imaging (MRI) are shown in Fig. 3. The chest CT/X-ray showed no obvious pulmonary lobes, segmental tendency of nodules, or patchy shadows. Cases of disseminated cryptococcosis had a higher likelihood of miliary lung disease and lymphadenopathy than non-disseminated cases (28 vs. 0% and 52 vs. 11%, respectively, P < 0.01).
Imaging findings of pediatric cryptococcosis cases. a A 3-year-old boy who presented with fever and headache for one month. MRI axial T2-weighted image: presented clustered tiny foci that were hyperintense in T2-weighted images, dilated Virchow-Robin spaces (VRS) in the basal ganglia region, and hydrocephalus with encephaledema. b A 5-year-old boy who presented with fever and headache for 15 days. Cranial MRI axial DWI-weighted image: multiple patchy hyperintensities of gelatinous pseudocyst with multiple patchy hyperintensities on T1-, T2-, and DWI-weighted images in the basal ganglia region. c A 6-year-old girl who was admitted with headache and seizures for 20 days. Magnetic resonance venography (MRV): left transverse sinus and sigmoid sinus stenosis. d A 5-year-old boy who presented with fever and cough for 1 month. CT scan: innumerable small bilateral pulmonary nodules consistent with a miliary pattern. e A 10-year-old girl who was admitted with headache for 15 days and cough for 7 days. CT scan: a nodule in left interior lung lobe with halo sign. f A 14-year-old HIV-infected boy who presented with headache for one month and fever and cough after admission. CT scan: a subpleural thin-walled cavity inside the right upper lung, the inner wall was smooth, with surrounding ground-glass opacity
Treatment and outcomes
The median length of hospital stay was 31 (interquartile range, 18–53) days. Fifty-one patients received treatment, one patient refused therapy without treatment, and the one HIV-infected patient transferred to a specialized infectious disease hospital with unknown therapy. The initial treatments were classified as follows: amphotericin B (AmB) combined with fluconazole (Flu) ± 5-fluorocytosine (5-FC) in 29 patients (56.9%); Flu ± 5-FC in 10 patients (19.6%); AmB ± 5-FC in 11 cases (21.5%); and voriconazole (VOR) alone for 1 child with osteomyelitis (Table 4).
Twenty-seven (50.9%) patients were followed by phone after discharge. The median follow-up time after first admission was 994 days (range 221–4413). Six patients (22.2%) died, all of whom had CM. Twenty-one (77.8%) patients survived, including 1 case that had blindness, tic disorder, and irritability; one case that had blindness and irritability; other cases did well at their ages and did not have symptoms or sequelae. The HIV-infected patient had good outcomes.
Our analysis showed that lymph node involvement was associated with good patient outcomes (P = 0.033) and that headache (P = 0.008), seizures (P = 0.006), visual impairment (P = 0.011), neck stiffness (P = 0.008), low ESRs (P = 0.024), and high (≥ 1:1024) CSF antigen titers (P = 0.038) were associated with poor patient status (Table 5).
Discussion
Our study provided an analysis of pediatric cryptococcosis cases in China. Cryptococcosis is a rare pediatric disease worldwide, accounting for only 0.9–2% of cases [22].
In this study, there was a predominance of the male gender (68.9%), similar to in previous reports [16]. The average age of our patients was 7 year old, and only two patients were younger than 2 years. This age distribution can be explained by the increased environmental exposures with age [9]. We found non-CM cases are more likely to occur from January to March and CM cases are more likely to occur in summer and autumn (July–December). Some articles mentioned about half of the CM cases occurred in summer (June–August) in children [11, 12]. The reason for this is unclear. Although the effects of climatic factors across the seasons may be an important epidemiologic characteristic of Cryptococcosis [33], the seasonal difference between CM and non-CM has not been reported as far as I know. Our data showed that only 22.6% of patients had underlying conditions, including only one who had HIV infection. Most previous reports worldwide have reported cryptococcosis in individuals with underlying immunocompromising conditions, AIDS in particular [32]. The reported proportions of afflicted children with underlying diseases in different countries were 86% in South Africa [22], 65.9% in Brazil [34], 63.5% in the USA [16], 56% in Taiwan [14], and 53.7% in Colombia [20]. However, the reported proportion of cryptococcosis cases in immunocompromised hosts in China has been low, at only 26.1% of children and 33.1% of adults with CM [11, 21, 38]. Together with previous studies, these studies may indicate that immunosuppression is not the primary risk factor for cryptococcosis in Chinese people. Host genetic factors may contribute to the high prevalence of the apparently healthy cases reported in China. However, “apparently healthy” patients may still have mannose-binding leptin (MBL) deficiency, which is known to predispose people of Han Chinese ethnicity to CM [28]. Moreover, FCGR2B 232I/T genotypes have been associated with HIV-uninfected Chinese patients compared with healthy controls [13].
