Abstract
Aortic dilation at the level of the aortic root can be caused by a variety of congenital or acquired conditions that lead to weakening of the aortic wall. In this retrospective study, we sought to determine the frequency of different associated diagnoses from children with aortic dilation seen at a single institution. A total of 377 children (68 % male) met study inclusion criteria. Patients were classified based on the suspected or confirmed associated diagnosis in one of the following categories: congenital heart disease (241/377, 64 %), chromosomal (34/377, 9 %), Marfan syndrome (26/377, 7 %), other genetic and non-genetic (22/377, 6 %), Loeys-Dietz syndrome (6/377, 2 %), and unknown (48/377, 13 %). Bicuspid aortic valve was by far the most prevalent congenital heart defect (206/241, 85 %), while Turner syndrome was the most frequent chromosomal abnormality (12/34, 35 %). Patients with Marfan syndrome were more likely to have severe dilation of the ascending aorta (p = 0.002) and to require aortic root replacement surgery (p < 0.001) compared to those in other diagnosis categories.
Conclusion: The differential diagnosis of aortic dilation is broad and requires a careful assessment of cardiac anatomy. Evaluation by a clinical geneticist in this setting should be strongly considered given the high frequency of associated genetic conditions.
What is Known: • Aortic dilation is frequent in bicuspid aortic valve and other congenital heart defects. • Aortic dilation can be seen in several connective tissue disorders. Limited information is available in regard to the differential diagnosis of aortic dilation in children. |
What is New: • In patients with aortic dilation concurrent congenital heart disease is frequently diagnosed. • Almost 18 % of cases in the present study had a defined presumptive or confirmed genetic diagnosis. We suggest considering a genetics evaluation in the setting of aortic dilation. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aortopathies are a group of disorders characterized by dilation, tortuosity, and aneurysms of the aorta. Aortic dilation (AoD) leading to aortic dissection has been associated with several syndromic connective tissue disorders such as Marfan syndrome (MFS; MIM154700), Loeys-Dietz syndrome (LDS; 609192), and Ehlers-Danlos syndrome (EDS) type IV (MIM 130050), among others [6–8, 22].
Aortopathy is also seen in other conditions apart from clearly defined connective tissue disorders, specifically congenital heart defects (CHD). The aorta in patients with bicuspid aortic valve (BAV), the most common CHD, may manifest similar histological changes to those seen in patients with MFS. De novo AoD occurs frequently in the setting of BAV and is not related to the presence of hemodynamically significant aortic valve stenosis or regurgitation [3]. Other CHDs reported to have de novo or postsurgical AoD and aortic dissection include conotruncal lesions, hypoplastic left heart syndrome, and coarctation of the aorta [1, 2, 18, 19, 23, 24]. Neo-aortic root dilation after arterial switch operation for d-transposition of the great arteries, Ross procedure for aortic valve disease, and balloon valvuloplasty for congenital aortic stenosis have also been observed [2, 14, 18].
The literature is more limited however in the differential diagnosis of AoD in children in the setting of recent advances in molecular genetic techniques. We sought to determine the most frequent associated genetic diagnoses in a large pediatric population with AoD.
Methods
Study design and definitions
After obtaining approval from the Arkansas Children’s Hospital Institutional Review Board, a retrospective review was performed in all patients with AoD evaluated at our center from January 1, 2009 to July 1, 2013. Study subjects were identified by querying the Syngo Dynamics v 9.0 (Siemens Healthcare, Vienna, Austria) database for all echocardiograms performed at our institution during the study period. Subjects were included if there was an echocardiographic diagnosis of at least mild dilation at the level of the aortic sinus of Valsalva or the ascending aorta. Additional inclusion criteria were age <18 years at the time of echocardiogram and prior evaluation by a cardiologist and/or geneticist at our institution. Exclusion criteria included: inability to identify the primary diagnosis, history of certain congenital heart defects (conotruncal anomalies, hypoplastic left heart syndrome, and heterotaxy), history of heart transplantation, and lack of persistence of the diagnosis of AoD in at least two separate studies in those with multiple echocardiograms. Medical records were systematically reviewed, and a separate database was created with the following data abstracted: age at echocardiogram, age at diagnosis of AoD, gender, anatomic location of the AoD, aortic dimensions, anthropometric measurements, genetic evaluation, family history, suspected or confirmed diagnoses, associated clinical findings, and concurrent CHDs, if present. When available, results of genetic testing were also reviewed.
