Abstract
The Irish Childhood Diabetes National Register (ICDNR) was established in 2008 to define accurately the incidence and monitor the epidemiology of type 1 diabetes (T1D) in the Irish population. Here, we report data from the first 6 years of the National Register and compare with previous national data. Prospective national incident data regarding T1D in those under 15 years resident in Ireland were collected from 2008 to 2013 and national incidence rates (IRs) calculated. Ascertainment completeness was assessed using capture-recapture methodology. The period identified 1566 new cases of T1D, ascertainment reached 96.8 % in 2013. The standardised incidence rate was 27.5 in 2008 stabilising at 28.7 and 28.8 cases /100,000/year in 2012 and 2013. There was no evidence that the incidence changed significantly in the 6-year period either overall or for each age group and gender. There was evidence of a difference in the incidence of T1D across the age groups with the overall incidence highest in the 10–14 year age category. A strong seasonal association was demonstrated.
Conclusions: This study confirms Ireland as a high-incidence country for type 1 diabetes whilst demonstrating that the previous marked increase in IR from 16.3 cases/100,000/year in 1997 has not continued. Ongoing monitoring through the robust mechanism of the ICDNR is required to clarify whether this is a fluctuation or if the incidence of T1D diabetes has stopped rising in our population. Alternatively, this apparent stabilisation may reflect a shift to a later age at diagnosis.
“What is known :” • The incidence of Type 1 diabetes (T1D) is increasing in most populations worldwide although in certain high-incidence populations, it may be stabilising • There was a marked increase in T1D in Ireland between 1997 and 2008 • T1D incidence increases with affluence |
“What is New:” • The high incidence of T1D in Ireland has been confirmed at 28.8 cases/100,000/year in 2013 and has been effectively stable in the period 2008–2013 • Incidence is highest in Irish 10–14 year olds • Changes in incidence possibly reflecting life style and economic climate • Marked seasonality of diagnosis confirmed |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes in childhood is associated with serious medical and psychosocial complications; many of which can be prevented by good metabolic control [3, 27]. However, good metabolic control requires considerable multidisciplinary care [18, 19] which is resource intensive. In conditions of economic restraint, in which the majority of healthcare systems operate, careful targeting of these scarce resources is crucial to optimise disease outcomes. Robust reliable information is required to inform these decisions, and monitoring the epidemiology of incident type 1 diabetes is essential for effective service planning and appropriate resource allocation. This requires a national register with a robust information base [20].
The incidence of type 1 diabetes in childhood and adolescence is considered an important national health indicator by the World Health Organisation (WHO). The incidence of type 1 diabetes in childhood and adolescence has been increasing internationally in the majority of centres and in Europe has increased over a 20-year period (1989–2008) by approximately 3–4 % per annum [17].
There is marked international variation in the incidence of type 1 diabetes with almost a 600-fold difference between high- and low-incidence countries worldwide [26]. The incidence is highest in Europe and those of European descent with a marked north south gradient [15]. Finland has the highest incidence of type 1 diabetes in the world with a peak of 64.9 cases/100,000/year in 2006 [7] and amongst the lowest incidence at 2.37 and 3.1 cases/100,000/year is found in Asia [11, 29]. The incidence of diabetes has been subject to ongoing monitoring with regional and more rarely national diabetes registries since the 1990s with the World Health Organisation DIAMOND project [5] and more latterly by the Eurodiab collaboration [13].
A robust national study undertaken in 1997 noted for the first time that Ireland had a high incidence of type 1 diabetes at 16.3 cases/100,000/year [22]. In order to confirm the disease incidence, prospectively monitor the epidemiology of this important disease in the Irish population and support healthcare planning, the Irish Childhood Diabetes National Register (ICDNR) was established in January 2008 [20]. The aim of this study is to report the incidence data of the first 6 years of the Irish Childhood Diabetes National Register and examine trends in incidence in the Irish population.
Methods
National prospective recording of incident cases of type 1 diabetes under the age of 15 years, resident within the Republic of Ireland (ROI) at diagnosis and diagnosed by a physician was commenced on January 1, 2008 with the establishment of the Irish Childhood Diabetes National Register (ICDNR). The case definition was similar to that of the Diabetes Mondiale-Diamond study [28] and the earlier 1997 study [22]. All 20 paediatric centres nationally caring for those with diabetes prospectively notified cases, which were subsequently confirmed and additional information provided.
