Abstract
Preoperative anxiety is a major problem in paediatric surgical patients. Melatonin has been used as a premedicant agent and data regarding effectiveness are controversial. The primary outcome of this randomized clinical trial was to evaluate the effectiveness of oral melatonin premedication, in comparison to midazolam, in reducing preoperative anxiety in children undergoing elective surgery. As secondary outcome, compliance to intravenous induction anaesthesia was assessed. There were 80 children undergoing surgery randomly assigned, 40 per group, to receive oral midazolam (0.5 mg/kg, max 20 mg) or oral melatonin (0.5 mg/kg, max 20 mg). Trait anxiety of children and their mothers (State-Trait Anxiety Inventory) at admission, preoperative anxiety and during anaesthesia induction (Modified Yale Pre-operative Anxiety Scale), and children’s compliance with anaesthesia induction (Induction Compliance Checklist) were all assessed. Children premedicated with melatonin and midazolam did not show significant differences in preoperative anxiety levels, either in the preoperative room or during anaesthesia induction. Moreover, compliance during anaesthesia induction was similar in both groups.
Conclusions: This study adds new encouraging data, further supporting the potential use of melatonin premedication in reducing anxiety and improving compliance to induction of anaesthesia in children undergoing surgery. Nevertheless, further larger controlled clinical trials are needed to confirm the real effectiveness of melatonin as a premedicant agent in paediatric population.
What is Known: • Although midazolam represents the preferred treatment as a premedication for children before induction of anaesthesia, it has several side effects. • Melatonin has been successfully used as a premedicant agent in adults, while data regarding effectiveness in children are controversial. |
What is New: • In this study, melatonin was as effective as midazolam in reducing children’s anxiety in both preoperative room and at induction of anaesthesia. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of children, even those well prepared and with a positive attitude, experience stress and anxiety in the operating theatre and during the postoperative period. In particular, anaesthesia induction is known to be the most anxiety provoking part of the preoperative experience [24].
Pain and anxiety are often related in surgery, in association with environmental changes such as a hospital stay, medication, and oxidative stress (OS). Increased levels of OS during the inflammatory response also contribute to nociception. Furthermore, reactive oxygen species and reactive nitrogen species can act directly and indirectly to induce nociceptor sensitization and activation [34]. It has been documented that OS occurs early already in pregnancy and continues in the neonatal and paediatric period [19]. Prolonged pain exposure triggers the production of pro-inflammatory cytokines, such as IL-1β, IL-6, and TNF-α. Moreover, it has been reported that procedural pain causes higher levels of pro-inflammatory cytokines [7].
Positive correlation between anxiety and pain is a common finding in the clinical setting, and it is known that pain-related anxiety can increase perceived pain intensity [31]. Moreover, it is recognized that preoperative anxiety is involved in postoperative outcomes and represents an independent predictor for postoperative negative behaviours [40]. Therefore, perioperative anxiety is part of the larger problem of anxiety associated with medical environments involving children, and several strategies have been adopted to reduce it, including sedative premedication. In detail, the goals for pharmacological premedication are the promotion of short-term amnesia and anxiolysis, reduction of secretions and vagal reflexes after intubation, properly preparing patients for induction, and enhancing the hypnotic effects of general anaesthesia [40].
Midazolam, a fast-acting benzodiazepine with a short elimination half-life, represents the preferred treatment as a premedication for children before induction of anaesthesia. It has, in fact, sedative, anxiolytic, hypnotic, and anterograde amnesic properties. However, midazolam has several side effects including paradoxical reactions, interactions with opioids, excessive sedation, disorientation, and impaired psychomotor performance.
Melatonin is an endogenous indoleamine produced and secreted by the pineal gland, mainly known as a regulator of circadian rhythms. In addition to sleep promotion, melatonin exerts numerous other sedative and anti-excitatory effects that support use during anaesthetic procedures, from premedication to induction of general anaesthesia [1, 21]. Previous studies demonstrated that melatonin is as effective as midazolam in reducing preoperative anxiety in adults [30], but data on paediatric patients are still controversial, as the only two published studies [14, 35] that investigated the anxiolytic effect of melatonin in children undergoing surgery reported opposite results. Samarkandi et Colleagues [35] reported that melatonin was as effective as an anxiolytic oral midazolam, unlike Kain et al. [14] who found that not only was melatonin inferior to midazolam, but also, it did not differ from placebo.