For younger patients (from birth to 4 years of age) whose first echocardiographic evaluation occurred during the study period, the age at the first echocardiogram that demonstrated AoD objectively also represented the age at diagnosis of AoD. For older patients (ages 4 to 18 years), whenever possible, the first available study with AoD was used for analysis.
Family history was determined to be positive if first-degree relatives were affected with one of the following: CHD, MFS, other aortopathies (aortic dilation, dissection, rupture, or aneurysms), and other connective tissue disorder (EDS, LDS, or unknown). For the purpose of this study, the suspected or confirmed associated diagnosis included the following six categories: CHD, MFS, chromosomal (Turner syndrome and other chromosomal), LDS, other (genetic and non-genetic conditions), and unknown. Only patients with isolated, anatomical cardiovascular defects were classified in the category of “CHD.” Patients with major aneuploidies or submicroscopic pathogenic microdeletions/microduplications were classified into the “chromosomal” category. Patients who had other non-chromosomal genetic syndromes and associations either confirmed or highly suspected and those with other heart conditions different than CHDs (i.e., congenital AV blocks, cardiomyopathy, etc.) were classified into the “other” category. Lastly, patients who had multiple congenital anomalies, developmental delay, and/or dysmorphic features in whom a genetic diagnosis was not pursued or could not be confirmed were classified as “unknown.”
Echocardiographic measurements
Echocardiograms were performed with the patient in the supine position using commercially available ultrasound machines (Siemens Acuson Sequoia 512 with 10, 7, 5, and 3 MHz probes and Philips iE33 with 12, 8, and 5 MHz probes). The performing echosonographer and the cardiologist reading the study obtained two-dimensional measurements in accordance with the recommendations of the American Society of Echocardiography using parasternal long-axis views of the aortic sinus of Valsalva and ascending aorta [10]. Measurements were made from inner-edge to inner-edge during mid-systole. All measurements were made at the maximum diameter. Using the body surface area determined according to the method of Haycock, Z-scores were then calculated for the aortic sinus of Valsalva and ascending aorta measurements available for each subject using the regression equations by Warren et al. [5, 21]. For the purposes of this study, AoD was described as mild for Z-scores between 2 and 3.99, moderate for Z-scores between 4 and 5.99, and severe for Z-scores ≥ 6 [4].
Statistical analysis
All data were analyzed using R version 3.1.0 (R Foundation for Statistical Computing, Vienna, Austria). Summary statistics were expressed as median and interquartile range (1st quartile, 3rd quartile) for continuous variables and frequency and percentage for categorical variables. The distributions of continuous variables were compared among severity groups using the Kruskal-Wallis tests and between with and without replacement using the Mann-Whitney U tests, while the proportions of categorical variables were compared using the chi-square tests. p values <0.05 were considered statistically significant.
Results
Population description
A total of 1248 charts were reviewed, and data were collected on 377 patients (68 % male) who met study inclusion criteria. Because several patients had AoD at more than one level, a total of 421 observations were made. The median age at echocardiogram for the entire cohort was 11 years (range, 1 day–17 years) (Table 1). Only 84/377 patients (22 %) were evaluated by a geneticist. A total of 54/377 cases (14 %) had a positive family history, though in 140/377 cases (37 %), the family history was unknown.
Aortic dilation characteristics
Aortic dilation was most often reported in the ascending aorta, whether alone (238/377, 63 %) or in combination with the sinus of Valsalva (44/377, 12 %). Isolated dilation of the sinus of Valsalva was seen in 95/377 patients (25 %). The severity of AoD was mild in 60 % (252/421) of cases regardless of the location (Table 1).
Differential diagnosis
Congenital heart disease was the most frequent associated diagnosis (64 % of cases) (Table 1). BAV was the most prevalent defect in the present cohort and was seen in 242/377 patients (64 %), 206 of whom were classified within the CHD category. Indeed, BAV was seen in isolation, in combination with other heart or birth defects, and in several patients with other established primary genetic diagnoses. Other less common CHDs without BAV included coarctation of the aorta, aortic/subaortic stenosis, atrial septal or ventricular septal defects (ASD/VSD), pulmonary stenosis, Ebstein anomaly, and patent ductus arteriosus. MFS was the most commonly identified connective tissue disorder. Of the 26 cases (7 %), 13 had pathogenic mutations in the FBN1 gene while the others were diagnosed clinically using the old Ghent criteria or their revised version [11]. Only six patients with LDS were identified (2 %), all with pathogenic mutations in either TGFBR1 or TGFBR2. Of the 34 patients classified as chromosomal (9 %), Turner syndrome was the most frequent (12 cases), followed by 22q11.2 deletion (6 cases), and Down syndrome (2 cases). Of interest, all patients with Turner syndrome had CHD (10/12 with BAV, 83 %) but 8/22 (36 %) of the remaining patients with chromosomal abnormalities had structurally normal hearts by echocardiogram (including 2 patients with 22q11.2 deletion).