The degree of completeness of ascertainment was estimated using capture-recapture methodology [12, 28]. This was confirmed by a second source of identification provided by the central government agency, the Primary Care Reimbursement Service (PCRS) which finances care for those with diabetes. Further detail regarding the methodology of the ICDNR has been previously published [21]. Ascertainment rates for the primary source (the ICDNR) were calculated to provide a measure of the ability of the ICDNR to detect incident cases of diabetes in the population.
Data were recorded on a wide range of clinical and sociodemographic characteristics including age, gender, birth history, birth order, ethnicity, geographical location, parental occupation, family history and clinical presentation. All participants are on insulin therapy.
Data were analysed using SPSS 22. Confidence intervals for rates were derived using Stata version 12 and for standardised rates using the normal approximation to the binomial using Microsoft Excel. The direct method of standardisation was employed, using the common standard population, to permit comparison of incidence rates internationally and over time [4]. The common standard population assumes equal numbers in each of the age groups 0–4.9, 5–9.9 and 10–14.9 years for each sex.
Ethical approval for the ICDNR was granted by the SJH/AMNCH Joint Research Ethics Committee in accordance with the Declaration of Helsinki.
Results
Participation rate
In the 6-year period (2008–2013), 1566 (816 male/750 female) incident cases of type 1 diabetes were notified. All centres nationally caring for children with diabetes participated in the ICDNR and notified incident cases. The overall participation rate in the ICDNR, the proportion of incident cases identified who consent to join the Register, was 98.4 % over the 6 years (2008–2013) with no significant difference between years (Fisher’s exact test, F = 8.67; p = 0.104). There were only 25 non-participants over the 6-year period; however, anonymised baseline information was available on all notifications for inclusion in incidence rate calculations. Reasons for non-participation in the Register include emigration, non-national status, inability to obtain consent despite numerous reminders or where a child is in the care system.
Ascertainment rates
Annual ascertainment rates for the ICDNR were 66.3, 75.4, 73, 95.1,95.4 and 96.8 % in the period 2008–2013.
Age and gender
The average age at diagnosis over the years ranged from 7.92 to 8.93 years and overall was 8.4 years (SD of 3.9). The ratio of male to female cases was 1.1:1, but this was not significant (χ 2 = 2.78, df = 1, p = 0.1).
Incidence rates
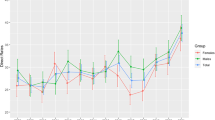
The crude incidence rates, which document the actual experience of the population regarding the number of new cases per year, ranged from 25.2 in 2008 to 28.4 cases/100,000/year in 2013. Age- and sex-category specific rates for the period are shown in Table 1, Fig. 1.
Poisson regression was used to examine the effects of age, gender and year on the age- and sex- category specific rates over the years. Each of the independent variables was treated as a categorical variable. The interactions between each of the three variables was also examined. There was no evidence of any interactions between any pair of variables, and there was no evidence of differences between years and genders. However, there was a significant difference between the age groups (χ 2 = 109.42, df = 2 p < 0.001). This effect did not depend on gender and year as mentioned above. The age difference suggested that the rate for age 5–9 age band was between 1.49 and 1.94 times higher than the rate for the 0–4 age group, and the rate for the 10–14 age group was between 1.72 and 2.23 times higher than the rate for the 0–4 age group (see Fig. 1).
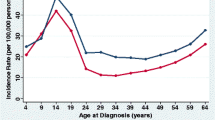
Standardised incidence rates, which correct for underlying changes in the population structure and permit comparison of incidence rate internationally and over time, were calculated. There were minor fluctuations during the 6-year period of the Register; the standardised incidence rates (95 % confidence intervals) were 27.5 (24.0, 30.9); 26.0 (22.7, 29.3); 25.6 (22.3, 28.8); 28.6 (25.2, 31.9); 28.7 (25.3, 32.1) and 28.8 (25.4, 32.1) cases/100,000/year respectively from 2008 to 2013. The standardised incidence rate was effectively unchanged between 2012 and 2013 (Fig. 2).