Globally, the majority of cases are caused by the Cryptococcus neoformans var. grubii subspecies (especially molecular type VNI) [23]. Chen et al. [3] analyzed 129 clinical isolates from China and showed that 93% were VNI, demonstrating significant genetic homogeneity, as cases had the same subgenotype, VNIc. However, this prevalence of VNIc is not unique to China; C. neoformans in the Korean clinical population has also been reported to be genetically homogeneous, with a strong majority of VNIc subgenotype (93%). However, the hosts in Korea predominantly had underlying conditions [4]. Therefore, the prevalent strain type alone cannot explain why the majority of infections in China have occurred in apparently healthy persons. Limited data are available regarding the species isolated from pediatric patients [20, 24]. Therefore, further studies on the molecular epidemiology of Cryptococcus strains in Chinese children are needed.
Disseminated cryptococcosis occurred in a high proportion of patients (47.2%), with Cryptococcus spp. present in numerous sites, most commonly the CNS and lungs. Other sites such as the lymph nodes, spleen, liver, skin, and bone marrow were reported in very few cases [2, 15, 26, 27, 37]. The clinical manifestations of cryptococcosis are not specific, and it could easily be misdiagnosed as tuberculosis.
Diffuse miliary nodules and lymphadenopathy were more common in pediatric patients than in adults. Only 4% of pulmonary cryptococcosis cases in adults showed diffuse miliary nodules, and 5.7% showed lymphadenopathy [6, 19]. Our study illustrated that miliary manifestations and lymphadenopathy were highly prevalent in pediatric cases without underlying disease. These imaging features could lead these cases to be misdiagnosed as tuberculosis.
Our results showed that eosinophilia was prevalent, with 10/45 (22.2%) moderately or severely elevated cases. One article described how eosinophils are immune to Cryptococcus spp. [8]. Eosinophils have been shown to be a major source of Th2 cytokine IL-4 during cryptococcal infection. Eosinophil-deficient mice infected with C. neoformans had fewer Th2 cells and increased Th1/Th17 cells, in addition to a reduction of inflammatory cells. This again indicates a detrimental role of eosinophils, whereby a Th2 profile is induced in their presence. An interesting clinical observation of an immunocompetent patient with disseminated C. neoformans infection and elevated eosinophil levels suggests that Cryptococcus is able to induce a Th2 profile that may lead to eosinophilia. [8]. Very few studies have noted elevations in eosinophilia [35].
Given the high rate of loss of outpatient treatment information, we could not fully evaluate the therapeutic regimens and ultimate outcomes. Most patients received a combination of AmB and Flu with or without 5-FC as their initial treatment regimen. Only one patient received VOR. Although VOR may show activity against cryptococcosis, its effectiveness as a first-line agent in children has not been established. In our study, VOR was effective for osteomyelitis. Although treatment guidelines recommend AmB with 5-FC as the induction therapy for cryptococcal meningitis, evidence of treatment in children are still insufficient, especially in non-HIV children. In our clinical work, we add AmB dose gradually, in that way, Amb with fluconazole and 5-FC may be physicians’ first choice, especially in severe patients. In addition, some articles mentioned the effectiveness of AmB with fluconazole both in HIV and non-HIV population [38]. In conditions of children who were intolerable of Amb, fluconazone would also be prescribed. In terms of prognosis, in spite of six patients who were treated with AmB + Flu + −5-FC had poor status in this study, therapy selection bias may exist because severe cases were more easily taken this prescription.
The mortality rate in this study was 22.2%, which is similar to the rate identified in Chinese pediatric CM data in Shijiazhuang [11], lower than 39.19% reported in Sichuan province of China and 43% reported in African children with acquired immunodeficiency syndrome [10, 21]. Previous studies have reported that the factors associated with high mortality include cryptococcemia, organ failure or hematologic malignancy, unsuccessful therapy, non-pulmonary infection site, intracranial hypertension, and high serum antigen titers [5, 29]. In our study, patients with headache, seizures, visual impairment, neck stiffness, low ESRs, and high (≥ 1:2014) CSF antigen titers had a poor long-term prognosis. Furthermore, we found that all patients who died had CM.