Recently, it has been demonstrated that premedication with melatonin decreases anxiety and pain levels in neonates and children undergoing painful procedures [8, 22] and that melatonin premedication, in comparison to midazolam, significantly reduces the dose of propofol required for induction of anaesthesia in paediatric patients [9].
The aim of this prospective randomized study was to compare the effects of oral melatonin premedication on preoperative anxiety and compliance during induction of anaesthesia, in comparison to midazolam premedication, in children undergoing elective surgery.
Materials and methods
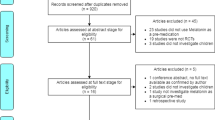
In this double-blind, randomized trial, the study population consisted of 80 children, aged 8–14 yrs., American Society of Anesthesiologists physical status I or II, scheduled for elective surgery at the Paediatric Surgery Department of the University Hospital of Messina, Italy, between January 2012 and December 2013. The study was approved by the local institutional ethics committee, and written informed consent was obtained from the patients’ legal guardians.
Patients’ medical reports
A physician performed the clinical examination for each child (80 children, aged 8–14 yrs), and an amnestic data were collected. Exclusion criteria were patients who had taken benzodiazepines, opioid drugs, or any other sedative in the previous month, those who had previously undergone sedation, prematurity, developmental delay, behavioural disorders, or patients undergoing emergency surgery.
The primary end-point of this study was the anxiety manifested by children in the operating room undergoing the induction of anaesthesia. Children’s compliance during the induction of anaesthesia was a secondary end-point.
The day before surgery, after recruitment, and informed written consent being obtained, trait anxiety of children and their mothers was separately assessed by two psychologists, using the State-Trait Anxiety Inventory for Children (STAI-C) and the State-Trait Anxiety Inventory (STAI).
On the day of surgery, patients were randomly assigned to two groups receiving either 0.5 mg/kg (max 20 mg) oral melatonin premedication (group A) or 0.5 mg/kg (max 20 mg) oral midazolam premedication (group B) before induction anaesthesia with propofol. Allocation to treatment groups was undertaken by an independent researcher using a permuted block design. A fixed block size of 10 was used to ensure that equal numbers of participants were randomized into the two groups (ratio 1:1). Randomization details were provided in an opaque sealed envelope containing allocation. Following hospital policy, all elective surgery procedures were performed early in the morning, and, therefore, in all children, premedication was performed between 07:30 a.m. and 09:30 a.m.. Approximately 40 min before induction of general anaesthesia, patients were transported to a quiet room in the operating suite where they received melatonin or midazolam orally. The melatonin (Melamil® oral drops, Milte Italia SpA, Milan, Italy) was prepared by a dedicated resident in a fixed volume of 5 ml adding water to a syringe without needle. To simulate the sweet taste of the melatonin formulation used, midazolam was expanded to the fixed volume with 5% dextrose. The content of the syringe, in both cases marked with a coded label, was blindly administrated to patients by the attendant nurse, not involved in the study.
Parents were not present at induction of anaesthesia. The children’s anxiety level, immediately after separation from parents, was independently evaluated by the same two psychologists blinded to the premedication treatment arm using the Modified Yale Pre-operative Anxiety Scale (m-YPAS) before leaving the preoperating room and, in theatre, during anaesthesia induction. Moreover, children’s compliance with induction (Induction Compliance Checklist- ICC) was assessed.
The induction of general anaesthesia was obtained in all children through bolus doses of 1 mg/kg over 20 s of intravenous propofol, followed by similar bolus doses of propofol until the patient was anaesthetised, and anaesthesia was maintained with inhaled sevoflourane. As the intravenous cannula needed for the propofol infusion had been previously inserted in the surgical paediatric ward, 2 hours before carrying the child in the operating theatre, the evaluation of anxiety related to cannulation had not been performed. However, local anaesthetic cream containing lidocaine and prilocaine (EMLA 5%) had been used to minimize pain and discomfort. The child was manually restrained if he/she became noncompliant during induction, and no other measures to limit pain due to propofol injection were adopted.