Month of diagnosis
There was no difference between years in the monthly pattern of diabetes onset (χ 2 = 65.43, df = 55, p = 0.158). The highest number of cases across all years were diagnosed in January, with diagnosis in the winter months of November, December and January being the most common (χ 2 = 47.97, df = 11, p < 0.0001 (Fig. 3).
Discussion
Monitoring the epidemiology of incident type 1 diabetes is essential for service provision, resource allocation, disease monitoring and audit. National registries, such as the ICDNR, provide a robust information base on which to make informed health planning decisions.
The previous 1997 study of national incidence, which used the same methodology, demonstrated that type 1 diabetes incidence was higher than expected in Irish children at 16.3/100,000/year, thereby establishing Ireland as a high-incidence country [22]. The ICDNR demonstrates that this high incidence has been maintained. In addition, there has been a substantial increase in incidence when compared with this first study where the standardised incidence rate (SIR) of type 1 diabetes increased from 16.3 to 27.5 cases/100,000/year between 1997 and 2008 [21]. There have been marked changes in lifestyle, family structure and medical care in Ireland over the last 20 years. Childhood infectious diseases have decreased, increased vaccinations are provided and medication use has increased. Increasing affluence has been associated with changed behaviours, particularly relating to diet and activity for children and adults. However, this increased SIR appears to have stabilised in the period 2008–2013 at this higher rate, with a SIR of 28.8/100,000/year in 2013.
The ascertainment rate of the ICDNR was falsely low in the early years of the Register due to innacuracies in the secondary case identification source (PCRS). This suspicion was confirmed by a further study using the local health offices as a secondary source of case identification; these local offices take reports from the treating hospitals and provide the information to the PCRS. Using these data from the local health offices, the ICDNR ascertainment levels were 88.9, 96.9 and 100 % compared with 66.3, 75.4 and 73 % when using PCRS data alone in the years 2008–2010 and 92.2 % in the period 2008/2009, which has been previously published [21]. Through ongoing collaboration with the PCRS and further rounds of verification, the ascertainment level of the ICDNR continues to improve. The ascertainment rate of the ICDNR is high, maintained at over 95 % since 2009 [21] and has improved to 96.8 % in 2013. Thus, this apparent stabilisation of incidence rates is not due to reduced ascertainment (which if anything has improved). That the incidence has remained relatively stable over the first 6 years of the ICDNR despite improved ascertainment may suggest a stabilisation in incidence rates and that whatever environmental agent(s) that prompted the increase in the late 1990s/early 2000s has now passed. A number of other studies have described an association between increasing affluence and rising incidence rates [8, 14]. Ireland experienced a period of sustained economic prosperity, evidenced by rising gross domestic product (GDP) from 1995 until 2007; thereafter, GDP fell and the country entered a period of recession and austerity, with GDP only returning to 2007 levels in 2014 [10]. It is interesting that Ireland experienced an increase in incidence from 1997 during its “Celtic tiger” years of economic prosperity and a slowing or stabilisation of incidence at a time when the economy has contracted (or GDP has fallen). Ireland would be expected to be a high-incidence country, considering its ethnicity and geographical location and that this high incidence has been maintained is not surprising. While it would not be expected that diabetes incidence rates would follow the fall in GDP so closely, a prompt increase in incidence rates was also be noted in the Irish population between 1997 and 2008 when GDP was rising.
It is possible that this apparent stabilisation in the incidence of T1D in childhood and adolescence could merely reflect a shift to a later presentation. Unfortunately, similar to many other countries, there are no data available regarding the incidence of type 1 diabetes in those aged over 15 years or in young adults in Ireland. Monitoring of type 1 diabetes incidence across the lifespan would be required to address this issue and be ideal; however, ascertainment would be particularly challenging.
Other centres, such as Finland, Norway and Sweden, are suggesting that type 1 diabetes may have stabilised in their populations also [1, 7, 23]. However, there is concern that the time frame in these studies or the analysis is not sufficient to draw such a conclusion [26]. Previous studies by Patterson et al. in their evaluation of 23 Eurodiab centres over a 20-year period demonstrate that increases in IRs are not uniform over time [17] and it is thought demonstrate 4–6 year cycles [9, 17]. The change in the Irish population may reflect a fluctuation in incidence rates as experienced in other centres rather than a true stabilisation in incidence rates. However, it is too early to say. To confirm if the incidence of type 1 diabetes has stopped rising in the Irish childhood population or if the changes in IR represent merely a fluctuation [26], ongoing monitoring through the robust mechanism of the ICDNR is required.