Aortic dilation was present in 15 patients (4 %) with a number of other genetic conditions such as VACTERL association (5 cases, 3 with no BAV), Shimke immunoosseous dysplasia (2 cases, both with structurally normal hearts), and Duchenne muscular dystrophy, among others. Other miscellaneous cardiac diagnoses associated with AoD included congenital AV block (3 cases), rheumatic fever (2 cases), endocarditis (1 case), and supraventricular tachycardia (1 case) (total 7/377 = 2 %). An underlying etiology for AoD could not be identified in the 13 % (48/377) of cases classified as unknown despite additional comprehensive genetic testing (microarrays, connective tissue gene panels, FBN1 sequencing, or other single genes) performed in many of them. Of these, only 7 (15 %) had isolated AoD with no underlying heart disease while the remaining 42 (85 %) had other birth defects, developmental delay, and/or dysmorphic features.
Clinical predictors and outcome
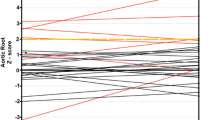
On univariate analysis of the 139 patients with AoD at the level of the sinus of Valsalva, no demographic or clinical variable was associated with the severity of dilation (data not shown). In the 282 patients with dilation of the ascending aorta, univariate analysis demonstrated that the presence of MFS (p = 0.002) was associated with increased likelihood of severe AoD (Table 2).
Eight patients in the cohort (2 %) underwent aortic root replacement (Table 3). The median age at surgery was 15 years (range 9–17 years). For all cases, severe AoD was the main indication alone (5 cases) or in combination with severe aortic (1 case) or mitral (2 cases) insufficiency. The latter 2 cases also underwent mitral valvuloplasty. Surgical intervention was most commonly undertaken in patients with MFS (3/26, 12 %) and LDS (1/6, 17 %). The latter was the only patient in the cohort who died (1/8, 12 %), and this as a complication of the surgery.
Discussion
The objective of this study was to investigate the differential diagnosis of AoD in the pediatric population focusing on associated genetic conditions. Overall, we found a high frequency of such conditions and positive family history. To our knowledge, no similar study has been conducted in a series of pediatric patients, making this information useful to the general pediatrician, geneticist, and/or cardiologist who may evaluate such patients.
Unsurprisingly, CHD (BAV in particular) was the most common associated diagnosis in the majority of patients. With an incidence of 1 to 2 % of live births, BAV is the most common form of CHD and is known to be associated with AoD in 45–50 % of affected patients [13, 15–17, 20, 23]. For those patients with AoD who do not have isolated BAV or other CHD, several associated diagnoses can be found. Overall, including patients with connective tissue disorders and chromosomal abnormalities, 18 % of cases had a defined presumptive or confirmed genetic diagnosis. When combined with the genetic nature of BAV, these findings strongly suggest that AoD and aortopathy have a primarily genetically mediated etiology. Based on our results and previous American Heart Association recommendations [6], we propose a practicing algorithm to aid pediatricians and cardiologists in the clinical evaluation of patients with AoD, highlighting the importance of a genetic evaluation (Fig. 1).
In this population, major aneuploidies were seen relatively frequently, in many cases with conditions that should be easily recognizable, such as Down syndrome and Turner syndrome. Although the majority of patients with Turner syndrome in the present study had BAV, this chromosomal anomaly has been identified previously as an independent risk factor for AoD [12]. The second most common chromosomal abnormality identified was 22q11.2 deletion syndrome, a condition that also appears to be an independent risk factor for AoD regardless of the presence of conotruncal defects [8, 9]. Structurally normal hearts, ASD/VSDs, and subaortic stenosis were frequent in the remaining cases suggesting that, in some instances and depending on the associated physical exam findings or medical history, primary chromosomal abnormalities should be ruled out prior to defining a case as being of “idiopathic” origin.