Instruments
-
STAI [37] and STAI-C [36] have been used extensively in research with both adults and children to provide a measure of individual differences in proneness to anxiety. This self-report anxiety instrument contains two separate subscales that measure trait (baseline) and state (situational) anxiety. Each scale contains 20 items that require the respondent to rate how often they generally experience tension, nervousness, and apprehension on a 4-point scale (1 = hardly ever, 2 = sometimes, 3 = often, 4 = almost always). State anxiety items include: “I am tense; I am worried” and “I feel calm; I feel secure.” Trait anxiety items include: “I worry too much over something that really doesn’t matter” and “I am content; I am a steady person”. The items are rated on a scale of 1–4. Total scores range from 20 to 80. Higher scores indicate greater anxiety.
STAI has high internal consistency and high test–retest reliability. Also in the present study, the internal consistency coefficients ranged from 0.86 to 0.95 and the test-retest coefficients ranged from 0.69 to 0.89.
-
The mYPAS is an observational measure of anxiety and contains 22 items in five categories (activity, emotional expressivity, state of arousal, vocalization, and use of parents) that indicate preoperative anxiety in children. The mYPAS score ranges from 22.5 to 100, with higher scores indicating greater anxiety. It has excellent reliability and validity for measuring children’s anxiety in the preoperative holding area and during induction of anaesthesia [11]. In this study, reliability (r) in the pre-operative holding area (0.87) and at induction of anaesthesia (0.88) were very good.
-
The ICC is an observational checklist, previously developed by Kain et al. [12], containing ten negative behavioural groupings that describe a child’s anxiety, fear, and negative behaviours during induction of anaesthesia, with good reliability. The ICC score is the sum of the items checked. Perfect induction i.e. the child does not exhibit negative behaviours, fear, or anxiety, is scored as 0. ICC ≥ 4 is considered poor behavioural compliance. This instrument has very high interclass r values between observers and, also, in this study interclass r values were high (0.98).
Data analysis
Sample size was based on a previous study involving anxiety levels in children undergoing induction of anaesthesia [13]. A mean anxiety score of 50 ± 12 (mYPAS score; mean ± SD) has been reported before induction of anaesthesia [13]. The null hypothesis of this study was that there was no difference in anxiety between children premedicated with melatonin or midazolam. Thus, a sample size of 32 subjects in each group was calculated to be sufficient to detect a 25% difference in anxiety level with a power of 0.80 and an α of 0.05.
Examined variables did not present normal distribution as verified by the Kolmogorov Smirnov test; consequently, the non-parametric approach was used. To analyse differences in trait and state anxiety measures between children of the two premedication groups, and between their mothers, Mann-Whitney and Wilcoxon rank tests were performed. The Spearman’s rank correlation coefficient test was used to delineate interactions between mothers’ and children’s anxiety scores. We did not correct p values for multiple testing, which may increase the likelihood of type I errors.
Significance was accepted at p = 0.05. Data were analysed with SPSS 19.0 (SPSS Inc., Chicago, IL).
Results
Forty children were premedicated with melatonin and 40 with midazolam.
Patient characteristics are presented in Table 1. The median age of all patients enrolled was 9 years (Interquantile ranges- IQR 8–12); 64 (80%) were males and 16 (20%) females. This is due to the fact that elective surgeries were mostly performed for conditions occurring in males. In detail, principal diagnoses were the following: phimosis 25%, cryptorchidism 15%, appendicopathy 10%, varicocele 10%, hypospadias 5%, hydrocele or inguinal hernia 20%, and other minor diseases or conditions 15%. However, patients in the two treatment groups were comparable with respect to age, gender distribution, weight, and duration of anaesthesia. No statistically significant differences in state and trait anxiety levels were detected between mothers of children of the two groups (p = 0.677 and p = 0.829, respectively). As expected, a significant positive correlation between mothers’ and children’s state anxiety level was observed, both in the melatonin (r = 0.232; p = 0.037) and midazolam group (r = 0.242; p = 0.020).
Table 1 presents medians and interquantile ranges (IQR) of anxiety experienced by the children of the two groups. No significant differences in children’s state anxiety and trait anxiety were observed during the sampling.
Similarly, children premedicated with melatonin and midazolam did not show significant differences in anxiety levels, either in the preoperative room or during anaesthesia induction.
In addition, as an indicator of anxiety worsening due to upcoming surgery, difference between anxiety level in the preoperative room and at anaesthesia induction, was evaluated, resulting in a non significant increase in the melatonin group (p = 0.110), and borderline in the midazolam group (p = 0.051). Moreover, children premedicated with melatonin and with midazolam did not differ in compliance during induction of anaesthesia.