The ICDNR is acceptable to clinicians, patients and their families with all centres participating and returning data; 98.4 % of incident cases consented to join the National Register over the first 6 years. The participation rate has increased since the Register was commenced remaining high in 2013 at 99.3 %.
The total number of new cases of type 1 diabetes diagnosed annually in those aged under 15 years increased each year. There were 248 cases in 2008 and by 2013, this had increased to 286.
The mean age at diagnosis ranges from 7.92 to 8.93 years and overall was 8.4 years. The highest incidence was in the 10–14 year age group, followed by the 5–9 year age group and the lowest in 0–4 year age group. We found the change relative to baseline in new cases of diabetes to be similar across the age groups. This is unlike other reports which have described the highest relative increase in the under 5’s [13, 6, 25]. However, we have not found this and the numbers of children being diagnosed in the 0–4 year age band do not appear to be increasing as rapidly as European research predicted to date [13].
Our results are similar to many centres, including Germany and Norway, which have also found that there are more children diagnosed in the older 10–14 age category [6, 13, 23]. The onset of diabetes in the adolescent years can be particularly challenging for young people and their families [2]. Additional resources are required to manage diabetes in this vulnerable age group. Teenagers already experiencing the normal challenges of adolescence when faced with a new diagnosis of type 1 diabetes can have difficulties in a number of areas, such as interacting with healthcare services, glycaemic control, adherence to treatment regimens, mental health and psychosocial issues which require an alternative approach and additional supports. In the Irish population, resources should now be directed to the care of those in the older age groups, where diabetes can be particularly challenging.
There is a slight but not significant excess of males which varies by year, and this is similar to reports from other high-incidence countries who note a slight but not significant excess of males under 15 years.
The highest number of cases were diagnosed in January and in the winter months of November and December. This seasonality in the onset of type 1 diabetes is well recognised [16, 24]. Recognition of the seasonality of diagnosis can help inform service delivery decisions.
Conclusions
The first 6 years of the ICDNR have confirmed the high incidence of type 1 diabetes in the Irish population which has been maintained and appears to have stabilised in the period 2008–2013. The Incidence is highest in the 10–14 year age group. Ongoing monitoring through the robust mechanism of the ICDNR is required to confirm if this stabilisation is merely a fluctuation in the disease incidence in the Irish population and whether the incidence will remain stable or increase. Monitoring of disease incidence across the lifespan while technically challenging would be ideal to prove whether the disease incidence is changing or merely a shift in the age of diagnosis. Continued monitoring of the numbers of newly diagnosed children with type 1 diabetes annually is important to inform health planning, tailor resources to target the needs of specific groups and support audit. New methods to prevent this important disease are required as all previous trials to date have failed.