Epidemiological data on cryptococcosis in children are scarce, and we provided a comparatively large sample of data using a comprehensive clinical analysis. However, this study had some limitations. It was a single-center inpatient-based retrospective study with a high rate of loss to follow-up. Additionally, there was a wide range of follow-up periods. Finally, we did not determine the molecular type of the involved species. As the epidemiology of Cryptococcus spp. appears to be changing [17], species classification and further molecular typing would allow for a better understanding of the epidemiology of pediatric cryptococcosis in Chinese children.
Conclusions
The majority of cryptococcosis cases in China occurred in children without underlying conditions. These infections damaged multiple organs, with the central nervous system being the most common involved site. Neurological complications and mortality occurred in patients who had headaches, seizures, and high CSF antigen titers.
Abbreviations
- 5-FC:
-
5-Flucytosine
- AIDS:
-
Acquired immune deficiency syndrome
- AmB:
-
Amphotericin B deoxycholate
- CM:
-
Cryptococcal meningitis
- CNS:
-
Central nervous system
- CRP:
-
C-reactive protein
- CSF:
-
Cerebrospinal fluid
- ESR:
-
Erythrocyte sedimentation rate
- Flu:
-
Fluconazole
- HIV:
-
Human immunodeficiency virus
- MBL:
-
Mannose-binding lectin
- MRA:
-
Magnetic resonance angiography
- MRI:
-
Magnetic resonance imaging
- MRV:
-
Magnetic resonance venography
- VOR:
-
Voriconazole
- WBC:
-
White blood cell
- XLA:
-
X-linked agammaglobulinemia
References
Abadi J, Nachman S, Kressel AB, Pirofski L (1999) Cryptococcosis in children with AIDS. Clin Infect Dis 28(2):309–313. doi:10.1086/515130
Chaudhary MW, Sardana K, Kumar P, Dewan V, Anand VK (2005) Disseminated infection with Cryptococcus neoformans var neoformans in an 8 years immunocompetent girl. Indian J Pediatr 72(1):85
Chen J, Varma A, Diaz MR, Litvintseva AP, Wollenberg KK, Kwon-Chung KJ (2008) Cryptococcus neoformans strains and infection in apparently immunocompetent patients, China. Emerg Infect Dis 14(5):755–762. doi:10.3201/eid1405.071312
Choi YH, Ngamskulrungroj P, Varma A, Sionov E, Hwang SM, Carriconde F, Meyer W, Litvintseva AP, Lee WG, Shin JH et al (2010) Prevalence of the VNIc genotype of Cryptococcus neoformans in non-HIV-associated cryptococcosis in the Republic of Korea. FEMS Yeast Res 10(6):769–778. doi:10.1111/j.1567-1364.2010.00648.x
Dromer F, Mathoulin-Pélissier S, Launay O, Lortholary O (2007) French Cryptococcosis Study Group. Determinants of disease presentation and outcome during cryptococcosis: the CryptoA/D study. PLoS Med 4(2):e21. doi:10.1371/journal.pmed.0040021
Fan BJ, Wang BQ, Zhang HZ, He LX, Zhang ZY (2013) Analysis on clinical characteristics of pulmonary cryptococcosis under different immune status. Chin J Myco 8(4):193–197 (in Chinese)
Fang W, Fa Z, Liao W (2015) Epidemiology of Cryptococcus and cryptococcosis in China. Fungal Genet Biol 78:7–15. doi:10.1016/j.fgb.2014.10.017
Gibson JF, Johnston SA (2015) Immunity to Cryptococcus neoformans and C. gattii during cryptococcosis. Fungal Genet Biol 78:76–86. doi:10.1016/j.fgb.2014.11.006
Goldman DL, Khine H, Abadi J, Lindenberg DJ, La P, Niang R, Casadevall A (2001) Serologic evidence for Cryptococcus neoformans infection in early childhood. Pediatrics 107(5):E66
Gumbo T, Kadzirange G, Mielke J, Gangaidzo IT, Hakim JG (2002) Cryptococcus neoformans meningoencephalitis in African children with acquired immunodeficiency syndrome. Pediatr Infect Dis J 21(1):54–56
Guo J, Zhou J, Zhang S, Zhang X, Li J, Sun Y, Qi S (2012) A case-control study of risk factors for HIV-negative children with cryptococcal meningitis in Shi Jiazhuang, China. BMC Infect Dis 12:376. doi:10.1186/1471-2334-12-376