Discussion
Anaesthesia induction is recognized as the most stressful procedure of the perioperative period, and management of preoperative anxiety should be a part of the perioperative management of children. We found that children premedicated with melatonin and midazolam did not show significant differences in preoperative anxiety levels, either in the preoperative room or during anaesthesia induction. Moreover, compliance during anaesthesia induction was similar in both groups.
Midazolam was first introduced as a premedication for children in the 1980s and rapidly achieved widespread acceptance as a preferred treatment before induction of anaesthesia because of its rapid absorption and low incidence of nausea compared to other benzodiazepines [25], despite its preoperative use being argued [17]. Midazolam premedication may be associated with paradoxical reactions (delayed recovery, anxiety, behavioural changes, agitation), and irregular breathing patterns, arrhythmias, respiratory failure, and unusual or involuntary muscle movements may, rarely, be observed in children [4]. In light of these adverse effects with midazolam, and for the sedative and hypnotic properties associated with melatonin, the latter has been proposed as an alternative to midazolam as a premedicant agent in children undergoing procedures that require sedation or general anaesthesia [10]. Nevertheless, data on effectiveness of perioperative melatonin in paediatric patients are controversial. Samarkandi et al. [35] found that melatonin was not only as effective as midazolam in alleviating preoperative anxiety in children, but was associated with a tendency toward faster recovery, lower incidence of excitement at 10 min postoperatively and of sleep disturbance at week 2 postoperatively than that observed with midazolam. On the contrary, in another study, it has been demonstrated that midazolam was more effective than melatonin in reducing children’s anxiety at induction of anaesthesia, but the individuals who received melatonin showed less emergence of delirium compared to those who received midazolam [14]. In the present study, oral melatonin and midazolam premedication had comparable effects on preoperative anxiety in children who underwent elective surgery, both in the preoperative room and during anaesthesia induction. Moreover, children premedicated with melatonin experienced a non significant increase in anxiety levels between preoperative and induction assessment (p = 0.110), while weak evidence for a difference was observed in the midazolam group between preoperative and induction assessment (p = 0.051). As secondary outcome, compliance to anaesthesia induction was evaluated. By assessment of the ICC, we observed that children in the melatonin and midazolam group did not differ in compliance with induction of anaesthesia. Generally, oppositional and aggressive behaviours were absent; however, none of the children receiving melatonin needed physical restraint during the propofol injection, as against two children in the midazolam group. Therefore, in light of these results, in our experience, melatonin, as a premedicant agent, is as effective as midazolam.
In this study, time of recovery was not evaluated, and no case of delirium or impaired psychomotor skills was noted in either group, although this could be ascribed to the small sample of patients enrolled. However, in a previous study comparing melatonin and midazolam premedication, we calculated the Aldrete post anaesthesia recovery score after 10 min from conclusion of anaesthesia, and found it comparable in both groups [9].
The study presents a few possible limitations, one of which is that our population was mainly constituted of males. However, unlike in adult populations in which female sex has been identified as a risk factor for preoperative anxiety [3], the gender of the child has not been demonstrated to influence preoperative anxiety [39, 40]. Another limitation is the age range included in the study. Indeed, as we used self reporting anxiety scales, the population study was restricted to older children aged 8–14 years. Although the use of premedicant agents seems particularly useful in younger children, the majority of paediatric patients, who are hospitalized and subject to surgery, suffer anxiety from a number of sources: separation from parents, fear of surgery itself and potential pain afterward, fear disease and treatment, mutilation, loss of control, and inability to cope with their plight. For these reasons, we believed that all children should receive premedication before surgery. Further studies, using proper anxiety scales, could investigate the effectiveness of preoperative melatonin in younger children.
The use of several different dosages of oral or sublingual melatonin, from 0.05 mg/kg to 50 mg/kg [2] has been reported. We planned a dosage of 0.5 mg/kg (max 20 mg) on the basis of the knowledge of the dose dependent analgesic and sedative effects of melatonin [38] and on our previous experience [9]. After oral administration of melatonin, peak serum concentration is reached after approximately 60 min; thereafter, concentration declines after a 4-h period. The sleep onset effect of oral melatonin has been reported to be around 30 min [26]. Conversely, oral midazolam acts more rapidly, and its effect is reported to start in 10 and end in 45 min [16]. We chose to administer both melatonin and midazolam 40 min before anaesthesia to maintain the double blind nature of the study, although this could represent a limitation of the study, as it is possible that the midazolam peak of action was missed.