In addition to the better-known syndromic conditions that predispose to AoD such as MFS and LDS, other less common genetic conditions were diagnosed in this study. Given the single case occurrence of the majority of them, a direct link is difficult to establish.
Identifying a potential cause or associated diagnosis in the setting of AoD could have several implications. Besides the obvious potential of comorbidities that may need to be explored further and the genetic counseling associated with different conditions, making a specific genetic diagnosis could also help predict severity and/or potential need for surgical repair, as illustrated by the more severe dilation seen in patients with MFS and the greater chance of needing aortic root replacement for both MFS and LDS in the present study.
The present study is retrospective in nature and is subject to the limitations intrinsic to such an investigation. In some cases, the clinical data were based on those collected by others. Although the age when the AoD was diagnosed was possible to obtain in the large majority of cases, this study was not by design a natural history project. Therefore, the progression or potential resolution of the AoD was not analyzed. In some cases, a single echocardiogram was available for analysis, and therefore it was not possible to confirm persistence of AoD. The echocardiograms were not evaluated by a single cardiologist, likely resulting in some degree of interpretive variability although the use of aortic measurements and validated Z-scores to determine the severity of AoD obviates subjective interobserver variability to a large degree. Z-scores were classified as mild, moderate, or severe according to a previous report [4], and this categorization should not be mistaken for clinical importance. Equally important in this study, genetic evaluations were sometimes incomplete and when conducted, not routinely systematic or uniform with different tests ordered using a variety of platforms. Finally, while the sample size was relatively large, a prospective study is desirable to validate the present results.
In conclusion, this large retrospective study analyzed the associated diagnoses in children with AoD at a single institution. Despite the abovementioned limitations, based on these results, at our institution, we are now using the proposed practicing algorithm to determine who may benefit from further genetic evaluation or testing. We can also make some recommendations and meaningful conclusions. First, CHDs (BAV in particular) are the most commonly associated diagnoses in the setting of AoD. Second, given the combined high frequency of chromosomal anomalies, connective tissue disorders, and other less common genetic conditions, a referral for an evaluation by a geneticist is appropriate, especially in the context of other anomalies. Furthermore, a geneticist could also assist in the diagnostic evaluation of the relatively high frequency of unknown cases. Lastly, patients with MFS and LDS are more likely to need aortic root replacement surgery compared to other coexistent associated diagnoses or otherwise “isolated” cases of CHD.
Abbreviations
- AoD:
-
Aortic dilation
- ASD:
-
Atrial septal defect
- BAV:
-
Bicuspid aortic valve
- CHD:
-
Congenital heart defect
- EDS:
-
Ehlers-Danlos syndrome
- LDS:
-
Loeys-Dietz syndrome
- MFS:
-
Marfan syndrome
- VSD:
-
Ventricular septal TOF
References
Carlo WF, McKenzie ED, Slesnick TC (2011) Root dilation in patients with truncus arteriosus. Congenit Heart Dis 6:228–233
Cohen MS, Marino BS, McElhinney DB, Robbers-Visser D, van der Woerd W, Gaynor JW, Spray TL, Wernovsky G (2003) Neo-aortic root dilation and valve regurgitation up to 21 years after staged reconstruction for hypoplastic left heart syndrome. J Am Coll Cardiol 42:533–540
Cozijnsen L, Braam RL, Waalewijn RA, Schepens MA, Loeys BL, van Oosterhout MF, Barge-Schaapveld DQ, Mulder BJ (2011) What is new in dilatation of the ascending aorta? Review of current literature and practical advice for the cardiologist. Circulation 123:924–928
Fernandes S, Khairy P, Graham DA, Colan SD, Galvin TC, Sanders SP, Singh MN, Bhatt A, Lacro RV (2012) Bicuspid aortic valve and associated aortic dilation in the young. Heart 98:1014–1019
Haycock GB, Schwartz GJ, Wisotsky DH (1978) Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr 93:62–66
Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA et al (2010) 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 121:e266–e369