Abbreviations
- GDP:
-
Gross domestic product
- ICDNR:
-
The Irish Childhood Diabetes National Register
- IRs:
-
Incidence rates
- PCRS:
-
Primary Care Reimbursement Service
- ROI:
-
Republic of Ireland/Ireland
- SJH/AMNCH:
-
St. James Hospital and the Adelaide and Meath Hospital incorporating the National Children’s Hospital
- T1D:
-
Type 1 diabetes
References
Berhan Y, Waernbaum I, Lind T (2011) Thirty years of prospective nationwide incidence of childhood type 1 diabetes. The accelerating increase by time trends to level off in Sweden. Diabetes 60(2):577–581
Cameron FJ, Amin R, de Beaufort C, Codner E, Acerini CL (2014) ISPAD clinical practice consensus guidelines—2014: diabetes in adolescence. Pediatr Diabetes 15(Suppl. 20):245–256
Cameron FJ, de Beaufort C, Aanstoot HJ, Hoey H, Lange K, Castano L, Mortensen HB, the Hvidoere International Study Group (2013) Lessons from the Hvidoere International Study Group on childhood diabetes: be dogmatic about outcome and flexible in approach. Pediatr Diabetes 14(7):473–480
Daly LE, Bourke GJ, McGilvray, J (1991) Interpretation and use of medical statistics, 4th edn. Blackwell Scientific publications, p 278
DIAMOND Project Group (2006) Incidence and trends of childhood type 1 diabetes worldwide 1990–1999. Diabet Med 23:857–866
Ehehalt S, Dietz K, Willasch AM, Neu A, for the Baden-Württemberg Diabetes Incidence Registry (DIARY) group (2010) Epidemiological perspectives on type 1 diabetes in childhood and adolescence in Germany 20 years of the Baden-Württemberg Diabetes Incidence Registry (DIARY). Diabetes Care 33:338–340
Harjutsalo V, Sund R, Knip M, Groop P (2013) Incidence of type 1 diabetes in Finland. JAMA 310(4):427–428
Haynes A, Bulsara MK, Bower C, Codde JP, Jones TW, Davis EA (2006) Independent effects of socioeconomic status and place of residence on the incidence of childhood type 1 diabetes in Western Australia. Paediaric Diabetes 7:94–100
Haynes A, Bulsara MK, Bower C, Jones TW, Davis EA (2012) Cyclical variation in the incidence of childhood type 1 diabetes in Western Australia (1985–2010. Diabetes Care 35(11):2300–2302
http://www.cso.ie/px/pxeirestat/Statire/SelectVarVal/Define.asp?maintable=NAHO4&Planguage=0, Central Statistics Office Databank accessed 27/10/2015
Kawasaki E, Matsuura N, Eguchi K (2006) Type 1 diabetes in Japan. Diabetologia 49:828–836
LaPorte RE, McCarthy D, Bruno G, Tajima N, Baba S (1993) Counting diabetes in the next millenium application of capture-recapture methodology. Diabetes Care 16:528–535
Patterson CC, Dahlquist GG, Gyurus E, Green A, Soltész G, and the EURODIAB study group (2009) Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–2020: a multicentre prospective registration study. Lancet 373:2027–2033
Patterson CC, Dahlquist G, Soltész G, Green A, on behalf of the EURODIAB ACE Study Group (2001) Is childhood-onset type I diabetes a wealth-related disease? An ecological analysis of European incidence rates. Diabetologia 44(Suppl 3):B9–16
Patterson CC, Guariguata L, Dahlquist G, Soltész G, Ogle G, Silink M, IDF Diabetes Atlas (2014) Diabetes in the young—a global view and worldwide estimates of numbers of children with type 1 diabetes. Diabetes Res Clin Pract 103:161–175
Patterson CC, Gyürüs E, Rosenbauer J, Cinek O, Neu A, Schober E, Parslow RC, Joner G, Svensson J, Castell C, Bingley PJ, Schoenle E, Jarosz-Chobot P, Urbonaite B, Rothe U, Krzisnik C, Ionescu-Tirgoviste C, Weets I, Kocova M, Stipancic G, Samardzic M, de Beaufort CE, Green A, Soltesz G, Dahlquist GG (2015) Seasonality variation in month of diagnosis in children with type 1 diabetes registered in 23 European centres during 1989–2008: little short-term influence of sunshine hours or average temperature. Paediatric. Diabetes 16(8):573–580
Patterson CC, Gyürüs E, Rosenbauer J, Cinek O, Neu A, Schober E, Parslow RC, Joner G, Svensson J, Castell C, Bingley PJ, Schoenle E, Jarosz-Chobot P, Urbonaité B, Rothe U, Krzisnik C, Ionescu-Tirgoviste C, Weets I, Kocova M, Stipancic G, Samardzic M, de Beaufort CE, Green A, Dahlquist GG, Soltész G (2012) Trends in childhood type 1 diabetes incidence in Europe during 1989–2008: evidence of non-uniformity over time in rates of increase. Diabetologia 55:2142–2147