In the present study, before melatonin premedication, the dosage of endogenous melatonin was not performed. Although interindividual differences in melatonin levels have been described, melatonin secretion occurs essentially during the night [5], whereas we administered melatonin between 07:30 a.m. and 09:30 a.m. to all children, as elective surgeries were scheduled early in the morning in compliance with hospital policy. Consequently, potential interindividual differences in melatonin secretion should not influence the effects of melatonin premedication.
Even though doubts have been raised regarding the safety of long-term melatonin treatment of sleep disorders in children [15], to date, safety issues have not been reported for short-term therapy. In this study, no related side effects were observed in the short term. Conversely, the potential beneficial effects of the antioxidant melatonin in children have been previously hypothesised [18, 20, 23]. Melatonin has antioxidant properties [6, 32] and can reduce the toxicity of a large number of drugs [33]. These actions of melatonin could be useful in children with diseases requiring surgical procedures, also considering the negative effects of anaesthetic drugs on the developing central nervous system [27] and that melatonin as an adjuvant agent, in animal models, could aid in reducing the neurotoxic side-effects of general anaesthetics [28, 29, 41].
In conclusion, this study adds new encouraging data supporting the use of melatonin in reducing anxiety and improving compliance to induction of anaesthesia in children. Further larger controlled clinical trials are needed to confirm the real effectiveness of melatonin premedication in children undergoing surgery.
Abbreviations
- ICC:
-
Induction Compliance Checklist
- IQR:
-
Interquantile ranges
- m-YPAS:
-
Modified Yale Pre-operative Anxiety Scale
- OS:
-
Oxidative stress
- STAI:
-
State-Trait Anxiety Inventory
- STAI-C:
-
State-Trait Anxiety Inventory for Children
References
Acil M, Basgul E, Celiker V, Karagöz AH, Demir B, Aypar U (2004) Perioperative effects of melatonin and midazolam premedication on sedation, orientation, anxiety scores and psychomotor performance. Eur J Anaesthesiol 21:553–557
Andersen LP, Werner MU, Rosenberg J, Gögenur I (2014) A systematic review of peri-operative melatonin. Anaesthesia 69:1163–1171. doi:10.1111/anae.12717
Caumo W, Schmidt AP, Schneider CN, Bergmann J, Iwamoto CW, Adamatti LC, Bandeira D, Ferreira MB (2001) Risk factors for postoperative anxiety in adults. Anaesthesia 56:720–728
Coté CJ, Karl HW, Notterman DA, Weinberg JA, McCloskey C (2000) Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics 106:633–664
Fourtillan JB, Brisson AM, Fourtillan M, Ingrand I, Decourt JP, Girault J (2001) Melatonin secretion occurs at a constant rate in both young and older men and women. Am J Physiol Endocrinol Metab 280:E11–E22
Galano A, Tan DX, Reiter RJ (2011) Melatonin as a naturally against oxidative stress: a physicochemical examination. J Pineal Res 51:1–14. doi:10.1111/j.1600-079X.2011.00916.x
Gitto E, Pellegrino S, Manfrida M, Aversa S, Trimarchi G, Barberi I, Reiter RJ (2012) Stress response and procedural pain in the preterm newborn: the role of pharmacological and non-pharmacological treatments. Eur J Pediatr 171:927–933. doi:10.1007/s00431-011-1655-7
Gitto E, Aversa S, Salpietro CD, Barberi I, Arrigo T, Trimarchi G, Reiter RJ, Pellegrino S (2012) Pain in neonatal intensive care: role of melatonin as an analgesic antioxidant. J Pineal Res 52:291–295. doi:10.1111/j.1600-079X.2011.00941.x
Gitto E, Marseglia L, D’Angelo G, Manti S, Crisafi C, Montalto AS, Impellizzeri P, Reiter RJ, Romeo C (2016) Melatonin versus midazolam premedication in children undergoing surgery: a pilot study. J Paediatr Child Health 52:291–295. doi:10.1111/jpc.13007