Jain D, Dietz HC, Oswald GL, Maleszewski JJ, Halushka MK (2011) Causes and histopathology of ascending aortic disease in children and young adults. Cardiovasc Pathol 20:15–25
John AS, McDonald-McGinn DM, Zackai EH, Goldmuntz E (2009) Aortic root dilation in patients with 22q11.2 deletion syndrome. Am J Med Genet A 149A:939–942
John AS, Rychik J, Khan M, Yang W, Goldmuntz E (2014) 22q11.2 deletion syndrome as a risk factor for aortic root dilation in tetralogy of Fallot. Cardiol Young 24:303–310
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group, American Society of Echocardiography’s Group, Standards Committee, European Association of Echochardiography (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, Hilhorst-Hofstee Y, Jondeau G, Faivre L, Milewicz DM, Pyeritz RE, Sponseller PD, Wordsworth P, De Paepe AM (2010) The revised Ghent nosology for the Marfan syndrome. J Med Genet 47:476–485
Lopez L, Arheart KL, Colan SD, Stein NS, Lopez-Mitnik G, Lin AE, Reller MD, Ventura R, Silberbach M (2008) Turner syndrome is an independent risk factor for aortic dilation in the young. Pediatrics 121:e1622–e1627
Mahle WT, Sutherland JL, Frias PA (2010) Outcome of isolated bicuspid aortic valve in childhood. J Pediatr 157:445–449
McElhinney DB, Lacro RV, Gauvreau K, O’Brien CM, Yaroglu Kazanci S, Vogel M, Emani S, Brown DW (2012) Dilation of the ascending aorta after balloon valvuloplasty for aortic stenosis during infancy and childhood. Am J Cardiol 110:702–708
Padang R, Bannon PG, Jeremy R, Richmond DR, Semsarian C, Vallely M, Wilson M, Yan TD (2013) The genetic and molecular basis of bicuspid aortic valve associated thoracic aortopathy: a link to phenotype heterogeneity. Ann Cardiothorac Surg 2:83–91
Paterick TE, Humphries JA, Ammar KA, Jan MF, Loberg R, Bush M, Khandheria BK, Tajik AJ (2013) Aortopathies: etiologies, genetics, differential diagnosis, prognosis and management. Am J Med 126:670–678
Pepe G, Nistri S, Giusti B, Sticchi E, Attanasio M, Porciani C, Abbate R, Bonow RO, Yacoub M, Gensini GF (2014) Identification of fibrillin 1 gene mutations in patients with bicuspid aortic valve (BAV) without Marfan syndrome. BMC Med Genet 15:23
Schwartz ML, Gauvreau K, del Nido P, Mayer JE, Colan SD (2004) Long-term predictors of aortic root dilation and aortic regurgitation after arterial switch operation. Circulation 110:II128–II132
Tan JL, Gatzoulis MA, Ho SY (2006) Aortic root disease in tetralogy of Fallot. Curr Opin Cardiol 21:569–572
Verma S, Siu SC (2014) Aortic dilatation in patients with bicuspid aortic valve. N Engl J Med 370:1920–1929
Warren AE, Boyd ML, O’Connell C, Dodds L (2006) Dilatation of the ascending aorta in paediatric patients with bicuspid aortic valve: frequency, rate of progression and risk factors. Heart 92:1496–1500
Wooderchak-Donahue WL, O’Fallon B, Furtado LV, Durtschi JD, Plant P, Ridge PG, Rope AF, Yetman AT, Bayrak-Toydemir P (2012) A direct comparison of next generation sequencing enrichment methods using an aortopathy gene panel—clinical diagnostics perspective. BMC Med Genet 5:50
Yetman AT, Graham T (2009) The dilated aorta in patients with congenital cardiac defects. J Am Coll Cardiol 53:461–467
Zanjani KS, Niwa K (2013) Aortic dilatation and aortopathy in congenital heart diseases. J Cardiol 61:16–21
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Authors’ contributions
Dr Yuri Zarate conceptualized and designed the study, contributed to data collection and analysis, drafted the initial manuscript, and approved the final manuscript as submitted. Dr Elizabeth Sellars contributed to data collection and analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted. Mrs Tiffany Lepard contributed to data collection and analysis, reviewed and revised the manuscript, and approved the final manuscript as submitted. Dr Waldemar Carlo contributed to the interpretation of clinical data, critically reviewed the manuscript, and approved the final manuscript as submitted. Dr Xinyu Tang contributed to the statistical analysis and interpretation of clinical data, reviewed and revised the manuscript, and approved the final manuscript as submitted. Dr R. Thomas Collins II contributed to data analysis and interpretation of clinical data, reviewed and revised the manuscript, and approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Jaan Toelen
Rights and permissions
About this article
Cite this article
Zarate, Y.A., Sellars, E., Lepard, T. et al. Aortic dilation in pediatric patients. Eur J Pediatr 174, 1585–1592 (2015). https://doi.org/10.1007/s00431-015-2575-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-015-2575-8