Guo LY, Liu LL, Liu Y, Chen TM, Li SY, Yang YH, Liu G (2016) Characteristics and outcomes of cryptococcal meningitis in HIV seronegative children in Beijing, China, 2002-2013. BMC Infect Dis 16(1):635
Hu XP, Wu JQ, Zhu LP, Wang X, Xu B, Wang RY, Ou XT, Weng XH (2012) Association of Fcγ receptor IIB polymorphism with cryptococcal meningitis in HIV-uninfected Chinese patients. PLoS One 7(8):e42439. doi:10.1371/journal.pone.0042439
Huang KY, Huang YC, Hung IJ, Lin TY (2010) Cryptococcosis in nonhuman immunodeficiency virus-infected children. Pediatr Neurol 42(4):267–270. doi:10.1016/j.pediatrneurol.2009.10.015
Jaın BB, Bose D, Mondal R, Chattopadhyay S (2014) Disseminated Cryptococcosis in an immunocompetent child. Turk Patoloji Derg. doi:10.5146/tjpath.2014.01230
Joshi NS, Fisher BT, Prasad PA, Zaoutis TE (2010) Epidemiology of cryptococcal infection in hospitalized children. Pediatr Infect Dis J 29(12):e91–e95. doi:10.1097/INF.0b013e3181fbc83d
Kidd SE, Hagen F, Tscharke RL, Huynh M, Bartlett KH, Fyfe M, Macdougall L, Boekhout T, Kwon-Chung KJ, Meyer W (2004) A rare genotype of Cryptococcus gattii caused the cryptococcosis outbreak on Vancouver Island (British Columbia Canada). Proc Natl Acad Sci 101:17258–17263. doi:10.1073/pnas.0402981101
Likasitwattanakul S, Poneprasert B, Sirisanthana V (2004) Cryptococcosis in HIV-infected children. Southeast Asian J Trop Med Public Health 35(4):935–939
Liu K, Ding H, Xu B, You R, Xing Z, Chen J, Lin Q, Qu J (2016) Clinical analysis of non-AIDS patients pathologically diagnosed with pulmonary cryptococcosis. J Thorac Dis 8(10):2813–2821. doi:10.21037/jtd.2016.10.36
Lizarazo J, Escandón P, Agudelo CI, Castañeda E (2014) Cryptococcosis in Colombian children and literature review. Mem Inst Oswaldo Cruz 109(6):797–804
Luo FL, Tao YH, Wang YM, Li H (2015) Clinical study of 23 pediatric patients with cryptococcosis. Eur Rev Med Pharmacol Sci 19(20):3801–3810
Meiring ST, Quan VC, Cohen C, Dawood H, Karstaedt AS, McCarthy KM, Whitelaw AC (2012) Govender NP; Group for Enteric, respiratory and meningeal disease surveillance in South Africa (GERMS-SA). A comparison of cases of paediatric-onset and adult-onset cryptococcosis detected through population-based surveillance, 2005-2007. AIDS 26(18):2307–2314. doi:10.1097/QAD.0b013e3283570567
Meyer W, Castañeda A, Jackson S, Huynh M, Castañeda E (2003) Molecular typing of IberoAmerican Cryptococcus neoformans isolates. Emerg Infect Dis 9(2):189–195. doi:10.3201/eid0902.020246
Miglia KJ, Govender NP, Rossouw J, Meiring S (2011) Mitchell TG; Group for Enteric, respiratory and meningeal disease surveillance in South Africa. Analyses of pediatric isolates of Cryptococcus neoformans from South Africa. J Clin Microbiol 49(1):307–314. doi:10.1128/JCM.01277-10
Mullan PC, Steenhoff AP, Draper H, Wedin T, Bafana M, Anabwani G, Jibril H, Tshepo M, Schutze GE (2011) Etiology of meningitis among patients admitted to a tertiary referral hospital in Botswana. Pediatr Infect Dis J 30(7):620–622. doi:10.1097/INF.0b013e318210b51e
Murphy SN, Parnell N (2005) Fluconazole treatment of cryptococcal rib osteomyelitis in an HIV-negative man. A case report and review of the literature. J Inf Secur 51(5):e309–e311. doi:10.1016/j.jinf.2005.02.028
Natukunda E, Musiime V, Ssali F, Kizito H, Kityo C, Mugyenyi P (2011) A case of Cryptococcal lymphadenitis in an HIV-infected child. AIDS Res Hum Retrovir 27(4):373–376. doi:10.1089/aid.2010.0167
Ou XT, Wu JQ, Zhu LP, Guan M, Xu B, Hu XP, Wang X, Weng XH (2011) Genotypes coding for mannose-binding lectin deficiency correlated with cryptococcal meningitis in HIV-uninfected Chinese patients. J Infect Dis 203(11):1686–1691. doi:10.1093/infdis/jir152
Pappas PG, Perfect JR, Cloud GA, Larsen RA, Pankey GA, Lancaster DJ, Henderson H, Kauffman CA, Haas DW, Saccente M et al (2001) Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis 33(5):690–699. doi:10.1086/322597
Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM (2009) Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 23(4):525–530. doi:10.1097/QAD.0b013e328322ffac
Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, Harrison TS, Larsen RA, Lortholary O, Nguyen MH et al (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis 50(3):291–322. doi:10.1086/649858
Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR (2013) Epidemiology of cryptococcal meningitis in the US: 1997-2009. PLoS One 8(2):e56269. doi:10.1371/journal.pone.0056269
Randhawa HS, Kowshik T, Chowdhary A, Prakash A, Khan ZU, Xu J (2011) Seasonal variations in the prevalence of Cryptococcus neoformans var. grubii and Cryptococcus gattii in decayed wood inside trunk hollows of diverse tree species in north-western India: a retrospective study. Med Mycol 49(3):320–323. doi:10.3109/13693786.2010.516457
Severo CB, Xavier MO, Gazzoni AF, Severo LC (2009) Cryptococcosis in children. Paediatr Respir Rev 10(4):166–171. doi:10.1016/j.prrv.2009.06.009
Yamaguchi H, Komase Y, Ikehara M, Yamamoto T, Shinagawa T (2008) Disseminated cryptococcal infection with eosinophilia in a healthy person. J Infect Chemother, 2008 14(4, Aug 17):319–324. doi:10.1007/s10156-008-0618-z.Epub
Yuanjie Z, Jianghan C, Nan X, Xiaojun W, Hai W, Wanqing L, Julin G (2012) Cryptococcal meningitis in immunocompetent children. Mycoses 55(2):168–171. doi:10.1111/j.1439-0507.2011.02063.x
Zhang C, Du L, Cai W, Wu Y, Lv F (2014) Isolated hepatobiliary cryptococcosis manifesting as obstructive jaundice in an immunocompetent child: case report and review of the literature. Eur J Pediatr 173(12):1569–1572. doi:10.1007/s00431-013-2132-2
Zhu LP, Wu JQ, Xu B, Ou XT, Zhang QQ, Weng XH (2010) Cryptococcal meningitis in non-HIV-infected patients in a Chinese tertiary care hospital, 1997–2007. Med Mycol 48:570–579. doi:10.3109/13693780903437876
Acknowledgements
We thank Dr. Mobeen Rathore for his valuable suggestions and critical review of this manuscript.
Author information
Authors and Affiliations
Contributions
All of the authors had access to the full dataset (including the statistical reportsand tables) and take responsibility for the integrity of the data and the accuracy of the data analysis. Gang Liu, Yonghong Yang, Lingyun Guo, Linlin Liu, Yue Liu and Shaoying Li conceived and designed thestudy. Gang Liu, Lingyun Guo, Linlin Liu, Yue Liu and Tianming Chen collected the data and designed the analysis. Gang Liu, Yonghong Yang, Lingyun Guo, Linlin Liu and Yue Liu interpreted the data. Lingyun Guo and Linlin Liu wrote the first draft of the paper. Gang Liu, Lingyun Guo and Linlin Liu reviewed and approved the final report.
Corresponding author
Ethics declarations
Funds
This work was supported by the Beijing Municipal Administration of Hospitals Incubating Program (No. PX2016035) and the Beijing Health System Top Level Health Technical Personnel Training Plan (No. 2015-3-082).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and informed consent
This study was reviewed and approved by the Ethics Committee of Beijing Children’s Hospital Affiliated to Capital Medical University (2017-k-26). Because this is a retrospectively study, we obtained the data of patients from the Medical Records and Statistics Room and we analyzed the data anonymously; thus, informed consent was not required.
Additional information
Communicated by Nicole Ritz
Rights and permissions
About this article
Cite this article
Liu, L., Guo, L., Liu, Y. et al. Clinical characteristics and prognosis of pediatric cryptococcosis in Beijing Children’s Hospital, 2002–2014. Eur J Pediatr 176, 1235–1244 (2017). https://doi.org/10.1007/s00431-017-2974-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2974-0