Isik B, Baygin O, Bodur H (2008) Premedication with melatonin vs midazolam in anxious children. Paediatr Anaesth 18:635–641. doi:10.1111/j.1460-9592.2008.02608.x
Kain ZN, Mayes LC, O’Connor TZ, Ciccheti DV, Caramico LA, Spieker M, Nygren MM, Rimar S (1995) Measurement tool for pre-operative anxiety in children: the Yale preoperative anxiety scale. Child Neuropsychol 1:203–210
Kain ZN, Mayes LC, Wang SM, Caramico LA, Hofstadter MB (1998) Parental presence during induction of anesthesia versus sedative pre-medication. Which intervention is more effective? Anesthesiology 89:1147–1156
Kain ZN, Caldwell-Andrews AA, Krivutza DM, Weinberg ME, Gaal D, Wang SM, Mayes LC (2004) Interactive music therapy as a treatment for preoperative anxiety in children: a randomized controlled trial. Anesth Analg 98:1260–1266
Kain ZN, MacLaren JE, Herrmann L, Mayes L, Rosenbaum A, Hata J, Lerman J (2009) Preoperative melatonin and its effects on induction and emergence in children undergoing anesthesia and surgery. Anesthesiology 111:44–49. doi:10.1097/ALN.0b013e3181a91870
Kennaway DJ (2015) Potential safety issues in the use of the hormone melatonin in paediatrics. J Paediatr Child Health 51:584–589. doi:10.1111/jpc.12840
Levine MF, Spahr Schopfer IA, Hartley E, Lerman J, MacPherson B (1993) Oral midazolam premedication in children: the minimum time interval for separation from parents. Can J Anaesth 40:726–729. doi:10.1007/BF03009769
Lönnqvist PA, Habre W (2005) Midazolam as premedication: is the emperor naked or just half-dressed? Paediatr Anaesth 15:263–265. doi:10.1111/j.1460-9592.2005.01600.x
Marseglia L, Aversa S, Barberi I, Salpietro CD, Cusumano E, Speciale A, Saija A, Romeo C, Trimarchi G, Reiter RJ, Gitto E (2013) High endogenous melatonin levels in critically ill children: a pilot study. J Pediatr 62:357–360. doi:10.1016/j.jpeds.2012.07.019
Marseglia L, D’Angelo G, Manti S, Arrigo T, Barberi I, Reiter RJ, Gitto E (2014) Oxidative stress-mediated aging during the fetal and perinatal periods. Oxidative Med Cell Longev 2014:358375. doi:10.1155/2014/358375
Marseglia L, D’Angelo G, Manti S, Salpietro C, Arrigo T, Barberi I, Reiter RJ, Gitto E (2014) Melatonin and atopy: role in atopic dermatitis and asthma. Int J Mol Sci 15:13482–13493. doi:10.3390/ijms150813482
Marseglia L, D’Angelo G, Manti S, Aversa S, Arrigo T, Reiter RJ, Gitto E (2015) Analgesic, anxiolytic and anaesthetic effects of melatonin: new potential uses in pediatrics. Int J Mol Sci 16:1209–1220. doi:10.3390/ijms16011209
Marseglia L, Manti S, D’Angelo G, Arrigo T, Cuppari C, Salpietro C, Gitto E (2015) Potential use of in procedural anxiety and pain in children undergoing blood withdrawal. J Biol Regul Homeost Agents 29:509–514
Marseglia L, D’Angelo G, Manti S, Aversa S, Reiter RJ, Antonuccio P, Centorrino A, Romeo C, Impellizzeri P, Gitto E (2015) Oxidative stress-mediated damage in newborns with necrotizing enterocolitis: a possible role of melatonin. Am J Perinatol 32:905–909. doi:10.1055/s-0035-1547328
McCann M, Kainz ZN (2001) Management of preoperative anxiety in children: an update. Anesth Analg 93:98–105
McMillan CO, Spahr-Schopfer IA, Sikich N, Hartley E, Lerman J (1992) Premedication of children with oral midazolam. Can J Anaesth 39:545–550. doi:10.1007/BF03008315
Mr S, Fairweather K (2006) The effect of melatonin on sedation of children undergoing magnetic resonance imaging. Br J Anaesth 97:220–225. doi:10.1093/bja/ael144
Nasr VG, Davis JM (2015) Anesthetic use in newborn infants: the urgent need for rigorous evaluation. Pediat Res 7:2–6. doi:10.1038/pr.2015.58
Ni C, Tan G, Luo A, Qian M, Tang Y, Zhou Y, Wang J, Li M, Zhang Y, Jia D, Wu C, Guo X (2013) Melatonin premedication attenuates isoflurane anesthesia-induced β-amyloid generation and cholinergic dysfunction in the hippocampus of aged rats. Int J Neurosci 123:213–220. doi:10.3109/00207454.2012.742895