Pihoker C, Forsander G, Fantahun B, Virmani A, Luo X, Hallman M, Wolfsdorf J, Maahs DM (2014) The delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatr Diabetes 15(Suppl. 20):86–101
Rewers MJ, Pillay K, de Beaufort C, Craig ME, Hanas R, Acerini CL, Maahs DM (2014) Assessment and monitoring of glycemic control in children and adolescents with diabetes. Pediatr Diabetes 15(Suppl. 20):102–114
Roche EF (2014) The National Paediatric Diabetes Register and its impact on healthcare. Ir Med J 107(7):197–198
Roche EF, McKenna A, Ryder K, Brennan A, O’Regan M, Hoey HMCV (2014) The incidence of childhood type 1 diabetes in Ireland and the National Childhood Diabetes Register. Ir Med J 107(9):278–281
Roche EF, Menon A, Gill D, Hoey HM (2002) Incidence of type 1 diabetes mellitus in children aged under 15 years in the Republic of Ireland. J Pediatr Endocrinol Metab 15(8):1191–1194
Skrivarhaug T, Stene LC, Drivvoll AK, Strøm H, Joner G, and the Norwegian Childhood Diabetes Study Group (2014) Incidence of type 1 diabetes in Norway among children aged 0–14 years between 1989 and 2012: has the incidence stopped rising? Results from the Norwegian Childhood Diabetes Registry. Diabetologia 57:57–62
Sloka S, Grant M, Newhook LA (2008) Time series analysis of ultraviolet B radiation and type 1 diabetes in Newfoundland. Paediatric. Diabetes 9:81–86
Svensson J, Carstensen B, Mølbak AG, Molbak A, Christau B, Mortensen HB, Nerup J, Borch-Johnsen K (2002) The Danish study group of diabetes in childhood. Increased risk of childhood type 1 diabetes in children born after 1985. Diabetes Care 25:2197–2201
Tuomilehto J (2013) The emerging global epidemic of type 1 diabetes. Curr Diab Rep 13:795–804
White NH, Cleary PA, Dahms W, Goldstein D, Malone J, Tamborlane WV, Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group (2001) Beneficial effects of intensive therapy of diabetes during adolescence: outcomes after the conclusion of the diabetes control and complications trial (DCCT). J Pediatr 139:804–812
WHO Multinational Project for Childhood Diabetes (Diabetes Mondiale) (1991) Diamond study, method of operations, version 2, Parts I-IV
Zhao Z, Sun C, Wang C, Li P, Wang W, Ye J, Gu X, Wang X, Shen S, Zhi D, Lu Z, Ye R, Cheng R, Xi L, Li X, Zheng Z, Zhang M, Luo F (2014) Rapidly rising incidence of childhood type 1 diabetes in Chinese population: epidemiology in Shanghai during 1997–2011. Acta Diabetol 51(6):947–953
Acknowledgments
We are grateful to the Primary Care Reimbursement Services (PCRS) for their assistance, Mr. B. Carr ICT Tallaght Hospital and Professor J Grimson, University of Dublin, Trinity College Dublin and HIQA, for their advice and support in the development of the ICDNR.
We are particularly grateful to all the participating centres, paediatric endocrinologists, paediatricians, parents and children with type 1 diabetes.
Authors’ contributions
E.R. conceived the project, wrote the manuscript and researched data. A.McK. researched data and reviewed/edited the manuscript. K.R. reviewed/edited the manuscript. A.B. reviewed/edited the manuscript. M.O’R. researched data and reviewed/edited the manuscript. H.H. contributed to the discussion and reviewed/edited the manuscript. E.R. is the guarantor for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study and the Irish Childhood Diabetes National Register was funded a grant from the National Children’s Hospital Foundation Ireland since its inception.
Conflict of interest
The authors declare that they have no competing interests. The authors do not have a financial relationship with the National Children’s Hospital Foundation who sponsored this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments. Ethical approval for the ICDNR was granted by the SJH/AMNCH Joint Research Ethics Committee in accordance with the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all individual participants included in the National Diabetes Register.
Additional information
Communicated by Beat Steinmann
Rights and permissions
About this article
Cite this article
Roche, E.F., McKenna, A.M., Ryder, K.J. et al. Is the incidence of type 1 diabetes in children and adolescents stabilising? The first 6 years of a National Register. Eur J Pediatr 175, 1913–1919 (2016). https://doi.org/10.1007/s00431-016-2787-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-016-2787-6