Pascual R, Pilar Zamora-León S, Pérez N, Rojas T, Rojo A, José Salinas M, Reyes A, Bustamante C (2011) Melatonin ameliorates neocortical neuronal dendritic impairment induced by toluene inhalation in the rat. Exp Toxicol Pathol 63:467–471. doi:10.1016/j.etp.2010.03.006
Patel T, Kurdi MS (2015) A comparative study between oral melatonin and oral midazolam on preoperative anxiety, cognitive, and psychomotor functions. J Anaesthesiol Clin Pharmacol 31:37–43. doi:10.4103/0970-9185.150534
Ploghaus A, Narain C, Beckmann CF, Clare S, Bantick S, Wise R, Matthews PM, Rawlins JN, Tracey I (2001) Exacerbation of pain by anxiety is associated with activity in a hippocampal network. J Neurosci 21:9896–9903
Reiter RJ, Tan DX, Osuna C, Gitto E (2000) Actions of melatonin in the reduction of oxidative stress: a review. J Biomed Sci 7:444–458
Reiter RJ, Tan DX, Sainz RM, Mayo JC, Lopez-Burillo S (2002) Melatonin: reducing the toxicity and increasing the efficacy of drugs. J Pharm Pharmacol 54:1299–1321. doi:10.1211/002235702760345374
Salvemini D, Little JW, Doyle T, Neumann WL (2011) Roles of reactive oxygen and nitrogen species in pain. Free Radic Biol Med 51:951–966. doi:10.1016/j.freeradbiomed.2011.01.026
Samarkandi A, Naguib M, Riad W, Thalaj A, Alotibi W, Aldammas F, Albassam A (2005) Melatonin versus midazolam premedication in children: a double blind, placebo-controlled study. Eur J Anaesthesiol 22:189–196
Spielberger CD (1973) Manual for the State–Trait Anxiety Inventory for Children. Consulting Psychologists Press, Palo Alto
Spielberger CD, Gorsuch Lushene RE (1970) STAI manual for the State–Trait Anxiety Inventory. Consulting Psychologists Press, Palo Alto
Stefani LC, Muller S, Torres IL, Razzolini B, Rozisky JR, Fregni F, Markus R, Caumo W (2013) A phase II, randomized, double-blind, placebo controlled, dose-response trial of the melatonin effect on the pain threshold of healthy subjects. PLoS One 8:e74107. doi:10.1371/journal.pone.0074107
Vetter TR (1993) The epidemiology and selective identification of children at risk for preoperative anxiety reactions. Anesth Analg 77:96–99
Watson AT, Visram A (2003) Children’s preoperative anxiety and postoperative behavior. Paediatr Anaesth 13:188–204
Yon JH, Carter LB, Reiter RJ, Jevtovic-Todorovic V (2006) Melatonin reduces the severity of anesthesia-induced apoptotic neurodegeneration in the developing rat brain. Neurobiol Dis 21:522–530. doi:10.1016/j.nbd.2005.08.011
Author information
Authors and Affiliations
Contributions
Carmelo and Romeo Eloisa Gitto designed the study; Francesca Cuzzocrea, Rosalba Larcan, Tiziana Russo, and Maria Rosaria Gravina developed the methodology; Enrica Vinci, Maria Cristina Gugliandolo, and Angela Simona Montalto collected the data; Gabriella D’Angelo, Salvatore Arena, and Angela Alibrandi performed the analysis; and Lucia Marseglia and Pietro Impellizzeri wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of financial support
Prof Carmelo Romeo received 2513.70 euros as grant for a university research project (University of Messina) to support this study. All other authors declare that they did not receive any financial support for this research.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Jaan Toelen
Revisions received: 10 January 2017 / 20 April 2017 / 11 May 2017
Rights and permissions
About this article
Cite this article
Impellizzeri, P., Vinci, E., Gugliandolo, M.C. et al. Premedication with melatonin vs midazolam: efficacy on anxiety and compliance in paediatric surgical patients. Eur J Pediatr 176, 947–953 (2017). https://doi.org/10.1007/s00431-017-2933-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2933-9